Abstract
The aim of this paper was to study sound source localization by cochlear implant (CI) listeners with low-frequency (LF) acoustic hearing in both the operated ear and in the contralateral ear. Eight CI listeners had symmetrical LF acoustic hearing (symm) and four had asymmetric LF acoustic hearing (asymm). The effects of two variables were assessed: (i) the symmetry of the LF thresholds in the two ears and (ii) the presence/absence of bilateral acoustic amplification. Stimuli consisted of low-pass, high pass, and wide-band noise bursts presented in the frontal horizontal plane. Localization accuracy was 23 degrees of error for the symm listeners and 76 degrees of error for the asymm listeners. The presence of a unilateral CI used in conjunction with bilateral LF acoustic hearing does not impair sound source localization accuracy, but amplification for acoustic hearing can be detrimental to sound source localization accuracy.
Keywords: hearing preservation, localization, cochlear implants, hearing aids, acoustic hearing
One benefit of listening with two ears vs. one ear for individuals with normal hearing (NH) is the ability to localize sound sources on the horizontal plane with high accuracy – i.e., 6 – 7 degrees of error (e.g., Grantham et al., 2007; Yost et al., 2013). Localization ability is contingent on access to interaual level difference (ILD) cues in high frequencies (above 1.5kHz) and/or interaural time difference (ITD) cues in low frequencies (under 1.0kHz) (Blauert, 1997). Patients with unilateral hearing – such as that offered by a single cochlear implant (CI) lack access to interaural cues and thus, most commonly, demonstrate very poor performance on tests of sound source localization. Grantham et al. (2007) reported near chance levels of sound source localization by CI patients using a single CI. In contrast, patients with bilateral CIs do have access to interaural cues. Multiple studies have shown that bilateral patients have access to ILD cues but not ITD cues (e.g., Grantham et al., 2008) and show modest levels of sound source localization ability, e.g., 20 – 30 degrees of error (Grantham et al., 2007; Nopp et al., 2004, Litovsky et al., 2012). In this report we describe the sound source localization abilities of patients who have undergone hearing preservation CI surgery and who have two ears with LF acoustic hearing. At issue with these patients is the level of sound source localization performance that is allowed by access to the ITDs available in the bilateral areas of low-frequency acoustic hearing.
Individuals with relatively good LF hearing and precipitously sloping high-frequency (HF) hearing loss can benefit from a surgical technique for cochlear implantation that preserves the LF hearing in the implanted ear. Because these patients have LF acoustic hearing in the ear contralateral to the CI, a successful surgery provides these listeners with bilateral LF acoustic hearing, commonly in the range of 250–750 Hz, in addition to a CI in the implanted ear. Gifford et al. (2013) reported that hearing preservation patients are able to resolve ITDs although not as well as NH listeners. Six listeners with preserved hearing had ITD thresholds that ranged from 131 – 1271µsec compared to NH listeners with a range of 30–60 µsec for signals at 250Hz. Given these data, it is reasonable to suppose that some hearing preservation patients would be able to localize sound sources on the horizontal plane -- but with less accuracy than NH listeners.
A study by Dunn et al. (2010) suggests this is the case. Patients using a short electrode array of 10mm and bilateral hearing aids were tested on localization. Using ‘everyday’ sounds that varied in both temporal and spectral information, and testing with an 8 loudspeaker array over a 108 degree arc,Dunn et al. (2010) reported that hearing preservation listeners could localize with a root mean square (rms) error of about 25 degrees. Although no report was made of sound source localization by NH listeners in the same test environment, this level of performance for WB signals is poorer than the NH listeners in, for example,Yost et al. (2013) who showed a mean error of 6 degrees. Dunn et al. (2010) also reported that allowing the patients to use a unilateral CI, in addition to bilateral low-frequency acoustic hearing, did not degrade sound source localization accuracy.
The first aim of this project was to attempt to replicate the results of the Dunn et al. (2010) study. The second aim was to filter stimuli to better constrain the availability of ILD and ITD cues. The third aim was to extend our knowledge of sound source localization by hearing preservation patients by (i) testing patients with deeper electrode insertions than those used by the patients in Dunn et al. (2010), (ii) testing patients with and without symmetrical low-frequency acoustic hearing and (ii) determining whether hearing aids have a significant effect on sound source localization accuracy.
Methods
Subjects
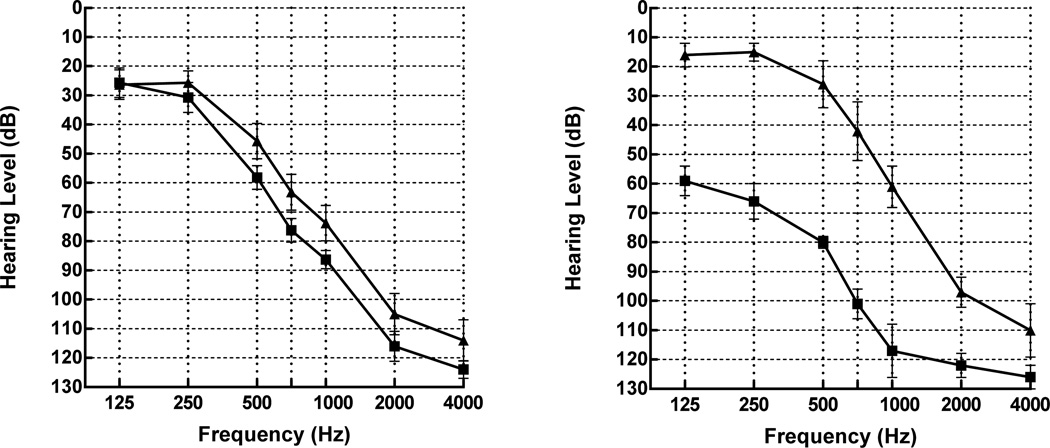
Twelve adult CI users with hearing preservation and a minimum of one year of CI use were tested following approval by the IRB at Arizona State University. All but two of the participants had been, or were enrolled in, the clinical trials for either the MED-EL EAS or the Cochlear Nucleus Hybrid device. Two of the MED-EL participants did not participate in the EAS clinical trial but had preserved hearing in the implanted ear. Eight subjects had symmetrical, low-frequency acoustic hearing, i.e., differences no greater than 15dB between ears at 250Hz (Figure 1, left). Of the MED-EL users with symmetrical acoustic hearing, four subjects were implanted with the MED-EL FLEXeas and one subject was implanted with the MED-EL Medium array (nominal insertion depth of 24 mm). One subject had bilateral CIs with bilaterally preserved hearing. For this study the second CI was not used; in other words, the implant part of the Duet processor was not worn. Three subjects were implanted with the Nucleus Hybrid-L24 (nominal insertion depth of 16 mm).
Figure 1.
Figure 1, left. Mean audiometric thresholds for the hearing preservation patients with symmetric, low frequency hearing, n = 8. Squares indicate thresholds for the implanted ear. Error bars indicate +/− 1 SEM. Figure 1, right. Mean audiometric thresholds for the patients with asymmetric, low frequency hearing, n = 4.
Four subjects lost a significant level of hearing resulting in asymmetrical low-frequency hearing with differences of 45 – 60dB at 250Hz between ears (Figure 1, right). Three of the subjects lost hearing following surgery and prior to activation. One subject lost hearing in the implanted ear seven years post-operatively due to an autoimmune disorder. (Previously, this subject had symmetrical LF hearing. Hearing in the contralateral ear was unaffected. This subject was tested approximately three months following the loss of hearing in the implanted ear.) Of the listeners with asymmetric LF hearing, one was implanted with the MED-EL FLEXeas array, one was implanted with the MED-EL Medium array, and two were implanted with the Nucleus Hybrid-L24. Audiometric thresholds are listed in Table 1. Typically, the poorest ear is chosen for this type of surgery, and as such, pre-implant audiometric thresholds would not be better than the unimplanted ear. Listeners used their preferred program on their own processors. Both the MED-EL Duet and Cochlear Nucleus Hybrid processors incorporate signal processing which directs signals to the hearing aid allowing combined acoustic and electric hearing in the same ear. Demographics for hearing preservation listeners are provided in Table 2.
Table 1.
Thresholds in dB by frequency (Hz) for each hearing preservation subject.
| Subject | 125Hz | .25kHz | .5kHz | .75Hz | 1kHz | 2kHz | 4kHz |
|---|---|---|---|---|---|---|---|
| 2 | 40/45 | 50/40 | 65/50 | 70/60 | 80/70 | 100/75 | NR/85 |
| 3 | 40/35 | 50/35 | 65/45 | 80/55 | 90/60 | NR/NR | NR/NR |
| 4 | 10/30 | 30/40 | 80/70 | 85/85 | 90/80 | 105/90 | NR/NR |
| 5 | 30/35 | 20/20 | 50/30 | 65/50 | 70/55 | 110/90 | 115/100 |
| 6 | 30/30 | 30/25 | 50/30 | 65/50 | 85/65 | 120/115 | 120/120 |
| 11 | 15/15 | 15/15 | 60/65 | 85/90 | 95/100 | NR/NR | NR/NR |
| 12 | 5/0 | 10/5 | 40/30 | 90/70 | 100/100 | NR/110 | NR/NR |
| 13 | 35/20 | 40/25 | 55/40 | 70/45 | 80/60 | 100/100 | 105/90 |
| 7* | 50/10 | 55/10 | 75/10 | 90/30 | 115/50 | 115/105 | 115/110 |
| 8* | 65/20 | 80/20 | 80/35 | 110/35 | NR/55 | NR/95 | NR/NR |
| 9* | 50/25 | 70/20 | 80/45 | 95/70 | 95/80 | 115/105 | NR/115 |
| 10* | 70/10 | 60/10 | 85/15 | 110/35 | NR/60 | NR/85 | NR/85 |
Thresholds are listed for the implanted/unimplanted ears. NR = no response at equipment limits >120dB.
An asterisk denotes listeners with asymmetric hearing.
Table 2.
Demographic information for hearing preservation users.
| Subj | Age | Gender | Age HL onset (in years) |
Processor/ HA |
Years of CI Use |
CI Ear/ Device |
Strategy | # Active Channels/ # Available Channels |
Frequency Allocation in Hz |
Etiology of Deafness |
|---|---|---|---|---|---|---|---|---|---|---|
| 2 | 68 | M | 27 | Tempo+Duet/Widex | 5 | L/MED-EL Pulsar EAS | CIS | 10/12 | 500–8500 | Unknown |
| 3 | 67 | M | 21 | Tempo+Duet/Phonak | 1 | R/ME Sonata EAS Flex | CIS | 10/12 | 500–8500 | Noise Exposure |
| 4 | 39 | F | 14 | Tempo+Duet/Tempo+Duet | 1 | R/ME Pulsar EAS Flex | CIS | 12/12 | 300–8500 | Unknown |
| 5 | 79 | M | 40 | Freedom/Phonak | 2 | R/CA Hybrid L24 | ACE | 18/24 | 1188–7938 | Hereditary |
| 6 | 55 | F | 40 | Freedom/Phonak | 2 | R/CA Hybrid L24 | ACE | 18/24 | 1188–7938 | Unknown |
| 7 | 70 | M | 42 | Freedom/Widex | 1.6 | L/CA Hybrid L24 | ACE | 18/24 | 1188–7938 | Hereditary |
| 8 | 64 | M | 20 | Opus 2 Duet/Danalogics | 6 | L/ME Pulsar Medium | FSP | 10/12 | 690–8500 | Hereditary |
| 9 | 69 | F | 47 | Opus 2/Phonak | 1 | R/ME Sonata Flex | FSP | 10/12 | 100–8000 | Hereditary |
| 10 | 47 | F | 32 | Freedom/Phonak | 3 | R/CA Hybrid L24 | ACE | 18/24 | 1188–7938 | Unknown |
| 11 | 35 | M | 5 | Opus 2/Unaided | 2 | L/ME Sonata Medium | FSP | 11/12 | 332–7500 | Unknown |
| 12 | 50 | F | 32 | Freedom/Phonak | 3 | R/CA Hybrid L24 | MP12 | 20/24 | 1188–7938 | Hereditary |
| 13 | 62 | F | 52 | Tempo+Duet/Phonak | 2 | L/ME Sonata EAS Flex | CIS | 12/12 | 500–8500 | Viral Infection |
ME = MED-EL. CC = Cochlear Corp.
Hearing aids
All hearing preservation subjects used their own behind-the-ear (BTE) hearing aid on the contralateral ear. Settings on the hearing aids (HA) and processors were not changed -- participants used their everyday settings. However, hearing aids were evaluated using real ear measurements to assess whether their settings met NAL-NL1 prescriptive targets (Dillon et al., 1998) in the low frequency region. For the symmetrical listeners, the prescriptive target was met for both hearing aids. These listeners all showed benefit from adding the acoustic hearing in the preserved ear to the CI when listening to speech in complex noise. For three of the participants with asymmetric hearing, the processor integrated HA was unable to meet target due to the degree of hearing loss, even with gain settings set to maximum. Although the hearing aid portion of the processor may not have met the prescriptive target, all subjects with asymmetric hearing reported that the addition of the hearing aid reduced listening effort. Critically, every subject with asymmetrical hearing showed improved performance on at least one measure of speech understanding in the ipsilateral hearing aid plus CI condition compared to the CI alone condition. This outcome indicates that the patients derived benefit from amplification in the implanted ear.
Test stimuli
Three, 200-msec, filtered (48 dB/octave) Gaussian noise stimuli of different spectral content were presented in random order. The stimuli were (i) low-pass (LP) noise filtered from 125–500Hz, (ii) high-pass (HP) noise filtered from 1500–6000 Hz and (iii) wideband (WB) noise filtered from 125–6000 Hz
Test environment
Testing was conducted in an 11’ × 15’ sound deadened room. The stimuli were presented from a 13 loudspeaker array with an arc of 180° in the frontal horizontal plane. There was 15° of separation between loud speakers. To reduce edge effects, stimuli were not presented from loud speakers 1 (far left) and 13 (far right). Listeners were not notified that these two loud speakers were ‘dummy’ loud speakers. Loud speakers were placed 1.67 meters from the listener’s head and were at the level of the listeners’ pinnae.
Test Conditions
Presentation of the stimuli was controlled by Matlab. Four blocks of 33 trials each were presented at 65dBA. Each stimulus (LP, HP, WB) was presented four times per loud speaker resulting in 132 presentations (11 speakers × 4 blocks × 3 stimuli). Overall level was roved ±2 dB to ensure that small differences between the output of the loud speakers was not a cue.
Prior to testing, a screening was carried out to ensure audibility for each set of stimuli in the unaided conditions. Adjustments were made to ensure comfortable audibility for each noise source. Listeners were evaluated in the following four conditions which were counter-balanced among subjects: (i) unaided, no CI, (ii) unaided plus CI, (iii) bilaterally aided, no CI, and (iv) bilaterally aided plus CI. None of the hearing preservation listeners were able to hear the HP stimuli without the CI due to the severity of their high frequency hearing loss. Therefore, the HP condition was eliminated for the unaided and aided conditions without the CI but was administered in the unaided and aided conditions using the CI.
A practice trial was provided to ensure (i) understanding of the test protocol and (ii) that the stimuli were audible. Subjects were instructed to look at a red dot on the center speaker (speaker #7) at midline until a stimulus was presented. Subjects were monitored via a webcam to ensure that they looked at the mid line prior to presentation of the stimuli. Each subject identified the speaker of the sound source by pushing a button on a numbered keypad corresponding to the number of the loud speaker. They were instructed to look at the red dot as soon as they pressed the enter button so that they would be looking at midline when the next stimulus was presented. During the practice trial stimuli were presented in consecutive order beginning with speaker #2 and stopping at speaker #12. Subjects were able to repeat the practice condition as many times as needed to feel comfortable with the test and using the keypad. Prior to the actual sound source localization test each subject was reinstructed that the sounds would be presented randomly from any speaker and not in order as in the practice test.
Results
RMS error in degrees was calculated after Rakerd and Hartman (1986) using the D statistic. Chance performance was calculated using a Monte Carlo method of 100 runs of 1000 Monte Carlo trials. Mean chance performance was 73.5° with a standard deviation of 3.2° for the three noise stimuli.
To provide a reference level of sound source localization accuracy, i.e., for normal hearing listeners, we have used data from Yost et al. (2013). The listeners in that study were tested in the same room and with the same stimuli as the patients in the present study.
Because hearing asymmetry is known to affect sound source localization (Moore 1996; Simon 2005), the hearing preservation group was divided into two groups for all statistical analyses -- patients with symmetrical, LF hearing at 250Hz and those with large asymmetries at 250Hz.
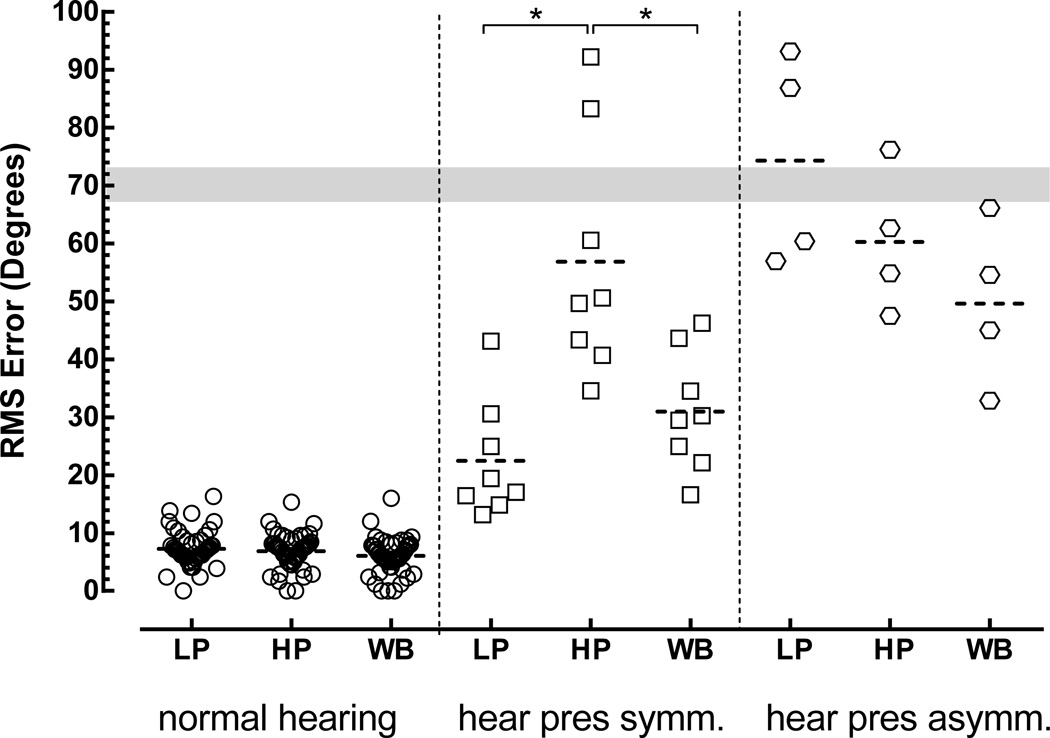
The results for the normal hearing listeners and the two groups of hearing preservation patients are shown in Figure 2 and in Table 3.
Figure 2.
Localization error as a function of spectral content for normal hearing listeners and for hearing preservation listeners with symmetric (symm) and asymmetric (asymm) low-frequency hearing in the combined condition (bilateral HA + CI). The gray bar represents +/− one standard deviation for chance performance. The dotted horizontal lines indicate mean scores. The vertical dotted lines are included to facilitate visual segregation of the data from the three listener groups. Key: * p<.01
Table 3.
Mean rms error and standard deviations for localization performance in response to WB, LP and HP stimuli for three groups of listeners in the combined condition (CI + bilateral hearing aids).
| Wideband | Low Pass | High Pass | |
|---|---|---|---|
| Normal hearing | 5.98 (2.72) | 6.95 (1.95) | 6.70 (2.61) |
| Hrg Pres: Symmetrical | 33.03 (8.38) | 23.32 (9.84) | 57.77 (20.52) |
| Hrg Pres: Asymmetrical | 49.83 (14.32) | 76.48 (20.64) | 60.31 (12.27) |
Patients with symmetrical hearing loss
For the eight patients in this group, the mean sound source localization accuracy in the combined condition (CI + bilateral hearing aids) for the LP, HP and WB stimuli were 23, 58 and 33 degrees of error, respectively. A repeated measures ANOVA revealed a main effect for conditions (F2,23=19.6, p.= .0006). Post tests (Holm-Sidak) indicated that (i) the scores in the LP condition differed from those in the HP condition, (ii) the scores in the HP condition differed from those in the WB condition and (iii) that the scores in the LP condition did not differ from those in the WB condition – although the mean scores suggest poorer performance in the WB condition. We return to this issue in the section on the effect of hearing aids on performance.
Patients with asymmetrical hearing loss
For the four patients in this group, the mean sound source localization accuracy for the LP, HP and WB stimuli in the combined condition was 76, 60 and 50 degrees of error, respectively. Both aided and unaided results for the low passed condition were at chance levels of performance for all four listeners. The small number of listeners precluded a useful statistical evaluation of the differences in mean scores. However, inspection of Figure 2 reveals that none of the patients in the asymmetrical hearing loss group performed as well as the patients in the symmetrical hearing loss group when the stimulus was a low-pass noise signal, i.e., the signal that maximized the availability of ITD cues.
Effect of hearing aids and CIs on sound source localization
This analysis compares the performance of patients who showed symmetrical low-frequency hearing loss (i) with and without amplification for their acoustic hearing and (ii) with and without the CI. The signals were the LP and WB noise signals. The results are shown in Table 4. Inspection of Table 4 indicates that, for the LP signal, neither amplification nor the use of a unilateral CI significantly altered sound source localization performance, i.e., all mean error scores were between 19 and 23 degrees.
Table 4.
RMS errors for LP and WB stimuli for hearing preservation listeners with symmetrical LF hearing in the unaided and aided conditions with and without the CI. Standard deviations are in parentheses.
| LP | WB | |
|---|---|---|
| Unaided without CI | 18.88 (6.0) | 21.36 (12.19) |
| Unaided with CI | 22.73 (12.08) | 23.01 (11.5) |
| Aided without CI | 20.33 (7.35) | 32.52 (8.2) |
| Aided with CI | 23.32 (9.8) | 33.03 (8.38) |
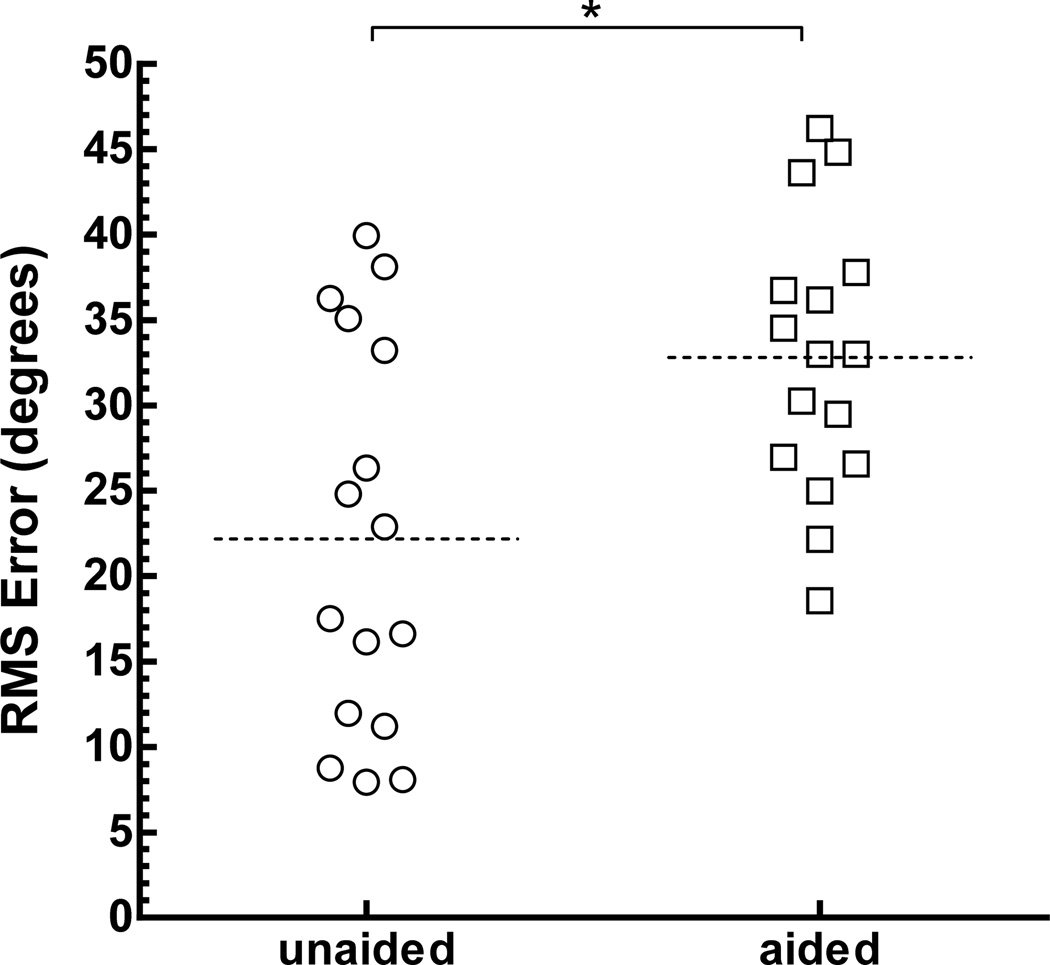
A similar inspection of Table 4 for the WB stimulus suggests a different outcome. For this stimulus, the presence of a unilateral CI did not alter the mean error scores, but amplification did. In Figure 3, the scores from the WB unaided condition, (without and with CI) and for the WB aided condition, (without and with CI) are plotted. Performance in the aided and unaided conditions differed significantly: Aided = 33 degrees of error, Unaided = 22 degrees of error (t15 = 3.562, p. = 0.0038).
Figure 3.
Localization error for hearing preservation patients with symmetrical LF hearing loss in the unaided and aided test conditions. Each patient in each group contributed two scores. The unaided condition consists of responses when tested with a unilateral CI and one without a unilateral CI. The bilaterally aided condition consists of listening with and without the CI for each listener. Key: p<.01
Discussion
The present study has replicated and extended the work of Dunn et al. (2010). These authors reported for patients with shallow (10 mm) electrode arrays that (i) the mean sound source localization error, to spectrally and temporally complex signals, was about 25 degrees and (ii) that the presence of a unilateral CI used in conjunction with bilateral LF acoustic hearing did not detrimentally alter sound source localization accuracy. We have obtained similar outcomes for patients with deeper electrode insertions (nominally 16–24 mm). We find a mean sound source localization error of 33 degrees for a wideband stimulus and no deleterious effect of a unilateral CI combined with bilateral LF acoustic hearing.
ITDs and sound source localization to the LP stimulus
In the work reported here, the LP stimulus served to reduce the possibility that ILD cues were used for sound source localization. That is, over the range 200–500 Hz, maximum ILDs are small -- from 3–6dB (e.g., Shaw, 1974). It is reasonable to suppose that the performance of the patients with symmetrical low-frequency hearing loss in the combined condition (bilateral HAs + one CI), e.g., 23 degrees of error, reflects use of ITD cues. The poorer-than-normal performance is consistent with the Gifford et al. (2013) report of ITD thresholds for this group that were significantly higher (i.e., poorer) than normal.
LF symmetry and sound source localization ability
Our research extends the work of Dunn et al. (2010) by documenting that large asymmetries in LF hearing between ears has a detrimental effect on sound source localization accuracy. Listeners with asymmetrical LF hearing showed sound source localization to the LP stimulus in the combined condition that was near the level of chance performance and the mean level in response to the WB stimulus was 50 degrees of error. One practical consequence of these outcomes is that, before surgery, patients should be told that they will localize reasonably well, following surgery, only if there is minimal additional hearing loss in the operated ear. More work is necessary to quantify the degree of symmetry that is necessary for the level of sound source localization accuracy shown in this study.
Hearing aids impair sound source localization performance for WB stimuli but not LP stimuli
We have found that sound source localization errors in response to the WB stimulus were larger by about 10 degrees in conditions where amplification was provided for acoustic hearing than in conditions in which amplification was not provided. In contrast, errors in response to LP stimuli were not affected by the presence of amplification.
Our data do not speak to the mechanisms underlying the poorer performance using the WB stimulus in the amplified test conditions (see and contrast localization results by Boymans et al. 2008; Kobler and Rosenhall, 2002 and Van den Bogaert et al., 2006 for patients with and without conventional hearing aids). However, given the steeply sloping hearing losses and poor thresholds above 500 Hz, it is likely that dead regions were present (Zhang et al., 2014) and amplification into dead regions could distort relevant information for localization (e.g., Moore, 2004). Finally, we note that outside of the laboratory, the patients were accustomed to listening to WB stimuli with amplification and with a single CI. This, however, was not the condition that allowed the best sound source localization performance. Because sound source localization was best in test conditions that were relatively ‘unpracticed’, i.e., those without amplification, we suspect that amplification was indeed detrimental to sound source localization ability.
All of our subjects used different hearing aids on each ear – that is, they used a hearing aid coupled to the processor on their CI ear and used a conventional BTE on their contralateral ear. More research needs to be conducted to determine whether other schemes for amplification would produce different results.
Summary
Hearing preservation patients with symmetrical LF acoustic hearing coupled with a single CI are able to locate sound sources on the horizontal plane, in the most favorable test conditions, with approximately 20 degrees of error. Test performance, in response to LP stimuli, suggests that the patients were using ITD cues for sound source localization. The presence of a unilateral CI combined with bilateral, LF acoustic hearing does not impair sound source localization accuracy, but amplification for acoustic hearing can be detrimental to sound source localization accuracy. Finally, patients with asymmetrical LF hearing loss show much poorer results than patients with symmetrical LF hearing.
Acknowledgements
Author LL was supported by NIDCD F31DC011684 and MED-EL Corporation; MFD by NIH R01 DC 010821; RG by NIH R01 DC009404; WY by AFOSR FA9550-12-1-0312.
References
- Blauert J. Spatial hearing: the psychophysics of human sound localization. MIT press; 1997. [Google Scholar]
- Boymans M, Goverts S. Theo, Kramer Sophia E, Festen Joost M, Dreschler Wouter A. A Prospective Multi-Centre Study of the Benefits of Bilateral Hearing Aids. Ear Hear. 2008;29(6):930–941. doi: 10.1097/aud.0b013e31818713a8. [DOI] [PubMed] [Google Scholar]
- Dillon H, Katsch R, Byrne D, Ching T, Keidser G, Brewer S. National Acoustics Laboratories Research and Development, Annual Report, 1997/98. Sydney, Australia: National Acoustics Laboratories; 1998. The NAL-NL1 prescription procedure for non-linear hearing aids; pp. 4–7. [Google Scholar]
- Dunn C, Perreau A, Gantz B, Tyler R. Benefits of localization and speech perception with multiple noise sources in listeners with a short-electrode cochlear implant. J Am Acad Audiol. 2010;21:44–51. doi: 10.3766/jaaa.21.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gifford RH, Dorman MF, Skarzynski H, Lorens A, Polak M, Driscoll C, Roland P, Buchman CA. Evaluating the benefit of hearing preservation with cochlear implantation: speech recognition in complex listening environments. Ear Hear. 2013:413–424. doi: 10.1097/AUD.0b013e31827e8163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grantham W, Ashmead D, Ricketts T, Labadie R, Haynes D. Horizontal-plane localization of noise and speech signals by postlingually deafened adults fitted with bilateral cochlear implants. Ear Hear. 2007;28(4):524–541. doi: 10.1097/AUD.0b013e31806dc21a. [DOI] [PubMed] [Google Scholar]
- Grantham W, Ashmead D, Ricketts T, Haynes D, Labadie R. Interaural time and level difference thresholds for acoustically presented signals in post-lingually deafened adults fitted with bilateral cochlear implants using CIS processing. Ear Hear. 2008;29(1):33–44. doi: 10.1097/AUD.0b013e31815d636f. [DOI] [PubMed] [Google Scholar]
- Kobler S, Rosenhall U. Horizontal localization and speech intelligibility with bilateral and unilateral hearing aid amplification. Intn J of Aud. 2002;41:395–400. doi: 10.3109/14992020209090416. [DOI] [PubMed] [Google Scholar]
- Moore Brian CJ. Perceptual Consequences of Cochlear Hearing Loss listeners and their Implications for the Design of Hearing Aids. Ear Hear. 1996;17(2):133–161. doi: 10.1097/00003446-199604000-00007. [DOI] [PubMed] [Google Scholar]
- Moore BCJ. Dead regions in the cochlea: conceptual foundations, diagnosis and clinical applications. Ear Hear. 2004;25:98–116. doi: 10.1097/01.aud.0000120359.49711.d7. [DOI] [PubMed] [Google Scholar]
- Nopp P, Schleich P, D’Haese P. Sound Localization in Bilateral Users of MED-EL COMBI 40/40+ Cochlear Implants. Ear Hear. 2004;25(3):205–214. doi: 10.1097/01.aud.0000130793.20444.50. [DOI] [PubMed] [Google Scholar]
- Rakerd B, Hartmann WM. Localization of sound in rooms, III: Onset and duration effects. J Acoust Soc Am. 1986;80(6):1695–1706. doi: 10.1121/1.394282. [DOI] [PubMed] [Google Scholar]
- Shaw EAG. Transformation of sound pressure level from the free field to the eardrum in the horizontal plane. J Acoust Soc Am. 1974;56(6):1848–1861. doi: 10.1121/1.1903522. [DOI] [PubMed] [Google Scholar]
- Simon H. Bilateral amplification and sound localization: Then and now. JRRD. 2005;42(4) Supplement 2:117–132. doi: 10.1682/jrrd.2005.01.0021. [DOI] [PubMed] [Google Scholar]
- Van den Bogaert T, Klasen T, Moonen M, van Deun L, Wouters J. Horizontal localization with bilateral hearing aids: Without is better than with. J Acoust Soc Am. 2006;119(1):515–526. doi: 10.1121/1.2139653. [DOI] [PubMed] [Google Scholar]
- Yost WA, Loiselle L, Dorman M, Burns J, Brown CA. Sound Source localization of Filtered Noises by Listeners with Normal Hearing: A Statistical Analysis. J Acoust Soc Am. 2013;133(5):2876–2882. doi: 10.1121/1.4799803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang T, Dorman M, Gifford R, Moore B. Cochlear dead regions constrain. the benefit of combining acoustic stimulation with electric stimulation. Ear Hear. 2014;35(4):410–117. doi: 10.1097/AUD.0000000000000032. [DOI] [PMC free article] [PubMed] [Google Scholar]