SUMMARY OF THE ISSUES
Restless leg syndrome (RLS) is a common yet frequently underdiagnosed disorder. This condition comprises the symptoms of spontaneous continuous leg movements associated with unpleasant paresthesias.1 These symptoms occur only at rest, and are relieved by movement. RLS is divided into two categories, primary, in which the etiology is idiopathic, and secondary, which is most commonly associated with iron-deficiency anemia, uremia, diabetes mellitus, and rheumatoid arthritis.2
The diagnosis of RLS is missed because there is no single test that can diagnose this condition. The International Restless Legs Study Group has proposed the following four criteria essential in diagnosis of RLS:3
An urge to move the legs, accompanied with or caused by unpleasant sensations in the legs. Sometimes the urge is present without unpleasant sensations, and sometimes these sensations are present in arms;
Urge to move the legs is present when resting or inactive;
Urge to move the legs is partially or totally relieved with movement;
Urge to move or unpleasant sensations are worse at night time as compared to day or only occur at night.
Confirmation of diagnosis can be supplemented with family history and positive response to dopaminergic drugs.
False positive diagnosis of RLS have been reported in more than 10% of the investigated populations and included conditions such as nocturnal cramps and various neuropathies. In addition, RLS may be underdiagnosed because of poor recognition of symptoms. No guideline has been published describing how the criteria should be applied, and there is a lack of information about how essential and supportive criteria or associated features are related.
SUMMARY OF THE EVIDENCE
A diagnostic algorithm for the diagnosis of RLS, the RLS-Diagnostic Index (RLS-DI), has been validated for use by non-experts.4 The RLS-DI:
Identifies patients with a definite diagnosis of RLS;
Excludes the diagnosis of RLS in other patients; and
Sorts out a subgroup of patients in whom RLS is possible and cannot be safely excluded or confirmed at the time of the interview without further diagnostic information
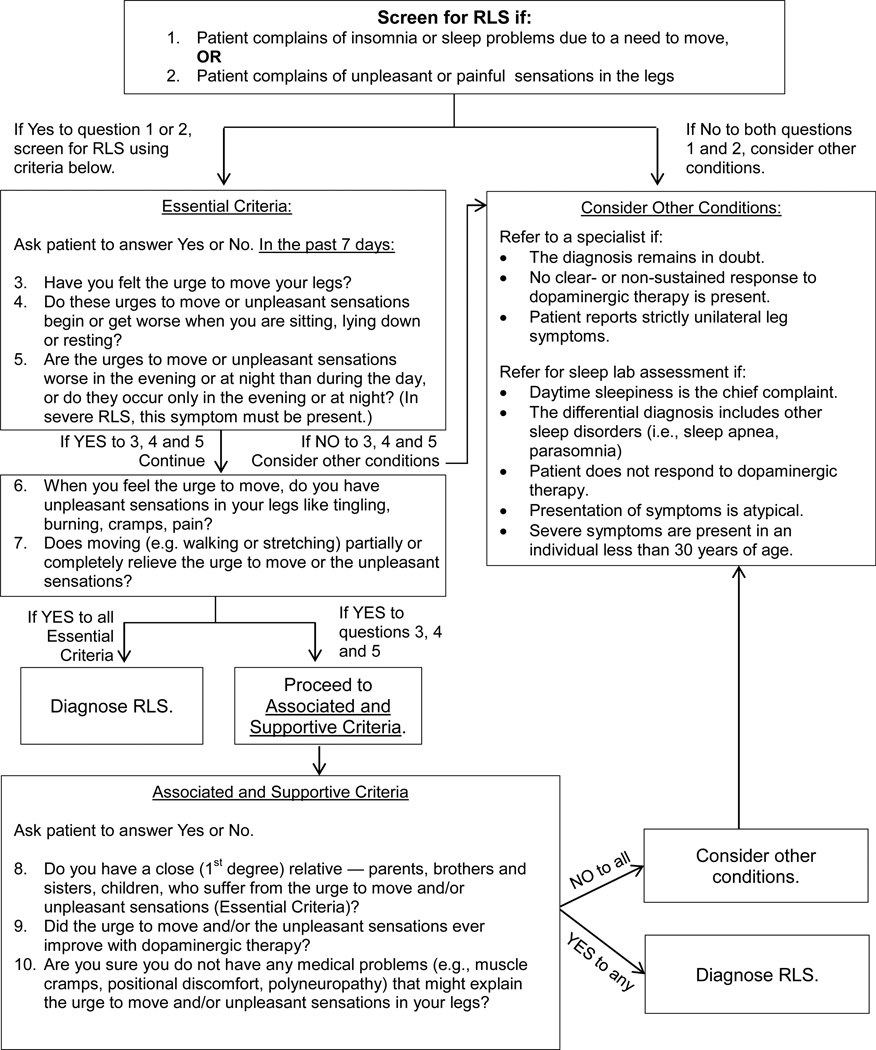
The RLS-DI consists of 10 items which are related to the essential diagnostic criteria established by the International Study Group as well as their supportive criteria and features associated with RLS. The sensitivity and specificity of the 10 RLS-DI items were based on clinical expert diagnosis, which represented the “true” diagnosis. According to RLS-DI, any patient who presents with: 1. insomnia or sleep problems due to a need to move, and/or 2. unpleasant sensations in legs should be screened for RLS. Questions 3 through 7, the Essential Criteria, should be asked of the patient as shown in the RLS diagnostic algorithm (Figure 1).
Figure 1.
The RLS Diagnostic Algorithm
If the patients answers Yes to all 5 Essential Criteria questions, then the patient is given a diagnosis of RLS. If the patient answers Yes to questions 3, 4 and 5 only, then the questions from the Associated and Supportive Criteria should be considered (see Figure 1). If the answer is Yes to any one of the Associated and Supportive Criteria, a diagnosis of RLS is given.
If the patient answers No to all Essential Criteria questions or to questions 3, 4 and 5, other conditions should be considered. Similarly, if the patient answers Yes to questions 3, 4 and 5 and No to questions 8, 9 and 10 on the diagnostic algorithm (Figure 1), other diagnoses should be considered as the possible etiology of the patient’s symptoms.
The RLS-DI was administered in a telephone interview to 179 individuals (86 with RLS, 93 with other sleep disorders) from one sleep center in Germany.4 The study participants were patients who were seen in a sleep lab for sleep related disorders between January 01, 2003 and September 30, 2004. To improve the quality of the interview, interview questions were mailed beforehand to individuals who agreed to participate. Two well-trained interviewers conducted the interviews between November 2004 and January 2005. These interviewers were not sleep experts. Two senior physician sleep specialists provided RLS expert diagnosis for each individual, and that diagnosis was used to validate the RLS-DI study. The results demonstrated a sensitivity of 93.0% and a specificity of 98.9%. Agreement with the sleep specialist diagnosis occurred in 96.1% of the patients.
Garcia-Borreguero et al4 reanalyzed the data from a validation study of the RLS-DI using a logistic regression model to determine the extent of accuracy of the diagnosis of RLS. This analysis confirmed that items 3, 4 and 5 of the Essential Criteria had the most diagnostic value. Yes to question 9 of the Associated and Supportive Criteria (positive response to dopaminergic therapy) further improved the accuracy of the diagnosis of RLS (Figure 1).
CONCLUSION
RLS is a common yet frequently underdiagnosed disorder. Given the impact of RLS on quality of life and the therapeutic efficacy of current treatments in improving these symptoms, early identification and treatment of RLS is highly relevant. Thus, it is important for primary care providers to be familiar with diagnostic criteria for RLS.
Using the diagnostic algorithm shown in Figure 1, the diagnosis of RLS can be given with reasonable confidence at two points. Proceeding through the algorithm, if a patient answers Yes to all five Essential Criteria, the patient has RLS.
If the patient answers Yes to questions 3, 4 and 5 on the algorithm, then the clinician can proceed to ask the Associated and Supportive Criteria questions. If the answer is Yes to any of those questions, it is highly likely the patient have RLS. When there is a high suspicion of RLS and the patient has not received dopaminergic therapy, a positive response to these medications can confirm the diagnosis of RLS and exclude other disorders that mimic RLS.
If an individual presents in clinic with symptoms concerning for RLS, physicians should consider using the RLS Diagnostic Index, as displayed in Figure 1, to better diagnose this condition.
Inclusion and Exclusion Criteria.
Inclusion Criteria: Published clinical reviews, systematic reviews/meta-analysis and clinical research trials on diagnostic criteria and algorithms for Restless Leg Syndrome (RLS).
Exclusion Criteria: Other sleep-related disorders that do not meet the diagnostic criteria for RLS
REFERENCES
- 1.Allen RP, Picchietti D, Hening WA, Trenkwalder C, Walters AS, Montplaisir J. Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med. 2003;4(2):101–119. doi: 10.1016/s1389-9457(03)00010-8. [DOI] [PubMed] [Google Scholar]
- 2.Beneš H, vonEye A, Kohnen R. Empirical evaluation of the accuracy of diagnostic criteria for Restless Legs Syndrome. Sleep Med. 2009;10(5):524–530. doi: 10.1016/j.sleep.2008.06.007. [DOI] [PubMed] [Google Scholar]
- 3.Garcia-Borreguero D, et al. Algorithms for the diagnosis and treatment of restless legs syndrome in primary care. BMC Neurol. 2011;11:28. doi: 10.1186/1471-2377-11-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beneš H, Kohnen R. Validation of an algorithm for the diagnosis of Restless Legs Syndrome: The Restless Legs Syndrome-Diagnostic Index (RLS-DI) Sleep Med. 2009;10(5):515–523. doi: 10.1016/j.sleep.2008.06.006. [DOI] [PubMed] [Google Scholar]