Abstract
Thyroid-like follicular carcinoma (TLFC) of the kidney is an extremely rare type of renal tumor, which has not been classified under a known subtype of renal cell carcinoma. It is histologically similar to the primary thyroid follicular carcinoma; however, the characteristics lack thyroid immunohistochemical markers. The aim of the present study was to illustrate the clinical characteristics of 3 new cases along with a review of the literature. The patients were compared with regards to gender, age, location and size of the tumor, imageology, morphology, immunohistochemistry and prognosis. According to the limited data, TLFC occurs mainly in young women and its clinical manifestations have no difference with other renal tumors. Its imageological features resemble a large spectrum of benign and malignant renal and extra-renal conditions, which should be eliminated in the diagnostic process. Confirmed diagnosis depends on the examination of pathology and immunohistochemistry. Surgical ablation is the preferred therapeutic method. Currently, TLFC has a relatively good prognosis; however, this conclusion requires further cases and long-term follow-ups. Improving the understanding of TLFC can help avoid misdiagnosis and prevent inappropriate treatment.
Keywords: renal cell carcinoma, thyroid-like follicular carcinoma, clinical characteristics, pathology
Introduction
Cancers of the kidney and renal pelvis represent 3–4% of all adult malignancies (1) with renal cell carcinoma accounting for 80–85% (2). The World Health Organization Classification of Tumors (3) introduced several new entities in 2004, such as renal cell carcinoma (RCC) associated with neuroblastoma and mucinous tubular and spindle cell carcinoma. Thyroid-like follicular carcinoma of the kidney (TLFC) is a rare type of RCC that has not been included in this classification. TLFC is an unusual histological type of renal cell carcinoma, which is morphologically similar with follicular carcinoma of the thyroid, but is characteristically negative for thyroid immunohistochemical markers. First described in 1996 (4), only 23 cases have since been described (5–19). All the literature regarding TLFC are reports of isolated cases stating their morphological and immunohistochemical features. However, the clinical characteristics of gender, age, tumor size, location and their imageological features were seldom analyzed. The present study reports 3 new cases of TLFC focusing on their clinical characteristics, imageology, and morphology and immunohistochemistry profile. These cases were also combined with the previously published cases for a comprehensive study.
Case reports
Consent and specimens
Written informed consent was obtained from all the patients. Surgical specimens were fixed in 10% neutral buffered formalin, embedded in paraffin and serially sectioned into 4-µm sections. Routine staining with hematoxylin and eosin was performed. Immunohistochemistry was carried out using standard immunohistochemical techniques.
Data analysis was performed by SPSS 18.0 software (SPSS Inc., Chicago, IL, USA). The mean age of the male and female groups was calculated with an independent sample t-test.
Case 1
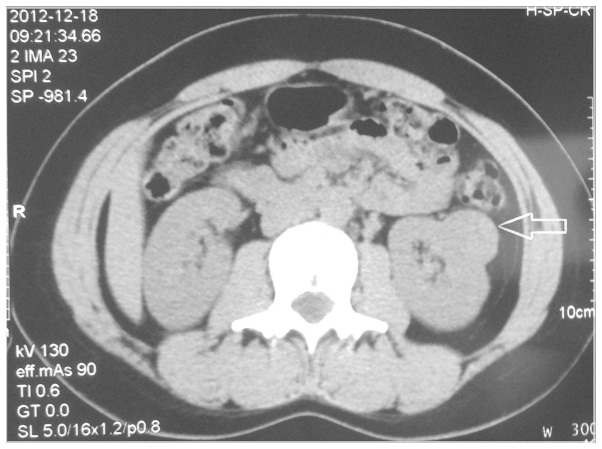
A 35-year-old woman was identified to have a renal mass during a return visit for left rib fractures. The patient had no haematuria, urinary tract infections or lower urinary tract symptoms, but had a history of ovarian teratoma and received surgical treatment 4 years previously. There were no relevant medical or family histories of note, or evident abnormalities detected by physical examinations. Laboratory data, including thyroid-function tests, were within normal limits. The computed tomography (CT) scan confirmed a 2.5×2.4×1.7 cm circumscribed soft tissue-like lesion protruding the renal cortex at the lower pole extending to the mid portion of the left kidney. The attenuation of the signals of the lesion was similar to the renal cortex (Fig. 1), with no clear enhancement following contrast medium administration (Fig. 2). Subsequent investigation with an ultrasound scan revealed a 2.8×2.7×2.7 cm solid nodule in the lower-middle section of the left kidney with a clear boundary and regular shape. The structure highlighted the outline of the kidney and it was echo-inhomogeneous. On color Doppler flow imaging, dot or streak blood flow was signaled in the nodule. On January 2013, the patient underwent a laparoscopic partial nephrectomy. During the surgery a tumor was identified that was confined to the lateral aspect of the middle pole of the left kidney with no evidence of protrusion outside the renal fascia or metastasis to regional lymph nodes. The postoperative course was uneventful and the patient was discharged 7 days later. Macroscopically, the gross specimen exhibited a well-circumscribed red-grey mass (3×3×2.8 cm). On the cut surface, the lesion was yellow-tan and soft. The tumor cells were immunoreactive for cytokeratin (CK) (Fig. 3A), CK18, CK19 and vimentin (Fig. 3B) and lacked immunoreactivity for CK117, human chromogranin A and synaptophysin. Postoperative follow-up, including CT scan, at 14 months revealed no evidence of metastatic or recurrent tumors, and the thyroid ultrasound findings were within the normal limits.
Figure 1.
Noncontrast coronal computed tomography scan shows a 2.5×1.7×5.8 cm mass in the lower pole extending to mid-portion of the left kidney (arrow).
Figure 2.
Postcontrast coronal computed tomography scan shows no evident enhancement in the lesion of the left kidney.
Figure 3.
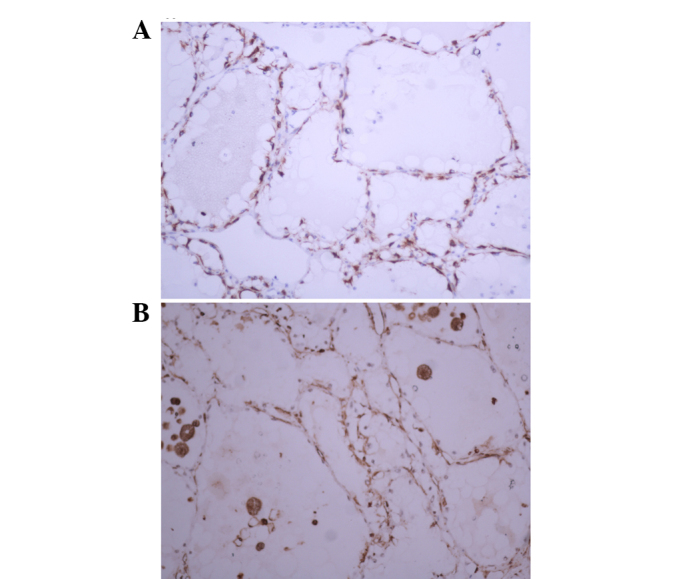
Strong immunoreactivity for (A) cytokeratin and (B) vimentin.
Case 2
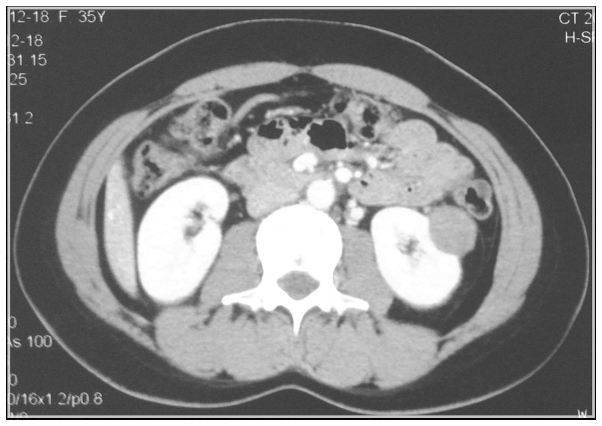
The patient was a 41-year-old man with no relevant family or social history. The patient was admitted to the Department of Emergency, Qilu Hospital (Jinan, Shandong, China) due to a sudden onset of gross hematuria, with a blood clot in the urine and left flank pain. A solid mass (6.5×6.1 cm) at the mid-pole of the left kidney was discovered by ultrasound examination. The patient subsequently underwent a CT scan that identified the existence of a fluid-filled round mass measuring 7.0 cm in its largest diameter in the middle section of the left kidney, which compressed the calyces and pelvis. The lack of enhancement following contrast and the existing high-density blood area suggested a final radiological diagnosis of a hemorrhagic cyst (Fig. 4). Combining clinical symptoms with imaging results, it was not believed to be a benign disease. Subsequently, the patient underwent a radical nephrectomy in October 2012. The radical nephrectomy specimen disclosed a renal mass that was breaking out of the renal fascia and protruding into the perinephric fat tissue. It was well-circumscribed, measuring 6.0 cm in the largest diameter and on section the tumor showed a tan to brown appearance with extensive necrosis. Hemorrhage was identified in the perinephric adipose. No renal vein invasion was identified. CK7 staining was positive. During the surgery, there was a large hematoma in the adipose capsule following the opening of the renal fascia, and the mass was located in the central and upper sections of the left kidney. Subsequently the mass was opened and there were a large number of necrotic tissues and hemorrhagic zones. The patient appeared well after 17 months, without any other signs of disease.
Figure 4.
Enhanced computed tomography scan shows the presence of a 7-cm fluid-filled round mass in the middle section of the left kidney, with a final diagnosis of a hemorrhagic cyst.
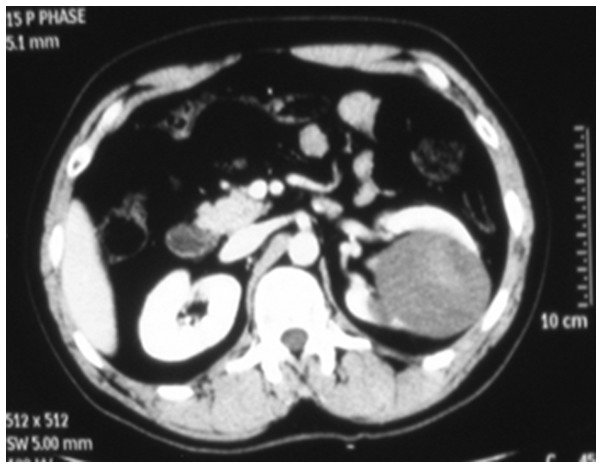
Case 3
A renal mass was incidentally discovered during a medical checkup in a 25-year-old woman with a past medical history of hypertension for 20 months. Clinical examinations were not noteworthy, except for blood pressure, which was 200/130 mmHg (1 mmHg = 0.133 KPa). Laboratory data, such as thyroid function, urinalysis, routine blood count, liver and kidney functions, and blood catecholamine were within the normal ranges. A computed tomography scan demonstrated a quasi-circular and well-circumscribed mass in the upper pole of the right kidney. The lesion was density-inhomogeneous and the renal vessel was pushed down. The patient underwent right partial nephrectomy in March 2011 under the clinical diagnosis of RCC. The gross specimen showed a well-circumscribed round mass measuring 2.5 cm in its largest diameter and it had a complete capsule. On the cut surface, the lesion was pale red to gray and was a multiloculated cystic. The necrosis that was present appeared coffee-like. The tumor exhibited strong and diffuse cytoplasmic/membranous reactivity for CK7, CK20, vimentin and epithelial membrane antigen. The blood pressure returned to normal following the surgery. At the 24-month follow-up the patient was alive without signs of tumor relapse.
Histological analysis
Histologically, all the tumors were characterized by a notable follicular architecture composed of macrofollicles and microfollicles filled with inspissated colloid-like material that mirrored follicular carcinoma of the thyroid (Fig. 5). The follicles were irregular and lined by cuboidal cells with finely granular cytoplasm and round to ovoid nuclei showing a fine chromatin pattern and inconspicuous nucleoli. Mitotic activity was absent. All the tumors were well-circumscribed with a distinct fibrous capsule.
Figure 5.
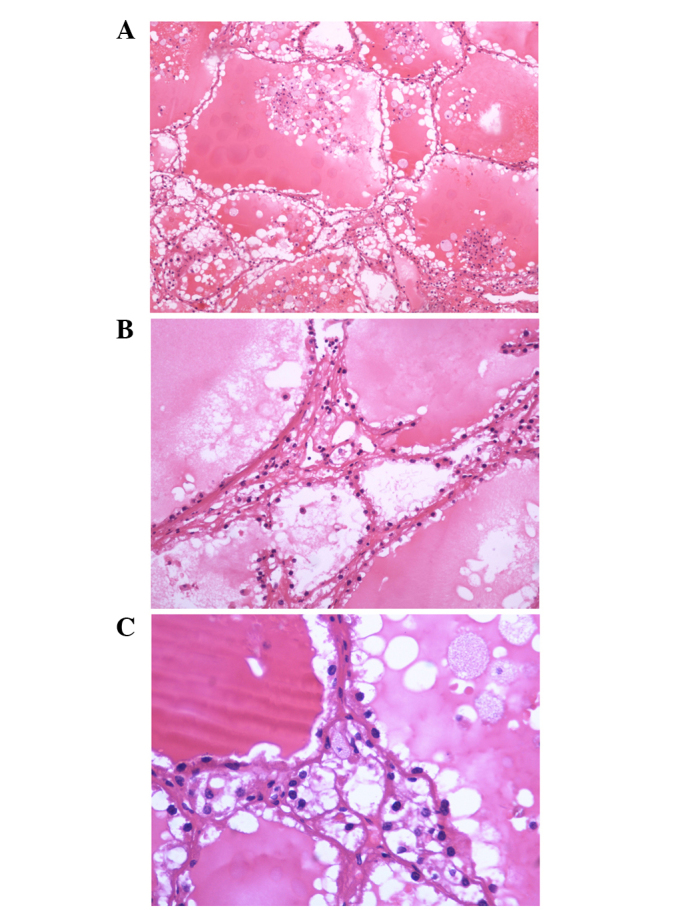
(A) Follicles of various sized are filled with colloid-like material (hematoxylin and eosin; original magnification, ×100). (B) Follicles are lined by cuboidal cells with scant eosinophilic cytoplasm and round to oval nuclei with evenly distributed chromatin (hematoxylin and eosin; original magnification, ×200). (C) Nucleic features show round nuclear contours, uniform chromatin distribution and occasional nucleoli (hematoxylin and eosin; original magnification, ×400).
Immunohistochemical analysis
Immunohistochemical studies identified that the histogenetic markers for follicular cell origins, which are thyroglobulin and thyroid transcription factor-1, were negative in all lesions.
The clinicopathological characteristics and immunohistochemical profile of the present and previously reported cases are listed in Table I.
Table I.
Clinicopathological characteristics and immunohistochemical profile of the present and previously reported cases.
| (Refs.) | Cases, n | Age, years/gender | Clinical presentation | Tumor size, cm | Location | pTNM | Follow-up, months | Negative immunohistochemical markers | Positive immunohistochemical markers |
|---|---|---|---|---|---|---|---|---|---|
| (4) | 1 | 39/F | Abdominal pain | 1.5 | Right kidney/lower pole | pT1aN0 | 18 | CD15 | TG, estrogen receptor |
| (5) | 6 | 53/F | Incidental | 2.1 | Right kidney/mid-pole | pT1aNx | 54 | PAX-2, RCC, CD10, WT-1, | CK7 (1 case) |
| 29/F | Incidental | 1.9 | Right kidney/upper pole | pT1aNx | 84 | Ksp-cadherin, α-methyl-CoA | |||
| 45/M | Incidental | 3.5 | Right kidney/lower pole | pT1aN1 | 17 | racemase, vimentin, CD56, | |||
| 83/M | Incidental | 2.1 | Left kidney/lower pole | pT1aNx | 48 | CD57, TG, TTF-1 | |||
| 35/M | Incidental | 3.0 | Right kidney/mid-pole | pT1aNx | 20 | ||||
| 50/F | Incidental | 4.0 | Right kidney/mid-pole | pT1aN0 | 7 | ||||
| (6) | 1 | 32/F | Incidental | 11.8 | Right kidney/lower and mid-pole | pT2Nx | 6 | CK, 34βE12, CK7, CK19, CK20, CD15, EMA, CEA, TG, TTF-1 | CK, AE1/AE3, CD10, CK 35βH11 (focal), vimentin (focal) |
| (7) | 1 | 31/F | Flank pain, weight loss and gross hematuria | 4.0 | Left kidney/upper and mid-pole | pT1aN0 | 21 | CK20, CD10, TG, TTF-1, α-methyl-CoA racemase, | CK, AE1/AE3, CK7, CK19, vimentin, RCC, galectin-3, HBME-1, PAX-2 |
| (8) | 1 | 34/F | Gross hematuria, right flank pain | 6.2 | Right kidney/mid-pole | pT1bN2M1 | 3 | CK20, TG, TTF-1, CD10, CD117, RCC, CEA, WT-1, α-methy-CoA racemase, p63 | In the lungs: PAX-2, PAX-8, CK7, CK5, vimentin, EMA, N-cadherin; in the kidneys PAX-2, vimentin, CK7 |
| (9) | 1 | 29/F | Incidental | 5.0 | Left kidney/mid-pole | pT1bNoM1 | 60 | CD10, CD117, TG, TTF-1 | CAM 5.2, CK7, CK20, vimentin |
| (10) | 2 | 76/M | Gross hematuria | 4.5 | Left kidney/upper pole | pT1bN0 | 11 | CK20, CD10, RCC, CEA, WT-1, | CK7, CK19, EMA, vimentin, |
| 41/F | Incidental | 4.3 | Right kidney/lower pole | pT1bNx | 4 | chromogranin, Syn, CD56, NSE, TG, TTF-1, galectin-3, HBME-1, Ulex europaeus lectin | 34βE12 (focal), E-cadherin (focal) | ||
| (11) | 1 | 29/F | Abdominal pain | 6.5 | Left kidney/lower pole | pT1bN0M0 | 4 | TTF-1, CD117, CK20, TG | EMA, vimentin, CD10 (focal), CK7 (focal) |
| (12) | 1 | 26/F | Incidental | 4.0 | Right kidney/upper and mid-pole | pT1aNxMx | Unknown | TTF-1, TG, TPO, CK20, RCC, ER, PR, WT-1, CAM 5.2, CK7, CD57, CD56, Syn, CgA | CK AE1/AE3, CAM 5.2, CK7, vimentin, CD10 (weakly), EMA (focal) |
| (13) | 1 | 34/M | Left flank pain | 5.5 | Left kidney/lower pole | pT1bNx | 6 | RCC, CD10, CD15, CD56, CD117, CEA, CK20, TFE3, TG, TTF-1, WT-1 | CAM5.2, P504S, vimentin, CK7, CK34β12, EMA, CK AE1/AE3, |
| (14) | 1 | 36/F | Gross hematuria | 10.0 | Left kidney | pT2N1M0 | 12 | RCC, CD117, TTF-1, TG, WT-1, CgA, Syn | EMA, vimentin, CK7, CD10 (focal), CD15 (focal), CD99 (focal) |
| (15) | 1 | 22/F | Gross hematuria | 8.0 | Left kidney | pT2N0M0 | Unknown | TG, TTF-1, vimentin, CD63, P63 | CKpan, CK19, EMA, CK7 (focal), CK20 (focal), NSE (focal), Syn (focal) |
| (16) | 1 | 66/M | Gross hematuria, right flank pain | 8.0 | Right kidney | pT3aN0 | 20 | TG, TTF-1, WT-1, CD117, AMACR, 34BE12, Syn, CK20, CD56, CD34, CD57, CD99, CD15 | Ckpan, vimentin, EMA, NSE, CK7 (focal), CK19 (focal) |
| (17) | 1 | 68/F | Relapsing urinary infection | 1.1 | Right kidney/mid pole | pT1aN0M0 | 6 | CD10, 504 s protein, TTF-1, TG | EMA, CK7 (focal), CK19, CKAE1/AE3 (focal), CK34Be 12 (focal), vimentin, CD117 |
| (18) | 1 | 19/F | Abdominal pain | 2.0 | Right kidney/lower pole | pT3aN0M0 | 21 | TTF-1, TG, CD10, CD56, WT-1, SMMHC, CEA, S-100 | CK7, AE1/AE3, EMA, PAX-2, PAX-8B |
| (19) | 2 | 65/M | Hematuria and right back pain | 8.0 | Right kidney/middle-lower pole | pT2N0M0 | 15 | CK20, CK10, TTF-1, TG, | CK7 (focal), CK19, EMA, |
| 59/M | Incidental | 5.2 | Right kidney/middle-lower pole | pT1aN0M0 | 1 | TTF-1, TG | CK7, CK20, EMA | ||
| Present | 3 | 35/F | Incidental | 2.8 | Left kidney/lower and mid-pole | pT1aN0M0 | 14 | CD10, CK7, CD68, TG, TTF-1 | CK, CK18, CK19, vimentin |
| 38/M | Gross hematuria, left flank pain | 6.0 | Left kidney/upper and mid-pole | pT3aN0M0 | 17 | TTF-1, TG | CK7 | ||
| 25/F | Incidental | 2.5 | Right kidney/upper pole | pT1aN0M0 | 24 | CD117, TTF-1, TG, CgA, Syn | EMA, vimentin, CK7, CK20 |
M, male; F, female; CD, cluster of differentiation; PAX-2, paxillin-2; RCC, renal cell carcinoma; WT-1, Wilms' tumor gene 1; TG, thyroglobulin; TTF-1, thyroid transcription factor-1; CK, cytokeratin; CEA, carcinoembryonic antigen; EMA, epithelial membrane antigen; HBME, human bone marrow endothelial; Syn, synaptophysin; NSE, neuron-specific enolase; CAM 5.2, cell adhesion molecule 5.2; AMACR, α-methylacyl-CoA racemase; SMMHC, smooth muscle myosin heavy chain.
Discussion
Primary TLFC of the kidney is a rare entity, with only 23 cases reported in the literature to date (Table I) (4–19). First described by Angell et al (4) in 1996, several cases have since emerged. In the current study, among all the reported cases, the mean age was 42.3 years (range, 19 to 83 years; median, 35.5 years), and women were the majority of the patients (17/26, 65.38%) with a significant difference in the age of onset between males and females (P<0.05). RCC occurs twice as often in men compared to women (2), and patients are generally >40 years at diagnosis, predominantly in the seventh decade of life (20). However, TLFC was more common in young females (average, 35.17 years), with 76.4% (13/17) of female patients <40 years old. It should be noted that TLFC is different from common RCC in terms of epidemiology.
The mean tumor size was 4.75 cm (range, 1.1 to 11.8 cm; median, 4.2 cm). All the tumors were unilateral renal diseases with 38.46% (10/26) located in the left kidney, while 61.54% (16/26) were located on the right side. The tumor was an incidental finding in 13 patients, but 13 others were symptomatic. Evidently, gross hematuria occurred most frequently among all the symptoms, followed by flank or abdominal pain. The clinical manifestations of TLFC had no difference with other renal tumors. Although the majority of cases were low grade with an indolent course, one presented with renal hilar lymph node involvement (tumor diameter, 3.5 cm) (5), one had widespread retroperitoneal lymph node and lung metastases at presentation (tumor diameter, 6.2 cm) (8), and another was identified to focus in the lower left lung lobe, the biopsy of which presented identical histomorphology as a renal tumor 2 months after nephrectomy (tumor diameter, 5.0 cm) (9), highlighting the low but distinct malignant potential of these tumors. Despite this, all 9 patients were alive and disease-free at a mean follow-up of 20.5 months.
The imageological features of TLFC resemble a large spectrum of benign and malignant renal and extra-renal conditions, which should be eliminated in the diagnostic process. In order to improve the understanding of its imageological features, the present cases are listed with the previously reported cases in Table II. Using the limited data, TLFC was observed to present a cystic or solid change and sometimes combines with the necrotic or hemorrhagic area. The most prominent feature of TLFC was the nearly no measurable enhancement following contrast administration, which is different from the common form of RCC and should be distinguished from the renal benign tumor. Ultrasound scan and magnetic resonance imaging can also be used in the preoperative diagnosis. In order to avoid misdiagnosis and over-treatment, ultrasound-guided fine needle aspiration biopsy is sometimes necessary.
Table II.
Imageological features of the present and the previously reported cases.
| (Refs.) | Cases, n | Computed tomography scan | Ultrasonography | Magnetic resonance imaging |
|---|---|---|---|---|
| (4) | 1 | A solid, irregular, enhancing lesion | A hyper-echoic lesion | |
| (6) | 1 | A relatively homogeneously enhancing mass | ||
| (7) | 1 | A enhancing heterogeneous mass | ||
| (9) | 1 | An echo-inhomogeneous lesion with a 5-mm broad edematous border | ||
| (10) | 1 | A round moderately hyperdense and well-vascularized solid mass with a necrotic central area | ||
| 1 | A fluid-filled round mass. The lack of enhancement after contrast and the presence of septa | A round mass with solid septa | ||
| (11) | 1 | A lobulated, low-attenuation lesion, no measurable enhancement following contrast administration | A complex multi-septated, partly cystic mass | No haemorrhagic component, no enhancement following gadolinium |
| (12) | 1 | A solid, homogeneous lesion, mild enhancement following contrast administration | A hyper-echoic lesion | |
| (13) | 1 | A hyper-echogenic cyst | ||
| (16) | 1 | A heterogeneous mass with soft tissue, mild enhancement following contrast administration | A echo-inhomogeneous lesion, with streak blood flow signals | |
| (17) | 1 | A partially cystic enhancing lesion | No enhancement following gadolinium injection | |
| (18) | 1 | A heterogeneous, hyperdense, and partiallyexophytic lesion | ||
| (19) | 1 | A heterogeneous enhancing lesion | A solid mass with hypoechogenicity | A mass with involvement of the renal fascia |
| 1 | A heterogeneous enhancing lesion with thickened renal fascia | |||
| Present | 1 | A circumscribed soft tissue-like lesion, no obvious enhancement following contrast administration | A echo-inhomogeneous lesion, with dot or streak blood flow signals | |
| 1 | A fluid-filled round mass with blood high-density area, no obvious enhancement following contrast | A mild echo-inhomogeneous solid lesion, without blood flow signals | ||
| 1 | A density-inhomogeneous mass, well-circumscribed |
On gross examination, all the tumors were circumscribed with or without areas of hemorrhage and necrosis. Two of the tumors grossly protruded into the renal pelvis cavity (6,15) and another focally extended into the perinephric adipose tissue (10). The unique histological features of this tumor are identical to the findings in the present report, with widespread macrofollicles and microfollicles containing abundant colloid-like material, bearing a striking resemblance to follicular carcinoma of the thyroid gland. Immunohistochemically, the TLFC described in the literature varied, except for that the majority of cases were consistently negative for thyroid transcription factor-1 (TTF-1) and thyroglobulin, which are markers of thyroid carcinoma (Table I).
TLFC of the kidney should be distinguished from thyroidization of the kidney, metastatic follicular carcinoma from a primary thyroid tumor and metastasis from an ovarian teratoma composed of thyroid tissue (struma ovarii).
Thyroidization of the kidney is a benign process that extensively involves the kidney, most frequently as a consequence of end-stage renal diseases or pyelonephritis. It is characterized by atrophic distal tubules and collecting ducts with colloid-like material in the lumen (21,22). However, this is a benign phenomenon that is typically bilateral and widespread, as opposed to TLFC, which is well-circumscribed and occurs in patients without renal disease, as in the present cases.
Metastatic thyroid follicular carcinoma to the kidney is extremely rare and only 16 cases have been reported, all but 1 occurring in the presence of widespread metastatic disease involving other organs (23–25). It can be easily distinguished from TLFC of the kidney by its positive immunohistochemical staining for TTF-1 and thyroglobulin.
In case 1, the patient had a history of ovarian teratoma and received surgical treatment 4 years ago. Therefore, a hypothetical metastasis from a malignant ovarian lesion was eliminated. Struma ovarii is a germ cell tumor of the ovary mainly composed of thyroid tissue: Malignant transformation is rare and localized to the liver, peritoneum and omentum. To the best of our knowledge, there are no previous cases of struma ovarii metastasizing to the kidney. In any case, pelvis imaging would be expected to reveal an ovarian tumour, and the tissue would show positive immunoreactivity to TTF-1 and thyroglobulin (26). These two features were absent in the present case. The pelvic ultrasound was normal and immunoreactivity was negative for TTF-1 and thyroglobulin.
Surgery is the main treatment for TLFC of the kidney. The surgical options contain radical nephrectomy, robotic-assisted partial nephrectomy and laparoscopic partial nephrectomy. Limited data indicate that this tumor behaves in a low malignant manner and the majority of patients have a good prognosis; however, more cases and long-term follow-ups are required.
In conclusion, the present study reports 3 new cases of TLFC, which is a rare variant of RCC with unique morphological and immunohistochemical features. Based on the previously reported cases, TLFC occurs mainly in young women and its clinical manifestations have no difference with other renal tumors. Its imageological features resemble a large spectrum of benign and malignant renal and extra-renal conditions, which should be eliminated in the diagnostic process. Confirmed diagnosis depends on the examinations of pathology and immunohistochemistry. Surgical ablation is the preferred therapeutic method. To date, the disease appears to have a good prognosis, however, it requires the accumulation of more cases and long-term follow-ups.
Acknowledgements
The present study was supported by the National Natural Science Foundation of China (grant nos. 81470987 and 81170702), and the Science and Technology Development Project of Shandong Province (grant no. 2014GSF118054).
Glossary
Abbreviations
- RCC
renal cell carcinoma
- TG
thyroglobulin
- TLFC
thyroid-like follicular carcinoma
- TTF-1
thyroid transcription factor-1
- CT
computed tomography
- CK
cytokeratin
- EMA
epithelial membrane antigen
- Syn
synaptophysin
- CD
cluster of differentiation
- CEA
carcinoembryonic antigen
- PAX
paxillin
- HBME
human bone marrow endothelial
- CAM
cell adhesion molecule
References
- 1.Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ. Cancer statistics, 2007. CA Cancer J Clin. 2007;57:43–66. doi: 10.3322/canjclin.57.1.43. [DOI] [PubMed] [Google Scholar]
- 2.Kosary CL, McLaughlin JK. Kidney and renal pelvis. SEER Cancer Statistics Review. In: Miller BA, Ries LAG, Hankey BF, et al., editors. 1973–1990. Bethesda, MD: National Cancer Institute; 1993. NIH publication no. 93–2789, XI.1-XI.22. [Google Scholar]
- 3.Eble JN, Sauter G, Epstein JI, Sesterhenn IA, editors. World Health Organization Classification of Tumours. 3rd. Lyon: IARC Press; 2004. Pathology and genetics of tumours of the urinary system and male genital organs. [Google Scholar]
- 4.Angell SK, Pruthi R, Freiha FS. Primary thyroid-like carcinoma of the kidney. Urology. 1996;48:632–635. doi: 10.1016/S0090-4295(96)00223-3. [DOI] [PubMed] [Google Scholar]
- 5.Amin MB, Gupta R, Ondrej H, McKenney JK, Michal M, Young AN, Paner GP, Junker K, Epstein JI. Primary thyroid-like follicular carcinoma of the kidney: Report of 6 cases of a histologically distinctive adult renal epithelial neoplasm. Am J Surg Pathol. 2009;33:393–400. doi: 10.1097/PAS.0b013e31818cb8f5. [DOI] [PubMed] [Google Scholar]
- 6.Jung SJ, Chung JI, Park SH, Ayala AG, Ro JY. Thyroid follicular carcinoma-like tumor of kidney: A case report with morphologic, immunohistochemical and genetic analysis. Am J Surg Pathol. 2006;30:411–415. doi: 10.1097/01.pas.0000194745.10670.dd. [DOI] [PubMed] [Google Scholar]
- 7.Khoja HA, Almutawa A, Binmahfooz A, Aslam M, Ghazi AA, Almaiman S. Papillary thyroid carcinoma-like tumor of the kidney: A case report. Int J Surg Pathol. 2012;20:411–415. doi: 10.1177/1066896911429942. [DOI] [PubMed] [Google Scholar]
- 8.Dhillon J, Tannir NM, Matin SF, Tamboli P, Czerniak BA, Guo CC. Thyroid-like follicular carcinoma of the kidney with metastases to the lungs and retroperitoneal lymph nodes. Hum Pathol. 2011;42:146–150. doi: 10.1016/j.humpath.2010.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sterlacci W, Verdorfer I, Gabriel M, Mikuz G. Thyroid follicular carcinoma-like renal tumor: A case report with morphologic, immunophenotypic, cytogenetic, and scintigraphic studies. Virchows Arch. 2008;452:91–95. doi: 10.1007/s00428-007-0486-4. [DOI] [PubMed] [Google Scholar]
- 10.Alessandrini L, Fassan M, Gardiman MP, Guttilla A, Zattoni F, Galletti TP, Zattoni F. Thyroid-like follicular carcinoma of the kidney: Report of two cases with detailed immunohistochemical profile and literature review. Virchows Arch. 2012;461:345–350. doi: 10.1007/s00428-012-1298-8. [DOI] [PubMed] [Google Scholar]
- 11.Malde S, Sheikh I, Woodman I, Fish D, Bilagi P, Sheriff MK. Primary thyroid-like follicular renal cell carcinoma: An emerging entity. Case Rep Pathol. 2013;2013:687427. doi: 10.1155/2013/687427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu HW, Chen WJ, You Y, Cui QC, Liu TH. Clinicopathologic characteristics of primary thyroid-like follicular carcinoma in kidney. Zhonghua Bing Li Xue Za Zhi. 2013;42:37–41. doi: 10.3760/cma.j.issn.0529-5807.2013.01.008. (In Chinese) [DOI] [PubMed] [Google Scholar]
- 13.Volavšek M, Strojan-Fležar M, Mikuz G. Thyroid-like follicular carcinoma of the kidney in a patient with nephrolithiasis and polycystic kidney disease: A case report. Diagn Pathol. 2013;8:108. doi: 10.1186/1746-1596-8-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xu H, Zhang WY. Clinicopathological features of thyroid follicular carcinoma-like renal cell carcinoma. Chin J Diag Pathol. 2010;17:46–49. [Google Scholar]
- 15.He CN, Li P, Zhao HF, Zhai JP, Liu YQ, Ma LN. Thyroid follicular carcinoma-like tumor of kidney: Report of a case. Zhonghua Bing Li Xue Za Zhi. 2008;37:428–430. (In Chinese) [PubMed] [Google Scholar]
- 16.Li XD, Xu N, Xue XY, Zheng QS, Li GP, Wei Y, Jiang T, Huang JB. Thyroid follicular carcinoma-like tumor of kidney: A case report and literature review. J Mod Urol. 2013;18:2. [Google Scholar]
- 17.Ghaouti M, Roquet L, Baron M, Pfister C, Sabourin JC. Thyroid-like follicular carcinoma of the kidney: A case report and review of the literature. Diagn Pathol. 2014;9:186. doi: 10.1186/s13000-014-0186-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu WW, Chu JT, Nael A, Rezk SA, Romansky SG, Shane L. Thyroid-like follicular carcinoma of the kidney in a young patient with history of pediatric acute lymphoblastic leukemia. Case Rep Pathol. 2014;2014:313974. doi: 10.1155/2014/313974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lin YZ, Wei Y, Xu N, Li XD, Xue XY, Zheng QS, Jiang T, Huang JB. Thyroid-like follicular carcinoma of the kidney: A report of two cases and literature review. Oncol Lett. 2014;7:1796–1802. doi: 10.3892/ol.2014.2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cao Y, Paner GP, Perry KT, Flanigan RC, Campbell SC, Picken MM. Renal neoplasms in younger adults: Analysis of 112 tumors from a single institution according to the new 2004 World Health Organization classification and 2002 American Joint Committee on Cancer Staging System. Arch Pathol Lab Med. 2005;129:487–491. doi: 10.5858/2005-129-487-RNIYAA. [DOI] [PubMed] [Google Scholar]
- 21.Laberke HG, Klingebiel T, Quack G. A contribution to the morphology and pathogenesis of thyroid-like lesions in the kidney. Pathol Res Pract. 1983;176:284–296. doi: 10.1016/S0344-0338(83)80018-1. [DOI] [PubMed] [Google Scholar]
- 22.Nadasdy T, Laszik Z, Blick KE, Johnson DL, Silva FG. Tubular atrophy in the end-stage kidney: A lectin and immunohistochemical study. Hum Pathol. 1994;25:22–28. doi: 10.1016/0046-8177(94)90166-X. [DOI] [PubMed] [Google Scholar]
- 23.Garcia-Sanchis L, Lopez-Aznar D, Oltra A, Rivas A, Alonso J, Montalar J, Mateo A. Metastatic follicular thyroid carcinoma to the kidney: A case report. Clin Nucl Med. 1999;24:48–50. doi: 10.1097/00003072-199901000-00010. [DOI] [PubMed] [Google Scholar]
- 24.Matei DV, Verweij F, Scardino E, Rocco B, Renne G, Tradati N, De Cobelli O. Late solitary thyroid carcinoma metastasis to the kidney: A case report. Anticancer Res. 2003;23:561–564. [PubMed] [Google Scholar]
- 25.Regojo Balboa JM, Sánchez Zalabardo D, Rioja Zuazu J, Fernández Montero JM, López Ferrandis J, Zudaire Bergera JJ, Rosell Costa D, Robles García JE, Berián Polo JM. Follicula carcinoma of the thyroid manifested initially asympton primary renal neoplasm. Actas Urol Esp. 2004;28:308–310. doi: 10.1016/s0210-4806(04)73079-x. (In Spanish) [DOI] [PubMed] [Google Scholar]
- 26.Robboy SJ, Shaco-Levy R, Peng RY, Snyder MJ, Donahue J, Bentley RC, Bean S, Krigman HR, Roth LM, Young RH. Malignant struma ovarii: An analysis of 88 cases, including 27 with extraovarian spread. Int J Gynecol Pathol. 2009;28:405–422. doi: 10.1097/PGP.0b013e3181a27777. [DOI] [PubMed] [Google Scholar]