Abstract
This report describes two cases of disseminated cutaneous Mycobacterium chelonae after hematopoietic stem cell transplantation (HSCT).
Keywords: Mycobacterium chelonae, Hematopoietic stem cell transplantation, Chronic graft versus host disease
This report describes two cases of disseminated cutaneous Mycobacterium chelonae after hematopoietic stem cell transplantation (HSCT).
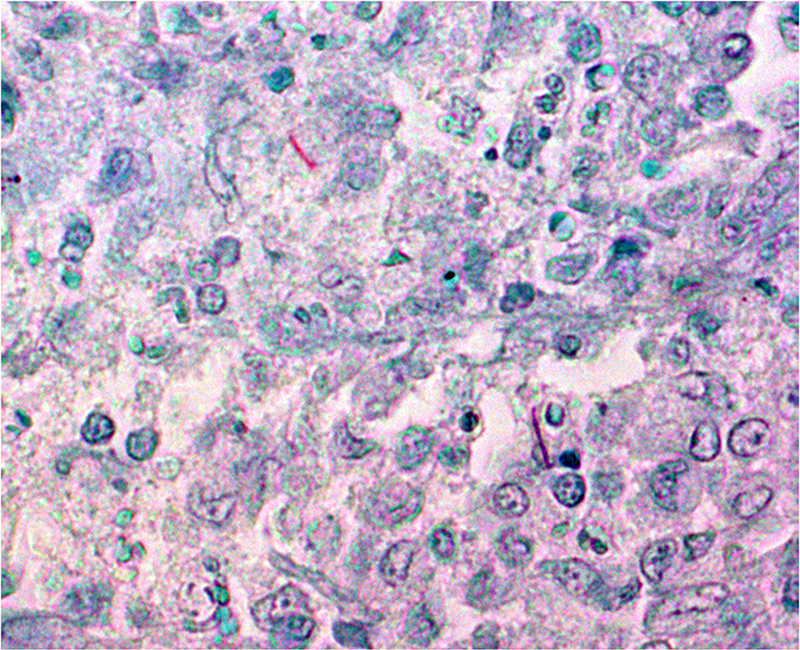
Both patients were 57-years-old and received an unrelated peripheral HSCT for malignant hematologic disease (follicular lymphoma and myelofibrosis). Both developed chronic graft-versus-host-disease (cGVHD) and received prolonged systemic steroids. They subsequently developed multiple erythematous subcutaneous nodules on legs and arms (eleven months after transplantation for patient #1 and eighteen months for patient #2; Fig. 1). Biopsies of subcutaneous nodules revealed a septal panniculitis with granulomatous components. The Ziehl-Neelsen stain (Fig. 2) was positive and culture identified M. chelonae. Hemocultures were negative.
Fig. 1.
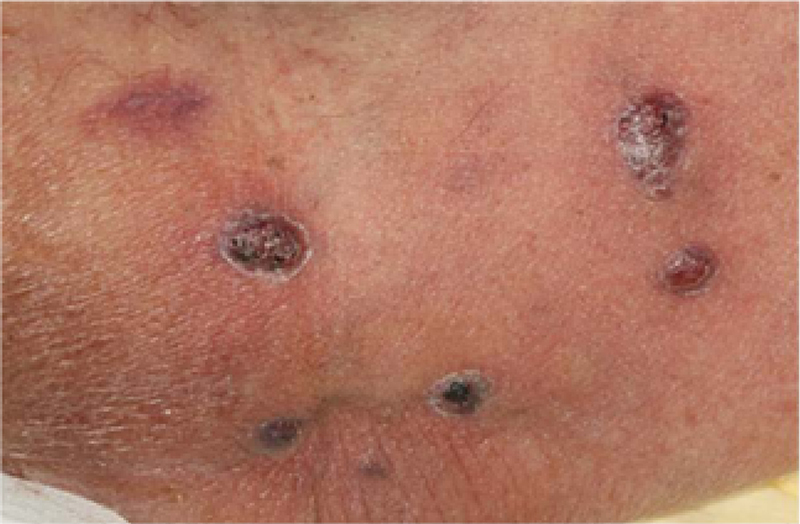
Fig. 2.
Patient #1 was treated with a combination of clarythromycin, tobramycin and tigecycline. The nodules rapidly decreased. However he died three months later of cardiac failure in a context of uncontrolled cGVHD and Enterococcus faecium sepsis. Patient #2 responded well to treatment with azithromycin, imipinem and tobramycin was then given azithromycin alone.
M. chelonae is a rapidly growing non-tuberculous mycobacteria isolated from various environmental sources. Water is a major source of contamination. M. chelonae infections are usually described in the setting of immunosuppression and particularly in patients receiving steroids therapy. After HSCT, M. chelonae infections are mostly due to central venous catheters or pulmonary infections, and skin involvement has not yet been described in previous reports.
In our two patients, prolonged steroid therapy led to skin atrophy with multiple lesions on limbs. Microbiological analyses of water of one hospital were performed and were positive for M. chelonae. As none of the patients had signs of disseminated infection, it can therefore be hypothesized that a possible source of contamination in our patients was tap water used for washing.
In conclusion, cutaneous M. chelonae infection should be suspected in HSCT recipients developing isolated subcutaneous nodules in the context of cGVHD.
Conflict of interest
None.
Author contributions
All authors have contributed equally to the manuscript.


