Summary
Point of care ultrasonography (POCUS) is revolutionizing care of critically ill patients. However, training in POCUS is extremely variable, with no accepted curriculum or certification process. We aimed to delineate the training experience and use of POCUS among trauma providers across Canada via a secure e-questionnaire sent to members of the Trauma Association of Canada. This commentary discusses our survey results and argues for the standardization of POCUS training and certification in Canada.
Point of care ultrasonography (POCUS) has become an integral part of patient care worldwide. The Focused Assessment with Sonography for Trauma (FAST) examination remains the most common form of POCUS used in trauma care. Despite its popularity, however, we suspect that there remains a wide disparity in the level of training among practitioners. We conducted a brief survey to illustrate the training experience among trauma care providers across Canada.
We chose to survey members of the Trauma Association of Canada (TAC), as it is a multidisciplinary group that we feel is representative of trauma care providers in Canada. All physician members of TAC (n = 133), regardless of specialty, were surveyed via SurveyMonkey.
Seventy-two (54.1%) TAC members responded: 43.1% surgeons, 52.8% emergency physicians and 4.2% other specialties. In total 75% work in a level I trauma centre. The majority (83%) of respondents reported using FAST regularly. In addition, 83% of respondents use POCUS for applications beyond FAST, including thoracic and cardiac ultrasonography and for the guidance of invasive procedures.
Training experience
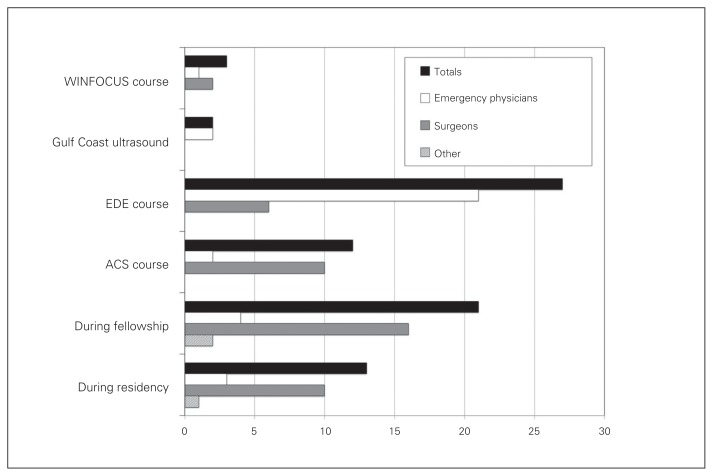
There is a paucity of literature describing the POCUS training experiences of current trauma care providers. Many POCUS courses are offered worldwide. Our survey results illustrate this inconsistency, with trauma providers in Canada reporting training by at least 4 distinct courses. There is also variability by specialty, with many surgeons participating in courses from the American College of Surgeons (ACS), while most emergency physicians have completed the Emergency Department Echo (EDE) course (Fig. 1). In addition, a larger percentage of surgeons than emergency physicians reported receiving training during residency or fellowship. This gives the impression that POCUS skills acquired may not be uniform among trauma care providers in Canada. In addition, 24.3% reported that they had not received any formal POCUS training, suggesting the possibility of self teaching with variable results. Given that ultrasonography is a user-dependent skill and that the learning curve for FAST may be steep, this creates the potential for misinterpretation of ultrasound findings. All in all, this emphasizes the need for a national, standardized course for all trauma providers.
Fig. 1.
Number of respondents who have completed formal Focused Assessment with Sonography for Trauma (FAST) training courses, including totals and by base specialty. ACS = American College of Surgeons; EDE = Emergency Department Echo; WINFOCUS = World Interactive Network Focused On Critical Ultrasound.
Certification
Not all POCUS courses in North America offer a formal certification. Certification is a process in which the trainee is assessed by a governing body. In Canada, the Canadian Emergency Ultrasound Society offers such certification. Overall, only 35% of respondents had completed a formal certification process. There was a clear disparity between those from a surgical versus emergency medicine training background, with 16% and 50%, respectively, completing a certification process. This disparity may be for a number of reasons. First, surgeons may have been slower to accept the idea of formal certification of training for FAST. Being from a procedure-based specialty, surgeons may not feel that formal certification is necessary. Further, a larger percentage of surgeon respondents acquired those skills during residency or fellowship rather than through formal courses. The most likely reason, however, is the lack of formal certification offered through the surgical societies in Canada. This further emphasizes the need for a national, standard certification process that transcends specialties.
Most respondents (61.1%) reported that having a unified certification process of some sort is essential. The majority of courses currently define a certified user based on the completion of a training curriculum that includes practical and didactic components, followed by a variable number of mentored examinations. The main aim of setting a minimum number of exams for the certification process seems to be related to building confidence and raising accuracy. This number of mentored exams differs based on course and certification body and ranges from 10 to 150.1–4 None of these recommendations, however, are evidence-based. The challenge with setting a minimum number of examinations rests in the fact that the learning curve may vary by individual. Our survey showed a similar lack of consensus among respondents as to the ideal number of mentored examinations, with the majority of respondents suggesting it is somewhere between 11 and 50. In addition, most respondents recognized the limitations of defining certification based solely on a set number of examinations, with 72.2% advocating that a change in the current certification process was necessary. The majority supported the introduction of a standardized assessment of ultrasonography technique potentially combined with the current mentored examinations and/or a written examination of ultrasound interpretation. A new definition of certification would be consistent with the shift in the medical education community toward competency-based education.
Confidence and accuracy
A direct correlation between confidence and accuracy of exams has been established by Jang and colleagues.5 Tracking one’s accuracy can give objective feedback on performance and can help guide the practitioner by increasing confidence in medical decision making and conversely can alert the end user as to the need for review or retraining if accuracy is sub-par. In total, 67% of respondents supported the statement that trauma care providers should regularly track their accuracy in FAST, with 56.9% already doing so. Various options exist when developing a quality assurance program. The simplest method may involve tracking positive and negative scans and comparing these predicted results to the appropriate gold standard (laparotomy findings, computed tomography scan, or formal ultrasonography), depending on the clinical scenario. This, however, can be logistically challenging, especially in small centres where patients may need to be transported out for definitive management. Using video archiving and regular, blinded peer review of captured images represents a complementary option. Some respondents suggested, via open-ended response, that keeping track of POCUS accuracy must be incorporated in the hospitals’ quality assessment processes rather than being driven by the practitioner.
Conclusion
Despite obvious potential limitations in sample size and response bias, we feel our survey results represent a “needs analysis,” which has identified a number of areas in POCUS training requiring further study. There is a wide variation in POCUS training among trauma providers in Canada, with only a minority completing a formal certification process. There is no consensus on the optimal curriculum for POCUS training. Creation of a standardized POCUS curriculum and certification process for trauma providers, regardless of profession, affiliation or specialty, is desired and necessary.
Footnotes
This study was presented as an oral presentation at the Trauma Association of Canada Conference 2014, Montreal, Canada.
Competing interests: None declared.
Contributors: All authors contributed substantially to the conception, writing and revision of this commentary and approved the final version for publication.
References
- 1.Bahner D, Blaivas M, Cohen HL, et al. AIUM practice guideline for the performance of the focused assessment with sonography for trauma (FAST) examination. J Ultrasound Med. 2008;27:313–8. doi: 10.7863/jum.2008.27.2.313. [DOI] [PubMed] [Google Scholar]
- 2.Canadian Emergency Ultrasound Society. CEUS recommended standards. 2014. [accessed 2014 Mar. 5]. Available: http://ceus.ca/002-standards/002-00.standards.htm.
- 3.College of Emergency Medicine (South Africa) Policy document: emergency ultrasound in South Africa. 2009. [accessed 2014 Mar. 5]. Available: http://academic.sun.ac.za/emergencymedicine/documents/CEM(SA)%20Emergency%20Ultrasound%20POLICY%20v3.pdf.
- 4.College of Emergency Medicine (UK) Ultrasound Subcommittee. Ultrasound training 2013. [accessed 2014 Mar. 5]. Available: www.collemergencymed.ac.uk/Training-Exams/Training/Ultrasound.
- 5.Jang T, Naunheim R, Sineff S, et al. Operator confidence correlates with more accurate abdominal ultrasounds by emergency medicine residents. J Emerg Med. 2007;33:175–9. doi: 10.1016/j.jemermed.2007.01.018. [DOI] [PubMed] [Google Scholar]