Because of the epidemic nature of this disease and its distinctive clinical features in this area, surveillance should continue.
Keywords: Streptococcus pneumoniae, serotype 1, South Africa, pneumococcal conjugate vaccine, PCV13, epidemiology, surveillance, invasive, vaccination, incidence, pneumonia, bacteremia, immunization, streptococci
Abstract
In South Africa, 7-valent pneumococcal conjugate vaccine (PCV) was introduced in April 2009 and replaced with 13-valent PCV in April 2011. We describe the epidemiology of serotype 1 Streptococcus pneumoniae disease during the pre- and post-PCV eras (2003–2013). Using laboratory-based invasive pneumococcal disease (IPD) surveillance, we calculated annual incidences, identified IPD clusters, and determined serotype 1–associated factors. Of 46,483 IPD cases, 4,544 (10%) were caused by serotype 1. Two clusters of serotype 1 infection were detected during 2003–2004 and 2008–2012, but incidence decreased after 2011. Among children <5 years of age, those who had non–serotype 1 IPD had shorter hospital stays, fewer cases of penicillin-nonsusceptible disease, and lower HIV prevalence and in-hospital death rates than did those with serotype 1 IPD; similar factors were noted for older patients. Serotype 1 IPD had distinctive clinical features in South Africa, and annual incidences fluctuated, with decreases noted after the introduction of PCV13.
Streptococcus pneumoniae serotype 1 is highly invasive and rarely carried asymptomatically (1). The incidence of serotype 1 invasive pneumococcal disease (IPD) fluctuates year to year; disease is associated with outbreaks in closed communities and hospitals and, in Africa, with communitywide meningitis outbreaks (2). Compared with other S. pneumoniae serotypes, serotype 1 tends to cause fewer cases of fatal disease, and antibiotic-resistant cases are unusual (1).
IPD is common in children with underlying diseases, especially HIV. A study conducted among children <18 years of age in Israel before introduction of 7-valent pneumococcal conjugate vaccine (PCV7) showed that, compared with other common serotypes, serotype 1 caused more bacteremic pneumonia and peritonitis, occurred in older children and certain ethnic groups, and affected otherwise healthy children (3). After PCV7 introduction, infections caused by serotypes included in the vaccine declined, but other pneumococcal serotypes (e.g., serotype 1, which was later included in 13-valent vaccine [PCV13]) became relatively more common (4–6); serotype 1 ranked among the top 4 serotypes infecting children <5 years of age (7). Although PCV7 use may have contributed to the relative increase in serotype 1 infections, some studies showed no correlation between the vaccine and serotype 1 disease incidence (8). Lack of correlation is likely due to the epidemic-prone nature of serotype 1 disease and annual fluctuations in disease incidence (9). In addition, replacement disease is mainly due to common colonizing serotypes. An indirect cohort analysis using data from the United Kingdom Health Protection Agency (now Public Health England) surveillance program could not demonstrate significant protection against serotype 1 IPD by PCV13, although the point estimate suggested protection (vaccine effectiveness 62% [95% CI −112% to 92%]) (10). Two trials of a 9-valent vaccine showed waning protection against serotype 1 in the absence of a booster vaccine dose in the second year of life; vaccine failures clustered in children >18 months of age (11,12).
In South Africa, PCV7 was introduced into the national immunization schedule in April 2009 as a 3-dose regimen for infants 6 weeks, 14 weeks, and 9 months of age; in April 2011, the vaccine was replaced with PCV13. Among children <1 year of age, reported coverage for the third dose of PCV improved from 10% in 2009 to 81% in 2012 but declined to 62% in 2013 (13). In 2012, after PCV13 introduction, serotype 1 IPD incidence showed a temporally associated decline in children <2 years of age (−57%, 95% CI −79% to −16%) and adults 25–44 years of age (−33%, 95% CI −46% to −17%) compared with incidence in 2005–2008 (14).
Information regarding S. pneumoniae serotype 1 epidemiology in Africa is limited. We compared serotype 1 disease epidemiology in South Africa with that of other serotypes over an 11-year period, before and after introduction of PCV7 and PCV13. We also explored whether temporal or spatial clusters of serotype 1 disease occurred during the study period.
Methods
Study Design and Setting
Persons of any age were included in the study if they were hospitalized in South Africa during 2003–2013 for laboratory-confirmed IPD and had an available S. pneumoniae serotype result for an isolate from a normally sterile site. Patients were identified through an active national, laboratory-based surveillance program for S. pneumoniae. Data were contributed by >200 hospital-based diagnostic laboratories that submitted pneumococcal isolates to the National Institute for Communicable Diseases, Johannesburg, South Africa. Most laboratories were nonenhanced sites where only isolates and accompanying laboratory report forms with patient age, sex, date and source of the specimen were submitted. However, 24 sites (primarily tertiary hospitals) implemented enhanced surveillance, in which dedicated surveillance officers collected additional clinical information on identified patients; at least 1 site was located in each South Africa province, giving national representation (14). Enhanced sites were chosen on the basis of convenience, interest from site investigators, and number of isolates submitted each year; thus, some differences existed between enhanced and nonenhanced sites (Technical Appendix). Annual audits conducted by using a laboratory-based information system were used to identify unreported cases, which were included and used in incidence calculations.
Participants identified from enhanced and nonenhanced sites were included for determining incidence rates and cluster mapping. For the analyses of factors associated with serotype 1 pneumococcal disease and fatality, only participants from enhanced sites with detailed clinical information and known in-hospital outcomes were included.
Approval was obtained from the Human Research Ethics Committee (Medical), University of the Witwatersrand, Johannesburg (M081117), and other hospital or provincial ethics committees, as required. Informed consent was obtained for all patients.
Definitions
IPD cases were defined as disease in persons with S. pneumoniae detected in cultures of specimens from normally sterile sites or persons with culture-negative samples that were positive by latex agglutination and/or Gram stain microscopy or lytA PCR (15). Pneumococci were serotyped by the Quellung method (Statens Serum Institut, Copenhagen, Denmark).
Serotype 1 clusters were defined as an increase in serotype 1 IPD numbers relative to other serotype numbers in a specific geographic area and time. Cluster location was based on hospital district where cases were diagnosed; actual geographic location was considered to be the centroid of the district polygon. Other definitions are provided in the online Technical Appendix.
Incidence Estimations
We calculated annual incidence of serotype 1 disease per 100,000 population during 2003–2013 by using data for participants in defined age groups. We divided the number of age-specific, culture-positive serotype 1 IPD cases reported each year by age-specific midyear population estimates. Incidences for non–serotype 1 disease were similarly calculated. Serotype data for cases without serotype results from culture (including cases with only PCR serotype results) were imputed by age and year to obtain final incidence rates. Missing data were assumed to be random among different serotypes. Midyear population denominators were obtained from Statistics South Africa (http://www.statssa.gov.za/). To show differences in serotype incidences between prevaccine and postvaccine years, we compared an average incidence from prevaccine years (2003–2008) to 1 postvaccine year (2013). As a baseline for comparison, we included the average for years without clusters (2005–2007). CIs were calculated by using Poisson distribution for incidence rates.
Factors Associated with Serotype 1 IPD and Case-Fatality Rates
For the analyses of factors associated with serotype 1 IPD, we included only participants with culture- and PCR-positive results from enhanced sites during 2003–2013. Patients were stratified into 2 age groups (<5 and >5 years), and disease-associated factors in those with serotype 1 IPD were compared with those in patients with non–serotype 1 IPD by using a multivariable logistic regression model. A second model to assess in-hospital fatalities restricted the analysis to serotype 1 IPD cases.
For both models, we assessed all variables considered significant (p<0.2) on univariate analysis and removed nonsignificant factors (p>0.05) by manual backward elimination. Patients with missing data for included variables were excluded. Statistical analysis was implemented by using Stata version 13.1 (StataCorp LP, College Station, TX, USA).
Spatiotemporal Analysis for Detection of Serotype 1 IPD Clusters
We conducted a space–time scan analysis to detect serotype 1 clusters by aggregating IPD cases with available serotype results from January 2003–December 2013 by month and district. To minimize potential biases introduced by temporal and geographic differences in specimen-collecting practices, healthcare-seeking behavior, or surveillance system improvements over time, we compared cases (serotype 1 IPD cases) with controls (non–serotype 1 IPD cases) from the same geographic area and time period; a Bernoulli model (16,17) was used for the comparison.
To account for control number reductions after PCV7 introduction, we adjusted (increased) observed control numbers by the percent reduction from the prevaccine period (14). To obtain estimated monthly numbers of controls, assuming no PCV introduction, we linearly interpolated estimated annual proportional reductions from June to June of consecutive years from 2009 through 2013. Because the percentage of reduction in the control numbers may have differed by geographic area due to locality differences in PCV7 uptake over time, we obtained monthly adjustment factors for each province. This adjustment would decrease the likelihood of detecting a cluster if, in fact, a cluster did not occur (null hypothesis).
To identify spatial clusters, we used an elliptical area of search that was allowed to vary in size, shape, and direction. Significance was assessed at p<0.05 over 999 replications. Space-time analysis was conducted by using SaTScan version 9.3.1 (http://www.satscan.org/); maps were generated by using ArcGIS version 9.2 (http://www.esri.com/). To calculate relative risks for districts, we divided observed number of cases by expected number of cases in each district.
Results
During 2003–2013, a total of 46,483 persons with IPD were enrolled in the study; 32,841 (71%) had viable isolates and known S. pneumoniae serotype, and 1,204 (3%) had serotype determination by PCR. Of the 46,483 persons, 20,564 (44%) were enrolled from enhanced sites; of these 6,211 (30%) were <5 years of age, 14,004 (68%) were >5 years of age, and 349 (2%) had unknown age (Figure 1). Of the 4,985 patients who died, 68% (3,365) did so within 3 days of admission. Of the 12,013 patients who recovered, 14% (1,673) were hospitalized for <3 days, 62% (7,427) for 4–14 days, and 24% (2,913) for >2 weeks. In the pre-PCV7 period (2003–2008), serotype 1 was the sixth most common S. pneumoniae serotype among children <5 years of age, but by 2013, it was eleventh. In contrast, among persons >5 years of age, serotype 1 was the most common serotype across all years, although case numbers decreased after PCV13 introduction.
Figure 1.
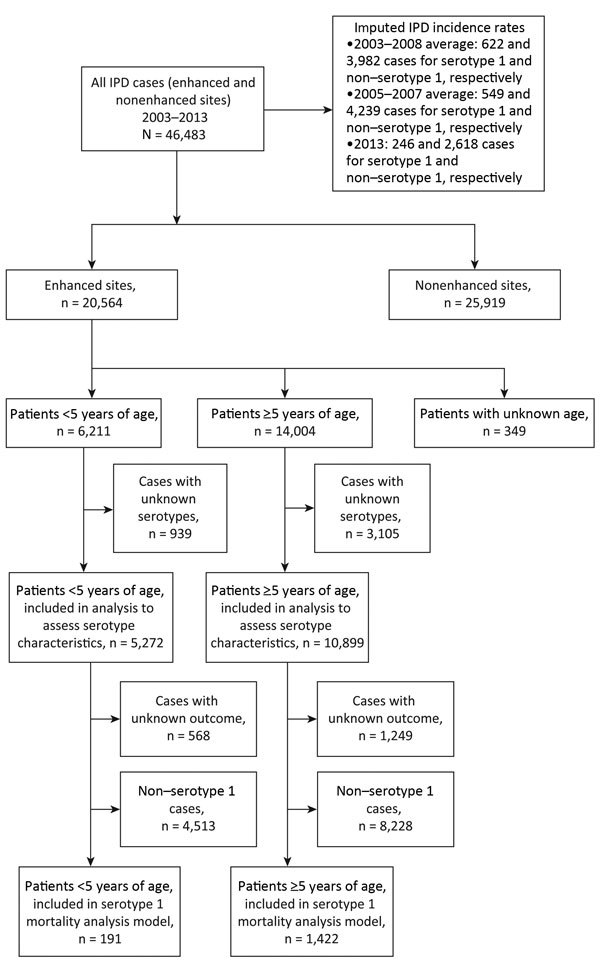
Selection flowchart for study of invasive Streptococcus pneumoniae disease (IPD) cases in South Africa, 2003–2013. Cases were reported by Group for Enteric Respiratory and Meningeal Disease Surveillance sites (GERMS-SA). Years indicate prevaccine (2003–2008), baseline (2005–2007), and postvaccine (2013) periods. Nonenhanced sites only submitted isolates and accompanying laboratory report forms, which included patient age and sex and the date and source of the specimen; enhanced sites (primarily tertiary hospitals) implemented enhanced surveillance, in which dedicated surveillance officers collected additional clinical information on identified patients.
Comparison of Enhanced and Nonenhanced Sites
Characteristics of enhanced and nonenhanced sites differed (Technical Appendix Table 1). Compared with nonenhanced sites, enhanced sites had a higher proportion of cases among younger children, more cases from certain provinces, fewer cases in 2012–2013, more penicillin-nonsusceptible cases, more blood culture results, and fewer serotype 1 IPD cases.
Incidence of Serotype-Specific IPD in Different Age Groups
During the prevaccine era (2003–2008), serotype 1 incidence per 100,000 population was highest among persons <1 (1.8 cases), 5–9 (1.6 cases), and 25–44 (1.8 cases) years of age (Figure 2, panel A). Serotype 1 incidence did not differ significantly for 2003–2008 compared with 2005–2007, when there were no clusters. In 2013, serotype 1 incidence was highest among persons 5–9 (0.7 cases) and 25–44 (0.6 cases) years of age; reductions were significant (p<0.001) in all age groups except the >64-year-old age group (p = 0.07).
Figure 2.
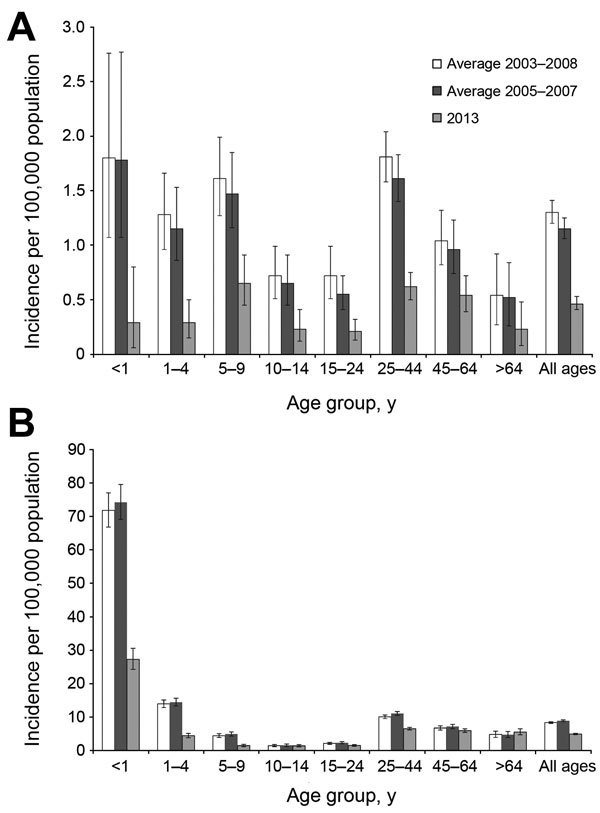
Incidence of serotype 1 and non–serotype 1 invasive pneumococcal disease (IPD) by age group, South Africa, 2003–2013. Years indicate prevaccine (2003–2008), baseline without clusters (2005–2007), and postvaccine (2013) periods. A) Serotype 1 IPD incidence by age group during prevaccine (no. cases = 622), baseline (no. cases = 549), and postvaccine (no. cases = 246) years. B) Non–serotype 1 IPD incidence by age group during prevaccine (no. cases = 3,982), baseline (no. cases = 4,239), and postvaccine years (no. cases = 2,618). Error bars indicate 95% CIs.
For all other serotypes during 2003–2008, the highest incidence rates per 100,000 population were among persons <1 (71.8 cases), 1–4 (13.9 cases), and 25–44 (10.1 cases) years of age (Figure 2, panel B). In 2013, the highest incidence rates were among persons <1 (27.3 cases) and >25 (>5.0 cases) years of age. Reductions in incidence among persons <5 and 25–44 years of age were significant (p<0.001).
The incidence of serotype 1 IPD fluctuated over the 11-year period (Technical Appendix Figure 1). For the <5-year-old age group, incidence rates were significantly reduced in 2006 (p = 0.01), 2007 (p = 0.03), 2010 (p = 0.006), and 2012–2013 (p<0.001) compared with rates in 2005. In the >5-year-old age group, incidence rates were significantly higher in 2003 (p = 0.001) and 2004 (p = 0.002) compared with 2005 but lower during 2006–2008 and 2010–2013 (p<0.001).
Factors Associated with Serotype 1 IPD
After adjustment for geographic location (province), year (based on prominent serotype 1 fluctuations), and clinical syndrome, we saw a difference among patients at enhanced sites who had IPD caused by serotype 1 versus other serotypes. Multivariable analysis showed a difference in disease distribution by province, year, and age among children <5 years of age; these difference were more apparent in children >3 than <1 years of age. Compared with children with non–serotype 1 IPD, those with serotype 1 disease had significantly shorter hospitalizations (<3 days vs. 4–14 days [odds ratio (OR) 0.58, 95% CI 0.33–1.02] or >15 days [OR 0.44, 95% CI 0.23–0.85]) and were less likely to have HIV disease (OR 0.19, 95% CI 0.12–0.31), to die while hospitalized (OR 0.38, 95% CI 0.19–0.76), or to have penicillin-nonsusceptible disease (OR 0.02, 95 CI 0.01–0.05) (Table 1).
Table 1. Characteristics of 5,272 patients <5 years of age with invasive pneumococcal disease caused by serotype 1 or non–serotype 1 Streptococcus pneumoniae, South Africa, 2003–2013*.
| Variable | No. cases/no. total (%) |
Univariate analysis† |
Multivariable analysis† |
|||||
|---|---|---|---|---|---|---|---|---|
| Serotype 1 | Non–serotype 1 | OR (95% CI) | p value | aOR (95% CI) | p value | |||
| Age, y | ||||||||
| <1 | 63/211 (30) | 2,754/5,061 (54) | Reference | <0.001 | Reference | <0.001 | ||
| 1 | 35/211 (17) | 1,155/5,061 (23) | 1.32 (0.87–2.01) | 2.36 (1.31–4.26) | ||||
| 2 | 43/211 (20) | 519/5,061 (10) | 3.62 (2.43–5.40) | 6.91 (3.78–12.64) | ||||
| 3 | 37/211 (18) | 355/5,061 (7) | 4.56 (2.99–6.94) | 12.03 (6.12–23.64) | ||||
| 4 |
33/211 (16) |
278/5,061 (5) |
|
5.19 (3.35–8.05) |
|
|
7.13 (3.60–14.13) |
|
| Province | ||||||||
| Gauteng | 95/211 (45) | 2,067/5,061 (41) | Reference | <0.001 | Reference | <0.001 | ||
| Western Cape | 11/211 (5) | 1,158/5,061 (23) | 0.21 (0.11–0.39) | 0.11 (0.04–0.26) | ||||
| KwaZulu-Natal | 46/211 (22) | 957/5,061 (19) | 1.05 (0.73–1.50) | 1.04 (0.59–1.84) | ||||
| Eastern Cape | 15/211 (7) | 152/5,061 (3) | 2.15 (1.22–3.79) | 1.98 (0.74–5.28) | ||||
| Free State | 25/211 (12) | 383/5,061 (8) | 1.42 (0.90–2.24) | 1.06 (0.56–2.00) | ||||
| Mpumalanga | 4/211 (2) | 104/5,061 (2) | 0.84 (0.30–2.32) | 0.58 (0.07–4.86) | ||||
| North-West | 5/211 (2) | 46/5,061 (1) | 2.36 (0.92–6.09) | 5.65 (1.33–24.05) | ||||
| Limpopo | 4/211 (2) | 48/5,061 (1) | 1.81 (0.64–5.13) | 1.79 (0.41–7.90) | ||||
| Northern Cape |
6/211 (3) |
146/5,061 (3) |
|
0.89 (0.39–2.08) |
|
|
0.50 (0.15–1.64) |
|
| Year of specimen collection | ||||||||
| 2003 | 31/211 (15) | 544/5,061 (11) | 1.20 (0.72–1.99) | 0.004 | 1.10 (0.49–2.49) | 0.05 | ||
| 2004 | 26/211 (12) | 699/5,061 (14) | 0.78 (0.46–1.32) | 0.58 (0.25–1.34) | ||||
| 2005 | 32/211 (15) | 672/5,061 (13) | Reference | Reference | ||||
| 2006 | 21/211 (10) | 551/5,061 (11) | 0.80 (0.46–1.40) | 0.77 (0.34–1.72) | ||||
| 2007 | 15/211 (7) | 547/5,061 (11) | 0.58 (0.31–1.07) | 0.67 (0.26–1.75) | ||||
| 2008 | 10/211 (5) | 542/5,061 (11) | 0.39 (0.19–0.80) | 0.40 (0.15–1.03) | ||||
| 2009 | 23/211 (11) | 494/5,061 (10) | 0.98 (0.57–1.69) | 1.43 (0.63–3.24) | ||||
| 2010 | 19/211 (9) | 361/5,061 (7) | 1.11 (0.62–1.98) | 0.82 (0.33–2.08) | ||||
| 2011 | 19/211 (9) | 240/5,061 (5) | 1.66 (0.92–2.99) | 1.04 (0.44–2.44) | ||||
| 2012 | 12/211 (6) | 190/5,061 (4) | 1.33 (0.67–2.63) | 0.49 (0.18–1.33) | ||||
| 2013 |
3/211 (1) |
221/5,061 (4) |
|
0.29 (0.09–0.94) |
|
|
0.12 (0.02–0.59) |
|
| Medical conditions/treatment | ||||||||
| Length of hospital stay, d | ||||||||
| <3 | 57/186 (31) | 1,238/4,489 (28) | Reference | 0.09 | Reference | 0.04 | ||
| 4–14 | 96/186 (52) | 2,138/4,489 (48) | 0.98 (0.70–1.36) | 0.58 (0.33–1.02) | ||||
| >15 | 33/186 (18) | 1,113/4,489 (25) | 0.64 (0.42–1.00) | 0.44 (0.23–0.85) | ||||
| Previously hospitalized | 39/164 (24) | 1,676/4,110 (41) | 0.45 (0.31–0.65) | <0.001 | ||||
| Underlying medical condition‡ | 27/114 (24) | 1,321/3,371 (39) | 0.48 (0.31–0.75) | 0.001 | ||||
| Antimicrobial drug use in previous 2 mo§ | 10/147 (7) | 742/3,549 (21) | 0.28 (0.14–0.53) | <0.001 | ||||
| HIV infected | 43/132 (33) | 2,125/3,539 (60) | 0.32 (0.22–0.47) | <0.001 | 0.19 (0.12–0.31) | <0.001 | ||
| TB treatment in previous 3 mo | 11/161 (7) | 570/3,928 (15) | 0.43 (0.23–0.80) | 0.008 | ||||
| Malnourished¶ | 24/95 (25) | 1,109/2,619 (42) | 0.46 (0.29–0.74) | 0.001 | ||||
| Died during hospitalization |
24/191 (13) |
1,105/4,513 (24) |
|
0.44 (0.29–0.68) |
<0.001 |
|
0.38 (0.19–0.76) |
0.006 |
| Pneumococcal isolate characteristics | ||||||||
| Penicillin nonsusceptible# | 4/203 (2) | 2,580/4,950 (52) | 0.02 (0.01–0.05) | <0.001 | 0.02 (0.01–0.05) | <0.001 | ||
| Previous invasive pneumococcal disease** |
2/211 (1) |
356/5,061 (7) |
|
0.13 (0.03–0.51) |
0.004 |
|
|
|
| Clinical syndrome†† | ||||||||
| Meningitis | 59/198 (30) | 1,668/4,736 (35) | Reference | 0.001 | ||||
| Pneumonia | 124/198 (63) | 2,358/4,736 (50) | 1.49 (1.08–2.04) | |||||
| Bacteremia | 15/198 (8) | 710/4,736 (15) | 0.60 (0.34–1.06) | |||||
*All patients were reported from the enhanced Group for Enteric, Respiratory, and Meningeal Disease Surveillance in South Africa (GERMS-SA) surveillance sites. aOR, adjusted odds ratio; OR, odds ratio; TB, tuberculosis. †Only variables significant on univariate and multivariable analysis are shown. Variables not included are sex, race, Pitt bacteremia score, prematurity, antimicrobial drug use in previous 24 h, viable culture, and specimen type. ‡Includes asplenia or sickle cell anemia; chronic illness (i.e., chronic lung, renal, liver, cardiac disease, and diabetes); other immunocompromising conditions (i.e. including organ transplant, primary immunodeficiency, immunotherapy, and malignancy, but excluding HIV); and other risk factors (i.e., head injury with possible cerebral spinal fluid leak, neurologic disorders, burns, and chromosomal abnormalities). Excludes malnutrition. §Use of any antimicrobial drug in 2 mo prior to admission. ¶Malnutrition was classified as a weight-for-age z-score of less than −2 (World Health Organization child growth standards 2009) (18), nutritional edema, or both. #Considered penicillin nonsusceptible at MIC >0.12 μg/mL; intermediately resistant and resistant groups were combined into a nonsusceptible group. **Invasive pneumococcal disease diagnosis >21 d before this episode. ††Clinical diagnoses were made on the basis of documented discharge diagnoses in patient medical records; clinical syndrome were separated into 3 groups: meningitis, bacteremic pneumonia, and bacteremia without focus or other diagnosis (e.g., septic arthritis, endopthalmitis, peritonitis, pericarditis).
Among persons >5 years of age, serotype 1 IPD (compared with non–serotype 1 IPD) was significantly associated with province, year, and patient age: compared with persons >64 years of age, ORs (95% CIs) were 13.48 (5.53–32.82) for children 5–9 years of age; 8.02 (3.15–20.43) for children 10–14 years of age; 5.65 (2.31–13.82) for persons 15–24 years of age; 3.67 (1.53–8.76) for persons 25–44 years of age; and 2.57 (1.06–6.23) for persons 45–64 years of age (Technical Appendix Table 2). Compared with persons with non–serotype 1 IPD, those with serotype 1 disease had significantly shorter hospitalization (<3 days vs. 4–14 days [OR 0.86, 95% CI 0.68–1.09] and vs. >15 days [OR 0.64, 95% CI 0.48–0.86]) and lower rates of previous admissions (OR 0.45, 95% CI 0.35–0.57) and tuberculosis treatment (OR 0.73, 95% CI 0.57–0.95).
Persons >5 years of age with serotype 1 disease were also significantly less likely to have HIV (OR 0.39, 95% CI 0.31–0.49) or penicillin-nonsusceptible disease (OR 0.02, 95% CI 0.01–0.04), and they were more likely than those with non–serotype 1 IPD to receive a diagnosis of pneumonia (OR 1.28, 95% CI 1.03–1.58) or bacteremia (OR 1.76, 95% CI 1.22–2.55) rather than meningitis. In-hospital death compared with recovery was not significant in the >5 year age group.
Factors Associated with In-Hospital Deaths among Patients with Serotype 1 IPD
We conducted multivariable analysis to explore factors associated with death in children <5 years of age with serotype 1 IPD (Table 2). Compared with 4-year-old children, those <1 year of age were more likely to die (OR 12.06, 95% CI 1.45–100.26), as were children with underlying medical conditions than those without. Odds of death were also increased among children with HIV (OR 2.82, 95% CI 1.36–5.84) or meningitis versus those with pneumonia or bacteremia. Duration of hospitalization was shorter among persons who died compared with those who recovered (<3 days vs. 4–14 days [OR 0.06, 95% CI 0.03–0.15] or >15 days [OR 0.02, 95% CI 0.01–0.07]).
Table 2. Factors associated with death in patients <5 years of age with serotype 1 invasive pneumococcal disease, South Africa, 2003–2013*.
| Variable | Univariate analysis |
Multivariable analysis |
||||
|---|---|---|---|---|---|---|
| No. deaths/no. cases (%) | OR (95% CI) | p value | aOR (95% CI) | p value | ||
| Age group, y | ||||||
| <1 | 102/355 (29) | 11.49 (2.75–47.95) | <0.001 | 12.06 (1.45–100.26) | 0.02 | |
| 1 | 22/154 (14) | 4.75 (1.08–20.88) | 3.83 (0.41–35.35) | |||
| 2 | 11/94 (12) | 3.78 (0.81–17.69) | 1.30 (0.12–14.34) | |||
| 3 | 6/73 (8) | 2.55 (0.49–13.14) | 1.40 (0.12–15.82) | |||
| 4 |
2/59 (3) |
Reference |
|
|
Reference |
|
| Province | ||||||
| Gauteng | 53/327 (16) | Reference | 0.001 | |||
| Western Cape | 15/111 (14) | 0.81 (0.44–1.50) | ||||
| KwaZulu-Natal | 26/111 (23) | 1.58 (0.93–2.68) | ||||
| Eastern Cape | 12/44 (27) | 1.94 (0.94–4.01) | ||||
| Free State | 11/62 (18) | 1.11 (0.55–2.28) | ||||
| Mpumalanga | 7/19 (37) | 3.02 (1.13–8.01) | ||||
| North-West | 11/23 (48) | 4.74 (1.99–11.30) | ||||
| Limpopo | 7/21 (33) | 2.58 (1.00–6.71) | ||||
| Northern Cape |
1/17 (6) |
0.32 (0.04–2.49) |
|
|
|
|
| Medical condition/treatment | ||||||
| Length of hospital stay, d | ||||||
| <3 | 94/209 (45) | Reference | <0.001 | Reference | <0.001 | |
| 4–14 | 36/354 (10) | 0.14 (0.09–0.21) | 0.06 (0.03–0.15) | |||
| >15 | 10/160 (6) | 0.08 (0.04–0.16) | 0.02 (0.01–0.07) | |||
| Pitt bacteremia score† | ||||||
| 0–3 | 102/608 (17) | Reference | <0.001 | |||
| >4 | 16/28 (58) | 6.61 (3.04–14.40) | ||||
| Underlying medical condition‡ | ||||||
| No | 55/343 (16) | Reference | 0.19 | Reference | 0.003 | |
| Yes | 33/158 (21) | 1.38 (0.86–2.23) | 3.21 (1.49–6.91) | |||
| Antimicrobial drug use in 24 h before admission | ||||||
| No | 82/504 (16) | Reference | 0.05 | |||
| Yes | 15/56 (26) | 1.88 (1.00–3.56) | ||||
| HIV status | ||||||
| HIV-uninfected | 37/252 (15) | Reference | 0.13 | Reference | 0.005 | |
| HIV-infected | 52/263 (20) | 1.43 (0.90–2.27) | 2.82 (1.36–5.84) | |||
| Malnourished§ | ||||||
| No | 44/277 (16) | Reference | 0.03 | |||
| Yes |
43/176 (24) |
1.71 (1.07–2.74) |
|
|
|
|
| Clinical syndrome/specimen type | ||||||
| Specimen type | ||||||
| CSF | 59/166 (36) | Reference | <0.001 | |||
| Blood | 83/530 (16) | 0.34 (0.23–0.50) | ||||
| Other | 1/39 (3) | 0.05 (0.01–0.36) | ||||
| Clinical syndrome¶ | ||||||
| Meningitis | 74/209 (35) | Reference | <0.001 | Reference | 0.0003 | |
| Pneumonia | 50/410 (12) | 0.25 (0.17–0.38) | 0.25 (0.11–0.54) | |||
| Bacteremia | 18/111 (16) | 0.35 (0.20–0.63) | 0.11 (0.03–0.42) | |||
*All patients were reported from the enhanced Group for Enteric, Respiratory, and Meningeal Disease Surveillance in South Africa (GERMS-SA) surveillance sites. Only variables significant on univariate and multivariable analysis are shown. Variables not included in table are sex, year, previous hospital admission, prematurity, antimicrobial drug in previous 2 mo, and penicillin nonsusceptible invasive pneumococcal disease. aOR, adjusted odds ratio; OR, odds ratio. †Pitt bacteremia score calculated using temperature, hypotension, mechanical ventilation, cardiac arrest and mental status. Severe disease defined as score of >4 points. ‡Includes asplenia or sickle cell anemia; chronic illness (i.e., chronic lung, renal, liver, cardiac disease, and diabetes); other immunocompromising conditions (i.e., organ transplant, primary immunodeficiency, immunotherapy, and malignancy, but excluding HIV); and other risk factors (i.e., head injury with possible cerebral spinal fluid leak, neurologic disorders, burns, and chromosomal abnormalities). Excludes malnutrition. §Children with weight-for-age z-score of less than −2 (World Health Organization child growth standards 2009) (18), nutritional edema, or both. ¶Clinical diagnoses were made on the basis of documented discharge diagnoses in patient medical records, with clinical syndrome separated into 3 groups: meningitis, bacteremic pneumonia, and bacteremia without focus or other diagnosis (e.g., septic arthritis, endopthalmitis, peritonitis, pericarditis)
Similar factors were associated with increased odds of death in persons >5 years of age with serotype 1 IPD (Technical Appendix Table 3). In addition, death was more likely among persons who had received tuberculosis treatment in the previous 3 months (OR 1.75, 95% CI 1.25–2.45) and among severely ill persons (OR 5.26, 95% CI 3.53–7.84 for patients with a Pitt bacteremia score >4). No difference was seen in the odds of death by HIV status. Compared with children 5–9 years of age, persons >25 years of age had incrementally increased odds of death by age group: 25–44 years of age, OR 5.07 (95% CI 2.74–9.38); 45–64 years of age, OR 9.00 (95% CI 4.66–17.35); and >64 years of age, OR 10.13 (95% CI 4.46–23.00).
Detection of Serotype 1 IPD Clusters
Of the 46,483 IPD cases, 34,032 (73%) had available data (i.e., date of specimen collection, geographic location of patient, and serotype results) and were included in the space–time scan analysis. Of these 34,032 cases, 4,544 (13%) were caused by serotype 1 IPD. Two clusters of serotype 1 were detected. The first (713 cases) occurred during May 2003–December 2004 and affected Gauteng Province and adjacent districts of Mpumalanga, Limpopo, and North-West Provinces (Figure 3, panel A; Technical Appendix Table 4). The second cluster (718 cases) occurred during September 2008–April 2012 and affected KwaZulu-Natal and Free State Provinces and adjacent districts of Gauteng, North-West, Mpumalanga, and Eastern Cape Provinces (Figure 3, panel B; Technical Appendix Table 4). We also assessed clustering of disease caused by 2 other epidemic-prone serotypes (serotypes 5 and 8); neither showed significant increases in case numbers compared with numbers in 2005.
Figure 3.
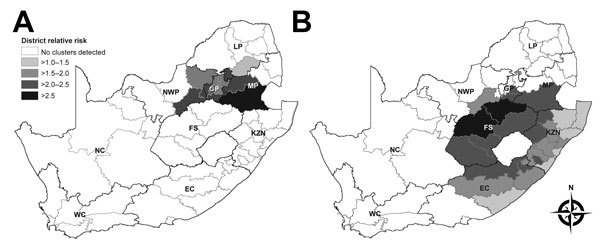
Serotype 1 invasive pneumococcal disease clusters by district, South Africa. A) May 2003–December 2004. B) September 2008–April 2012. Gray borders indicate district boundaries; black borders indicate provincial boundaries. Provinces: EC, Eastern Cape; FS, Free State; GP, Gauteng; KZN, KwaZulu-Natal; LP, Limpopo; MP, Mpumalanga; NC, Northern Cape; NWP, North-West; WC, Western Cape. District relative risk was calculated by dividing the observed number of cases per district by the number of cases expected by district (as determined on the basis of numbers in control groups).
Discussion
In South Africa, serotype 1 pneumococcal disease had a number of distinct features. Children <5 years of age with serotype 1 IPD were less likely to die than were children with disease caused by other serotypes; this association between serotype 1 and death was not seen in older children and adults. Patients with serotype 1 IPD had fewer cases of penicillin-nonsusceptible disease, a lower prevalence of HIV, and less severe disease than patients with non–serotype 1 IPD. However, pneumonia and bacteremia occurred more commonly in patients with serotype 1 IPD than in patients with IPD caused by other serotypes.
Serotype 1 IPD incidence differed by geographic area and year, reflecting its epidemic potential (1). In older children and adults, serotype 1 was the most common serotype over the entire study period, even though numbers were lower after PCV13 introduction. Before PCV7 introduction, serotype 1 was the sixth most common serotype in children <5 years of age; by 2013, it no longer ranked in the top 10 serotypes in this age group.
IPD is common in children with underlying diseases, including HIV. Compared with infections caused by other common pneumococcal serotypes, serotype 1 IPD was associated with more bacteremic pneumonia and peritonitis, occurred in older children and specific ethnic groups, and affected otherwise healthy children (3).
Serotype 1 IPD has marked temporal variability (19) and is associated with outbreaks (20,21). In our study, we noted fluctuations in incidence rates for serotype 1 IPD, especially among young children before PCV introduction. Incidence of serotype 1 IPD decreased in all age groups after 2011, likely due to the effect of PCV13, and serotype 1 disease nearly disappeared among the youngest children by 2013, two years after PCV13 introduction (10). We cannot exclude that other factors (e.g., improvements in access to antiretroviral treatment and programs for the prevention of mother-to-child HIV transmission) may have contributed to this decrease (14,22). We identified 2 large clusters that were not recognized prospectively because of the difficulty in identifying communitywide clusters in real time, especially using laboratory-based surveillance.
Our findings showed differences in the geographic distribution of serotype 1 and non–serotype 1 disease. Serotype 1 has been described to occur more frequently in underprivileged populations in developing countries (19); in our study, differences in specimen collection practices between provinces may have contributed to differences seen in disease distribution, as shown in other studies (23). Similar to findings by others (24,25), we found a difference in serotype distribution by age: serotype 1 IPD incidence was proportionally similar among older children and adults compared with that among children <1 year of age, whereas other serotypes predominated in the youngest age group and showed only a small peak in young adults. A number of factors may contribute to these age-associated differences (25). Compared with other serotypes, serotypes 1 and 5 are rarely carried by healthy persons; a short duration of carriage results in less opportunity for recombination events and less antibiotic selection pressure, resulting in reduced antibiotic nonsusceptibility in serotype 1 isolates (26).
Similar to findings in other studies (3), we found that, compared with other pneumococcal serotypes, serotype 1 caused more bacteremic pneumonia than meningitis. In addition, among HIV-uninfected children, serotype 1 IPD made up a larger proportion of disease than in HIV-infected children (27,28), suggesting that serotype 1 is more invasive and virulent, thus affecting otherwise healthy persons (29,30). Among children <5 years of age, those with serotype 1 disease were less likely to die than those with disease caused by other serotypes (31), and those most at risk of death were the very young (<1 year of age) and those HIV infected. In older persons, no association was found between serotype 1 disease and death when compared with other serotypes. Another analysis from the prevaccine era showed an increased risk of death among adults with serotype 1 disease compared with those with serotype 4 disease (32); this increased risk has been shown in few other studies (33).
Our study had several limitations. First, we included only patients who sought care at healthcare facilities with laboratories that submitted pneumococcal isolates to the National Institute for Communicable Diseases and who had specimens collected; patients with mild clinical pneumococcal disease treated in the community were not included. Second, we were able to map serotype 1 IPD incidence only at district level, so minor changes in incidence and clusters at the individual healthcare facility level may have been missed. Third, because of the small number of patients in the <5-year-old age group, we did not show clusters by age. We expect that reported clusters would have been similar for all ages. Fourth, we did not collect details regarding duration of symptoms before admission and thus could not assess whether intensity of symptoms when healthcare was sought affected case-fatality rates. Fifth, PCR serotype results from samples with a lytA cycle threshold (Ct) of >35 may not be accurate. We did not use PCR results in the trend analysis, and the proportion of lytA samples with high Ct values was low in the surveillance program (34), so the Ct accuracy is unlikely to have affected our results. Sixth, we used non–serotype 1 cases as our comparison group in the descriptive factor analysis; although this group changed over the study period, PCV13 serotypes (excluding serotype 1) made up >50% of this group until 2012 and 40% in 2013. Last, our study covered only a short period of observation after PCV13 introduction, making it difficult to determine whether reductions in serotype 1 IPD were due to introduction of this vaccine.
In conclusion, compared with IPD caused by other serotypes, IPD caused by serotype 1 in South Africa was characterized by shorter hospital stays, fewer cases of resistant disease, fewer in-hospital fatalities in children <5 years of age, and lower prevalence among HIV-infected persons. Serotype 1 caused disease in all age groups, although prevalence peaked in older children and young adults. Temporal reductions in serotype 1 IPD have been observed within 2 years of PCV13 introduction in South Africa; this observation must be corroborated by ongoing surveillance over an extended period of time.
Methods and case comparisons from enhanced and nonenhanced sites, South Africa, 2003–2013.
Acknowledgments
We thank all persons, and their caregivers, who kindly agreed to be included in this study. We acknowledge all GERMS-SA surveillance officers for their hard work in enrolling participants into the study and obtaining vaccination histories; the GERMS-SA coordinators for assisting the surveillance officers and clinical and intellectual input for the surveillance; laboratory staff throughout the country for submitting isolates to NICD; and staff at the NICD laboratory, Centre for Respiratory Diseases and Meningitis, for their efforts in processing and characterizing these isolates.
This study was supported by NICD/National Health Laboratory Service, South Africa; PEPFAR (President’s Emergency Plan for AIDS Relief) through the Centers for Disease Control and Prevention (cooperative agreement No. 5U2GPS001328); and the Global Alliance for Vaccines and Immunisation, Accelerated Vaccine Introduction Initiative Special Studies Team.
C.vM. has received honoraria from Pfizer. A.vG. has received research funding from Pfizer. S.A.M. has received honoraria from GlaxoSmithKline, Pfizer, and Sanofi Pasteur, and research funding from GlaxoSmithKline, Pfizer, and Novartis. H.D. has received honoraria from Novartis, Pfizer, Merck & Co., Inc. and a travel grant from Mylan. C.C. has received research funding from Pfizer and Sanofi Pasteur.
Biography
Dr. von Mollendorf is a medical epidemiologist in the Centre for Respiratory Diseases and Meningitis at the National Institute for Communicable Diseases in Johannesburg, South Africa. Her primary research interests include the epidemiology of respiratory diseases and meningitis and vaccine-preventable diseases.
Footnotes
Suggested citation for this article: von Mollendorf C, Cohen C, Tempia S, Meiring S, de Gouveia L, Quan V, et al. Epidemiology of serotype 1 invasive pneumococcal disease, South Africa, 2003–2013. Emerg Infect Dis. 2016 Feb [date cited]. http://dx.doi.org/10.3201/eid2202.150967
References
- 1.Ritchie ND, Mitchell TJ, Evans TJ. What is different about serotype 1 pneumococci? Future Microbiol. 2012;7:33–46. 10.2217/fmb.11.146 [DOI] [PubMed] [Google Scholar]
- 2.Gessner BD, Mueller JE, Yaro S. African meningitis belt pneumococcal disease epidemiology indicates a need for an effective serotype 1 containing vaccine, including for older children and adults. BMC Infect Dis. 2010;10:22. 10.1186/1471-2334-10-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fuchs I, Dagan R, Givon-Lavi N, Greenberg D. Serotype 1 childhood invasive pneumococcal disease has unique characteristics compared to disease caused by other Streptococcus pneumoniae serotypes. Pediatr Infect Dis J. 2013;32:614–8. 10.1097/INF.0b013e31828691cb [DOI] [PubMed] [Google Scholar]
- 4.Calbo E, Diaz A, Canadell E, Fabrega J, Uriz S, Xercavins M, et al. Invasive pneumococcal disease among children in a health district of Barcelona: early impact of pneumococcal conjugate vaccine. Clin Microbiol Infect. 2006;12:867–72. 10.1111/j.1469-0691.2006.1502_1.x [DOI] [PubMed] [Google Scholar]
- 5.Aguiar SI, Brito MJ, Goncalo-Marques J, Melo-Cristino J, Ramirez M. Serotypes 1, 7F and 19A became the leading causes of pediatric invasive pneumococcal infections in Portugal after 7 years of heptavalent conjugate vaccine use. Vaccine. 2010;28:5167–73. 10.1016/j.vaccine.2010.06.008 [DOI] [PubMed] [Google Scholar]
- 6.Feikin DR, Kagucia EW, Loo JD, Link-Gelles R, Puhan MA, Cherian T, et al. Serotype-specific changes in invasive pneumococcal disease after pneumococcal conjugate vaccine introduction: a pooled analysis of multiple surveillance sites. PLoS Med. 2013;10:e1001517. 10.1371/journal.pmed.1001517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson HL, Deloria-Knoll M, Levine OS, Stoszek SK, Freimanis Hance L, Reithinger R, et al. Systematic evaluation of serotypes causing invasive pneumococcal disease among children under five: the pneumococcal global serotype project. PLoS Med. 2010;7:e1000348. 10.1371/journal.pmed.1000348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hanquet G, Kissling E, Fenoll A, George R, Lepoutre A, Lernout T, et al. Pneumococcal serotypes in children in 4 European countries. Emerg Infect Dis. 2010;16:1428–39. 10.3201/eid1609.100102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jefferies JM, Smith AJ, Edwards GF, McMenamin J, Mitchell TJ, Clarke SC. Temporal analysis of invasive pneumococcal clones from Scotland illustrates fluctuations in diversity of serotype and genotype in the absence of pneumococcal conjugate vaccine. J Clin Microbiol. 2010;48:87–96. 10.1128/JCM.01485-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miller E, Andrews NJ, Waight PA, Slack MP, George RC. Effectiveness of the new serotypes in the 13-valent pneumococcal conjugate vaccine. Vaccine. 2011;29:9127–31. 10.1016/j.vaccine.2011.09.112 [DOI] [PubMed] [Google Scholar]
- 11.Klugman KP, Madhi SA, Adegbola RA, Cutts F, Greenwood B, Hausdorff WP. Timing of serotype 1 pneumococcal disease suggests the need for evaluation of a booster dose. Vaccine. 2011;29:3372–3. 10.1016/j.vaccine.2011.02.089 [DOI] [PubMed] [Google Scholar]
- 12.Cutts FT, Zaman SM, Enwere G, Jaffar S, Levine OS, Okoko JB, et al. Efficacy of nine-valent pneumococcal conjugate vaccine against pneumonia and invasive pneumococcal disease in The Gambia: randomised, double-blind, placebo-controlled trial. Lancet. 2005;365:1139–46. 10.1016/S0140-6736(05)71876-6 [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization. WHO UNICEF estimates of PCV3 coverage [cited 2015 Aug 14]. http://apps.who.int/immunization_monitoring/globalsummary/timeseries/tswucoveragepcv3.html
- 14.von Gottberg A, de Gouveia L, Tempia S, Quan V, Meiring S, von Mollendorf C, et al. Effects of vaccination on invasive pneumococcal disease in South Africa. N Engl J Med. 2014;371:1889–99. 10.1056/NEJMoa1401914 [DOI] [PubMed] [Google Scholar]
- 15.Carvalho MG, Tondella ML, McCaustland K, Weidlich L, McGee L, Mayer LW, et al. Evaluation and improvement of real-time PCR assays targeting lytA, ply, and psaA genes for detection of pneumococcal DNA. J Clin Microbiol. 2007;45:2460–6. 10.1128/JCM.02498-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kulldorff M. A spatial scan statistic. Comm Stat Theory Methods. 1997;26:1481–96. 10.1080/03610929708831995 [DOI] [Google Scholar]
- 17.Kulldorff M, Nagarwalla N. Spatial disease clusters: detection and inference. Stat Med. 1995;14:799–810. 10.1002/sim.4780140809 [DOI] [PubMed] [Google Scholar]
- 18.WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards: Growth velocity based on weight, length and head circumference: Methods and development. Geneva: World Health Organization; 2009. [cited 2015 Aug 14]. http://www.who.int/childgrowth/publications/technical_report_velocity/en/
- 19.Lagos R, Muñoz A, San Martin O, Maldonado A, Hormazabal JC, Blackwelder WC, et al. Age- and serotype-specific pediatric invasive pneumococcal disease: insights from systematic surveillance in Santiago, Chile, 1994–2007. J Infect Dis. 2008;198:1809–17. 10.1086/593334 [DOI] [PubMed] [Google Scholar]
- 20.Le Hello S, Watson M, Levy M, Marcon S, Brown M, Yvon JF, et al. Invasive serotype 1 Streptococcus pneumoniae outbreaks in the South Pacific from 2000 to 2007. J Clin Microbiol. 2010;48:2968–71. 10.1128/JCM.01615-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Antonio M, Hakeem I, Awine T, Secka O, Sankareh K, Nsekpong D, et al. Seasonality and outbreak of a predominant Streptococcus pneumoniae serotype 1 clone from The Gambia: expansion of ST217 hypervirulent clonal complex in West Africa. BMC Microbiol. 2008;8:198. 10.1186/1471-2180-8-198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnson LF. Access to antiretroviral treatment in South Africa, 2004–2011. Southern African Journal of HIV Medicine. 2012;13:22–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hausdorff WP, Siber G, Paradiso PR. Geographical differences in invasive pneumococcal disease rates and serotype frequency in young children. Lancet. 2001;357:950–2. 10.1016/S0140-6736(00)04222-7 [DOI] [PubMed] [Google Scholar]
- 24.Ciruela P, Soldevila N, Selva L, Hernández S, Garcia-Garcia JJ, Moraga F, et al. Are risk factors associated with invasive pneumococcal disease according to different serotypes? Hum Vaccin Immunother. 2013;9:712–9. 10.4161/hv.23270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hausdorff WP, Feikin DR, Klugman KP. Epidemiological differences among pneumococcal serotypes. Lancet Infect Dis. 2005;5:83–93. 10.1016/S1473-3099(05)70083-9 [DOI] [PubMed] [Google Scholar]
- 26.Porat N, Trefler R, Dagan R. Persistence of two invasive Streptococcus pneumoniae clones of serotypes 1 and 5 in comparison to that of multiple clones of serotypes 6B and 23F among children in southern Israel. J Clin Microbiol. 2001;39:1827–32. 10.1128/JCM.39.5.1827-1832.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jones N, Huebner R, Khoosal M, Crewe-Brown H, Klugman K. The impact of HIV on Streptococcus pneumoniae bacteraemia in a South African population. AIDS. 1998;12:2177–84. 10.1097/00002030-199816000-00013 [DOI] [PubMed] [Google Scholar]
- 28.Scott JA, Hall AJ, Hannington A, Edwards R, Mwarumba S, Lowe B, et al. Serotype distribution and prevalence of resistance to benzylpenicillin in three representative populations of Streptococcus pneumoniae isolates from the coast of Kenya. Clin Infect Dis. 1998;27:1442–50. 10.1086/515013 [DOI] [PubMed] [Google Scholar]
- 29.Brueggemann AB, Peto TE, Crook DW, Butler JC, Kristinsson KG, Spratt BG. Temporal and geographic stability of the serogroup-specific invasive disease potential of Streptococcus pneumoniae in children. J Infect Dis. 2004;190:1203–11. 10.1086/423820 [DOI] [PubMed] [Google Scholar]
- 30.Hausdorff WP. The roles of pneumococcal serotypes 1 and 5 in paediatric invasive disease. Vaccine. 2007;25:2406–12. 10.1016/j.vaccine.2006.09.009 [DOI] [PubMed] [Google Scholar]
- 31.Weinberger DM, Harboe ZB, Sanders EA, Ndiritu M, Klugman KP, Ruckinger S, et al. Association of serotype with risk of death due to pneumococcal pneumonia: a meta-analysis. Clin Infect Dis. 2010;51:692–9. 10.1086/655828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cohen C, Naidoo N, Meiring S, de Gouveia L, von Mollendorf C, Walaza S, et al. Streptococcus pneumoniae serotypes and mortality in adults and adolescents in South Africa: analysis of national surveillance data, 2003–2008. PLoS ONE. 2015;10:e0140185. 10.1371/journal.pone.0140185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Martens P, Worm SW, Lundgren B, Konradsen HB, Benfield T. Serotype-specific mortality from invasive Streptococcus pneumoniae disease revisited. BMC Infect Dis. 2004;4:21. 10.1186/1471-2334-4-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Magomani V, Wolter N, Tempia S, du Plessis M, de Gouveia L, von Gottberg A. Challenges of using molecular serotyping for surveillance of pneumococcal disease. J Clin Microbiol. 2014;52:3271–6. 10.1128/JCM.01061-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Methods and case comparisons from enhanced and nonenhanced sites, South Africa, 2003–2013.


