Abstract
Background
Obesity in childhood is related to multiple lifestyle factors. Our objective was to evaluate the relationship between consumption of 100% fruit juice and weight status over time among preschool children.
Methods
We used linear and logistic multivariable regression to evaluate body mass index (BMI) z-score and overweight/obese status as a function of 100% fruit juice intake for 8,950 children examined at ages 2, 4, and 5 years as part of the Early Childhood Longitudinal Study–Birth Cohort, a representative sample of the United States.
Results
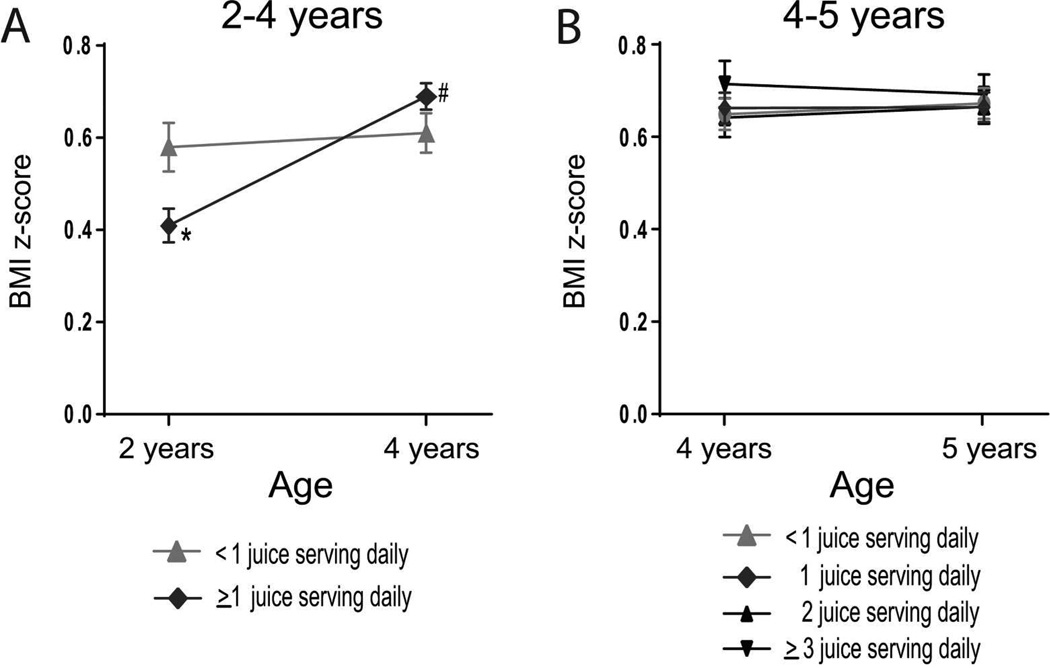
Cross-sectional analysis at ages 2, 4, and 5 years showed no difference in the prevalence of overweight and obesity between consistent juice drinkers and inconsistent/non-drinkers. Longitudinal analysis found that children who drank 100% juice consistently at age 2 years had greater increases in BMI z-score by age 4 years than infrequent/non-drinkers (p<0.0001), a difference driven by lesser increases in height z-score (p=0.0003) and slightly greater increases in weight z-score (p=0.0550) among consistent juice drinkers over the 2 to 4 year time period. Additionally, consistent juice drinkers at age 2 had higher odds of becoming overweight by age 4 (adjusted odds ratio 1.30; CI 1.06–1.60). These differences in growth parameters were not noted between ages 4 and 5 years.
Conclusions
Drinking 100% fruit juice regularly at age 2 is associated with higher odds of becoming overweight between 2 and 4 years. Pediatricians and parents can discourage excessive fruit juice consumption as part of a larger effort to avoid unhealthy gain in BMI in young children.
Keywords: fruit juice, weight gain, obesity, preschool, sugar
INTRODUCTION
Childhood obesity is a worsening problem in the United States, leading to a focus on individual health habits associated with unhealthy weight gain, such as television viewing (1,2), soft drink consumption (3,4) and lack of exercise (5,6). In recent years, 100% fruit juice consumption has been questioned as another high-calorie, high-sugar food increasing likelihood of obesity in preschoolers (7).
The American Academy of Pediatrics (AAP) recommends limiting juice to 4–6 ounces per day for children ages 1–6 years (8), but no strong studies directly related to weight gain currently back this recommendation among preschool children. Previous studies linking fruit juice consumption to weight gain are mixed. One cross-sectional study of preschool-aged children concluded that drinking >12 oz/day of juice was associated with a greater likelihood of both obesity and short stature (9). Several longitudinal studies in response to this controversial paper found either no statistically significant correlation between childhood BMI or height and fruit juice consumption or only associations among children who were already overweight (10–13). However, these previous studies all either had small sample sizes or drew only from regional or specialized populations. Thus, the association of juice consumption and unhealthy weight gain is unclear.
Our goal was to evaluate longitudinal relationships between 100% fruit juice consumption and changes in early childhood height, weight, and BMI in 2–5 year-old children followed as part of the Early Childhood Longitudinal Study, Birth Cohort (ECLS-B), a prospective, representative survey of \ children born in the US in 2001. We assessed whether regular juice intake at ages 2 and 4 years predicted the development of overweight/obesity over 2–3 years of longitudinal follow-up. Our hypothesis was that compared to infrequent/non-drinkers, higher juice intake would be associated with higher gains in BMI-z-score over time.
METHODS
Data set
The ECLS-B is a large, multi-source, multi-method study sponsored by the National Center for Education Statistics (NCES; US Department of Education) to examine health and lifestyle influences on early childhood experiences (14,15). The NCES ethics review board approved the study. Greater than 14,000 birth certificates from 2001 were randomly sampled to create a nationally representative cohort. Approximately 10,700 parents gave informed consent and completed interviews, a 77% response rate. We evaluated data from 2, 4 and 5 years, enabling prospective analysis.
Measures
During the evaluations at ages 2, 4 and 5 years, parents were interviewed at home by trained assessors. The primary caregiver (the biological mother in 97.3% of survey respondents in the 2 year-old wave) completed a computer-assisted interview. Juice intake was assessed by parental responses to several questions. At the 2-year visit, parents were asked what beverages their child usually drinks with meals: choices were milk, 100% juice, sodas, water, coffee/tea, none, or other, and were asked to check all that apply. Parents were also asked what their child usually drinks between meals or before bedtime, with the same options. For the 2-year visit, children described as drinking juice at/between meals were categorized as regular drinkers, while children not described as drinking juice at meals/ between meals were non-drinkers.. At the 4- and 5-year visits, parents were more specifically asked: “During the past 7 days, how many times did your child drink 100% fruit juices such as orange juice, apple juice, or grape juice? Do not include punch, Sunny Delight, Kool-Aid, sports drinks, or other fruit-flavored drinks.” Categories included: no intake during the past 7 days, 1–3 times during the past 7 days, 4–6 times during the past 7 days, once daily, twice daily, three times daily, and four or more times daily. One serving was quantified as 8 oz and was described for parents as the size of a half-pint milk carton. Quantities were converted to <1 serving daily and ≥1 serving daily, as well as into categories of no juice, juice at snack only, juice at dinner only and juice at both snack and dinner.
As described previously (3), direct measurements of height and weight were obtained by trained researchers using standardized protocols and equipment and converted to age- and gender-specific percentiles and z-scores using the 2000 Centers for Disease Control growth charts and SAS code (16). Weight categories were normal weight (<85th%), overweight (85th%–<95th%), and obese (≥95th%). For BMI analyses,, children <24 months old were excluded, as BMI is not a validated measure below this age. Maternal weight was directly measured at each wave, and mothers reported their height; from these BMI was calculated and categorized as normal weight (<25 kg/m2), overweight (25–<30), and obese (≥30).
Parents identified their child’s gender and race/ethnicity (white, black, Asian, Hispanic, and other). NCES determined quintiles of socio-economic status (lowest SES = 1; highest SES = 5) based on family income, maternal education, maternal occupation, paternal education, and paternal occupation.
Data analysis
We performed all analyses using SAS software, V.9.4 (SAS Institute Inc., Cary, NC,), utilizing survey procedures with sampling weights provided by the NCES to account for the complex sampling design. This accounts for over-sampling of certain groups and for drop-out/non-response, allowing the data to be representative of all children born in the US in 2001. All statistical significance tests were two-sided with a significance level of α=0.05. Criteria for multiple comparison correction were considered and did not apply. Unweighted sample sizes were rounded to the nearest 50 in compliance with NCES rules. Using multivariable linear regression models, we performed both cross-sectional and longitudinal analyses. First we regressed: (i) age 2-year BMI-z-score with consumption of juice versus no juice cross-sectionally; (ii) age 4- and 5-year BMI-z-score with amount of juice consumption cross-sectionally; (iii) longitudinal change in BMI-z-score (i.e., 2-year BMI-z-score subtracted from 4-year BMI-z-score, and 4-year BMI-z-score subtracted from 5-year BMI-z-score) with amount of juice consumption; (iv) longitudinal change in height-z-score with juice; and (v) longitudinal change in weight-z-score with amount of juice consumed. Similarly, multivariable logistic regression models were used to examine: (i) the odds of overweight/obese across the quantities of juice consumption in cross-sectional analyses; and (ii) the odds of becoming overweight/obese between 2–4 years and 4–5 years for children who were normal weight at baseline and were consistent drinkers of juice vs. infrequent/non-drinkers in longitudinal analyses. In evaluating longitudinal changes in BMI-z-score, we used baseline juice drinking status as performed previously (17) to minimize reverse causality. All longitudinal and cross-sectional multivariable models, including adjusted mean values of anthropometric measures, were adjusted for sex, race, SES, and maternal BMI, given the possible influence on weight and/or juice consumption. Longitudinal analyses of changes in height, weight and BMI-z-score were further adjusted for baseline z-score. We used χ2 tests to determine differences in proportions of juice drinkers by participant characteristics.
RESULTS
Demographics
We analyzed data from 10,700 ECLS-B participants. Of these, 8,950 participants at the 2-year evaluation were ≥24 months and had complete data on juice intake. At the 4- and 5-year evaluations, 8,400 children and 6,250 children had complete data on juice intake, respectively. Overall demographic statistics are shown in Table 1. Juice consumption was high at all ages but tended to decrease as children got older, with about 72% of 2-year-olds drinking juice regularly and about 60% of 5-year-olds drinking juice greater than or equal to one serving daily. Consumption varied significantly by race/ethnicity, with higher rates of regular juice consumption among non-Hispanic-black children and Hispanic children at all ages studied (p<0.0001). Regular juice consumption also varied significantly by SES with higher rates among the lowest SES group at all ages (p<0.0001). Children who drank juice regularly at age 2 were less likely to drink milk regularly (adjusted odds ratio 0.79, confidence interval 0.65, 0.96).
TABLE 1.
Descriptive Statistics Overall and by Juice Intake
| Variable | 2-year-olds | 4-year-olds | 5-year-olds | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total Na (weighted %b) |
Juice Consumption (%) | Total Na (weighted %b) |
Juice Consumption (%) | Total Na (weighted %b) |
Juice Consumption (%) | |||||
| Nod | Yesd | <1e | ≥1d | <1e | ≥1d | |||||
| Gender | ||||||||||
| Male | 4550 (51.2) | 28.5 | 71.5 | 4250 (51.3) | 33.8 | 66.2 | 3150 (51.2) | 40.3 | 59.7 | |
| Female | 4350 (48.8) | 27.6 | 72.4 | 4100 (48.7) | 31.7 | 68.3 | 3100 (48.8) | 39.6 | 60.4 | |
| p valuec | 0.5068 | 0.1256 | 0.7090 | |||||||
| Weight Status | ||||||||||
| Normal Weight | 5200 (67.5) | 27.7 | 72.3 | 5550 (64.0) | 33.4 | 66.6 | 4200 (64.8) | 40.0 | 60.0 | |
| Overweight | 1100 (15.6) | 28.4 | 71.6 | 1350 (17.6) | 31.6 | 68.4 | 1050 (17.9) | 42.9 | 57.1 | |
| Obese | 1100 (16.9) | 31.3 | 68.7 | 1300 (18.4) | 30.7 | 69.3 | 950 (17.3) | 37.0 | 63.0 | |
| p valuec | 0.1888 | 0.3108 | 0.1499 | |||||||
| Race/Ethnicity | ||||||||||
| White | 3800 (53.6) | 32.2 | 67.8 | 3650 (53.7) | 38.4 | 61.6 | 2600 (53.7) | 46.5 | 53.5 | |
| Black | 1400 (13.7) | 20.3 | 79.7 | 1300 (13.9) | 25.5 | 74.5 | 1000 (13.9) | 27.9 | 72.1 | |
| Hispanic | 1800 (25.3) | 23.0 | 77.0 | 1650 (25.2) | 23.7 | 76.3 | 1250 (25.3) | 30.8 | 69.2 | |
| Asian | 900 (2.7) | 32.2 | 67.9 | 850 (2.6) | 36.0 | 64.0 | 650 (2.7) | 45.4 | 54.6 | |
| Other | 1000 (4.8) | 28.5 | 71.5 | 950 (4.6) | 37.7 | 62.3 | 750 (4.5) | 47.4 | 52.6 | |
| p valuec | <0.0001 | <0.0001 | <0.0001 | |||||||
| Socio-economic status | ||||||||||
| High (5) | 1900 (20.7) | 35.4 | 64.6 | 1950 (20.0) | 37.6 | 62.4 | 1500 (19.5) | 49.8 | 50.2 | |
| Medium high (4) | 1650 (20.6) | 30.4 | 69.6 | 1650 (20.0) | 36.4 | 63.6 | 1250 (19.9) | 44.4 | 55.6 | |
| Medium (3) | 1600 (20.1) | 27.7 | 72.3 | 1650 (20.0) | 35.1 | 64.9 | 1200 (20.9) | 40.5 | 59.5 | |
| Medium low (2) | 1550 (19.7) | 24.0 | 76.0 | 1600 (20.1) | 29.2 | 70.8 | 1200 (20.3) | 35.6 | 64.5 | |
| Low (1) | 1450 (18.9) | 24.1 | 75.9 | 1500 (19.9) | 25.5 | 74.5 | 1100 (19.4) | 29.4 | 70.6 | |
| p valuec | <0.0001 | <0.0001 | <0.0001 | |||||||
| Maternal BMI category | ||||||||||
| Normal weight | 3650 (40.2) | 28.5 | 71.5 | 3350 (38.9) | 32.7 | 67.3 | 2450 (38.5) | 39.2 | 60.8 | |
| Overweight | 2350 (28.1) | 29.2 | 70.8 | 2200 (28.3) | 31.5 | 68.6 | 1650 (28.1) | 39.7 | 60.3 | |
| Obese | 2750 (31.6) | 25.8 | 74.2 | 2650 (32.9) | 34.7 | 65.3 | 2000 (33.4) | 42.3 | 57.7 | |
| p valuec | 0.0984 | 0.2023 | 0.3086 | |||||||
All N’s are rounded to the nearest 50 in compliance with NCES rules.
All percents are weighted to the population.
X2 test comparing rates of juice consumption between groups.
Parents of 2-year-old children that were asked if there children drink juice at meals or snacks and the amount was not quantified.
Parents of 4- and 5-year-old children were asked to quantify the amount of juice consumption. Percentage is in table are split into children to drank less than 1 serving of juice daily and children who drank 1 or more servings of juice daily.
Cross-sectional analysis of 100% fruit juice and weight status among US children aged 2–5 years
Approximately one-third of the study population was classified as overweight or obese according to CDC growth chart guidelines at each time-point (Table 1). Among participants, approximately the same percentage of children with overweight and obesity drank juice regularly as participants who had normal weights (Table 1). At age 2 but not at age 4 or 5, the BMI z-score was lower for children who consistently drank juice (p<0.05). There was no difference in BMI z-score by the timing of juice consumption (snack, dinner, both—data not shown). On cross-sectional analysis, there were no differences in the odds ratios for overweight or obesity when comparing consistent drinkers and infrequent/non-drinkers at any time point (Supplementary Table 1). Similarly, there were no cross-sectional differences in the associations between juice consumption as a linear measure and z-scores for weight or height at any time-point (data not shown). Results for the above analyses were also not significant when juice at 4 and 5 years was evaluated by the total number of servings daily or as <1 vs. ≥1 serving daily.
Longitudinal changes in height, weight, and BMI-z-scores
Change in BMI-z-score over time is shown in Figures 1A–B. Children who drank juice consistently at 2 years old (vs. infrequent/non-drinkers) initially had a lower BMI-z-score at age 2 but exhibited a greater increase in BMI-z-score between 2–4 years old (Table 2). Children who did not drink juice regularly at meals or snacks at age 2 gained 0.03 units in their BMI-z-score by the time they turned 4 years old, whereas children who drank juice consistently at meals/snacks at age 2 gained 0.28 z-score units (Table 2, Figure 1; p=0.0003). Compared to non-juice drinkers (change in BMI z-score +0.166), this increase in BMI z-score was higher for those drinking juice at snacks (+0.332, p=0.002) and at meals and snacks (+0.302, p=0.005) than for those drinking juice at meals only (+0.262, p=0.057). This change in BMI-z-score was associated with differences in both the change in height-z-score and weight-z-score. Consistent juice drinkers (vs. inconsistent/non-drinkers) had less linear growth between 2–4 years, (change in height-z-score 0.31 vs. 0.41, p=0.001), while differences in the change in weight-z-score were less pronounced (change for drinkers vs. inconsistent/non-drinkers, 0.43 vs. 0.37, p=0.0550).
Figure 1. Change in BMI-z-score over time for regular juice drinkers vs. infrequent/non-drinkers.
A. BMI-z-scores at age 2 years and 4 years for children drinking ≥1 serving of juice daily (vs. <1) at age 2. B. BMI-z-scores at 4 years and 5 years for children drinking ≥1 serving of juice daily (vs. <1) at 4 years. All values adjusted for race/ethnicity, socio-economic status and maternal BMI.
# p<0.001 for longitudinal change in BMI-z for daily juice drinkers vs. non-drinkers;
* p<0.01 for cross-sectional BMI-z for daily juice drinkers vs. infrequent/non-drinkers using linear regression.
TABLE 2.
Logistic Regression - Odds of Normal-Weight Children Becoming Overweight Over Time by Juice Consumption Category (≥1 vs. <1)
| Juice | Overweight OR (CI) | P value | Obese OR (CI) | P value |
|---|---|---|---|---|
| Between Age 2 to 4 years | ||||
| Model 0 (no adjustments) | 1.28 (1.04–1.58) | 0.0179 | 1.32 (0.96–1.83) | 0.0921 |
| Model 1 (adjusted for sex, race/ethnicity, SES) | 1.24 (1.01–1.52) | 0.0378 | 1.25 (0.90–1.73) | 0.1867 |
| Model 2 (adjusted for sex, race/ethnicity, SES, BMI z-score at age 2) | 1.30 (1.06–1.59) | 0.0129 | 1.30 (0.93–1.83) | 0.1293 |
| Between Age 4 to 5 years | ||||
| Model 0 (no adjustments) | 0.90 (0.64–1.26) | 0.5420 | 0.79 (0.43–1.46) | 0.4534 |
| Model 1 (adjusted for sex, race/ethnicity, SES) | 0.85 (0.62–1.18) | 0.3435 | 0.79 (0.42–1.48) | 0.4624 |
| Model 2 (adjusted for sex, race/ethnicity, SES, BMI z-score at age 4) | 0.86 (0.63–1.16) | 0.4010 | 0.80 (0.43–1.49) | 0.4730 |
Among children who were normal weight at 2 years-old, those who consistently drank juice were more likely to become overweight but not obese from 2–4 years (OR 1.30 adjusted for sex, race/ethnicity, SES, and weight at age 2; CI 1.06–1.59, p=0.0129) (Table 3). None of these differences in growth parameters varied by juice consumption analyzed by the number of servings daily in the interval from 4 to 5 years (Figure 1B).
TABLE 3.
Adjusted Mean Change in Z-score for Height, Weight, and BMI z-Scores Between Ages 2–4 Years and 4–5 Years by Juice Consumption.
| Change in Height z-score (standard error) |
Change in Weight z-score (standard error) |
Change in BMI z-score (standard error) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| <1 serving |
≥1 serving |
p value | <1 serving |
≥1 serving |
p value | <1 serving |
≥1 serving |
p value | |
| Age 2 to 4 | |||||||||
| Model 0 (no adjustments) | 0.332 (0.027) |
0.229 (0.018) |
<0.0001 | 0.213 (0.051) |
0.314 (0.030) |
<0.0001 | 0.024 (0.056) |
0.257 (0.042) |
<0.0001 |
| Model 1 (adjusted for sex, race/ethnicity, SES) | 0.372 (0.030) |
0.252 (0.021) |
0.0004 | 0.247 (0.048) |
0.346 (0.032) |
0.0436 | 0.028 (0.057) |
0.270 (0.043) |
<0.0001 |
| Model 2 (model 1 plus maternal BMI) | 0.374 (0.031) |
0.257 (0.021) |
0.0009 | 0.247 (0.046) |
0.354 (0.031) |
0.0263 | 0.033 (0.055) |
0.279 (0.043) |
<0.0001 |
| Model 3 (model 2 plus baseline z-score) | 0.410 (0.028) |
0.308 (0.020) |
0.0010 | 0.371 (0.032) |
0.432 (0.024) |
0.0550 | 0.030 (0.037) |
0.282 (0.028) |
0.0003 |
| Age 4 to 5 | |||||||||
| Model 0 (no adjustments) | 0.037 (0.018) |
0.051 (0.015) |
0.5160 | 0.017 (0.017) |
0.002 (0.012) |
0.3772 | −0.002 (0.036) |
−0.028 (0.026) |
0.4899 |
| Model 1 (adjusted for sex, race/ethnicity, SES) | 0.027 (0.019) |
0.046 (0.015) |
0.3585 | 0.024 (0.016) |
0.004 (0.012) |
0.2333 | 0.016 (0.035) |
−0.012 (0.025) |
0.4562 |
| Model 2 (model 1 plus maternal BMI) | 0.018 (0.021) |
0.040 (0.014) |
0.3131 | 0.020 (0.016) |
0.006 (0.013) |
0.4031 | 0.018 (0.035) |
−0.006 (0.026) |
0.5219 |
| Model 3 (model 2 plus baseline BMI z-score) | 0.052 (0.020) |
0.071 (0.015) |
0.3670 | 0.042 (0.016) |
0.029 (0.012) |
0.4553 | 0.034 (0.031) |
0.020 (0.021) |
0.6778 |
DISCUSSION
Recommendations regarding fruit juice intake are frequently discussed at pediatric well-child visits, particularly when the parents or pediatrician are concerned about a child being overweight or obese (18). Often assuming that juice has the health benefits, parents may be reluctant to associate 100% fruit juice with other sweet drinks such as soft drinks, sports drinks, and other sweetened drink mixes (19). Thus, parents are often unaware of the potential relationship between juice intake and unhealthy weight gain and thus are reluctant to limit juice consumption in their child’s diet—potentially in also part because of the convenience of pre-packaged servings of juice (19,20). As parental attitudes have been ambiguous, however, so have prior studies on the association of fruit juice consumption with childhood obesity, with one study demonstrating an association of high fruit juice consumption obesity and short stature (9), multiple studies suggesting a lack of unhealthy weight gain following fruit juice consumption (10–12) and another study suggesting such weight gain only among children who were already overweight (13). Our study is unique in analyzing longitudinal and cross-sectional data of fruit juice consumption and weight status with adjustment for important potential confounders in a large, nationally representative cohort of children age 2–5 years. Our findings demonstrate that compared with infrequent/nondrinkers of 100% fruit juice, children drinking juice daily at age 2 years had a greater increase in BMI-z-score over the preschool years and had higher odds of becoming overweight. These data support our hypothesis that daily fruit juice consumption is associated with unhealthy childhood weight gain and suggest that this association is more significantly present in the early preschool years.
The benefits of eating whole fruit over fruit juice have been recognized for many years. Fruit juice contains less fiber than solid fruit, giving children less satiety (21,22). Moreover, fruit juice contains sugar as its only significant calorie source and thus may be less likely to induce satiety than drinks containing protein or fat (23,24). Of note, we found higher changes in BMI z-score among children drinking juice at snacks. After drinking 120 calories of apple juice (vs. a 120-calorie apple), children may be more likely to feel hungry and continue to snack, leading to a higher overall calorie consumption. Without adequate adjustment in energy expenditure, these excess calories could be converted to fat mass and contribute to unhealthy weight gain. (25,26) Juicing fruits typically eliminates the skin of the fruit causing loss of important nutrients and antioxidants, including flavonoids and carotenoids—associated in some studies with a lower risk of cancer (8,27,28).
In 1997, Dennison et al. (9) reported that in a study of 168 2 and 5 year-olds, excessive fruit juice consumption ≥12 fl oz/day was associated with short stature and obesity. Several papers subsequently stated that a longitudinal rather than a cross-sectional study was needed. Alexy et al. (11) in 1999 studied 205 children annually at the ages of 3, 4, and 5 years, evaluating anthropometry and dietary report. They found that growth velocity, BMI, and height-z-score were not significantly correlated with fruit juice consumption. In 2006, Faith et al. (13) evaluated the fruit juice intake and adiposity gain in 2,801 low-income children aged 1–4 years, reporting that the relationship between juice intake and adiposity gain depended on children’s initial overweight status. The association between increased juice intake and greater change in BMI-z-score was only present in those children already at risk for overweight.
We evaluated a larger, nationally-representative group than prior studies (10–13). As with Alexy, we found the cross-sectional data less compelling, with no significant association between regular juice intake defined as one or more servings per day at ages 2, 4, or 5 years and high BMI-z-score at the same age, although the odds ratios for obesity were higher as the children grew older. However, in an analysis adjusted for potential confounders, we noted a higher increase in BMI-z-score between 2–4 years old among drinkers of ≥1 serving of fruit juice per day vs <1 juice serving daily. It is interesting that those who drank juice regularly at age 2 had a lower BMI-z-score at age 2, but that over time, this cohort of consistent juice drinkers gained weight faster, surpassing the average BMI-z-score of infrequent/non-drinkers by age 4 (p<0.0001). Consistent juice intake at age 2 was also found to be associated with less growth in height, while the association of juice intake with longitudinal weight gain was attenuated following adjustment for baseline weight-z-score, with both factors contributing to the greater change in BMI-z-score among consistent juice drinkers and a 30% greater odds of becoming overweight. As was true for the study by Dennison et al., the underlying explanation for the association between juice consumption and decreased linear growth is unclear. One potential explanation is a lower amount of milk intake among juice drinkers. We recently reported from this cohort that higher milk consumption was associated with taller stature (29). Regular juice drinkers in the current study were less likely to drink larger amounts of milk at age 2 years. Unfortunately, we were not able to quantify milk consumption at age 2 years, so it remains unclear how milk consumption may relate to height gain in this age range. More research is needed to further define these relationships, particularly at a time when fruit juice perhaps makes up a large portion of the diet in this characteristically “picky” age group (30).
This study had several limitations. Fruit juice intake was based on parental report and not direct observation of intake. Additionally, the juice intake information asked on the survey for the 2-year-old assessment did not quantify higher volumes of intake—only whether children drank regularly at meals or snacks. Calculation of maternal BMI was based on heights that were reported, not measured (though weights were measured). Finally, we were limited by lack of information on physical activity or complete dietary information, making assessment of total calorie intake and caloric expenditure unavailable. Despite these points, this study had several strengths, including its longitudinal nature, its nationally representative sample, its high rate of retention, and the largest-to-date cohort of children followed from ages 2–5 years and analyzed for associations between fruit juice intake and weight gain.
CONCLUSIONS
We found in a large cohort of children followed longitudinally from ages 2–5 years that regular consumption of 100% fruit juice as a 2-year-old was associated with a greater increase in BMI-z-score over the toddler years. 2-year-old children who regularly consume fruit juice had higher odds of becoming overweight. These findings were in contrast to some previous longitudinal studies in this age range completed with smaller sample sizes. As the issue of childhood obesity comes to the forefront in national matters of health, starting children in healthy lifestyle habits from an early age should become a priority as part of a multifaceted approach to combating childhood obesity. To encourage a healthy weight in early childhood, pediatricians can encourage parents and caregivers to offer their children water instead of fruit juice or sugar-sweetened beverages as part of overall lifestyle changes. Better awareness of the contribution of liquid calories to childhood BMI may help improve the lifestyles of many children affected by the childhood obesity epidemic.
Supplementary Material
What’s Known on This Subject
Data are mixed regarding the association between consumption of 100% fruit juice and prospective weight gain in preschoolers.
What This Study Adds
Preschool children drinking 100% juice (compared to inconsistent/non-drinkers) had greater increases in BMI-z-scores and lower increases in height-z-score over a 2-year period. This supports current AAP recommendations to limit juice intake in early childhood.
Acknowledgments
Funding source: This work was supported by NIH grant 5K08HD060739-05 (MDD), Doris Duke Charitable Foundation Career Development Award (RJS).
Abbreviations
- AAP
American Academy of Pediatrics
- BMI
body mass index
- CDC
Centers for Disease Control and Prevention
- ECLS-B
Early Childhood Longitudinal Survey – Birth cohort
- NCES
National Center for Education Statistics
- SES
socio-economic status
Footnotes
Conflict of interest statement: The authors have no conflicts of interest
REFERENCES
- 1.Reilly JJ, Armstrong J, Dorosty AR, et al. Early life risk factors for obesity in childhood: cohort study. British Medical Journal. 2005;330(7504):1357–1359. doi: 10.1136/bmj.38470.670903.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wells JCK, Hallal PC, Reichert FF, et al. Sleep patterns and television viewing in relation to obesity and blood pressure: evidence from an adolescent Brazilian birth cohort. International Journal of Obesity. 2008;32(7):1042–1049. doi: 10.1038/ijo.2008.37. [DOI] [PubMed] [Google Scholar]
- 3.DeBoer MD, Scharf RJ, Demmer RT. Sugar-sweetened beverages and weight gain in 2- to 5-year-old children. Pediatrics. 2013;132(3):413–420. doi: 10.1542/peds.2013-0570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Libuda L, Kersting M. Soft drinks and body weight development in childhood: is there a relationship? Current Opinion in Clinical Nutrition and Metabolic Care. 2009;12(6):596–600. doi: 10.1097/MCO.0b013e32833189f6. [DOI] [PubMed] [Google Scholar]
- 5.Summerbell CD, Moore HJ, Voegele C, et al. Evidence-based recommendations for the development of obesity prevention programs targeted at preschool children. Obesity Reviews. 2012;13:129–132. doi: 10.1111/j.1467-789X.2011.00940.x. [DOI] [PubMed] [Google Scholar]
- 6.Vanhala M, Korpelainen R, Tapanainen P, et al. Lifestyle risk factors for obesity in 7-year-old children. Obesity Research & Clinical Practice. 2009;3(2):99–107. doi: 10.1016/j.orcp.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 7.van Grieken A, Renders CM, van de Gaar VM, et al. Associations between the home environment and children's sweet beverage consumption at 2-year follow-up: the 'Be active, eat right' study. Pediatr Obes. 2015;10(2):126–133. doi: 10.1111/ijpo.235. [DOI] [PubMed] [Google Scholar]
- 8.Baker SS, Cochran WJ, Greer FR, et al. The use and misuse of fruit juice in pediatrics. Pediatrics. 2001;107(5):1210–1213. doi: 10.1542/peds.107.5.1210. [DOI] [PubMed] [Google Scholar]
- 9.Dennison BA, Rockwell HL, Baker SL. Excess fruit juice consumption by preschool-aged children is associated with short stature and obesity. Pediatrics. 1997;99(1):15–22. [PubMed] [Google Scholar]
- 10.Skinner JD, Carruth BR, Moran J, et al. Fruit juice intake is not related to children's growth. Pediatrics. 1999;103(1):58–64. doi: 10.1542/peds.103.1.58. [DOI] [PubMed] [Google Scholar]
- 11.Alexy U, Sichert-Hellert W, Kersting M, et al. Fruit juice consumption and the prevalence of obesity and short stature in German preschool children: Results of the DONALD Study. Journal of Pediatric Gastroenterology and Nutrition. 1999;29(3):343–349. doi: 10.1097/00005176-199909000-00019. [DOI] [PubMed] [Google Scholar]
- 12.Welsh JA, Cogswell ME, Rogers S, et al. Overweight among low-income preschool children associated with the consumption of sweet drinks: Missouri, 1999–2002. Pediatrics. 2005;115(2):E223–E229. doi: 10.1542/peds.2004-1148. [DOI] [PubMed] [Google Scholar]
- 13.Faith MS, Dennison BA, Edmunds LS, et al. Fruit juice intake predicts increased adiposity gain in children from low-income families: Weight status-by-environment interaction. Pediatrics. 2006;118(5):2066–2075. doi: 10.1542/peds.2006-1117. [DOI] [PubMed] [Google Scholar]
- 14.Scharf RJ, Demmer RT, DeBoer MD. Longitudinal evaluation of milk type consumed and weight status in preschoolers. Archives of Disease in Childhood. 2013;98(5):335–340. doi: 10.1136/archdischild-2012-302941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scharf RJ, DeBoer MD. Sleep timing and longitudinal weight gain in 4- and 5-year-old children. Pediatr Obes. 2015;10(2):141–148. doi: 10.1111/ijpo.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat. 2002;11(246):1–190. [PubMed] [Google Scholar]
- 17.Qi Q, Chu AY, Kang JH, et al. Sugar-sweetened beverages and genetic risk of obesity. N Engl J Med. 2012;367(15):1387–1396. doi: 10.1056/NEJMoa1203039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krebs NF, Himes JH, Jacobson D, et al. Assessment of child and adolescent overweight and obesity. Pediatrics. 2007;120:S193–S228. doi: 10.1542/peds.2007-2329D. [DOI] [PubMed] [Google Scholar]
- 19.Bolling C, Crosby L, Boles R, et al. How Pediatricians Can Improve Diet and Activity for Overweight Preschoolers: A Qualitative Study of Parental Attitudes. Academic Pediatrics. 2009;9(3):172–178. doi: 10.1016/j.acap.2009.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Etelson D, Brand DA, Patrick PA, et al. Childhood obesity: Do parents recognize this health risk? Obesity Research. 2003;11(11):1362–1368. doi: 10.1038/oby.2003.184. [DOI] [PubMed] [Google Scholar]
- 21.Bolton RP, Heaton KW, Burroughs LF. THE ROLE OF DIETARY FIBER IN SATIETY, GLUCOSE, AND INSULIN - STUDIES WITH FRUIT AND FRUIT JUICE. American Journal of Clinical Nutrition. 1981;34(2):211–217. doi: 10.1093/ajcn/34.2.211. [DOI] [PubMed] [Google Scholar]
- 22.Bertenshaw EJ, Lluch A, Yeomans MR. Satiating effects of protein but not carbohydrate consumed in a between-meal beverage context. Physiology & Behavior. 2008;93(3):427–436. doi: 10.1016/j.physbeh.2007.09.014. [DOI] [PubMed] [Google Scholar]
- 23.Birch LL, Fisher JO. Development of eating behaviors among children and adolescents. Pediatrics. 1998;101(3):539–549. [PubMed] [Google Scholar]
- 24.Grimes CA, Riddell LJ, Campbell KJ, et al. Dietary Salt Intake, Sugar-Sweetened Beverage Consumption, and Obesity Risk. Pediatrics. 2013;131(1):14–21. doi: 10.1542/peds.2012-1628. [DOI] [PubMed] [Google Scholar]
- 25.Mrdjenovic G, Levitsky DA. Nutritional and energetic consequences of sweetened drink consumption in 6-to 13-year-old children. Journal of Pediatrics. 2003;142(6):604–610. doi: 10.1067/mpd.2003.200. [DOI] [PubMed] [Google Scholar]
- 26.Marshall TA, Levy SM, Broffitt B, et al. Dental caries and beverage consumption in young children. Pediatrics. 2003;112(3):E184–E191. doi: 10.1542/peds.112.3.e184. [DOI] [PubMed] [Google Scholar]
- 27.Birt DF, Pelling JC, Nair S, et al. Diet intervention for modifying cancer risk. Genetics and Cancer Susceptibility: Implications for Risk Assessment. 1996;395:223–234. [PubMed] [Google Scholar]
- 28.Kootstra A. PROTECTION FROM UV-B-INDUCED DNA-DAMAGE BY FLAVONOIDS. Plant Molecular Biology. 1994;26(2):771–774. doi: 10.1007/BF00013762. [DOI] [PubMed] [Google Scholar]
- 29.DeBoer MD, Agard HE, Scharf RJ. Milk intake, height and body mass index in preschool children. Arch Dis Child. 2014 doi: 10.1136/archdischild-2014-306958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Allen RE, Myers AL. Nutrition in toddlers. American Family Physician. 2006;74(9):1527–1532. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.