Abstract
Typical clinical symptoms of chronic pancreatitis are vague and non-specific and therefore diagnostic tests are required, none of which provide absolute diagnostic certainly, especially in the early stages of disease. Recently-published guidelines bring much needed structure to the diagnostic work-up of patients with suspected chronic pancreatitis. In addition, novel diagnostic modalities bring promise for the future. The assessment and diagnosis of pancreatic exocrine insufficiency remains challenging and this review contests the accepted perspective that steatorrhea only occurs with > 90% destruction of the gland.
Keywords: Pancreatitis, chronic; Diagnosis; Exocrine pancreatic insufficiency; Pancreatic enzyme replacement therapy; Malabsorption
Core tip: Chronic pancreatitis presents a diagnostic challenge, especially in early disease. This paper summarizes the available diagnostic modalities as well as the most recently-published diagnostic guidelines. It is widely accepted that the pancreas has excellent exocrine reserve. We review the original studies which have supported this principle and suggest an alternative interpretation of the data.
INTRODUCTION
Defined as a chronic inflammatory disease of the pancreas characterized by irreversible morphological change and typically causing pain and/or permanent loss of function[1], chronic pancreatitis is beset by destruction of healthy pancreatic tissue and the development of fibrous scar tissue. Gradual loss of exocrine and endocrine function ensues with clinical manifestations such as steatorrhea, abdominal pain, and diabetes. Current treatments can only provide temporary pain relief and manage complications, but are unable to halt or slow the advance of this disease[2]. The overall incidence of chronic pancreatitis in Europe is thought to be about 6-7 per 100000[3], and data suggest increasing incidence[4]. A study from the United Kingdom in the 1990’s showed trends of rising incidence based on national statistics for admission[5]. Seven consecutive surveys from Japan have shown a definite increase in the prevalence of alcoholic chronic pancreatitis[6]. There are limited epidemiological data regarding the natural progression to chronic pancreatitis following an episode of acute pancreatitis. A study from North America[7] following over 7000 patients with an admission for acute pancreatitis found subsequent chronic pancreatitis in 12% of patients.
The majority of cases from western countries have been attributed to alcohol excess, although etiologies vary by region and country. The presenting symptom of most patients with chronic pancreatitis is abdominal pain, usually epigastric, dull and constant in nature. It is almost always localized in the upper half of the abdomen, from which it can radiate directly through to the back, or laterally around to the left or right flank. Initially the duration of pain is quite variable, ranging from several hours to several days, but as the disease progresses the attacks become more frequent and pain-free intervals shrink and vanish[8].
In some patients, chronic pancreatitis can be entirely silent, and in presentation patients may present with the sequelae of exocrine or endocrine insufficiency: steatorrhea, weight loss and diabetes. Less common initial presentations include biliary obstruction with recurrent episodes of mild jaundice, cholangitis, or vague attacks of indigestion[9]. Obstruction of the splenic vein by an inflamed tail of the pancreas can lead to left-sided portal hypertension, gastric varices and GI bleeding. Chronic pancreatitis and pancreatic cancer may present in a similar manner, making it difficult to distinguish between them[9].
Although chronic pancreatitis diagnosis may be suspected following presentation with suggestive symptoms, clinical presentation is usually insufficient for a firm diagnosis. In fact, a diagnosis of chronic pancreatitis is difficult to establish, especially in the early stages of disease. Typical symptoms such as weight loss, pain, steatorrhea, and malnutrition are vague and not specific to chronic pancreatitis. Therefore diagnostic tests of pancreatic structure and function are required - none of which provide absolute diagnostic certainly in the early stages.
The aim of this review is to: (1) summarize the available diagnostic modalities and the most recent diagnostic guidelines; (2) review emerging and novel diagnostic techniques; and (3) challenge the status quo regarding pancreatic exocrine insufficiency, specifically the accepted concept that steatorrhea occurs only with greater than 90% destruction of the gland.
DIAGNOSTIC TOOLS
There is no universally accepted diagnostic gold standard for chronic pancreatitis. While no one radiological, clinical or endoscopic tool can definitively diagnose this disease; there is an array of diagnostic instruments, which fall into four broad categories.
Histology
Histological features of chronic pancreatitis include parenchymal fibrosis, acinar atrophy, ductal distortion, and intraductal calcification[10,11]. Histological diagnosis is limited by a lack of consensus around grading for chronic pancreatitis[10]. Whilst histology is the most specific method of diagnosis, however it is rarely available and therefore proxy testing is required.
Radiological studies
Computed tomography: Computed tomography (CT) is a widely-used imaging modality and is an objective and reliable method of measuring pancreatic morphology. “Classical” diagnostic chronic pancreatitis findings on CT include atrophy, dilated pancreatic duct and pancreatic calcification (Figure 1A). While diagnosis of early chronic pancreatitis is not reliable, CT should nevertheless be performed in all patients to exclude a mass or gastro-intestinal malignancy[12]. In addition, CT may be used in the assessment of chronic pancreatitis-related complications, such as pseudocysts, pseudoaneurysm, duodenal stenosis and malignancy. CT should be performed using a non-contrast phase to identify calcifications followed by a “pancreas-protocol” contrast phase[13]. Overall, CT remains the best screening tool for detection of chronic pancreatitis and exclusion of other intra-abdominal pathology that may be indistinguishable from chronic pancreatitis based on clinical symptoms.
Figure 1.
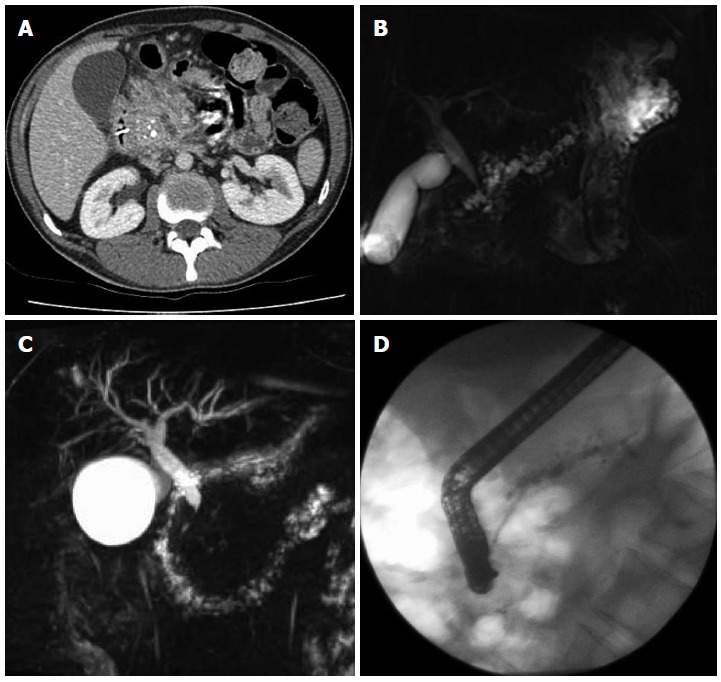
Computed tomography demonstrating enlarged head of pancreas with coarse calcification and a dilated main pancreatic duct (A), magnetic resonance cholangiopancreatography showing a tortuous, dilated pancreatic duct (B), inflammatory stricture of the distal common bile duct (C), endoscopic retrograde cholangiopancreatography showing a stent placed in a dilated pancreatic duct (D).
Magnetic resonance imaging, magnetic resonance cholangiopancreatography, and secretin-enhanced magnetic resonance cholangiopancreatography: Magnetic resonance imaging (MRI) is more sensitive than CT and is emerging as the initial radiological imaging modality of choice for the evaluation of chronic pancreatitis with unequivocal CT scans[12]. Magnetic resonance cholangiopancreatography (MRCP) allows for excellent visualization of the pancreatic duct (Figure 1B and C), although visualization of the side branches is not good[14]. However, the addition of secretin enhancement provides even better visualization of abnormalities of the pancreatic duct and its branches, which may not have been evident on routine MRCP. Secretin stimulates fluid secretion in the ductal system, and increases the tonus of the sphincter of Oddi during the first 5 min, hindering the release of fluid through the papilla of Vater[14,15]. Therefore secretin increases the absolute volume of intraductal free water and fills the collapsed branches with fluid, thereby allowing the detection of mild ductal changes in mild disease that are not detectable using routine MRCP[15]. MRCP allows for similar visualization of the pancreatic duct as is afforded during the much more invasive endoscopic retrograde cholangiopancreatography (ERCP). MRCP also facilitates the diagnosis of complications of chronic pancreatitis such as biliary strictures (Figure 1C). Negatives associated with these modalities include limited access to MR time combined with the technical complexity of the test[16].
Endoscopic studies
Endoscopic ultrasound: Endoscopic ultrasound (EUS) provides close-proximity imaging of the entire pancreas and adjacent structures[17]. Although more invasive than CT and MRI/MRCP, EUS is the most sensitive imaging method for detecting minimal structural changes associated with chronic pancreatitis, and therefore is useful in minimal change or non-calcified chronic pancreatitis. The EUS-Rosemount criteria were published in 2009[18] as consensus-based criteria for EUS features of chronic pancreatitis (Table 1). Depending on the number of features identifiable, the following classification is applied: “consistent with chronic pancreatitis”, “suggestive of chronic pancreatitis”, “indeterminate for chronic pancreatitis”, or “normal” (Table 2)[18]. It is still unresolved whether or not “indeterminate for chronic pancreatitis” refers to early-stage chronic pancreatitis[19]. The number of EUS criteria for diagnosis varies between institutions, and in additions, intra-observer agreement among endosonographers is low, which is one of its greatest limitations[20]. Conwell and colleagues[17] showed that based on a gold standard pancreatic function test [an endoscopic, secretin-stimulated pancreatic function test (PFT)], 6 or more EUS criteria are needed to establish a definitive diagnosis of chronic pancreatitis. However, less than 6 EUS criteria may be associated with pancreatic secretory dysfunction, and so, EUS may not be an adequate screening modality for early chronic pancreatitis where there is an absence of significant parenchymal and ductal scarring[17].
Table 1.
Rosemont criteria for chronic pancreatitis
| Parenchymal features | |
| Major A | Hyperechoic foci with stranding |
| Major B | Lobularity with honeycombing |
| Minor | Hyperechoic foci |
| Lobularity | |
| Cysts | |
| Hyperechoic strands | |
| Ductal features | |
| Major A | Calculi |
| Minor | Main pancreatic duct dilation |
| Irregular main pancreatic duct contour | |
| Hyperechoic main pancreatic duct margin | |
| Dilated side branches |
Table 2.
Endoscopic ultrasound diagnosis of chronic pancreatitis on the basis of Rosemont criteria
| Consistent with chronic pancreatitis | 1 major A feature + ≥ 3 minor features or |
| 1 major A feature + major B feature or | |
| 2 major A features | |
| Suggestive of chronic pancreatitis | 1 major A feature + < 3 minor features or |
| 1 major B + ≥ 3 minor features or | |
| ≥ 5 minor features | |
| Indeterminate for chronic pancreatitis | 3 or 4 minor features, no major features or |
| Major B feature alone with < 3 minor features | |
| Normal | ≤ 2 minor features, no major features |
ERCP: ERCP is considered a sensitive test for the diagnosis of chronic pancreatitis, having the ability to show dilation or stricture of the pancreatic duct and its branches, as well as early features of chronic pancreatitis[21]. ERCP provides therapeutic options, such as dilation, stone extraction, and stenting of the duct (Figure 1D). An additional benefit is the possibility of procuring pancreatic juice during ERCP[22]. The Cambridge criteria developed in 1984[23] allows the classification of chronic pancreatitis based on the number of ductal abnormalities found at ERCP. However, with the widespread availability of other non-invasive imaging modalities, ERCP should not be used for the diagnosis of chronic pancreatitis. ERCP is also limited by the fact that it does not allow evaluation of the pancreatic parenchyma[10]. Axial imaging (CT or MRCP) and EUS have replaced ERCP as a diagnostic tool and the principles of the Cambridge classification can be adapted to CT or MRCP.
Pancreatic function tests
Direct pancreatic function testing: PFTs for the testing of exocrine function may be classified as direct and indirect. Direct tests involve the stimulation of the pancreatic cells using secretagogues (secretin or cholecystokinin, CCK). These tests are invasive (requiring endoscopic procedures), expensive and tend not to be widely done outside of specialist centers. Sensitivity is high for direct PFTs in the diagnosis of late chronic pancreatitis, however lower (70%-75%) for early chronic pancreatitis. Direct PFTs have a long history (from the 1900s), and the original Dreiling tube method[24,25] (popularized at the University of Florida) and newer methods such as the endoscopic PFT (ePFT, developed at the Cleveland Clinic) are considered the nonhistological criterion standards for diagnosis of early chronic pancreatitis[2].
Indirect pancreatic function testing: The invasive nature of direct testing, along with the expense and unavailability of the tests, obligates indirect means of pancreatic function testing. Such tests include fecal elastase, fecal fat measurements and serum trypsinogen. The 3 d fecal fat collection test requires the collection of stool for a 72 h period following the ingestion of a precisely-known quantity of fat (100 g per day). Excretion of more than 7 g of fat in the stool per day is indicative of fat malabsorption, while loss of more than 15 g per day is considered severe fat malabsorption. However the 3 d fecal fat assessment is a cumbersome test for both patients and laboratory personnel, and is not routinely done. In general, indirect tests are moderately sensitive and specific for diagnosing advanced chronic pancreatitis, but less so for early disease. Pancreatic elastase-1 fecal elastase-1 (FE-1) is a human-specific enzyme that is not degraded during intestinal transit, is enriched 5-6 fold in the feces, and is therefore a test of pancreatic exocrine function. Benefits include the fact that patients do not have to consume a specific substrate (i.e., fat) prior to testing, nor must they halt pancreatic enzyme replacement therapy. However whilst FE-1 is an adequate measure of severe exocrine impairment, it is not a good indicator of mild to moderate disease.
DIAGNOSTIC GUIDELINES FOR CHRONIC PANCREATITIS
American pancreatic association guidelines
At the 2011 meeting of the American Pancreatic Association, a chronic pancreatitis conference was held to develop a 3-part set of practice guidelines for this disease. The first part of these guidelines relates to diagnosis and was published in 2014[2]. The document, which represents the first US practice guidelines for chronic pancreatitis, defines the diagnostic evidence for CP as definitive, probable and insufficient based on current knowledge. The guidelines emphasize that without sufficient evidence, patients should not be mislabeled as having chronic pancreatitis, and it is better to err on the side of not labelling the patient with chronic pancreatitis, recommending longitudinal follow-up with serial imaging and physiological testing in unequivocal cases until definitive evidence is present. The guidelines propose a diagnostic algorithm which proceeds from non-invasive to a more invasive approach (Figure 2). Upon confirmed diagnosis, the guidelines recommend a comprehensive etiological/morphological and physiological characterization of chronic pancreatitis, and propose an associated nomenclature. This nomenclature recommends the following structure: chronic (TIGARO etiology-induced) pancreatitis + MANNHEIM/Cambridge imaging grade + physiological stage (where TIGARO is toxic-metabolic, idiopathic, genetic, autoimmune, recurrent and severe acute pancreatitis associated, obstructive). The document details the available evidence for 9 topics, giving Evidence-Based Medicine Statements for each. With the exception of the anatomic pathology topic, each statement is given a recommendation (strong/conditional) and the level of evidence is defined as strong/moderate/low. The proportion of “strong” vs “conditional” statements was roughly half and half. The intention of the group is to modify these guidelines with emerging evidence. The APA diagnostic guidelines are summarized in Table 3.
Figure 2.
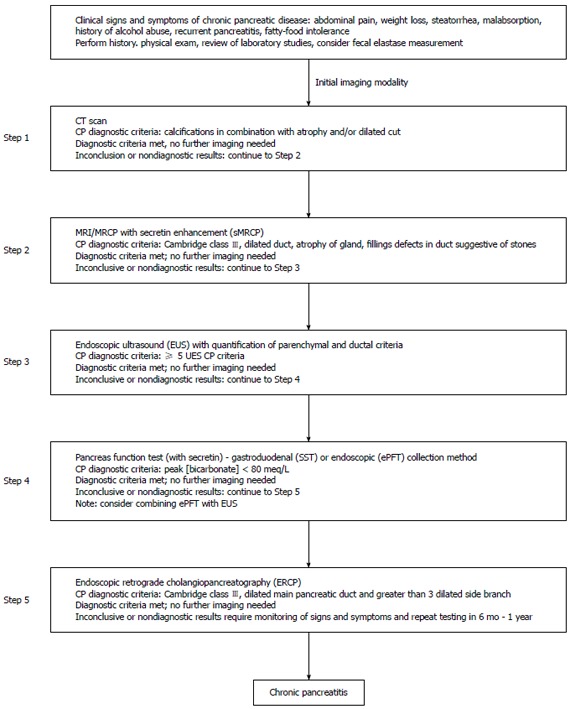
Step-wise algorithm approach to diagnosis of chronic pancreatitis. Step 1: Survey (data review, risk factors, CT-imaging); Step 2: Tomography (pancreas protocol CT scan, MRI/secretin-enhanced magnetic resonance cholangiopancreatography); Step 3: Endocopy [EUS (standard criteria)]; Step 4: Pancreas functioning (Dreiling, ePFT); Step 5: ERCP (with intent for therapeutic intervention). From Conwell et al[2]. CT: Computed tomography; MRI: Magnetic resonance imaging; EUS: Endoscopic ultrasound; ERCP: Endoscopic retrograde cholangiopancreatography.
Table 3.
A summary of the APA diagnostic guidelines (2014)
| Topic | Level | |
| Epidemiology and risk factors | Data on population-based estimates are emerging | C/L |
| A small fraction of patients progress from AP to CP | C/M | |
| Alcohol/smoking are independent risk factors for CP. Both are associated with disease progression and their risks are likely multiplicative | S/H | |
| The spectrum of risk factors for CP has broadened | C/L | |
| Genetic discoveries are rapidly uncovering new susceptibility factors. Knowledge of gene-environment interactions may translate into new diagnostic and treatment paradigms | S/M | |
| Pathological Definitions | CP is characterized by atrophy and fibrosis of the exocrine tissue with or without chronic inflammation | - |
| Scarring of the parenchyma may be focal, patchy or diffuse | - | |
| Progressive fibrosis and atrophy may lead to exocrine insufficiency followed by endocrine insufficiency | - | |
| Autoimmune pancreatitis can mimic pancreas carcinoma | - | |
| Ultrasound and CT | Ultrasound and CT are best for late findings of CP but are limited in the diagnosis of early or mild pancreatitis | C/M |
| Intraductal pancreatic calcifications are the most specific and reliable sonographic and CT signs of CP | S/M | |
| CT is helpful for the diagnosis of complications of CP | S/M | |
| CT is helpful for the diagnosis of other conditions that can mimic CT | C/L | |
| MRI imaging | Compared with ultrasound and CT, MRI is a more sensitive imaging tool for the diagnosis of CT | C/M |
| Ductal abnormalities are very specific and reliable MRI signs of CP | C/L | |
| Signal intensity changes in the pancreas, seen on MRI, may precede ductal abnormalities and suggest early CT | C/L | |
| Stimulation of the pancreas using IV secretin may improve the diagnostic accuracy in the detection of ductal and parenchymal abnormalities seen on CT | C/L | |
| Endoscopic ultrasound | The ideal threshold number of EUS criteria necessary to diagnose CP has not been firmly established, but the presence of 5 or more or 2 or less strongly suggests or refutes the diagnosis of CP | S/L |
| The EUS features of CP are not necessarily pathologic and may occur as a normal aging, as a normal variant, or due to the nonpathologic asymptomatic fibrosis in the absence of endocrine/exocrine dysfunction | S/L | |
| The relatively poor IOA for EUS CP features limits the diagnostic accuracy and overall utility of the EUS for diagnosing CP | S/M | |
| ERCP | ERP is rarely used for diagnostic purposes | S/M |
| The correlation between the Cambridge criteria and histology is highest in advanced CP | S/M | |
| Multiple confounders limit the interpretation of ductal changes by Cambridge criteria | S/L | |
| Indirect PFTs | Indirect PFTs generally are sensitive for steatorrhea and useful in quantifying the degree of exocrine insufficiency | C/L |
| Indirect PFTs are moderately sensitive and specific for diagnosing advanced CP but are less so for diagnosing early CP | C/S | |
| The FE-1 assay, polyclonal assay more than monoclonal, can be limited in specificity, especially if the stool has is watery and/or in the presence of small bowel disease | C/L | |
| Faecal chymotrypsin may be useful in detecting compliance with exogenous pancreatic enzyme supplementation | C/L | |
| Faecal fat assays are sensitive for steatorrhea but are of limited utility due to the cumbersome nature of patient collection and laboratory handling of samples. In addition, strict adherence to dietary recommendations for several days is required | C/M | |
| Direct PFTs | Direct PFTs have high sensitivity for detecting late CP, but lower sensitivity (70%-75%) for early CP | S/L |
| The traditional secretin and CCK PFTs performed with the aortoduodenal tube pancreas fluid collection are highly accurate but require fluoroscopy for confirmation of tube placement and are not widely utilized | S/M | |
| The ePFT has good correlation with the traditional Dreiling PFT | S/M | |
| Correlation of imaging and function with histology | As structural severity worsens in CP, exocrine function declines | S/M |
| Both EUS and PFT results correlate with fibrosis in CP | C/L | |
| A combined approach (e.g., EUS/ePFT) could improve detection of minimal change CP (MCCP) | C/L |
Levels relate to level of recommendation (conditional; strong)/level of evidence (low; moderate; high). AP: Acute pancreatitis; CP: Chronic pancreatitis; CT: Computed tomography; MRI: Magnetic resonance imaging; IV: Intravenous; EUS: Endoscopic ultrasound; IOA: Inter-observer variability; PFTs: Pancreatic function tests; FE-1: Fecal elastase-1; CCK: Cholecystokinin; ePFT: Endoscopic PFT; MCCP: Minimal change chronic pancreatitis.
Other guidelines
Conwell and Bechien[12] devised an algorithm for the stepwise diagnosis of chronic pancreatitis. Using the most commonly available radiological and endoscopic tests, the algorithm progresses from a non-invasive to an invasive approach, starting with a clinical Survey, Tomography (imaging), Endoscopy, and finally Pancreatic function. The authors caution against mislabeling patients with a chronic pancreatitis diagnosis where they instead have a chronic abdominal pain syndrome with a remote history of procedure-induced pancreatitis.
In 2010, the Japanese Clinical Diagnostic criteria for chronic pancreatitis were published[26]. These criteria were intended to diagnose “early chronic pancreatitis”, with the intention of preventing intractable disease by allowing early treatment. The diagnostic tool specifies that 2 of the following 4 items be present: repeated upper abdominal pain, abnormal pancreatic enzyme levels (serum or urine), abnormal pancreatic function, and on-going heavy alcohol ingestion (of > 80 g pure ethanol per day). These items, along with characteristic early findings by EUS imaging are said to be indicative of early chronic pancreatitis. According to this tool, more than 2 of the following EUS criteria are required for diagnosis (as well as at least one from the first 4 criteria: (1) lobulating with honeycombing; (2) lobulating without honeycombing; (3) hyperechoic foci with stranding; (4) stranding; (5) cysts; (6) dilated side branches; and (7) hyperechoic MPD margin. More recently, reports of the Tissue Harmonic Echo mode on EUS have suggested that these modes can reveal details of abnormalities of early chronic pancreatitis and might therefore contribute to a definite diagnosis in the early stages of disease[27].
Guidelines were published in 2010 by the Hepato-Pancreatico-Biliary Association of South Africa, along with the South Africa Gastroenterology Society which summarized the diagnostic tools for chronic pancreatitis[28]. The authors suggested that the choice of imaging study should be based on the available technology, the available skills and the invasive nature of the investigation. They emphasize the limitations of PFTs in the diagnosis of chronic pancreatitis, stressing that PFTs alone do not distinguish chronic pancreatitis from pancreatic exocrine insufficiency (PEI) without chronic pancreatitis.
Emerging diagnostic techniques
Engjom et al[16] in 2015 described a technique which evaluated ultrasonography of the fluid in the descending duodenum and Wirsung duct, after secretin stimulation, as a measure of pancreatic fluid flow. Using both chronic pancreatitis and cystic fibrosis patients, those with pancreatic exocrine insufficiency (Defined as FE-1 < 100 μg/g, or peak bicarbonate concentrations of > 80 meq/L) were compared to healthy controls. Ultrasonography gave precise measurement of the volume transported in the descending duodenum and Wirsung duct after secretin stimulation. The authors identified subjects with severe pancreatic output failure compared to healthy controls with good diagnostic accuracy.
EUS elastography is a recently described diagnostic tool which quantitatively analyses pancreatic tissue consistency. This method enables areas with varying elasticities to be differentiated within the pancreas. The principle of elastography is based on the assumption that compression of a target tissue by an echo-endoscopic probe creates a strain that differs according to the hardness and softness of the tissue. During the procedure, elastography is shown in real time as transparent colour images[29]. Quantitative elastography therefore allows for the quantitative assessment of fibrosis in chronic pancreatitis. In quantitative elastography, the tissue stiffness is measured in the targeted area [region of interest (ROI) A] and outside the targeted area in a region representing normal tissue (ROI B). Thereafter, the strain ratio value is calculated as the quotient B/A. One study[30] on EUS elastography in chronic pancreatitis found excellent concordance between EUS criteria for chronic pancreatitis and strain ratio, and reported a diagnostic accuracy of 91%. A further study from this group[31] evaluated whether EUS-elastography can predict PEI in chronic pancreatitis. Comparing elastography to the C-mixed triglyceride breath test, pancreatic strain ratio was higher in those with PEI than with a normal breath test. The probability of PEI was 87% with a strain ratio of greater than 4.5, and could therefore be considered for pancreatic enzyme therapy, even in the absence of any pancreatic function test. The relationship between pancreatic morphology and exocrine function is discussed in the following section.
The occurrence of nutrition deficiencies in chronic pancreatitis has recently been suggested by Lindkvist et al[32] as an indicator of PEI. One hundred and fourteen patients had a chronic pancreatitis diagnosis based on endoscopic ultrasonography or MRI, and PEI was investigated by the 13C-mixed triglyceride breath test. They found that serum nutritional markers were able to predict PEI with reasonably high sensitivity and specificity.
RELATIONSHIP BETWEEN PANCREATIC DESTRUCTION AND FAT MALABSORPTION: CHALLENGING THE STATUS QUO
PEI is the reduction in pancreatic enzyme activity in the intestinal lumen to a level that is below the threshold required to maintain normal digestion[33]. It is widely believed that the pancreas has a large exocrine reserve. This is largely due to a landmark study published in 1973 by DiMagno et al[34], which studied the relationship between malabsorption and lipase secretion of the pancreas. They reported confirmation “that 90% of the gland must be functionally destroyed or obstructed before steatorrhea or creatorrhea occurs”, and that “fat digestion is not clearly impaired until lipase outputs are decreased to about 10% of normal”. These findings were based on a comparison of 17 patients with chronic pancreatitis and 33 healthy controls. Total enzyme output was measured in response to duodenal perfusion with essential amino acids and intravenous cholecystokinin-pancreaozymin in patients and controls. Values were expressed as a percentage of normal, which was derived from the healthy controls. While the study was well-conducted, the data interpretation was open to debate. The low sample size of 17 was itself not necessarily a limitation, as few subjects are required to show statistical significance where there is a large effect. However, critically, 16/17 patients had poor pancreatic function (defined by lipase secretion < 10% of normal), therefore, the authors can only conclude that those with poor pancreatic secretory function (and presumably severe disease) suffer fat excretion consistent with steatorrhea (> 7 g per day) (Figure 3). The one patient with high percentage lipase secretion happened to have normal fat absorption; however, this sole patient does not provide enough evidence that those with greater than 10% pancreatic function have normal fat excretion. Moreover, among the majority that did have low lipase secretion (< 10% normal lipase output), the range of fat loss per day was extraordinarily broad. Those with severely reduced lipase output secondary to chronic pancreatitis exhibited fat malabsorption ranging from mild (about 10 g/24 h), to very severe (almost 100 g/24 h), an enormously broad range in clinical terms.
Figure 3.
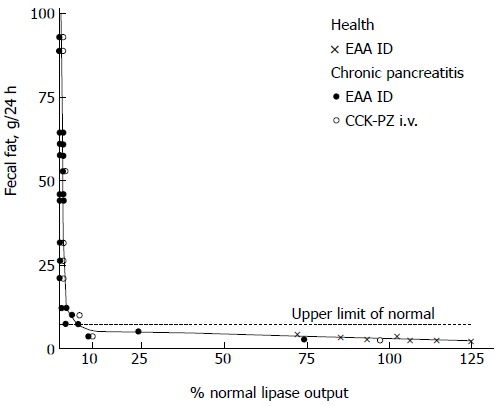
Relation of lipase outputs per 24 h to fecal fat excretion in healthy subjects and patients with chronic pancreatitis. Values above the horizontal dashed line denote steatorrhea (> 7 g per 24 h). The shaded area represents lipase outputs less than 10 percent of normal. From DiMagno et al[34]. Copyright © 2015 Massachusetts Medical Society. Reprinted with permission from Massachusetts Medical Society.
Lankisch et al[35] conducted a similar, larger study in 1986 (n = 47 chronic pancreatitis patients) with a broader range of exocrine impairment. Figure 4 displays the relationship between lipase output and fecal fat excretion from this study. Consistent with the DiMagno study, most patients with < 10% lipase excretion had steatorrhea. However not all did; three patients with < 10% lipase excretion had normal fecal fat excretion. And similarly consistent with the DiMagno study there was a remarkably broad variation in fecal fat excretion for those with lipase secretion of < 10 g/d, ranging from normal to greater than 60 g/d. Unlike the DiMagno study, the Lankisch study included subjects with moderately impaired lipase secretion, and of those patients, two (7.7%) had steatorrhea. Furthermore, 16.2% and 15.6% of patients with moderate impairment of amylase and trypsin respectively exhibited steatorrhea (graphs not shown). Therefore steatorrhea was not limited to those with extreme pancreatic damage.
Figure 4.
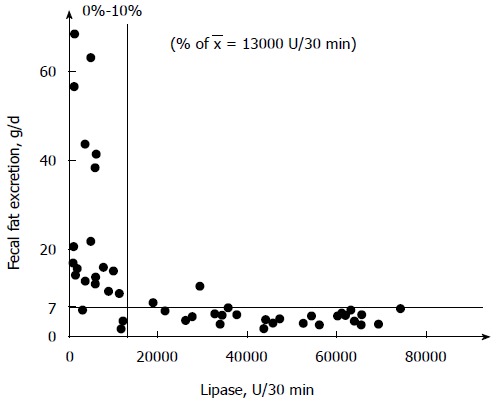
Relation of lipase output to fecal fat excretion in 47 patients with exocrine insufficiency. Reprinted with permission from Lankisch et al[35]. Copyright © 2015 Karger Publishers, Basel, Switzerland.
Various studies quantifying lipase excretion in chronic pancreatitis have been published. Conwell et al[36] investigated peak lipase concentration by means of a CCK-stimulated pancreatic function test in 19 healthy volunteers and 18 patients with chronic pancreatitis. They found that lipase concentration in duodenal fluid was markedly lower in those with chronic pancreatitis compared to controls; 50% in mild chronic pancreatitis, 23% in moderate chronic pancreatitis and 13% in severe chronic pancreatitis. Mizuno et al[37] found that lipase output in severe disease and mild disease was 10% and 60% respectively. Ideally, the studies conducted by DiMagno et al[34] and Lankisch et al[35] should be repeated on an adequately large number of subjects with a broad spectrum of lipase outputs. Intuitively one would expect a linear relationship between lipase secretion and fat excretion. The seemingly non-linear relationship suggested by DiMagno et al[34] has been contradicted in an artificial model of steatorrhea (induced by lipase-inhibitor orlistat). They showed a linear and positive correlation between lipolysis inhibition and fat excretion levels[38].
The appearance of sufficient pancreatic exocrine function (until > 90% gland destruction) may be in part due to the secretion and action of gastric lipase. There is an element of compensation by gastric lipase in chronic pancreatitis patients with advancing disease, essentially giving the illusion of adequate pancreatic exocrine function. As well as evidence of increased secretion of gastric lipase in severe (vs mild) chronic pancreatitis and healthy controls, gastric lipase is also more stable in severe chronic pancreatitis due to an increase in the specific activity of the enzyme[39]. Gastric lipase has higher specific activity at acidic pH values, and those with chronic pancreatitis are known to have more acidic small intestine contents than normal patients[40] (due to reduced bicarbonate excretion). Hence, this provides another reason to revisit data from early studies examining an association between lipase excretion and fecal fat loss, as the clinically relevant contribution of gastric lipase had not been considered. Indeed the contribution of gastric lipase may partially explain the remarkably broad range of fecal fat excretion in patients with pancreatic lipase excretion of < 10% normal (Figures 3 and 4).
The 1973 paper by DiMagno et al[34], along with the 1986 paper by Lankisch et al[35], appear to be the only studies that have examined exocrine insufficiency and fat excretion in this manner. The study by DiMagno in particular has greatly influenced understanding and practice in PEI and is widely cited as evidence of adequate exocrine function until almost total pancreatic destruction. Therefore it is possible that PEI is ignored, disregarded and untreated in all but the most morphologically severe patients. In fact, a study from The Netherlands[41] found that a considerable number of patients with PEI were undertreated, with 70% of subjects reporting ongoing steatorrhea-related symptoms, and 42% still suffering weight loss. Undertreatment may result in PEI-related abdominal symptoms, weight loss, muscle depletion, nutrient deficiency[42,43], and deficiency-related complications, including osteoporosis[44,45] and premature fragility fracture[46,47].
CONCLUSION
Diagnosis of chronic pancreatitis continues to present a clinical challenge; however recent guidelines have brought much need direction and clarity to this endeavor. In the assessment of pancreatic exocrine function, the traditional viewpoint that steatorrhea does not occur until > 90% of the pancreas is destroyed is still often quoted and accepted. We have challenged this perspective by revisiting the old data and suggesting an alternative interpretation. The perception that the pancreas has excellent exocrine reserve needs to be reconsidered, not least due to the potential disregard for PEI and resultant delays in establishing appropriate and adequate enzyme therapy that are likely to occur if this unsound principle continues to be accepted.
Footnotes
Supported by an unrestricted educational grant from The Meath Foundation www.meathfoundation.com (in part, to Duggan SN); unrestricted research grant from Mylan (in part, to Ní Chonchubhair HM).
Conflict-of-interest statement: Duggan SN has received fees for serving as a speaker and/or writer for Mylan, Fresenius Kabi, Merck and Nutricia.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: August 19, 2015
First decision: October 14, 2015
Article in press: December 8, 2015
P- Reviewer: Barauskas G, Wu WJ, Yan MX S- Editor: Yu J L- Editor: A E- Editor: Liu XM
References
- 1.Go VL, Dimagno EP, Gardner JD, Lebenthal E, Reber HA, Scheele GA. The Pancreas: Pathobiology and Disease. 2nd ed. New York: Raven; 1993. [Google Scholar]
- 2.Conwell DL, Lee LS, Yadav D, Longnecker DS, Miller FH, Mortele KJ, Levy MJ, Kwon R, Lieb JG, Stevens T, et al. American Pancreatic Association Practice Guidelines in Chronic Pancreatitis: evidence-based report on diagnostic guidelines. Pancreas. 2014;43:1143–1162. doi: 10.1097/MPA.0000000000000237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jupp J, Fine D, Johnson CD. The epidemiology and socioeconomic impact of chronic pancreatitis. Best Pract Res Clin Gastroenterol. 2010;24:219–231. doi: 10.1016/j.bpg.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 4.Joergensen M, Brusgaard K, Crüger DG, Gerdes AM, de Muckadell OB. Incidence, prevalence, etiology, and prognosis of first-time chronic pancreatitis in young patients: a nationwide cohort study. Dig Dis Sci. 2010;55:2988–2998. doi: 10.1007/s10620-009-1118-4. [DOI] [PubMed] [Google Scholar]
- 5.Tinto A, Lloyd DA, Kang JY, Majeed A, Ellis C, Williamson RC, Maxwell JD. Acute and chronic pancreatitis--diseases on the rise: a study of hospital admissions in England 1989/90-1999/2000. Aliment Pharmacol Ther. 2002;16:2097–2105. doi: 10.1046/j.1365-2036.2002.01367.x. [DOI] [PubMed] [Google Scholar]
- 6.Hirota M, Shimosegawa T, Masamune A, Kikuta K, Kume K, Hamada S, Kanno A, Kimura K, Tsuji I, Kuriyama S. The seventh nationwide epidemiological survey for chronic pancreatitis in Japan: clinical significance of smoking habit in Japanese patients. Pancreatology. 2014;14:490–496. doi: 10.1016/j.pan.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 7.Yadav D, O’Connell M, Papachristou GI. Natural history following the first attack of acute pancreatitis. Am J Gastroenterol. 2012;107:1096–1103. doi: 10.1038/ajg.2012.126. [DOI] [PubMed] [Google Scholar]
- 8.Bouchier IAD, Hodgson HJF, Keighley MRB. Chronic pancreatitis. Gastroenterology Clinical Science and Practice. 2nd ed. Philadelphia: Saunders; 1993. [Google Scholar]
- 9.Giger U, Stanga Z, DeLegge MH. Management of chronic pancreatitis. Nutr Clin Pract. 2004;19:37–49. doi: 10.1177/011542650401900137. [DOI] [PubMed] [Google Scholar]
- 10.Sze KC, Pirola RC, Apte MV, Wilson JS. Current options for the diagnosis of chronic pancreatitis. Expert Rev Mol Diagn. 2014;14:199–215. doi: 10.1586/14737159.2014.883277. [DOI] [PubMed] [Google Scholar]
- 11.Klöppel G, Maillet B. Chronic pancreatitis: evolution of the disease. Hepatogastroenterology. 1991;38:408–412. [PubMed] [Google Scholar]
- 12.Conwell DL, Wu BU. Chronic pancreatitis: making the diagnosis. Clin Gastroenterol Hepatol. 2012;10:1088–1095. doi: 10.1016/j.cgh.2012.05.015. [DOI] [PubMed] [Google Scholar]
- 13.Hollett MD, Jorgensen MJ, Jeffrey RB. Quantitative evaluation of pancreatic enhancement during dual-phase helical CT. Radiology. 1995;195:359–361. doi: 10.1148/radiology.195.2.7724753. [DOI] [PubMed] [Google Scholar]
- 14.Cappeliez O, Delhaye M, Devière J, Le Moine O, Metens T, Nicaise N, Cremer M, Stryuven J, Matos C. Chronic pancreatitis: evaluation of pancreatic exocrine function with MR pancreatography after secretin stimulation. Radiology. 2000;215:358–364. doi: 10.1148/radiology.215.2.r00ma10358. [DOI] [PubMed] [Google Scholar]
- 15.Sai JK, Suyama M, Kubokawa Y, Watanabe S. Diagnosis of mild chronic pancreatitis (Cambridge classification): comparative study using secretin injection-magnetic resonance cholangiopancreatography and endoscopic retrograde pancreatography. World J Gastroenterol. 2008;14:1218–1221. doi: 10.3748/wjg.14.1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Engjom T, Erchinger F, Tjora E, Lærum BN, Georg D, Gilja OH. Diagnostic accuracy of secretin-stimulated ultrasonography of the pancreas assessing exocrine pancreatic failure in cystic fibrosis and chronic pancreatitis. Scand J Gastroenterol. 2015;50:601–610. doi: 10.3109/00365521.2015.1004363. [DOI] [PubMed] [Google Scholar]
- 17.Conwell DL, Zuccaro G, Purich E, Fein S, Vargo JJ, Dumot JA, VanLente F, Lopez R, Trolli P. Comparison of endoscopic ultrasound chronic pancreatitis criteria to the endoscopic secretin-stimulated pancreatic function test. Dig Dis Sci. 2007;52:1206–1210. doi: 10.1007/s10620-006-9469-6. [DOI] [PubMed] [Google Scholar]
- 18.Catalano MF, Sahai A, Levy M, Romagnuolo J, Wiersema M, Brugge W, Freeman M, Yamao K, Canto M, Hernandez LV. EUS-based criteria for the diagnosis of chronic pancreatitis: the Rosemont classification. Gastrointest Endosc. 2009;69:1251–1261. doi: 10.1016/j.gie.2008.07.043. [DOI] [PubMed] [Google Scholar]
- 19.Hernandez LV, Catalano MF. EUS in the diagnosis of early-stage chronic pancreatitis. Best Pract Res Clin Gastroenterol. 2010;24:243–249. doi: 10.1016/j.bpg.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 20.Wallace MB, Hawes RH, Durkalski V, Chak A, Mallery S, Catalano MF, Wiersema MJ, Bhutani MS, Ciaccia D, Kochman ML, et al. The reliability of EUS for the diagnosis of chronic pancreatitis: interobserver agreement among experienced endosonographers. Gastrointest Endosc. 2001;53:294–299. doi: 10.1016/s0016-5107(01)70401-4. [DOI] [PubMed] [Google Scholar]
- 21.Afghani E, Sinha A, Singh VK. An overview of the diagnosis and management of nutrition in chronic pancreatitis. Nutr Clin Pract. 2014;29:295–311. doi: 10.1177/0884533614529996. [DOI] [PubMed] [Google Scholar]
- 22.Löhr JM. What are the useful biological and functional markers of early-stage chronic pancreatitis? J Gastroenterol. 2007;42 Suppl 17:66–71. doi: 10.1007/s00535-006-1932-9. [DOI] [PubMed] [Google Scholar]
- 23.Sarner M, Cotton PB. Classification of pancreatitis. Gut. 1984;25:756–759. doi: 10.1136/gut.25.7.756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dreiling DA, Hollander F. Studies in pancreatic function; preliminary series of clinical studies with the secretin test. Gastroenterology. 1948;11:714–729. [PubMed] [Google Scholar]
- 25.Chowdhury RS, Forsmark CE. Review article: Pancreatic function testing. Aliment Pharmacol Ther. 2003;17:733–750. doi: 10.1046/j.1365-2036.2003.01495.x. [DOI] [PubMed] [Google Scholar]
- 26.Shimosegawa T, Kataoka K, Kamisawa T, Miyakawa H, Ohara H, Ito T, Naruse S, Sata N, Suda K, Hirota M, et al. The revised Japanese clinical diagnostic criteria for chronic pancreatitis. J Gastroenterol. 2010;45:584–591. doi: 10.1007/s00535-010-0242-4. [DOI] [PubMed] [Google Scholar]
- 27.Shibukawa G, Irisawa A. Diagnostic efficacy of a brand-new endoscopic ultrasound processor for early-stage chronic pancreatitis. Dig Endosc. 2015;27 Suppl 1:75. doi: 10.1111/den.12430. [DOI] [PubMed] [Google Scholar]
- 28.Bornman PC, Botha JF, Ramos JM, Smith MD, Van der Merwe S, Watermeyer GA, Ziady CC. Guideline for the diagnosis and treatment of chronic pancreatitis. S Afr Med J. 2010;100:845–860. doi: 10.7196/samj.4530. [DOI] [PubMed] [Google Scholar]
- 29.Arcidiacono PG. Endoscopic ultrasound elastography. Gastroenterol Hepatol (N Y) 2012;8:48–67. [PMC free article] [PubMed] [Google Scholar]
- 30.Iglesias-Garcia J, Domínguez-Muñoz JE, Castiñeira-Alvariño M, Luaces-Regueira M, Lariño-Noia J. Quantitative elastography associated with endoscopic ultrasound for the diagnosis of chronic pancreatitis. Endoscopy. 2013;45:781–788. doi: 10.1055/s-0033-1344614. [DOI] [PubMed] [Google Scholar]
- 31.Dominguez-Muñoz JE, Iglesias-Garcia J, Castiñeira Alvariño M, Luaces Regueira M, Lariño-Noia J. EUS elastography to predict pancreatic exocrine insufficiency in patients with chronic pancreatitis. Gastrointest Endosc. 2015;81:136–142. doi: 10.1016/j.gie.2014.06.040. [DOI] [PubMed] [Google Scholar]
- 32.Lindkvist B, Domínguez-Muñoz JE, Luaces-Regueira M, Castiñeiras-Alvariño M, Nieto-Garcia L, Iglesias-Garcia J. Serum nutritional markers for prediction of pancreatic exocrine insufficiency in chronic pancreatitis. Pancreatology. 2012;12:305–310. doi: 10.1016/j.pan.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 33.Lindkvist B. Diagnosis and treatment of pancreatic exocrine insufficiency. World J Gastroenterol. 2013;19:7258–7266. doi: 10.3748/wjg.v19.i42.7258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.DiMagno EP, Go VL, Summerskill WH. Relations between pancreatic enzyme ouputs and malabsorption in severe pancreatic insufficiency. N Engl J Med. 1973;288:813–815. doi: 10.1056/NEJM197304192881603. [DOI] [PubMed] [Google Scholar]
- 35.Lankisch PG, Lembcke B, Wemken G, Creutzfeldt W. Functional reserve capacity of the exocrine pancreas. Digestion. 1986;35:175–181. doi: 10.1159/000199364. [DOI] [PubMed] [Google Scholar]
- 36.Conwell DL, Zuccaro G, Morrow JB, Van Lente F, Obuchowski N, Vargo JJ, Dumot JA, Trolli P, Shay SS. Cholecystokinin-stimulated peak lipase concentration in duodenal drainage fluid: a new pancreatic function test. Am J Gastroenterol. 2002;97:1392–1397. doi: 10.1111/j.1572-0241.2002.05675.x. [DOI] [PubMed] [Google Scholar]
- 37.Mizuno R, Hayakawa T, Noda A. Elastase secretion in pancreatic disease. Am J Gastroenterol. 1985;80:113–117. [PubMed] [Google Scholar]
- 38.Carrière F, Renou C, Ransac S, Lopez V, De Caro J, Ferrato F, De Caro A, Fleury A, Sanwald-Ducray P, Lengsfeld H, et al. Inhibition of gastrointestinal lipolysis by Orlistat during digestion of test meals in healthy volunteers. Am J Physiol Gastrointest Liver Physiol. 2001;281:G16–G28. doi: 10.1152/ajpgi.2001.281.1.G16. [DOI] [PubMed] [Google Scholar]
- 39.Carrière F, Grandval P, Renou C, Palomba A, Priéri F, Giallo J, Henniges F, Sander-Struckmeier S, Laugier R. Quantitative study of digestive enzyme secretion and gastrointestinal lipolysis in chronic pancreatitis. Clin Gastroenterol Hepatol. 2005;3:28–38. doi: 10.1016/s1542-3565(04)00601-9. [DOI] [PubMed] [Google Scholar]
- 40.Keller J, Layer P. Human pancreatic exocrine response to nutrients in health and disease. Gut. 2005;54 Suppl 6:vi1–v28. doi: 10.1136/gut.2005.065946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sikkens EC, Cahen DL, van Eijck C, Kuipers EJ, Bruno MJ. Patients with exocrine insufficiency due to chronic pancreatitis are undertreated: a Dutch national survey. Pancreatology. 2012;12:71–73. doi: 10.1016/j.pan.2011.12.010. [DOI] [PubMed] [Google Scholar]
- 42.Sikkens EC, Cahen DL, Koch AD, Braat H, Poley JW, Kuipers EJ, Bruno MJ. The prevalence of fat-soluble vitamin deficiencies and a decreased bone mass in patients with chronic pancreatitis. Pancreatology. 2013;13:238–242. doi: 10.1016/j.pan.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 43.Duggan SN, Smyth ND, O’Sullivan M, Feehan S, Ridgway PF, Conlon KC. The prevalence of malnutrition and fat-soluble vitamin deficiencies in chronic pancreatitis. Nutr Clin Pract. 2014;29:348–354. doi: 10.1177/0884533614528361. [DOI] [PubMed] [Google Scholar]
- 44.Duggan SN, Purcell C, Kilbane M, O’Keane M, McKenna M, Gaffney P, Ridgway PF, Boran G, Conlon KC. An association between abnormal bone turnover, systemic inflammation, and osteoporosis in patients with chronic pancreatitis: a case-matched study. Am J Gastroenterol. 2015;110:336–345. doi: 10.1038/ajg.2014.430. [DOI] [PubMed] [Google Scholar]
- 45.Duggan SN, Smyth ND, Murphy A, Macnaughton D, O’Keefe SJ, Conlon KC. High prevalence of osteoporosis in patients with chronic pancreatitis: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2014;12:219–228. doi: 10.1016/j.cgh.2013.06.016. [DOI] [PubMed] [Google Scholar]
- 46.Tignor AS, Wu BU, Whitlock TL, Lopez R, Repas K, Banks PA, Conwell D. High prevalence of low-trauma fracture in chronic pancreatitis. Am J Gastroenterol. 2010;105:2680–2686. doi: 10.1038/ajg.2010.325. [DOI] [PubMed] [Google Scholar]
- 47.Bang UC, Benfield T, Bendtsen F, Hyldstrup L, Beck Jensen JE. The risk of fractures among patients with cirrhosis or chronic pancreatitis. Clin Gastroenterol Hepatol. 2014;12:320–326. doi: 10.1016/j.cgh.2013.04.031. [DOI] [PubMed] [Google Scholar]


