Abstract
We examined whether maternal emotion coaching at pre-treatment predicted children's treatment response following a 12-week program addressing children's Oppositional Defiant Disorder (ODD) symptoms. Eighty-nine mother-child dyads participated. At pre-treatment, mothers and children engaged in an emotion talk task. Mothers also reported their beliefs about emotions at pre-treatment and their child's disruptive behavior symptoms, emotion regulation, and emotion lability/negativity at pre-, mid-, and post-treatment. Clinicians reported children's symptom severity at pre- and post-treatment. Children's emotion lability/negativity moderated effects of maternal emotion coaching on children's post-treatment ODD symptoms, with stronger benefits of emotion coaching for children high in emotion lability/negativity. Results suggest that emotion coaching may promote treatment response for children with ODD who are especially at risk due to their emotionality.
Oppositional Defiant Disorder (ODD) is characterized by persistent argumentative, defiant, and hostile behaviors toward authority figures (Loeber, Burke, Lahey, Winters & Zera, 2000; Murrihy, Kidman, & Ollendick, 2010). Symptoms include loss of temper, being easily annoyed, and being spiteful or vindictive (American Psychiatric Association, 2013). Parents of children with ODD are more likely to use child mental health services than parents of children with other disorders (Cohen et al., 1993; Murrihy et al., 2010). Even when accounting for its association with attention-deficit/hyperactivity disorder (ADHD), ODD adversely affects children's social and family functioning and long-term outcomes (Greene et al., 2002; Kazdin, 2009).
Parent management training (PMT) programs are viewed as the “standard of care” for ODD, predominating in research and clinical practice (Eyberg, Nelson, & Boggs, 2008; Murrihy et al., 2010; Nock, 2003). In general, PMT teaches parents to use contingency management procedures. Research documenting its efficacy qualifies PMT as an empirically supported psychosocial treatment (i.e., Eyberg et al., 2008; Ollendick & King, 2012; Webster-Stratton & Reid, 2010). Nonetheless, limitations in PMT outcomes exist. Even among families who fully complete treatment, a substantial percentage (30 – 50%) of children continue to show deviant behavior above normative levels when treatment is terminated (partial responders) or have returned to the clinical range at follow-up (i.e., treatment refractory; Ollendick & King, 2012; Webster-Stratton & Reid, 2010). Thus, it is important to identify factors that may promote the likelihood of treatment response for children with ODD.
The purpose of this study was to examine maternal emotion coaching as a factor that might enhance response to treatment for ODD. Emotion coaching is characterized by parents’ acknowledgement and acceptance of children's negative emotions and verbal coaching to help children understand, appropriately express, and cope with negative emotions (Gottman, Katz, & Hooven, 1997). With typically-developing and at-risk samples, emotion coaching is associated with better emotional competence (Katz, Maliken, & Stettler, 2012). Furthermore, both concurrent (Ramsden & Hubbard, 2002) and longitudinal (Cunningham, Kliewer, & Garner, 2009; Gottman, et al., 1996) research suggests that emotion coaching may indirectly affect child outcomes through its direct association with children's emotion regulation. This is pertinent for the current work given that deficits in self-regulation and affective modulation are viewed as important contributors to the development of ODD (see Greene & Doyle, 1999).
Emotion Coaching
Emotion coaching is part of a broader meta-emotion philosophy that includes parental awareness of children's emotions, beliefs accepting children's emotional experience as valid, behaviors acknowledging children's emotions, and teaching about understanding, coping with, and appropriately expressing emotions. Parental meta-emotion philosophies are unrelated to parental warmth and related to but separate from broader socialization constructs such as harsh or responsive parenting styles (Gottman et al., 1997; Katz et al., 2012). Emotion coaching is associated with adolescents’ lower externalizing (Shortt, Stoolmiller, Smith-Shine, Eddy, & Sheeber, 2010) and internalizing problems (Katz, & Hunter, 2007; Stocker, Richmond, Rhoades & Kiang, 2007).
Only two prior studies, to our knowledge, have examined emotion coaching in families with a child with a disruptive behavior disorder. Katz and Windecker-Nelson (2004) compared preschool-age children who met diagnostic criteria for ODD or for conduct disorder (CD) with matched control children with no diagnoses. Relative to control participants, mothers of children with ODD or CD were lower in emotion coaching and children with ODD or CD were higher in aggression and showed lower quality peer interaction. Moreover, across both groups of children, mothers’ emotion coaching was related to better quality peer interactions.
In the second study to examine emotion coaching - our own previous work with the current sample - we examined linkages of mothers’ emotion coaching with children's (7 – 14 years of age) adjustment in families seeking treatment for ODD. Higher levels of maternal emotion coaching were associated with higher maternal reports of children's emotion regulation and lower child-reported disruptive behavior problems (Dunsmore, Booker & Ollendick, 2013).
Both of these previous studies were cross-sectional, so directionality could not be established. Emotion coaching is posited to affect children's emotion regulation, which in turn is proposed to effect change in children's outcomes (Gottman et al., 1997). Alternatively, children with better emotion regulation skills or who experience less intense emotionality may be easier or more rewarding for parents to emotion coach. Because emotion regulation is the keystone of Gottman and colleagues’ (1997) theory of how emotion coaching influences child outcomes, we turn next to emotion regulation and emotion lability/negativity.
Emotion Regulation and Lability/Negativity
Definitions and interrelations
Emotion regulation involves children's ability to selectively maintain and alter emotional experiences and expressions (Shields & Cicchetti, 1998). This may include modifying attention, changing strategies when processing emotion-related stimuli, and making adjustments to current behaviors (Eisenberg, Fabes, Guthrie, & Reiser, 2000). Emotion lability/negativity involves high arousal and emotional intensity in responding to situations (Flett, Blankstein, Bator, & Plimer, 1989). People high in lability/negativity experience more quick and dramatic mood swings and may be emotionally inconsistent in responding to situations and events (Shields & Cicchetti, 1998).
Studies involving both typically-developing and maltreated children have shown a negative association between emotion regulation and emotion lability/negativity (Kim, Cicchetti, & Rogosch, 2012; Lunkenheimer, Shields & Cortina, 2007; Shields & Cicchetti, 1998). As such, it is possible to think of these constructs as two ends of a single spectrum. We prefer, however, to consider emotion regulation and emotion lability/negativity as distinct constructs. Conceptually, it is important to distinguish the experience of emotion from its regulation (Cole, Martin & Dennis, 2004). Whereas lability and negativity of emotional experience may reflect temperament dimensions of emotionality and attentional processes, emotion regulation includes skills and strategies, which may be learned (Halberstadt, Denham, & Dunsmore, 2001). Research also supports distinguishing between emotion regulation and lability/negativity. When examined longitudinally, emotion regulation is predicted by earlier emotion lability/negativity, whereas emotion lability/negativity is not predicted by earlier emotion regulation (Kim et al., 2012). This suggests that pre-existing lability/negativity may complicate the regulation of emotions; yet, developing emotion regulation skills may do little to alter the tendency toward labile reactivity and negative emotionality.
Difficulties with emotion regulation and lability/negativity are considered fundamental contributors to children's ODD symptoms and their treatment (Greene & Doyle, 1999). A low threshold for experiencing negative emotion and difficulty managing negative emotion in social interactions are apparent in the symptoms for ODD, such as temper tantrums, being argumentative, and behaving aggressively toward others. Given this, it is not surprising that negative emotionality at 3 years of age is predictive of ODD diagnosis at 7 ½ years (Stringaris, Maughan, & Goodman, 2010).
Associations with emotion coaching
Research with preschoolers and with youth from middle childhood to early adolescence suggests that earlier emotion coaching may indirectly affect later child outcomes through its direct effect on emotion regulation. Gottman and colleagues (1996) assessed parents’ emotion coaching and children's emotion regulation (indexed by vagal tone) with typically-developing preschoolers. Three years later, children of parents higher in emotion coaching showed better academic achievement and peer relations, through direct effects of children's emotion regulation. Notably, equivalent support was found for an alternative model with child emotion regulation showing an indirect association with academic achievement and peer relations through its direct effect on parent emotion coaching. This suggests bidirectionality of relations between emotion coaching and emotion regulation.
Cunningham and colleagues (2009) studied families with 9- to 13-year-old children living in violent neighborhoods. For boys (but not girls), associations of baseline maternal emotion coaching with six-month change in grades, internalizing behaviors, externalizing behaviors, and social skills were attenuated by emotion-regulation at six-month follow-up. Again, however, bidirectionality between emotion coaching and emotion regulation is possible.
Finally, in our previous work with this sample at pre-treatment, children whose mothers engaged in more emotion coaching were higher in emotion regulation, reported fewer internalizing symptoms and better psychological adjustment (a composite of self-esteem and social relations), and had mothers who reported their social skills as more adaptive (Dunsmore et al., 2013). The current study expands on previous work by including three time points – pre-treatment, mid-treatment, and post-treatment. Thus, we were able to test whether children's emotion regulation at mid-treatment mediated effects of maternal emotion coaching at pre-treatment on children's post-treatment ODD symptoms.
The frequent and intense emotional arousal experienced by children high in emotion lability/negativity places greater demands on parents and may make it difficult to immediately engage in emotion coaching, when children's intensity of negative emotion may interfere with their ability to attend to and process parents’ messages about emotions. Alternatively, children high in lability/negativity may be especially in need of parents’ emotion coaching, and their more frequent outbursts may, perhaps counterintuitively, provide parents with better opportunities for emotion coaching. When a child infrequently shows negative emotion, or is quickly able to regulate negative emotion without assistance, parents’ emotion coaching may seem unnecessary or even awkward, especially for older children and adolescents, who are more autonomously regulated and more sensitive to the social context than younger children (Zeman, Cassano, Perry-Parrish, & Stegall, 2006). However, when a child frequently shows negative emotion and appears to need guidance to regulate negative emotions, parents’ emotion coaching – whether in the moment or after a chance to regain composure – may seem more natural and be perceived as more helpful by both parent and child. In our previous work with this sample, we found that protective effects of emotion coaching for children's concurrent externalizing symptoms were stronger for children high in emotion lability/negativity. Thus, in the current study we examined whether a similar moderating effect would be found for children's treatment response.
The Present Study
The present study enrolled families seeking treatment for their child's ODD symptoms (Ollendick et al., 2014). Families were randomly assigned to one of two treatment conditions: Parent Management Training (PMT: Barkley, 1997) or Collaborative and Proactive Solutions (CPS: Greene, 1998, 2010). In general, PMT emphasizes ineffective parenting practices in the origins and course of oppositional behavior in youth. In contrast, CPS emphasizes lagging cognitive and emotional skills – especially in the domains of flexibility/adaptability and frustration tolerance/emotion dysregulation – as major factors contributing to the development of oppositional behavior. In each treatment, both children and parents participate to facilitate parents’ mastery of skills. In this randomized controlled trial, equivalence of outcomes between the two treatments was demonstrated (Ollendick et al., 2014).
Mothers’ emotion coaching at pre-treatment was measured through self-report of beliefs about emotions and observation of behaviors encouraging children's expression of positive and negative emotions during parent-child discussion of emotion-related family events. Though emotion coaching is often measured using the semi-structured Meta-Emotion Interview (Katz & Gottman, 1986) to access parents’ awareness and acceptance of their and their child's sadness and anger, and their coaching of children's sadness and anger, this method was too time-intensive for the current study and lacked behavioral observation for addressing both parents’ emotion socialization behaviors and beliefs. Furthermore, we thought it important to include parents’ coaching of positive as well as negative emotions because socialization of both positive and negative emotions is important in children's formation of schemas about themselves and the social world (Dunsmore & Halberstadt, 1997).
At pre-, mid- and post-treatment, mothers reported on children's disruptive behavior symptoms, emotion regulation, and emotion lability/negativity. Trained clinicians rated the severity of children's symptoms at pre- and post-treatment.
We expected mothers’ pre-treatment emotion coaching to be negatively associated with children's post-treatment symptoms after controlling for pre-treatment symptoms (i.e., higher emotion coaching would be associated with lower ODD symptoms following treatment). We expected further that benefits of emotion coaching would be stronger for children high in emotion lability/negativity. We also expected that mid-treatment emotion regulation would serve as a mediator for an indirect influence of pre-treatment emotion coaching on post-treatment symptoms.
Method
Participants
Families were a subset of a larger sample participating in an NIMH-funded clinical trial (Ollendick et al., 2014). Families were referred by mental health professionals, family practice physicians, and school personnel, or self-referred through advertisements and word of mouth. One-hundred thirty-four families participated in treatment, of whom 89 completed the pre-treatment and post-treatment assessments (66.42%). The current study includes only those 89 families. Compared with those who did not complete post-treatment assessment, families who remained in the study had higher average family incomes (t(112) = 2.18, p = .031) and more educated mothers (χ(6, N = 133) = 13.47, p = .036) and fathers (χ(7, N = 123) = 29.72, p < .001). The sample for the current study did not differ from the larger sample on pre-treatment maternal and clinician reports of disruptive behavior symptoms.
Within the final sample, 28 of the 89 families had both mother and father participate with the child in the emotion talk task; for the remaining 61 families only the mother participated. Children included 35 daughters and 54 sons (M child age = 9.47 years, SD = 1.78, range = 7 – 14 years; M mother age = 40.49 years, SD = 6.63, range = 26 – 58 years). Two children were Asian (2.2%), 14 were African-American (15.7%), four were Hispanic-American (4.5%), and 69 were Caucasian (77.5%). Most mothers (98.9%) had completed high school. Thirty-two mothers (36%) had completed college and 22 (24.7%) had completed post-graduate education. Most mothers were married to the child's father (62.9%), one (1.1%) was unmarried and living with the child's father, and six (6.7%) were married to the child's stepfather. Seven mothers (7.9%) reported being single parents and nine (10.1%) were separated or divorced from the child's father. Two mothers were adoptive or foster parents (2.2%), and three mothers (3.4%) reported other family structures. The mean family income was $72,240, with a range of $4,000 to $175,000. This is higher than the mean household incomes for the communities in which families primarily resided ($30,881 - $44,166 from 2008 – 2012; United States Census, 2012).
Procedures
Families visited a university-based research clinic to seek treatment for their child's oppositional behaviors. As part of a two-session pre-treatment assessment, mothers completed a semi-structured diagnostic interview and questionnaires concerning their emotion-related beliefs, their child's emotion regulation and lability/negativity, their child's disruptive behavior symptoms, and demographics. Mothers and children participated in a 9-minute discussion of emotion-related family events. Each assessment session lasted approximately 2 hours.
After completing pre-treatment assessment, families who qualified for this clinical trial were randomly assigned into one of two psychosocial treatment programs, Parent Management Training (PMT, n = 64) and Collaborative & Proactive Solutions (CPS, n = 70). Using principles of contingency management, PMT aids parents in altering children's behavior at home, in the school, and in the community - with the goal of building stronger skills in regulating emotions and behaviors (Barkley, 1997). Treatment sessions are highly structured to increase positive interactions between parents and children and decrease contentious behaviors (Forgatch & Patterson, 2010). PMT is considered the standard of care for ODD (Ollendick & King, 2012).
Treatment with CPS involves training parents to respond to disruptive behaviors with the understanding that children may not be in control of the situation and their behaviors (Greene, 2010). Parents learn to address the elements of the situation that may be contributing to detrimental behavior (Greene, 2010). This approach aims to improve both children's compliance and parents’ efficacy in managing children's disruptive behaviors (Greene, 1998, 2010). CPS, more recently-developed than PMT, is associated with improvement in parents’ management of children's behaviors and decreases in children's disruptive behaviors (Greene, 2010).
Clinicians trained specifically in each approach delivered treatments. All assessments and treatments were conducted by trained graduate students enrolled in an American Psychological Association-approved doctoral program in Clinical Psychology or postdoctoral fellows associated with that program. Children participated with parents in each treatment session. Both treatments were delivered to individual families for approximately twelve 75-minute sessions (range = 7 – 14 sessions). Number of sessions attended did not differ across treatment types, nor did attrition from pre- to post-treatment. Treatment adherence confirmed integrity of the individual treatments (Ollendick et al., 2014).
At the sixth week, or mid-point, of treatment families participated in a mid-treatment assessment that lasted approximately 1 hour. Again, mothers reported on children's disruptive behavior symptoms, emotion regulation and lability/negativity.
One week following completion of treatment, families returned for a 2-hour post-treatment assessment. Mothers completed a semi-structured diagnostic interview and reported on children's emotion regulation, lability/negativity and disruptive behavior symptoms. In both the larger clinical trial (Ollendick et al., 2014) and this sub-sample, no differences due to type of treatment were found in treatment outcomes. Both treatments were equally effective. In this sub-sample, maternal emotion coaching did not significantly differ across treatment type, t (87) = 1.64, p = .104, and regressions showed no significant moderation by treatment type on effects of emotion coaching on post-treatment clinician severity reports and maternal reports of disruptive behavior symptoms, ps > .20. Accordingly, analyses herein are collapsed across the two treatment groups.
Materials
The Anxiety Disorders Interview Schedule for DSM-IV, Parent Version (ADIS-P; Silverman & Albano, 1996)
The ADIS-P is a semi-structured interview designed to diagnose a number of disorders typical in childhood and adolescence. Clinicians interviewed parents to assess children's symptoms, their frequency and intensity, and the extent to which symptoms interfered with children's functioning. Binary responses and numbers from a 0-8 scale were used as appropriate. These ratings were used to identify diagnostic criteria for each child and to record the clinician's severity rating (CSR) for ODD. A CSR of 4 or above on the 0 – 8 scale indicated diagnosable ODD.
The ADIS-P shows satisfactory 7 to 14-day test-retest reliability for parent-derived diagnoses (Silverman, Saavedra, & Pina, 2001) and has demonstrated reliability and validity for youth with ODD (Anderson & Ollendick, 2012) and ADHD (Jarrett, Wolff, & Ollendick, 2007). All assessment interviews were videotaped; 35% of interviews were reviewed for inter-rater reliability (κ = .89 for diagnosis of ODD). All children included in this study were diagnosed with ODD as one of their three top diagnoses. ODD was the primary diagnosis for most participating children (56.4%) and in all cases it was the primary reason for referral. Among the first three diagnoses, the most frequent comorbid diagnoses included ADHD-combined type (44.5%), specific phobia (28.6%), social phobia (20.6%), and Generalized Anxiety Disorder (12.8%). A majority (87.3%) of the participating children had at least one comorbid diagnosis, and 47.6% had two or more comorbid diagnoses.
Disruptive Behavior Disorders Rating Scale (Pelham, Gnagy, Greensalde, & Milich, 1992)
Mothers reported on 42 items concerning four subscales: inattention; hyperactivity; Oppositional Defiant Disorder; and Conduct Disorder. The subscale of interest was Oppositional Defiant Disorder. This included 8 items tapping the eight ODD symptoms and rated on a 4-point Likert scale (0 = never or rarely, 3 = very often). Responses were dichotomized and only coded as affirmative if said to occur “often” or “very often.” This scale was completed at pre-treatment (α = .83), mid-treatment (α = .90) and post-treatment (α = .89).
Emotion Regulation Checklist (ERC; Shields & Cicchetti, 1997)
Mothers responded to 24 items on a 4-point Likert-type scale (1 = never, 4 = almost always). The ERC includes two subscales: (a) emotion regulation (8 items; sample item: “Is a cheerful child”) and (b) emotion lability/negativity (15 items; sample item “Is whiny or clingy with adults”). Mother reports of emotion regulation were found to have reliabilities of α = .42 at Pre-treatment, α = .51 at Mid-treatment, and α = .63 at Post-treatment. Mother reports of emotion lability/negativity were found to have reliabilities of α = .70 at Pre-treatment, α = .77 at Mid-treatment, and α = .83 at Post-treatment. Previous studies show internal consistency for the emotion regulation subscale ranging from α = .62 to α > .80 (i.e., Cunningham et al., 2009; Kim et al., 2012; Shields & Cicchetti, 1997), and for emotion lability/negativity α > .80 (Kim et al., 2012; Shields & Cicchetti, 1997).
Parents’ Beliefs about Children's Emotions Questionnaire (PBACE; Halberstadt et al., 2008)
Mothers rated their agreement with statements about beliefs about children's emotions on a six-point Likert scale (1 = strongly disagree, 6 = strongly agree). The 61-item short form of this questionnaire was used. Subscales of interest were (a) value of positive emotions (5 items; sample item: “It is important for children to express their happiness when they feel it”; α = .77 for this sample), (b) value of negative emotions (7 items; sample item: “Being angry can motivate children to change or fix something in their lives”; α = .93 for this sample), and (c) parents’ role in guiding children's emotions (5 items, sample item: “An important role for parents is to help their child understand the children's feelings”; α = .77 for this sample).
Parent-Child Emotion Talk Task
During the pre-treatment and post-treatment assessment sessions, families engaged in a 9-minute video-recorded conversation about family memories. Three cards were used to prompt emotion-related discussions: (a) describe something fun you did last week with the other person, (b) describe a time in the last week when you were with the other person and got upset, mad, sad, or scared, and (c) describe something you did last Sunday. Cards were shuffled before each family began and participants were instructed to freely discuss memories described by each other, just as they would at home. Families were encouraged to return to earlier cards if they finished before time was up; however, only the first response to each card was coded.
Videotapes were coded for mothers’ encouragement of their children's emotions during the children's response to each card. A 4-point scale was used: 0 = no evidence of encouragement, 1 = acknowledgement of the event described, 2 = acknowledgement of the child's emotion, and 3 = emotion coaching, which could include one or more of the following: labeling and empathizing with the emotion, discussing causes and consequences of the emotion, or helping the child to problem-solve about the emotion. Encouragement of positive and negative emotions was coded separately for each card, then averaged across the events discussed, yielding two scores. For example, within a single event, both positive and negative encouragement could be coded if mothers supported both positive and negative emotions pertaining to the same event. When families did not finish all three cards within the 9-minute time limit, scores for positive and negative encouragement were pro-rated according to the number of cards completed. At least 25% of all videotapes were coded for reliability by independent coders and reliability was maintained at ICC > .80 throughout the study.
Results
Preliminary Analyses
Independent samples t-tests were used to determine whether mothers’ scores for encouraging positive emotions and encouraging negative emotions differed according to whether only mother and child participated in the pre-treatment emotion talk task or whether both parents participated with the child in the task. There were no significant differences according to presence/absence of both parents, both ps > .20. Furthermore, regressions showed no interaction of child sex with presence/absence of both parents when predicting mothers’ encouragement of positive and negative emotions, both ps > .50. Therefore, we retained all mothers in the sample and proceeded with forming a maternal emotion coaching composite.
We standardized and summed scores for mothers’ belief that positive emotions are valuable, mothers’ belief that negative emotions are valuable, mothers’ belief in the role of parents to guide children's emotions, and mothers’ encouraging of children's positive and negative emotions to form an emotion-coaching composite. This is consistent with our earlier approach (Dunsmore et al., 2013) and uses both observed and self-reported information. When an index in the composite was missing, the composite was calculated across available indices. For four families, the mother completed neither the questionnaire measure for the emotion coaching composite nor the emotion interaction task at pre-treatment. Emotion coaching scores for these families were imputed using expectation maximization. There were no differences in mothers’ emotion coaching scores according to child sex (t(87) = .21, p = 205) or child race (F(3, 81) = .64, p = .592).
Despite completing the post-treatment assessment, 28 mothers did not turn in the post-treatment report of disruptive behavior symptoms. Missing values for mothers’ post-treatment reports were imputed using expectation maximization. Descriptive data for all study variables are reported in Table 1. A paired samples t-test showed that the clinician severity rating for ODD symptoms significantly decreased from pre- to post-treatment, t(88) = 9.85, p = .000. Repeated measures ANOVAs showed that maternal reports of emotion lability/negativity (Wilks’ lambda = .51, F (2, 87) = 42.42, p = .000) and disruptive behavior symptoms (Wilks’ lambda = .36, F (2, 87) = 77.73, p = .000) significantly decreased across pre-, mid-, and post-treatment time points, whereas emotion regulation significantly increased across pre-, mid-, and post-treatment time points, Wilks’ lambda = .89, F (2, 87) = 5.20, p = .007.
Table 1.
Descriptive Information for Study Variables
| Variable | Mean | SD | Range |
|---|---|---|---|
| Pre-treatment | |||
| Emotion coaching composite | 0.07 | 2.23 | −7.28 – 5.21 |
| Emotion regulation | 2.95 | 0.37 | 2.00 – 3.75 |
| Emotion lability/negativity | 2.50 | 0.35 | 1.60 – 3.33 |
| Disruptive behavior symptoms | 5.66 | 1.67 | 1 – 8 |
| Clinician severity rating | 5.82 | 1.02 | 4 – 8 |
| Mid-treatment | |||
| Emotion regulation | 2.93 | 0.42 | 1.88 – 4.00 |
| Emotion lability/negativity | 2.37 | 0.33 | 1.40 – 3.13 |
| Disruptive behavior symptoms | 2.22 | 2.64 | 0 – 8 |
| Post-treatment | |||
| Emotion regulation | 3.03 | 0.40 | 2.13 – 4.00 |
| Emotion lability/negativity | 2.15 | 0.40 | 1.20 – 3.07 |
| Disruptive behavior symptoms | 2.74 | 2.47 | 0 – 8 |
| Clinician severity rating | 3.66 | 2.07 | 0 – 8 |
Note. N = 89.
T-tests showed that mothers reported more disruptive behavior symptoms at post-treatment for daughters (M = 3.81, SD = 2.66) than for sons (M = 2.04, SD = 2.09; t(87) = 2.56, p = .001). However, there was no child sex difference in post-treatment clinician severity reports, t(87) = −1.35, p = .181. Correlations showed that both mothers and clinicians reported more disruptive behavior symptoms at post-treatment for older children, rs > .20, ps < .05. Child age was controlled in subsequent analyses, and child sex was controlled when predicting maternal post-treatment symptom report.
Hypothesis Testing
Correlations
See Table 2 for correlations among all study variables. In this paragraph, we focus only on correlations across constructs and across time-points. Though the maternal emotion coaching composite was not significantly correlated with children's post-treatment ODD symptoms, it was significantly related to mid-treatment emotion regulation. Emotion regulation and lability/negativity were inversely associated across time points. Pre- and mid-treatment emotion lability/negativity were related to post-treatment disruptive behavior symptoms. Mid-treatment lability/negativity was also related to post-treatment clinician severity report.
Table 2.
Correlations among Study Variables.
| 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Emotion coaching comp. (pre) | .18* | −.17 | −.08 | −.07 | .22* | −.11 | −.07 | .13 | −.19* | −.09 | −.04 |
| 2. Emotion regulation (pre) | -- | −.20* | −.21* | −.18* | .66*** | −.28** | −.04 | .67*** | −.30** | −.04 | .03 |
| 3. Emotion lability/negativity (pre) | -- | .44*** | .35** | −.34** | .57*** | .06 | −.27* | .49*** | .23* | .19* | |
| 4. Disruptive beh. symptoms (pre) | -- | .43*** | −.21* | .35** | .20* | −.23* | .18* | .21* | .08 | ||
| 5. Clinician severity report (pre) | -- | −.18* | .27* | .15 | −.24* | .28** | .18* | .25* | |||
| 6. Emotion regulation (mid) | -- | −.50*** | −.21* | .71*** | −.54*** | −.05 | −.08 | ||||
| 7. Emotion lability/negativity (mid) | -- | .41*** | −.50*** | .74*** | .47*** | .40*** | |||||
| 8. Disruptive beh. symptoms (mid) | -- | −.34** | .37*** | .44*** | .39*** | ||||||
| 9. Emotion regulation (post) | -- | −.67*** | −.32** | −.24* | |||||||
| 10. Emotion lability/negativity (post) | -- | .66*** | .50*** | ||||||||
| 11. Disruptive beh. symptoms (post) | -- | .62*** | |||||||||
| 12. Clinician severity report (post) | -- |
Note. N = 89.
p<.10
p<.05
p<.01
p<.001.
Regressions
Hierarchical regressions were conducted to determine whether emotion coaching predicted children's post-treatment ODD symptoms after controlling for pre-treatment ODD symptoms, and to test whether pre-treatment emotion lability/negativity moderated effects of emotion coaching. On step 1, child age, the pre-treatment score (maternal report when predicting maternal report; clinician severity report when predicting clinician severity report), and pre-treatment emotion lability/negativity were entered. Child sex was also controlled in analyses predicting maternal symptom reports. On step 2, the emotion coaching composite was entered. Results are presented in Table 3. The pre-treatment emotion coaching composite was not a significant predictor on step 2 in either model, both ps > .60.
Table 3.
Standard Coefficients and Standard Errors for Predictors of Child Treatment Outcomes
| Step and Variable | Disruptive behavior | Clinician severity report | ||||
|---|---|---|---|---|---|---|
| B | SE B | β | B | SE B | β | |
| Step 1: | ||||||
| Child age | .10 | .15 | .07 | .18 | .13 | .16 |
| Child sex | 1.72 | .54 | .33** | |||
| Pre-treatment score | .18 | .18 | .12 | .32 | .23 | .16 |
| Lability/negativity (pre-treatment) | .64 | .83 | .09 | .66 | .66 | .11 |
| Step 2: | ||||||
| Emotion coaching composite (pre-treatment) | −.06 | .12 | −.05 | −.03 | .10 | −.03 |
| Step 3: | ||||||
| Interaction of emotion coaching and lability/negativity | −.70 | .31 | −.23* | −.52 | .26 | −.21* |
Note.
N = 89.
β = standardized beta weight.
p<.05
p<.01
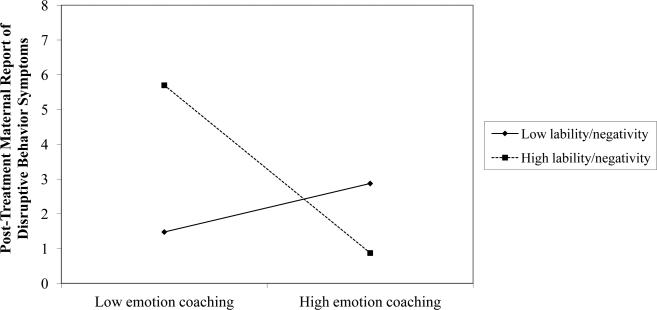
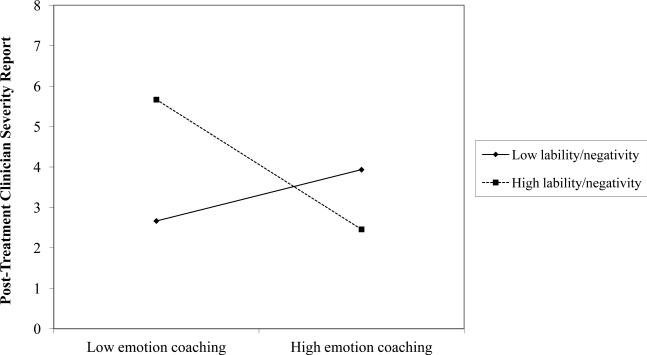
On step 3, the interaction term of emotion coaching with pre-treatment emotion lability/negativity was entered. Mothers’ emotion composite interacted with children's emotion lability/negativity to predict both maternal reports of children's post-treatment disruptive behavior (omnibus F(6, 82) = 3.82, p = .002, omnibus R2 = .22, ΔR2 = .05; for the interaction effect β = −.23, p = .025) and post-treatment clinician severity reports (omnibus F(5, 83) = 2.66, p = .028, omnibus R2 = .14, ΔR2 = .04; for the interaction effect β = −.21, p = .047). Simple slopes for each interaction are shown in Figures 1 (disruptive behavior) and 2 (clinician severity report). Covariates were controlled when calculating simple slopes.
Figure 1.
Mothers’ Report of Disruptive Behavior Symptoms at Post-Treatment as a Function of Pre-Treatment Emotion Coaching and Lability/Negativity
As Figure 1 shows, when children were high in emotion lability/negativity, those with mothers higher in emotion coaching at pre-treatment had lower disruptive behavior reports at post-treatment (β = −.39, p = .035). When children were low in emotion lability/negativity, mothers’ engagement in emotion coaching at pre-treatment had little effect on children's disruptive behavior at post-treatment (β = .11, p = .423).
As Figure 2 shows, when children were high in emotion lability/negativity, clinician severity reports at post-treatment tended to be lower for children of mothers higher in emotion coaching (β = −.26, p = .090). When children were low in emotion lability/negativity, there was little association between mothers’ emotion coaching and clinician severity reports at post-treatment (β = .10, p = .384)
Figure 2.
Clinician Severity Reports at Post-Treatment as a Function of Pre-Treatment Emotion Coaching and Lability/Negativity
Indirect associations
Indirect associations of pre-treatment emotion coaching with post-treatment child ODD symptoms, via mid-treatment emotion regulation, were tested using Preacher and Hayes’ (2008) SAS macro to bootstrap the estimate of the indirect effect. The number of bootstrapped resamples was set to 1,000. Children's age, pre-treatment scores and emotion lability/negativity were controlled. Children's sex was also controlled for maternal reports of disruptive behavior symptoms. There was no evidence for any indirect effect of emotion coaching on children's post-treatment ODD symptoms through mid-treatment emotion regulation, as all 95% confidence intervals included zero.
Discussion
The purpose of this study was to determine whether mothers’ emotion coaching predicts treatment outcomes in children with ODD. We expected mothers’ emotion coaching at pre-treatment to be both directly and indirectly (through mid-treatment emotion regulation) associated with children's fewer symptoms at post-treatment. We also expected that for children higher in emotion lability/negativity, associations of maternal emotion coaching with child symptoms would be stronger.
Assessment of Hypotheses
Direct and indirect associations
Contrary to expectation, maternal emotion coaching was unrelated to children's disruptive behavior symptoms at post-treatment. Also contrary to expectation, mothers’ emotion coaching at pre-treatment was not associated with child emotion regulation at mid-treatment. Indeed, the limited association of emotion coaching with emotion regulation – only mid-treatment emotion regulation was significantly correlated with emotion coaching – was surprising given the suggestion of bidirectionality between parental emotion coaching and child emotion regulation in extant literature. Furthermore, emotion regulation at mid-treatment was not significantly correlated with post-treatment ODD symptoms. Perhaps not surprisingly, then, the hypothesis that emotion coaching would be indirectly associated with child post-treatment ODD symptoms through mid-treatment emotion regulation was not supported. These findings contrast with previous research showing such indirect associations for emotion coaching through emotion regulation with aggression (Ramsden & Hubbard, 2002) and, longitudinally, with externalizing behavior (Cunningham et al., 2009; boys only). These findings are also in seeming contrast to earlier work with this sample at pre-treatment showing concurrent indirect associations of maternal emotion coaching with child internalizing symptoms and adjustment via emotion regulation.
It is possible that our reliance on parent report to assess children's emotion regulation was not precise enough to capture change over the course of treatment, thereby limiting the possibility of finding indirect associations. Zeman, Klimes-Dougan, Cassano and Adrian (2007) recommend integrating multiple methods to measure emotion regulation, including measurement of physiological arousal and observation of facial and behavioral responses to emotion-eliciting situations. However, the Emotion Regulation Checklist is well-used, and indeed was used in the studies cited above that showed indirect links of emotion coaching to aggression and externalizing behavior via emotion regulation. In our sample, though, the internal consistency of the emotion regulation subscale was lower than in previous work.
It is also possible that emotion regulation processes operate differently for children with ODD compared with typically-developing children. From late childhood to adolescence, it is developmentally typical to see heightened responsiveness to emotional stimuli and increased lability of both positive and negative emotions outpace slower-developing maturation in regulation. This pattern is heightened for youth with externalizing disorders, who show under-regulation not only of anger but also of high intensity, approach-related positive emotions (Gilbert, 2012).
Perhaps mechanisms other than child emotion regulation link emotion coaching with treatment outcomes for children with ODD. For example, an integral aspect of emotion coaching is parents’ awareness and validation of their child's perspective. Entering treatment with this stance would promote treatment response. For CPS, sensitivity to children's perspective would help parents identify cognitive distortions and attributional errors that may contribute to children's oppositional behavior. For PMT, sensitivity to children's perspective would help parents select meaningful contingencies and observe children's behavioral cues foreshadowing escalation or reduction of oppositionality. In general, this stance might help parents be more receptive to treatment strategies because they would be more aware of both their child's negative emotional experiences and the detrimental consequences of the oppositional behavior.
Emotion lability/negativity as a moderator
Finally, the hypothesis that effects of emotion coaching on post-treatment disruptive behavior symptoms would be stronger for children high in lability/negativity was supported for both clinician and maternal reports. This is consistent with earlier work with this sample at pre-treatment showing a concurrent negative association of child externalizing symptoms with maternal emotion coaching for children high in emotion lability/negativity. Our extension of this work to post-treatment ODD symptoms is critical in showing that emotion coaching predicts greater positive change over the course of treatment for children with ODD who are more at risk due to their emotion lability/negativity. These children may be in greater need of emotion coaching because of their intense, frequent, and rapidly changing experience of negative emotions. Moreover, these frequent experiences may provide more opportunities for parents to effectively emotion coach, and, in turn, children's difficulties in managing frequent and intense negative emotions may make them more receptive to parents’ emotion coaching. Children with ODD who are low in emotion lability/negativity may show less of the irritability dimension of ODD symptomatology and more of the hurtful dimension (Stringaris & Goodman, 2009), with a more cold and strategic pattern of oppositional behavior. If so, emotion coaching might have little effect for these children because their actions are goal-driven and not related to difficulty managing emotions.
Strengths, Limitations, and Future Directions
We note three strengths of this study. First, we address associations of emotion coaching with post-treatment ODD symptoms in a clinical sample. To our knowledge, we are the first to do so. Controlling for pre-treatment symptoms and following families longitudinally across treatment allows a stronger statement about the role of emotion coaching in treatment response for children with ODD. Second, our reliance on both maternal and clinician report provides greater confidence that results reflect changes in children's oppositional behavior rather than simply reporter effects. Third, our measures of emotion coaching relied on both mothers’ beliefs regarding emotions and observations of mothers’ behaviors. Using multiple methods to assess emotion coaching was especially important for this sample, for which displaying emotion coaching may be more difficult because of the symptoms characteristic of ODD.
We also note that our composite measure of emotion coaching included both positive and negative emotions. Despite the salience of negative emotions, especially for children with ODD, parents’ encouragement of positive emotions may be important for healthy child and family functioning. Expression of positive emotions contributes to a positive family climate, which is associated with children's better emotion regulation (Fosco & Grych, 2013). Only recently has the study of emotion socialization begun to address positive as well as negative emotions, with some taking the approach of testing for unique contributions of socialization of positive emotions compared with socialization of negative emotions (i.e., Lunkenheimer et al., 2007). We chose instead to calculate the emotion coaching composite so that a single index might reflect both extent of coaching-related beliefs and behaviors for each valence of emotion, and breadth of coaching-related beliefs and behaviors for both valences. Future research might expand this approach by examining granularity of emotion coaching. Granularity, or greater use of differentiated, discrete emotion concepts, is related to emotion regulation (Feldman Barrett, Gross, Christenson, & Benvenuto, 2001) and more effortful cognitive processing (Tugade, Fredrickson, & Feldman Barrett, 2004).
Our reliance solely on parent report to measure children's emotion regulation is a limitation of the current study. Because emotion regulation and lability/negativity are related to the occurrence of disruptive behavior symptoms, it is particularly important to have robust, distinct measures in order to differentiate the complex relations among these constructs. We note, also, the low internal consistency of the emotion regulation subscale compared with previous research, which further limited this measurement. Future research including other methods to assess emotion regulation, such as physiological arousal, facial expressions, and behavioral responses to emotion-eliciting situations, may be useful in determining whether emotion regulation mediates treatment response for ODD and whether emotion regulation serves as a mechanism for the effects of maternal emotion coaching for children with ODD. Another potential limitation was our focus on oppositional behavior symptoms as the outcome measure. Though oppositional behavior symptoms are the focus of treatment for ODD, future work might take a more holistic approach by including outcomes related to positive social functioning.
In future work, we plan to address ways to augment treatment for childhood disruptive behavior disorders by including parent training in emotion coaching. Parent interventions such as Tuning in to Kids have shown meaningful improvements in parents’ awareness and understanding of children's emotions and emotion coaching behaviors (Havighurst, Wilson, Harley, & Prior, 2009; Havighurst, Wilson, Harley, Prior & Kehoe, 2010) and decreases in dismissing beliefs and behaviors regarding children's emotions (Kehoe, Havighurst, & Harley, 2013; Wilson, Havighurst, & Harley, 2012). Reductions in child problem behaviors (Havighurst et al., 2009, 2010) and internalizing symptoms (Kehoe et al., 2013) are also seen. To date, much of the research with such programs has focused on community samples rather than clinical populations. Combining intervention approaches for parental emotion coaching with evidence-based treatment programs for disruptive behavior disorders may improve children's outcomes. Second, we plan to investigate potential mechanisms for the effect of emotion coaching on treatment outcomes, including child emotion-related skills, parent emotion-related styles and competencies, and quality of the parent-child relationship.
Conclusion
Results suggest that when children with ODD experience more frequent, intense, and unstable emotions, families are better able to benefit from treatment and reduce children's behavior problems when mothers begin treatment already engaging in emotion coaching. We did not find support for indirect associations between emotion coaching and child post-treatment ODD symptoms through emotion regulation. Identifying mechanisms for the long-term effects of emotion coaching on children's pathways of later adjustment is an important area for future research. Research addressing interventions promoting emotion coaching in combination with evidence-based treatment for disruptive behavior disorders may be useful both in increasing the understanding of typical and atypical patterns of social development and in helping improve the well-being of families and children dealing with disruptive behavior.
Acknowledgments
Funding was provided by R01 MH076141 from NIMH and by the Institute for Society, Culture, and Environment at Virginia Tech. We express appreciation to Stephen Brown and Lisa Buonomano for leading coding teams and to Lauren Catalano, Maria Cowart, Karla Delgado, Jack DiTripani, Stephanie Giunta, Lacy Grindstaff, Philip Grubbs, Michelle Hendrickson, Shelmeshia Hill, Justin Jordan, Angelica Melvin, Erin Pennington, Maggie Schwab, Hailey Vinchiarello, Shiqi Wang, and Jasmine Williams for assistance with coding. We are also appreciative to Kaushal Amatya, Kristy Benoit Allen, Kristin Austin, Kristin Canavera, Natoshia Cunningham, Maria Fraire, Marshaun Glover, Thorhildur Halldorsdottir, Matthew Jarrett, Krystal Lewis, Ryoichi Noguchi, Maria Whitmore, and Jennifer Wolff for their roles in assessment and treatment of participating children in this project. We are grateful to the families who participated in this research.
Contributor Information
Julie C. Dunsmore, Department of Psychology, Virginia Tech
Jordan A. Booker, Department of Psychology, Virginia Tech
Thomas H. Ollendick, Child Study Center, Department of Psychology, Virginia Tech
Ross W. Greene, Child Study Center, Department of Psychology, Virginia Tech.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5th ed American Psychiatric Association; Arlington, VA: 2013. [Google Scholar]
- Anderson SR, Ollendick TH. Diagnosing Oppositional Defiant Disorder using the Anxiety Disorders Interview Schedule for DSM-IV: Parent version and the diagnostic interview schedule for children. Journal of Psychopathology and Behavioral Assessment. 2012;34:467–475. doi: 10.1007/s10862-012-9294-5. [Google Scholar]
- Barkley RA. Defiant children: A clinician's manual for assessment and parent training. Guilford Press; New York: 1997. [Google Scholar]
- Cohen P, Cohen J, Kasen S, Velez CN, Hartmark C, Johnson J, Streuning EL. An epidemiological study of disorders in late childhood and adolescence—I. Age-and gender-specific prevalence. Journal of Child Psychology and Psychiatry. 1993;34:851–867. doi: 10.1111/j.1469-7610.1993.tb01094.x. doi: 10.1111/j.1469-7610.1993.tb01094.x. [DOI] [PubMed] [Google Scholar]
- Cole PM, Martin SE, Dennis TA. Emotion regulation as a scientific construct: Methodological challenges and directions for child development research. Child Development. 2004;75:317–333. doi: 10.1111/j.1467-8624.2004.00673.x. doi: 10.1111/j.1467-8624.2004.00673.x. [DOI] [PubMed] [Google Scholar]
- Cunningham J, Kliewer W, Garner P. Emotion socialization, child emotion understanding and regulation, and adjustment in urban African American families: Differential associations across child gender. Development and Psychopathology. 2009;21:261–283. doi: 10.1017/S0954579409000157. doi: 10.1017/S0954579409000157. [DOI] [PubMed] [Google Scholar]
- Dunsmore JC, Booker JA, Ollendick TH. Parental emotion coaching and child emotion regulation as protective factors for children with Oppositional Defiant Disorder. Social Development. 2013;22:444–466. doi: 10.1111/j.1467-9507.2011.00652.x. doi: 10.1111/j.1467-9507.2011.00652.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunsmore JC, Halberstadt AG. How does family emotional expressiveness affect children's schemas? In: Barrett KC, Damon W Editor-in-Chief, editors. The communication of emotion: Current research from diverse perspectives. New Directions for Child Development. Vol. 77. Jossey Bass; San Francisco: 1997. pp. 45–68. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Fabes RA, Guthrie IK, Reiser M. Dispositional emotionality and regulation: Their role in predicting quality of social functioning. Journal of Personality and Social Psychology. 2000;78:136–157. doi: 10.1037//0022-3514.78.1.136. doi: 10.1037/0022-3514.78.1.136. [DOI] [PubMed] [Google Scholar]
- Eyberg SM, Nelson MM, Boggs SR. Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. Journal of Clinical Child & Adolescent Psychology. 2008;37:215–237. doi: 10.1080/15374410701820117. doi: 10.1080/15374410701820117. [DOI] [PubMed] [Google Scholar]
- Feldman Barrett L, Gross J, Christenson TC, Benvenuto M. Knowing what you're feeling and knowing what to do about it: Mapping the relation between emotion differentiation and emotion regulation. Cognition and Emotion. 2001;15:713–724. doi: 10.1080/02699930143000239. [Google Scholar]
- Flett GL, Blankstein KR, Bator C, Pliner P. Affect intensity and self-control of emotional behaviour. Personality and Individual Differences. 1989;10:1–5. doi: 10.1016/0191-8869(89)90169-4. [Google Scholar]
- Forgatch MS, Patterson GR. Parent management training—Oregon model: an intervention for antisocial children and adolescents. In: Weisz JR, Kazdin AE, editors. Evidence-based psychotherapies for children and adolescents. The Guilford Press; New York: 2010. pp. 159–178. [Google Scholar]
- Fosco GM, Grych JH. Capturing the family context of emotion regulation: A family systems model comparison approach. Journal of Family Issues. 2013;34:557–578. doi: 10.1177/0192513X12445889. [Google Scholar]
- Gilbert KE. The neglected role of positive emotion in adolescent psychopathology. Clinical Psychology Review. 2012;32:467–481. doi: 10.1016/j.cpr.2012.05.005. doi: 10.1016/j.cpr.2012.05.005. [DOI] [PubMed] [Google Scholar]
- Gottman JM, Katz LF, Hooven C. Parental meta-emotion philosophy and the emotional life of families: Theoretical models and preliminary data. Journal of Family Psychology. 1996;10:284–291. doi: 10.1037/0893-3200.10.3.243. [Google Scholar]
- Gottman JM, Katz LF, Hooven C. Meta-emotion: How families communicate emotionally. Lawrence Erlbaum Associates; Mahwah, N.J: 1997. [Google Scholar]
- Greene RW. The explosive child: Understanding and parenting easily frustrated, “chronically inflexible” children. Harper Collins; New York: 1998. [Google Scholar]
- Greene RW. Collaborative problem solving. In: Murrihy RC, Kidman AD, Ollendick TH, editors. Clinical handbook of assessing and treating conduct problems in youth. 2010. pp. 193–220. doi:10.1007/978-1-4419-6297-3_8. [Google Scholar]
- Greene RW, Biederman J, Zerwas S, Monuteaux MC, Goring JC, Farone SV. Psychiatric comorbidity, family dysfunction, and social impairment in referred youth with oppositional defiant disorder. American Journal of Psychiatry. 2002;159:1214–1224. doi: 10.1176/appi.ajp.159.7.1214. doi: 10.1176/appi.ajp.159.7.1214. [DOI] [PubMed] [Google Scholar]
- Greene RW, Doyle AE. Toward a transactional conceptualization of oppositional defiant disorder: Implications for assessment and treatment. Clinical Child and Family Psychology Review. 1999;2:129–148. doi: 10.1023/a:1021850921476. doi: 10.1023/A:1021850921476. [DOI] [PubMed] [Google Scholar]
- Halberstadt AG, Denham SA, Dunsmore JC. Affective social competence. Social Development. 2001;10:79–119. doi: 10.1111/1467-9507.00150. [Google Scholar]
- Halberstadt AG, Dunsmore JC, Parker AE, Beale KS, Thompson JA, Bryant A., Jr. Unpublished questionnaire. North Carolina State University; Raleigh, NC.: 2008. Parents’ beliefs about children's emotions. [Google Scholar]
- Havighurst SS, Wilson KR, Harley AE, Prior MR. Tuning in to kids: an emotion-focused parenting program—initial findings from a community trial. Journal of Community Psychology. 2009;37:1008–1023. doi: 10.1002/jcop.20345. [Google Scholar]
- Havighurst SS, Wilson KR, Harley AE, Prior MR, Kehoe C. Tuning in to kids: Improving emotion socialization practices in parents of preschool children – findings from a community trial. Journal of Child Psychology and Psychiatry. 2010;51:1342–1350. doi: 10.1111/j.1469-7610.2010.02303.x. doi: 10.1111/j.1469-7610.2010.02303.x. [DOI] [PubMed] [Google Scholar]
- Jarrett MA, Wolff JC, Ollendick TH. Concurrent validity and informant agreement of the ADHD module of the Anxiety Disorders Interview Schedule for DSM-IV. Psychopathology and Behavioral Assessment. 2007;29(3):159–168. doi: 10.1007/s10862-006-9041-x. [Google Scholar]
- Katz LF, Gottman JM. Unpublished manuscript. University of Washington; 1986. The Meta-Emotion Interview. [Google Scholar]
- Katz LF, Hunter EC. Maternal meta-emotion philosophy and adolescent depressive symptomatology. Social Development. 2007;16:343–360. doi: 10.1111/j.1467-9507.2007.00388.x. [Google Scholar]
- Katz LF, Maliken AC, Stettler NM. Parental meta-emotion philosophy: A review of research and theoretical framework. Child Development Perspectives. 2012;6:417–422. doi: 10.1111/j.1750-8606.2012.00244.x. [Google Scholar]
- Katz LF, Windecker-Nelson B. Parental meta-emotion philosophy in families with conduct-problem children: Links with peer relationships. Journal of Abnormal Child Psychology. 2004;32:385–398. doi: 10.1023/b:jacp.0000030292.36168.30. doi: 10.1023/B:JACP.0000030292.36168.30. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Understanding how and why psychotherapy leads to change. Psychotherapy Research. 2009;19:418–428. doi: 10.1080/10503300802448899. doi: 10.1080/10503300802448899. [DOI] [PubMed] [Google Scholar]
- Kehoe CE, Havighurst SS, Harley AE. Tuning in to Teens: Improving parent emotion socialization to reduce youth internalizing difficulties. Social Development. 2013 Advance online publication. doi: 10.111/sode.12060. [Google Scholar]
- Kim J, Cicchetti D, Rogosch F. A longitudinal study of emotion regulation, lability/negativity, and internalizing symptomatology in maltreated and nonmaltreated children. Child Development. 2012;84:512–527. doi: 10.1111/j.1467-8624.2012.01857.x. doi: 10.1111/j.1467-8624.2012.01857.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeber R, Burke JD, Lahey BB, Winters A, Zera M. Oppositional defiant and conduct disorder: A review of the past 10 years, part I. Journal of the American Academy of Child Psychiatry. 2000;39:1468–1484. doi: 10.1097/00004583-200012000-00007. doi: 10.1097/00004583-200012000-00007. [DOI] [PubMed] [Google Scholar]
- Lunkenheimer ES, Shields AM, Cortina KS. Parental emotion coaching and dismissing in family interaction. Social Development. 2007;16:232–248. doi: 10.1111/j.1467-9507.2007.00382.x. [Google Scholar]
- Murrihy RC, Kidman AD, Ollendick TH. Clinical handbook of assessing and treating conduct problems in youth. Springer; New York: 2010. [Google Scholar]
- Nock MK. Progress review of the psychosocial treatment of child conduct problems. Clinical Psychology: Science and Practice. 2003;10:1–28. doi: 10.1093/clipsy.10.1.1. [Google Scholar]
- Ollendick TH, Greene RW, Fraire MG, Austin KE, Halldorsdottir T, Allen KB, Jarrett MA, Lewis KM, Whitmore MJ, Wolff JG. Parent Management Training (PMT) and Collaborative & Proactive Solutions (CPS) in the treatment of Oppositional Defiant Disorder in youth: A randomized control trial. 2014. Manuscript submitted for publication.
- Ollendick TH, King NJ. Evidence-based treatments for children and adolescents: Issues and controversies. In: Kendall PC, editor. Child and adolescent therapy: Cognitive-behavioral procedures. Guilford Publications; New York: 2012. pp. 499–519. [Google Scholar]
- Pelham WE, Jr., Gnagy EM, Greenslade KE, Milich R. Teacher ratings of DSM-III-R symptoms for the disruptive behavior disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 1992;31:210–218. doi: 10.1097/00004583-199203000-00006. doi: 10.1097/00004583-199203000-00006. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. doi: 10.3758/BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- Ramsden SR, Hubbard JA. Family expressiveness and parental emotion coaching: Their role in children's emotion regulation and aggression. Journal of Abnormal Child Psychology. 2002;30:657–667. doi: 10.1023/a:1020819915881. doi: 10.1023/A:1020819915881. [DOI] [PubMed] [Google Scholar]
- Shields A, Cicchetti D. Emotion regulation among school-age children: The development and validation of a new criterion Q-sort scale. Developmental Psychology. 1997;33:906–916. doi: 10.1037//0012-1649.33.6.906. doi: 10.1037/0012-1649.33.6.906. [DOI] [PubMed] [Google Scholar]
- Shields A, Cicchetti D. Reactive aggression among maltreated children: The contributions of attention and emotion dysregulation. Journal of Clinical Child Psychology. 1998;27:381–395. doi: 10.1207/s15374424jccp2704_2. doi: 10.1207/s15374424jccp2704_2. [DOI] [PubMed] [Google Scholar]
- Shortt JW, Stoolmiller M, Smith-Shine JN, Eddy JM, Sheeber L. Maternal emotion coaching, adolescent anger regulation, and siblings’ externalizing symptoms. Journal of Child Psychology and Psychiatry. 2010;51:799–808. doi: 10.1111/j.1469-7610.2009.02207.x. doi; 10.1111/j.1469-7610.2009.02207.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. Anxiety Disorders Interview Schedule for DSM-IV.: Parent interview schedule (Vol. 1) Oxford University Press; 1996. [Google Scholar]
- Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with the anxiety disorders interview schedule for DSM-IV: Child and parent versions. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:937–944. doi: 10.1097/00004583-200108000-00016. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- Stocker CM, Richmond MK, Rhoades GK, Kiang L. Family emotional processes and adolescents' adjustment. Social Development. 2007;16:310–325. doi: 10.1111/j.1467-9507.2007.00386.x. [Google Scholar]
- Stringaris A, Goodman R. Three dimensions of oppositionality in youth. Journal of Child Psychology and Psychiatry. 2009;50:216–223. doi: 10.1111/j.1469-7610.2008.01989.x. doi: 10.1111/j.1469-7610.2008.01989.x. [DOI] [PubMed] [Google Scholar]
- Stringaris A, Maughan B, Goodman R. What's in a disruptive disorder? Temperamental antecedents of oppositional defiant disorder: findings from the Avon longitudinal study. Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49:474–483. doi: 10.1097/00004583-201005000-00008. doi: 10.1016/j.jaac.2010.01.021. [DOI] [PubMed] [Google Scholar]
- Tugade MM, Fredrickson BL, Feldman Barrett L. Psychological resilience and positive emotional granularity: Examining the benefits of positive emotions on coping and health. Journal of Personality. 2004;72:1161–1190. doi: 10.1111/j.1467-6494.2004.00294.x. doi: 10.1111/j.1467-6494.2004.00294.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census State and county quickfacts: Virginia. 2012 Jun; Retrieved from U.S. Census website http://quickfacts.census.gov/qfd/states/51000.html.
- Webster-Stratton C, Reid MJ. The Incredible Years parents, teachers, and children training series: A multifaceted treatment approach for young children with conduct disorders. In: Weisz JR, Kazdin AE, editors. Evidence-based psychotherapies for children and adolescents. 2nd ed. Guilford Press; New York: 2010. pp. 194–210. [Google Scholar]
- Wilson KR, Havighurst SS, Harley AE. Tuning in to Kids: An effectiveness trial of a parenting program targeting emotion socialization of preschoolers. Journal of Family Psychology. 2012;26:56–65. doi: 10.1037/a0026480. doi: 10.1037/a0026480. [DOI] [PubMed] [Google Scholar]
- Zeman J, Cassano M, Perry-Parrish C, Stegall S. Emotion regulation in children and adolescents. Journal of Developmental and Behavioral Pediatrics. 2006;27:155–168. doi: 10.1097/00004703-200604000-00014. doi: 10.1097/00004703-200604000-00014. [DOI] [PubMed] [Google Scholar]
- Zeman J, Klimes-Dougan B, Cassano M, Adrian M. Measurement issues in emotion research with children and adolescents. Clinical Psychology: Science and Practice. 2007;14:377–401. doi: 10.1111/j.1468-2850.2007.00098.x. [Google Scholar]