Abstract
Objectives
General practitioner (GP)-led urgent care centres were established to meet the growing demand for urgent care. Staff members working in such centres are central in influencing patients’ choices about which services they use, but little is known about staff perceptions of patients’ motives for attending urgent care. We hence aimed to explore their perceptions of patients’ motives for attending such centres.
Design
A phenomenological, qualitative study, including semistructured interviews. The interviews were analysed using thematic content analysis.
Setting
2 GP-led urgent care centres in 2 academic hospitals in London.
Participants
15 staff members working at the centres including 8 GPs, 5 emergency nurse practitioners and 2 receptionists.
Results
We identified 4 main themes: ‘Confusion about choices’, ‘As if increase of appetite had grown; By what it fed on’, ‘Overt reasons, covert motives’ and ‘A question of legitimacy’. The participants thought that the centres introduce convenient and fast access for patients. So convenient, that an increasing number of patients use them as a regular alternative to their community GP. The participants perceived that patients attend the centres because they are anxious about their symptoms and view them as serious, cannot get an appointment with their GP quickly and conveniently, are dissatisfied with the GP, or lack self-care skills. Staff members perceived some motives as legitimate (an acute health need and difficulties in getting an appointment), and others as less legitimate (convenience, minor illness, and seeking quicker access to hospital facilities).
Conclusions
The participants perceived that patients attend urgent care centres because of the convenience of access relative to primary care, as well as sense of acuity and anxiety, lack self-care skills and other reasons. They perceived some motives as more legitimate than others. Attention to unmet needs in primary care can help in promoting balanced access to urgent care.
Keywords: ACCIDENT & EMERGENCY MEDICINE, QUALITATIVE RESEARCH, PRIMARY CARE
Strengths and limitations of this study.
The study addresses the topical issue of patient access to urgent care, a core policy concern in the UK and many other countries.
This study provides a glimpse into ambiguous staff perception on patients’ motives for attending urgent care centres, based on their daily experience of seeing patients in such centres.
The convenient access relative to primary care was perceived as the main reason for increasing demand for urgent care centres. Hence, the urgent care centres might serve as a ‘panacea’, responding to unmet needs in primary care.
Patient motives for attending the urgent care centres described here are as perceived by staff, not by patients themselves.
The findings are limited to the two centres which were studied.
Introduction
General practice and emergency medicine are traditionally the two main methods by which the UK population gains access to the National Health Service (NHS). While general practice provides long-term care and a continuous patient–doctor relationship, emergency medicine focuses on acute care. The demand for urgent and emergency care is multifactorial and includes epidemiological factors such as the ageing population,1–4 and social factors such as loneliness and lack of family support,1 4 improved health awareness and community expectations arising from health promotion campaigns and organisational changes in primary care services that reduced access to primary care.1 Likewise, the convenience of a ‘one stop shop’ with a full range of specialists and diagnostic facilities also increases the demand for urgent care.1
The UK's NHS provides a full range of access to emergency and urgent care services, including ambulance services, major trauma and emergency services, minor injuries units and walk-in centres (mainly staffed by nurse practitioners and that have limited diagnostic facilities). Procedures to access primary care services in the UK can vary widely. In most practices, appointments are booked directly by patients either by telephone, in person or online. Some practices have implemented ‘triage systems’ in which a clinician will assess each request for an appointment and determine when and by which member of the primary care team the patient should be seen.
In 2000, the UK introduced a model of GP-led urgent care centres (UCCs) in response to increasing demand for urgent care, unplanned hospital attendances, delays in accessing healthcare and associated rising healthcare costs. UCCs had been similarly introduced to implement the government’s vision to extend access to NHS and to fit in with the contemporary lifestyle of people in the UK.5 Such centres are commonly co-located with Accident and Emergency (A&E) departments, have a wide range of diagnostic facilities, and are staffed by GPs and nurse practitioners. Hence, they offer a greater level of expertise and facilities than walk-in centres. Similar models have been implemented internationally.6 The rationale for the model is that many patients attend emergency departments (EDs) for minor and non-urgent conditions,7 and that GPs working in EDs are effective in reducing the need to undertake diagnostic procedures and in referring patients to see hospital specialists.8
Research questions
Previous studies have described the reasons why patients attend EDs and NHS walk-in centres,9–15 and particularly why non-urgent patients prefer to access EDs rather than their primary care.16 Yet, only a few touched on staff views of NHS walk-in centres,17 18 and mainly dealt with organisational and staffing issues. Staff attitudes towards which attendances are more appropriate than others are likely to influence their attitude towards patients and are a major potential source of patient dissatisfaction.12 Healthcare professionals working in UCCs are at the frontline in educating patients about self-management, the range of services available and where they should seek help from. Furthermore, patients’ judgements about urgency of need, and their choices about what services to use are guided by previous experiences of care.19 We hence aimed to explore staff perceptions of patients’ motives for attending GP-led UCCs. The specific research questions were: (1) what are the reasons that drive patients to attend the UCCs, as perceived by staff members working in such centres, and (2) how do staff members relate to these motives.
Methods
The service commissioned in the Hammersmith and Fulham borough in west London consists of two GP-led UCCs, co-located with A&E departments at Charing Cross and Hammersmith Hospitals. The service was commissioned by NHS Hammersmith and Fulham in April 2009 to manage the rising number of urgent attendances at local hospitals. The service is operated by Partnership for Health, a consortium of London Central and West Unscheduled Care Collaborative, Imperial College Healthcare NHS Trust and Central London Community Healthcare NHS Trust. The GP-led UCCs we used for this study act as a ‘front-entrance’ to the ED. Patients arriving to these centres are first triaged by a GP, and allocated to an appropriate care pathway based on risk stratification. Most patients attending for emergency care and managed by the clinicians in the UCC. A minority of patients with more severe problems bypass the UCC and go directly to the ED. Some patients who are seen in the UCC are also referred to the ED for further management. Since the Charing Cross UCC was opened in 2009, an additional 20 000 users attended the UCC and A&E departments annually (c. 90 000 users annually attending the UCC and A&E departments, relatively to c. 70 000 users annually who attended the A&E department solely before the UCC was opened. A detailed description of the model appears elsewhere.20 This study is a part of ongoing evaluation of these UCCs.20–22
Interview design
We conducted a phenomenological qualitative study. Phenomenological studies aim to describe the subjective reality of an event, as perceived by the study population, and hence is a proper tool to study attitudes, behaviours and motives.23 We designed a semistructured, open-ended interview protocol that is systematic, yet remains sensitive to the dynamics of the conversation. The interview focused on patients’ motives for attending the UCC and how the participants relate to these, as well as day-to-day practicalities of working in the GP-led urgent care model, teamwork, facilitators and barriers to of the model, and future improvements (see online supplementary appendix 1). The interview was designed to fit a time frame of 20–25 min to account for the intense work environment of the staff being interviewed. The final interview protocol was stabilised after the fourth interview.
Participants and sampling
We conducted interviews with 15 staff members working at the GP-led UCCs at Charing Cross and Hammersmith Hospitals in west London. To reflect the diversity of the sample in respect to different professions and level of expertise, we used the purposive sampling technique. The aim of purposive sample is not to establish a random or representative sample of a population but to capture accounts of various groups of people who—in this case—work at the same environment where a social phenomenon being studied.24 25 We used the method of Maximum variation sampling (heterogeneous sampling), which aims to capture a wide range of perspectives relating to the studied phenomenon. The principle behind this method is to capture diverse insights into a phenomenon by looking at it from views of various informants. Hence, we interviewed staff members from various professions and various clinical expertise levels to reflect a variety of perspectives and attitudes. The sample included eight GPs, five emergency nurse practitioners (ENPs) and two receptionists. Most of the participants worked on both sites and hence were able to reflect their experiences of the same model in different sites. There were 45 clinicians and receptionists at the centres at the time of the study; hence, the sample covered a third of the staff. Being a part of a service evaluation, the study did not require an ethical review by a NHS or Social Care Research Ethics Committee, in line with National Research Ethics Service Guidance.26
Data collection and analysis
The interviews took place in consultation rooms of the UCCs during off-peak times, between November and December 2012. The interviews were conducted by researchers experienced in gathering and analysing qualitative data (GG and AI). The interviews were audio-taped and transcribed verbatim while ensuring anonymity. We conducted a thematic content analysis which is an appropriate method under the hermeneutic, phenomenological approach. During the open coding, conducted independently by two researchers (GG and AI), we identified data categories and started to developed these codes into themes. We worked in an iterative process, in which identified themes led to creation of new codes. This process involved an analysis of each new interview and constant comparison with previous interviews. Axial coding then formed relationships between the various codes. Once codes and themes were shaped, we held ongoing discussions with the other researchers to discuss the initial interpretations. Data collection and open coding continued until saturation, when new information produced little or no change to coding and thematisation. We coded and analysed the data using the Atlas.ti V.7 software.
Results
The themes emerged from the thematic content analysis reflect issues concerning demand for care (ie, patients’ motives for coming to the UCC), patient–provider relationship, teamwork, interface with community GPs and cost-benefit of the model. In this article, we chose to focus on how staff members perceived patients’ motives for coming to the UCC, and how did they relate to these motives. Within this topic, we identified four themes: ‘Confusion about choices’, ‘As if increase of appetite had grown; By what it fed on’, ‘Overt reasons, covert motives’ and ‘A question of legitimacy’, which are presented below.
Confusion about choices
Several participants assumed that many patients are unaware of what the GP-led UCC is. They simply want someone to see them. They go to the hospital, where they can get a relatively prompt medical attention. Most of them do not distinguish between the ‘A&E department’, the ‘walk-in centre’ or the ‘UCC’, nor are aware of the aims of the UCC and the services it provides. Most of them are unaware of the triage system (ie, being first triaged and then allocated to a certain stream, and treat accordingly), and hardly notice whether they were seen by a doctor or an ENP. This is reasonable, because in both sites there is a single entrance to the UCC and A&E department, and referred to A&E department only after triage in the UCC:
Obviously, if they have an injury, they'll come to A&E…however, they don't realise they're being seen in an Urgent Care Centre. More often than not, we have to tell them…They think they're still being seen in A&E, unless you tell them, no, it's not A&E, it's the Urgent Care Centre. (ENP3)
Well, the patients come, I think, many of them still see it as an A&E department; some see it as casualty, but I think, most people have forgotten that name, and see it as an A&E department, and they go, perceiving that—many of them think—they have a true emergency, and really need the hospital services. (GP5)
“As if increase of appetite had grown; By what it fed on”
The service was perceived by the participants as popular and successful in attracting new patients and in providing high-quality service, described with a sense of pride. The participants described the success in objective measures such as number of patients who come to the centres, patient satisfaction rates, meeting waiting time targets, succeeding in diverting minor cases from the A&E department and hence reducing the number of more expensive attendances, but also by the fact that the local model has been replicated in other locations across the UK and internationally:
Nationally we are one of the best in the country in terms of the way we sort patients, the speed with which patients go through the service, the quality of the service, complaints are tiny, two or three complaints a year, most of which are not upheld. (GP1)
Shakespeare's quote (see below), brought up by one of the participants, summarised what many of the participants told us. The quote conveyed both a sense of pride in attracting many patients, but also a concern about whether the supply creates superfluous demand. The phrase ‘becoming a victim of our success’, mentioned by several participants, raises more questions than answers: is it a sense of pride? If so, why a ‘victim’? Is it a concern about increasing workload? Is it a concern about whether the public is well informed about when should one attend the UCC? To which elements of ‘success’ do they refer to? Is it merely the volume of patients who attend to the UCC, patient satisfaction, short waiting times, good outcomes of care or the ability to compensate for perceived flaws of the community primary care?
I think some community GPs could definitely improve their access, but when you increase your access you can…what Shakespeare wrote in Hamlet talking of his mother's love for Hamlet's father, why it was as if hunger had increased by what it fed upon. So the more they get access to the GP, the more they'll go there for minor things at a very early stage, they won't wait. So you can become a victim of too much good access… (GP15)
Overt reasons, covert motives: perceived patient motives for attending the UCC
The participants mentioned several motives that they thought patients had for attending the UCC, and realised that many patients attend for a mixture of motives, not a single one. An underlying theme here was ‘Overt reasons, covert motives’, describing how some of the reasons expressed by patients, mask underlying reasons for attending the UCC. The most obvious and overt motive stated by patients attending the UCC, mentioned by the participants, is that patients seek urgent (at least in their view) medical attention, especially during out-of-hours. That could be a minor injury or an acute illness. Another overt reason given by patients is that they could not get an appointment with their GP. But these overt reasons frequently mask, according to the participants, deeper concerns patients have, particularly with the general practice, such as dissatisfaction with their GP, anxiety, inconvenience of appointment hours and wishing to discuss a clinical matter anonymously. Some of these motives are described below. Example quotes are brought in online supplementary appendix 2.
Anxiety (‘worried well’): Anxiety was mentioned as a major motive for coming to the UCCs. A sense of urgency that imposes coming to UCC instead of waiting to see their GP, or after seeing their GP, is commonly induced by anxiety and need for reassurance. Those were referred to by the participants as the ‘worried well’.
Convenient access: Most of the participants mentioned that many users of the UCC attend because of the convenience access, for example, because the UCC is close to their work and they can go at lunchtime or after work, which was reflected by increase in attendances around noon and 17:00. The UCC offers convenient access for commuters who cannot get an early morning or late evening appointments with their GP. The difficulty in getting an appointment with community GPs is confronted by the convenient access to the UCCs. The participants mentioned that patients are aware that they are very unlikely to get an appointment with their GP on the same day, and coming to the UCC is easier and quicker.
Belief in superiority of hospital expertise and seeking fasten access to hospital facilities: Another group of patients who attend the UCC, mentioned by the participants, are those who perceive their symptoms to be too serious or too urgent to be dealt with in community settings. The participants mentioned that some UCC attendees seek fastened access to hospital facilities and equipment unavailable at their GP practice, such as scans; or those who saw their GP as incompetent and sought to see a specialist quickly. With GPs acting as gatekeepers of accessing specialist care and long waiting times for the secondary care, attending the UCC is seen by patients a viable option. Most patients are unaware that the UCC can refer them to specialists and scans only in urgent and complex cases.
Dissatisfaction with GP: The participants told us that some patients attend the UCC regularly as an alternative to their community GP. While it is commonly masked by the patient claiming that they ‘cannot get an appointment with the GP’, the participants explained that the patients’ dissatisfaction stems from deeper motives rather than just the technicality of getting an appointment. Dissatisfaction with their GP was frequently mentioned as an underlying motive. It may reflect the patients’ dissatisfaction from the communication with the GP, feeling that they were not listened to. Likewise, for many patients, particularly the younger ones, lack of continuity of care is well weighted against the benefits the UCC offers. The participants remarked that some patients attend the UCC because they wish to discuss a concern which they do not want their GP to be involved for any particular reason, or getting a second opinion.
Those unregistered with a GP: Another group of people who attend the UCC is those unregistered with a GP for various reasons, such as students and people in transitions, tourists and immigrants, for whom the UCC is the only place where they can get medical advice (though not all of these groups are eligible for free access).
Lack of self-care skills: Lack of self-care skills was mentioned as another reason for attending the UCCs, which also reflects the view that easy access increased attendances for minor symptoms.
A question of legitimacy: what makes a ‘legitimate’ and ‘illegitimate’ attendance?
Beyond the motives that the participants attribute to patients attending the UCC, it is useful to describe how they related to these motives. Coming to the UCC in honest need for urgent medical attention was perceived as legitimate. The participants also realised that people often get anxious about symptoms that seem acute to them, although there is no real clinical urgency. Yet, ambiguity surrounded staff perceptions of some of the motives (table 1). For example, those unregistered with a GP (students away from home, tourists, people in transit, etc) and commuters to central London who cannot access their GP if they are unwell were perceived legitimate, as apparent in the first quote below. However, there was a distinction between these people and those who should register with a GP but do not do so, and those registered with a GP but using the UCC to sort out ongoing conditions, as apparent in the second quote:
I think it's there for all those people that are not in the system, number one, and that's appropriate use. At the end of the day, if you suddenly are ill and you're in the city of a civilised country, thank God, you can pitch up here and someone will see you and not demand a credit card…I don't think it's a malicious abuse. Every now and again someone is trying to jump a bit, but I don't think that's the main bit of it. I think they just don't know. (GP15)
There's some things are a bit more frustrating for me as a clinician and for the patients, and that's sometimes people come in with a problem that's gone on for weeks or months even, and they come in. Because it's a hospital they think that we can, or they assume that we…because it's a hospital, they've come here, we can deal with the problem very quickly or we can sort them out… (GP7)
Table 1.
Staff attitudes towards perceived patient motives for coming to the UCC
| Motives perceived as legitimate | Motives perceived as less legitimate |
|---|---|
|
|
GP, general practitioner; UCC, urgent care centre.
There was also an ambiguous view on the convenient access to the UCCs. Honest difficulties in getting an appointment with a GP were perceived as a legitimate reason to attend the UCCs, as apparent in the first quote below. However, there was a critical tone towards those who use the service for sheer connivance and an excuse to fasten access; it is not that they cannot get an appointment, they just cannot get it quickly and conveniently, as apparent in the other quotes below:
There was someone who came in, I think about two weeks ago, and they said they phoned their GP for an appointment and there was literally nothing for a month and I phoned up and said can this person be seen any quicker than that…I verified it myself and there was no, there were no GP appointments for a month unless, apart from urgent appointments. (ENP4)
And part of the problem is they say, I can't get to see my GP. I can tell you increasingly patients are being mendacious in this respect…So I don't buy that patients can't get…When they say I can't get to see my GP for ten days, frankly that's not true. If they really wanted to get to see their GP and were prepared to go when the GP offered a queue-up access, they would. (GP15)
It's very difficult because there are a lot of patients who try to, I don't know if abuse the system's the right word but certainly get access. They come in, they're not registered or they want free prescriptions, things like that because they know we keep medications on site here so that's very difficult when you're trying to balance between how you manage these patients clinically. (ENP6)
Coming to the UCC with minor ailments that could be self-managed, and attempts to shorten waiting time for imaging and secondary care were also perceived as less legitimate:
…So, there can be abuse of the system in that respect but, yeah, sometimes when people come in with a sore throat…I think it does clog up the system quite a lot for genuine people who actually, really, need a service. (Receptionist11)
While participants understood, and do not necessarily judge these motives to be illegitimate, there was an underlying critical tone, as they were thought to divert resources from patients in real need and costly to the system.
We tried to compare the opinions of the GPs, nurses and receptionists with regard to the differences or similarities between their accounts, and this comparison raised meaningful differences that refer to other subjects not covered in this manuscript such as teamwork, professional hierarchy, patient–physician communication and the sustainability of the model. With regard to patient motives for attending the UCCs, the variability in opinions was more related to personal opinions and values of individual professionals rather than to them belonging to a certain professional group.
Discussion
What have we learned in this study?
This study provides a glimpse into ambiguous staff perceptions on people's motives for attending UCCs. The findings highlight two main issues. First, their concern about whether the very convenient access to the UCCs created, as an unintended consequence, superfluous demand for attendances for non-urgent problems. But beyond the concern about increase in usage, there was an underlying discussion on the legitimacy of usage. The participants perceived some motives as more legitimate (such as acute health needs, honest difficulties in access to general practice, anxiety; and other motives as less legitimate (such as sheer convenience, minor ailments that could be self-managed, using the UCC as their regular GP, and seeking access to hospital facilities). The participants told us that many patients attend the UCC because of what they overtly present as difficulty or inability to get an appointment with their GP. But this ‘technicality’ was perceived as commonly masking deeper issues, reflecting unmet needs in the primary care, such as strong gatekeeping on access to specialists, hasty appointments and feeling not being listened to.
The findings in relation to other studies
While we are unaware of previous work on staff perceptions on the NHS UCCs, it is possible though to compare staff perceptions found here to similar services such as EDs and A&E departments. The most common reason mentioned by professionals for patients attending EDs is difficulties in access to general practice.27 28 Other reasons mentioned by ED clinicians were healthcare consumerism (patients wanting to decide how and when they should undergo treatment, wanting everything immediately and indiscriminately), and the perception that the consultation is free,27 lack of knowledge concerning GP services and GP availability, lack of understanding of the function of EDs, and inadequate health education.29 Clinicians working in ED in Ireland believed that appropriate attendances are those when the patient believes condition is serious or urgent, when the patient is subsequently admitted to the hospital, or requires an X-ray. Less legitimate attendances were those where the patient arrives by ambulance, wishes to seek a second opinion, prefers to be seen in the ED, has a psychiatric problem, is unable to see usual GP, can access ED more easily than elsewhere, have social issues they believe can be dealt with in the ED, does not have regular GP, requires a blood test or that the time after injury/illness is more than 48 h.30
Another valid comparison of our findings, though not directly related to the aim of this paper, is whether patient motives as reflected from professionals coincide with motives described by patients themselves. The motives described here by professionals resonance on motives described by patient themselves. A main reason for attending urgent care was lack of access to primary care.31 32 About a half NHS UCCs attendees reported that their reason for using a UCC was that they were unable to see their own GP.11 13 Patients also prefer to attend urgent care settings rather than their community GP because they are anxious about presenting the problem and unaware of alternative pathways,13 because they perceive the need for diagnostic facilities,33 or that the hospital specialist was best qualified to handle the problem, or that their symptoms are acute,31 32 or are dissatisfied with their GP.14 Positive experience of an urgent care department in the past may also attract patient to reattend.19 31 32 Unlike professionals, patients rarely perceive they attended for convenience—they simply sought a quicker and better medical care.28
The challenges raised by the results
Looking at the bigger picture, this discussion is part of a broader discussion on how healthcare systems should cope with the increasing demands for care in an era of financial austerity.34 Concerns about the increasing usage of urgent care is a major health policy question in the UK. The average occupancy of England's A&E units increased by around 8% between 2010/2011 and 2012/2013 (yet attendance rates have only increased in line with what would be expected from population growth).35
The question of the appropriateness of urgent care attendances trails back to the 1970s.7 28 36 37 But from the patient view, as reflected here by staff members, the UCC is allegedly a good solution to these concerns: it offers a free 24/7 access to medical care, at convenient locations, a prompt appointment with a clinician, no booking required, access to specialists and imaging facilities (limited to severe conditions only), and a longer consultation time without being rushed. Indeed, patients are mostly very satisfied with their visit to NHS UCCs11 12 and perceive these centres as a means to improve access to care.10 Patients prefer to attend EDs as rational consumers: because they had difficulties obtaining a rapid appointment with their GP, and because the access to technical facilities in EDs spares them from being overwhelmed with appointments with various specialists.27
What are the consequences or impact of providers’ attitudes?
Professionals as human beings inevitably have attitudes towards patients and these attitudes, whether natural, positive or negative, are inevitably ‘in’ the consultation room, and may affect the way they communicate with patients and the treatment they provide. Behavioural models stress a link between attitude and behaviour.38 Heritage and Maynard39 described in detail the reasons patients provide for seeking urgent medical care and how doctors react to such reasons. Strivers39 described the negotiations between doctors and parents in acute care encounters. Empirically, there is evidence showing that professionals’ attitudes towards ‘difficult patients’ affect their type and quality of treatment they provide.40 41 There is also a well-established link between the quality of the patient–physician communication patient satisfaction and compliance, which have a clear link to health outcomes.42 Physicians that are satisfied with the patient–physician communication are more likely to be satisfied from their work, and to have satisfied patients.42
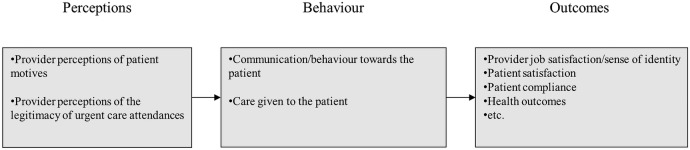
Clinicians’ attitudes towards patient motives for attending the UCC, and their perceptions of the legitimacy or appropriateness of the attendance, may appear in various levels (figure 1): (1) in the communication with the patient and the behaviour towards the patient; (2) the care being given to the patient; (3) in their job satisfaction and sense of identity; and (4) in the patient satisfaction from the care provided to them in the UCC. For example, if the clinician believes that the attendance is appropriate, they may have a more positive attitude towards the patient and be naturally more keen to help the patient. They may ‘go the extra mile’ to really understand the patient's concern, order relevant examinations and consider various treatment avenues. Eventually, they may end up being more satisfied from their work by helping a patient in need. Then, the patient is more likely to be satisfied, and if patients are very satisfied from the care they received, they may be inclined to come back.19 They may be more compliant with the treatment given by the clinician, and hence may recover quickly.
Figure 1.
The linkage between perceptions, behaviour and outcomes.
Provider attitudes are inevitably communicated to the patient, either verbally or through body language, and may affect the patient satisfaction, and make the patient to want to return to the UCC or to seek help elsewhere.19 Provider opinions about why patients come to the UCCs may have an impact on how they guide them about which services they should go to. For example, if the clinician think the attendance was appropriate, they may say nothing to the patient; however, if they felt it was inappropriate, they might highlight to the patient the appropriate services to approach in future cases.
Staff attitudes towards which attendances are more appropriate than others are likely to influence their attitude towards patients and are a major source of patient dissatisfaction.12 If they felt the attendances is inappropriate, they may naturally be less sympathetic towards the patient, will make less effort to help the patient and may feel less satisfied with their work. A negative doctor–patient interaction was found to be predictive of more frequent attendance in irritable bowel syndrome.43 Likewise, if a clinician thinks that the UCC should accept every patient regardless of the urgency of their symptoms, or if they believe that none of the ‘convenience’ related attendances should not be seen in the UCC, this may have an impact on their attitude towards the patient and the way they will treat and communicate with the patient.
Policy implications
The findings raise three policy implications. The first policy question is whether treating every ‘legitimate’ or ‘illegitimate’ complaint as an emergency which has to be attended to immediately is appropriate? On one hand, 24/7 access to free urgent care is an essential element of modern society. Claims that patients misuse the service might be wrong: many A&E department attendances are indeed justified,44 45 and on the contrary to ‘urban legends’,12 patients are very mindful not to overuse the NHS.10 But on the other hand, in an era of financial austerity, should national tax-funded UCCs serve as a panacea of the healthcare system, the last resort for all patients who cannot access their GPs, or those dissatisfied with their GP? Maybe patients should be asked to call a central help line before attending a UCC, where the problem is assessed by a professional concerning urgency of the matter and consequently the patient referred to the UCC, or asked to wait for an appointment at the GP? There is no right or wrong; this is a philosophical and political decision of the health service system. Likewise, other out-of-hours care models, such as the GP cooperative and the rota group could be considered, due to their strengths in comparison to the traditional A&E department.46
The second policy question is on the role of UCCs as a response to what patients perceived as unsatisfactory primary care. The lack of proper response from the primary care is well documented as one of the many reasons for increasing urgent care attendances.11 13 14 31 47 But is increased access to urgent care facilities the right solution? Attention to unmet needs can guide on how community GPs can adjust to meet current patient needs. If patients indeed use the UCC as a solution to inconvenient primary care, efforts to reduce urgent care should hence aim at strengthening community care. Such care would adjust to contemporary lifestyle, including early morning, late evening and weekend appointments, and enable longer consultation time to proper attention to patient concerns. Indeed, general practices providing more timely access to primary care have fewer self-referred discharged ED visits.48 Providers in the community, while being generally positive towards the concept of hospital-based UCCs, have a general feeling that limited NHS resources may be spent more appropriately in other settings.49 This though would require some radical changes to the contract between the NHS and GPs, and in the way in which general practice in the UK is funded.34 With such a solution, patients can enjoy both worlds: continuity of care together with extended access, which can potentially reduce urgent care attendances.
The third policy implication is about providing patients with more self-care skills and more information about different care and out-of-hours options. As apparent in our data and previous literature,29 many patients currently lack basic self-care skills and lack an understanding of the function of UCCS versus A&E departments, which might create confusion about choices and increase the number of attendances for minor ailments.
Strengths and limitations
This study gives a novel glimpse into staff perception on service users’ motives for using urgent care services, which has not been covered previously in the literature. The findings reflect perceptions of different types of staff, including GPs, nurses and receptionists. Yet, we acknowledge several limitations. First, patient motives for attending the UCC are described here as perceived by staff, not by patients themselves. However, there is prior research on patient perceptions on reasons for attending urgent care departments. Hence, we aimed to provide a novel approach, reflecting the daily experience of staff in seeing patients in the UCCs, as a complementary angle to this prior strand of research. Using ‘second-hand’ data is a valid approach in qualitative research which can broaden our understanding particularly on how things look like from the ‘other’ perspective.50–54 While we acknowledge the obvious limitation of second-hand data in its limited ability to state what are the ‘real’ accounts of the ‘second-hand’ person (patients in this case), this was the only way we could compare between what patients report as their reasons for attending and how things look like from the provider's perspective. Second, the generalisability of findings is limited as the interviews were conducted in academic hospitals in one city, interviews only performed during off-peak times and during 2 months (November and December), and the sample size (which yet fairly meeting the recommended sample size for qualitative studies55). Finally, interviewing staff might introduce a ‘Hawthorne effect’ as participants feeling evaluated might emphasise the more successful elements. We tried to minimise it reassuring the participants that we aimed to capture their authentic experience rather than ‘evaluating the model’.
Conclusions
The GP-led UCC is an innovative response to increasing demand for urgent care. Professionals working in an UCC perceived it as providing fast, safe and convenient access to care and this convenience made it popular among patients. So convenient, so patients gradually use it as an alternative to their community primary care. The overt motive commonly reasoned to the professionals by patients, is inability to get an appointment with their GP. But this ‘technicality’ commonly masks covert issues, reflecting unmet needs in the community GP, such as inflexible appointment hours, dissatisfaction or lack of trust in their GP, anxiety and need for reassurance. Patients attend the UCC from motives that were perceived legitimate by the participants, such as an authentic need for urgent medical attention and honest difficulties getting an appointment with their GP, but also for motives perceived less legitimate, such as sheer convenience and attempts to shorten waiting time. Attention to unmet needs in the primary care can help in designing a balanced access to urgent care.
Acknowledgments
The authors thank all the staff that have and currently work for Partnership for Health in setting up the services; and staff at Hammersmith and Charing Cross Emergency Departments for their help. They also thank Professor Chris Salisbury for his advice on the evaluation. Partnership for Health is a consortium of London Central and West Unscheduled Care Collaborative, Imperial College Healthcare NHS Trust and Central London Community Health Services.
Footnotes
Contributors: GG conducted the interviews, analysed the data and drafted the manuscript. AI conducted the interviews, analysed the data, helped to draft the manuscript and revised of the manuscript. SG helped in interpretation of the data, helped to draft the manuscript and revised the manuscript. MB, TL and HM participated in its design and coordination and revised the manuscript. JC and AM initiated the study, participated in its design and coordination, and revised the manuscript. All authors read and approved the final manuscript.
Funding: The new service model was funded by NHS Hammersmith & Fulham. The Department of Primary Care & Public Health at Imperial College received funding from the Imperial College NHS Trust to help evaluate the new model. Support for the evaluation was also received from the NIHR CLAHRC for NW London.
Competing interests: GG, AI, SG, JC and AM were employed by Imperial College London, which received funding to help evaluate the new model of care. TL, HM, SG and JC were employed by Partnership for Health, the provider of this service.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Lowthian JA, Curtis AJ, Cameron PA et al. Systematic review of trends in emergency department attendances: an Australian perspective. Emerg Med J 2011;28:373–7. 10.1136/emj.2010.099226 [DOI] [PubMed] [Google Scholar]
- 2.Lowthian JA, Curtis AJ, Jolley DJ et al. Demand at the emergency department front door: 10-year trends in presentations. Med J Aust 2012;196:128–32. 10.5694/mja11.10955 [DOI] [PubMed] [Google Scholar]
- 3.Gruneir A, Silver MJ, Rochon PA. Emergency department use by older adults: a literature review on trends, appropriateness, and consequences of unmet health care needs. Med Care Res Rev 2011;68:131–55. 10.1177/1077558710379422 [DOI] [PubMed] [Google Scholar]
- 4.McCusker J, Karp I, Cardin S et al. Determinants of emergency department visits by older adults: a systematic review. Acad Emerg Med 2003;10:1362–70. 10.1111/j.1553-2712.2003.tb00011.x [DOI] [PubMed] [Google Scholar]
- 5.Department of Health. Up to £30 million to develop 20 NHS fast access walk-in centres. Press Release 19990226 1999.
- 6.Bosmans JE, Boeke AJ, van Randwijck-Jacobze ME et al. Addition of a general practitioner to the accident and emergency department: a cost-effective innovation in emergency care. Emerg Med J 2012;29:192–6. 10.1136/emj.2010.101949 [DOI] [PubMed] [Google Scholar]
- 7.Murphy AW. “Inappropriate” attenders at accident and emergency departments I: definition, incidence and reasons for attendance. Fam Pract 1998;15:23–32. 10.1093/fampra/15.1.23 [DOI] [PubMed] [Google Scholar]
- 8.Dale J, Green J, Reid F et al. Primary care in the accident and emergency department: II. Comparison of general practitioners and hospital doctors. BMJ 1995;311:427–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gerard K, Lattimer V. Preferences of patients for emergency services available during usual GP surgery hours: a discrete choice experiment. Fam Pract 2005;22:28–36. 10.1093/fampra/cmh623 [DOI] [PubMed] [Google Scholar]
- 10.Jackson CJ, Dixon-Woods M, Hsu R et al. A qualitative study of choosing and using an NHS Walk-in Centre. Fam Pract 2005;22:269–74. 10.1093/fampra/cmi018 [DOI] [PubMed] [Google Scholar]
- 11.Arain M, Nicholl J, Campbell M. Patients’ experience and satisfaction with GP led walk-in centres in the UK; a cross sectional study. BMC Health Serv Res 2013;13:142 10.1186/1472-6963-13-142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Palmer CD, Jones KH, Jones PA et al. Urban legend versus rural reality: patients’ experience of attendance at accident and emergency departments in west Wales. Emerg Med J 2005;22:165–70. 10.1136/emj.2003.007674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agarwal S, Banerjee J, Baker R et al. Potentially avoidable emergency department attendance: interview study of patients’ reasons for attendance. Emerg Med J 2012;29:e3–e3. 10.1136/emermed-2011-200585 [DOI] [PubMed] [Google Scholar]
- 14.Moll van Charante PM, ter Riet G, Bindels P. Self-referrals to the A&E department during out-of-hours: Patients’ motives and characteristics. Patient Educ Couns 2008;70:256–65. 10.1016/j.pec.2007.10.012 [DOI] [PubMed] [Google Scholar]
- 15.O'Cathain A, Coleman P, Nicholl J. Characteristics of the emergency and urgent care system important to patients: a qualitative study. J Health Serv Res Policy 2008;13(Suppl 2):19–25. 10.1258/jhsrp.2007.007097 [DOI] [PubMed] [Google Scholar]
- 16.Lega F, Mengoni A. Why non-urgent patients choose emergency over primary care services? Empirical evidence and managerial implications. Health Policy 2008;88:326–38. 10.1016/j.healthpol.2008.04.005 [DOI] [PubMed] [Google Scholar]
- 17.Rosen R, Mountford L. Developing and supporting extended nursing roles: the challenges of NHS walk-in centres. J Adv Nurs 2002;39:241–8. 10.1046/j.1365-2648.2002.02270.x [DOI] [PubMed] [Google Scholar]
- 18.Salisbury C, Chalder M, Scott TM et al. What is the role of walk-in centres in the NHS? BMJ 2002;324:399–402. 10.1136/bmj.324.7334.399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hunter C, Chew-Graham C, Langer S et al. A qualitative study of patient choices in using emergency health care for long-term conditions: The importance of candidacy and recursivity. Patient Educ Couns 2013;93:335–41. 10.1016/j.pec.2013.06.001 [DOI] [PubMed] [Google Scholar]
- 20.Gnani S, Ramzan F, Ladbrooke T et al. Evaluation of a general practitioner-led urgent care centre in an urban setting: description of service model and plan of analysis. JRSM Short Rep 2013;4:2042533313486263 10.1177/2042533313486263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Amiel C, Williams B, Ramzan F et al. Reasons for attending an urban urgent care centre with minor illness: a questionnaire study. Emerg Med J 2014;31:e71–5. 10.1136/emermed-2012-202016 [DOI] [PubMed] [Google Scholar]
- 22.Gnani S, McDonald H, Islam S et al. Patterns of healthcare use among adolescents attending an urban general practitioner-led urgent care centre. Emerg Med J 2014;31:630–6. 10.1136/emermed-2012-202017 [DOI] [PubMed] [Google Scholar]
- 23.Green J, Thorogood N. Qualitative methods for health research. Los Angeles: SAGE, 2009. [Google Scholar]
- 24.Barbour RS. Checklists for improving rigour in qualitative research: a case of the tail wagging the dog? BMJ 2001;322:1115–17. 10.1136/bmj.322.7294.1115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mays N, Pope C. Qualitative research: rigour and qualitative research. BMJ 1995;311:109–12. 10.1136/bmj.311.6997.109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.NHS Health Research Authority. NRES—Is your project research? http://www.nres.nhs.uk/applications/is-your-project-research/ (accessed 12 Sep 2013).
- 27.Durand A-C, Palazzolo S, Tanti-Hardouin N et al. Nonurgent patients in emergency departments: rational or irresponsible consumers? Perceptions of professionals and patients. BMC Res Notes 2012;5:525 10.1186/1756-0500-5-525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sanders J. A review of health professional attitudes and patient perceptions on “inappropriate” accident and emergency attendances. The implications for current minor injury service provision in England and Wales. J Adv Nurs 2000;31:1097–105. 10.1046/j.1365-2648.2000.01379.x [DOI] [PubMed] [Google Scholar]
- 29.Lewis BR, Bradbury Y. The role of the nursing profession in hospital accident and emergency departments. J Adv Nurs 1982;7:211–21. 10.1111/j.1365-2648.1982.tb00233.x [DOI] [PubMed] [Google Scholar]
- 30.Breen BM, McCann M. Healthcare providers attitudes and perceptions of “inappropriate attendance” in the Emergency Department. Int Emerg Nurs 2013;21:180–5. 10.1016/j.ienj.2012.08.006 [DOI] [PubMed] [Google Scholar]
- 31.Penson R, Coleman P, Mason S et al. Why do patients with minor or moderate conditions that could be managed in other settings attend the emergency department? Emerg Med J 2012;29:487–91. 10.1136/emj.2010.107276 [DOI] [PubMed] [Google Scholar]
- 32.Benger JR, Jones V. Why are we here? A study of patient actions prior to emergency hospital admission. Emerg Med J 2008;25:424–7. 10.1136/emj.2007.050856 [DOI] [PubMed] [Google Scholar]
- 33.Coleman P, Irons R, Nicholl J. Will alternative immediate care services reduce demands for non-urgent treatment at accident and emergency? Emerg Med J 2001;18:482–7. 10.1136/emj.18.6.482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Majeed A. General practice in the United Kingdom: meeting the challenges of the early 21st century. J R Soc Med 2013;106: 384–5. 10.1177/0141076813504326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.QualityWatch. The Health Foundation and the Nuffield Trust. A&E attendances. http://www.qualitywatch.org.uk/focus-on/ae-attendances (accessed 4 Nov 2014).
- 36.Richardson S. Emergency departments and the inappropriate attender—is it time for a reconceptualisation of the role of primary care in emergency facilities? Nurs Prax N Z Inc 1999;14:13–20. [PubMed] [Google Scholar]
- 37.Lowy A, Kohler B, Nicholl J. Attendance at accident and emergency departments: unnecessary or inappropriate? J Public Health Med 1994;16:134–40. [DOI] [PubMed] [Google Scholar]
- 38.Ajzen I, Fishbein M. Attitude-behavior relations: a theoretical analysis and review of empirical research. Psychol Bull 1977;84:888–918. 10.1037/0033-2909.84.5.888 [DOI] [Google Scholar]
- 39.Heritage J, Maynard DW, eds. Communication in medical care: interaction between primary care physicians and patients. 1st edn Cambridge, UK; New York: Cambridge University Pres, 2006. [Google Scholar]
- 40.Hahn SR, Kroenke K, Spitzer RL et al. The difficult patient: prevalence, psychopathology, and functional impairment. J Gen Intern Med 1996;11:1–8. 10.1007/BF02603477 [DOI] [PubMed] [Google Scholar]
- 41.Steinmetz D, Tabenkin H. The “difficult patient” as perceived by family physicians. Fam Pract 2001;18:495–500. 10.1093/fampra/18.5.495 [DOI] [PubMed] [Google Scholar]
- 42.Roter D. Doctors talking with patients/patients talking with doctors: improving communication in medical visits. 2nd edn Westport, CT; London: Praeger, 2006. [Google Scholar]
- 43.Owens DM, Nelson DK, Talley NJ. The irritable bowel syndrome: long-term prognosis and the physician-patient interaction. Ann Intern Med 1995;122:107–12. 10.7326/0003-4819-122-2-199501150-00005 [DOI] [PubMed] [Google Scholar]
- 44.van der Linden Mc, van den Brand C, van der Linden N et al. Rate, characteristics, and factors associated with high emergency department utilization. Int J Emerg Med 2014;7:9 10.1186/1865-1380-7-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McHale P, Wood S, Hughes K et al. Who uses emergency departments inappropriately and when—a national cross-sectional study using a monitoring data system. BMC Med 2013;11:258 10.1186/1741-7015-11-258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Huibers L, Giesen P, Wensing M et al. Out-of-hours care in western countries: assessment of different organizational models. BMC Health Serv Res 2009;9:105 10.1186/1472-6963-9-105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cowling TE, Harris M, Watt H et al. Access to primary care and the route of emergency admission to hospital: retrospective analysis of national hospital administrative data. BMJ Qual Saf. 2015. Aug 25. pii: bmjqs-2015-004338. 10.1136/bmjqs-2015-004338. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cowling TE, Cecil EV, Soljak MA et al. Access to primary care and visits to emergency departments in England: a cross-sectional, population-based study. PLoS ONE 2013;8:e66699 10.1371/journal.pone.0066699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pope C, Chalder M, Moore L et al. What do other local providers think of NHS walk-in centres? Results of a postal survey. Public Health 2005;119:39–44. 10.1016/j.puhe.2003.12.014 [DOI] [PubMed] [Google Scholar]
- 50.Wens J, Vermeire E, Royen PV et al. GPs’ perspectives of type 2 diabetes patients’ adherence to treatment: a qualitative analysis of barriers and solutions. BMC Fam Pract 2005;6:20 10.1186/1471-2296-6-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sale JEM, Bogoch E, Hawker G et al. Patient perceptions of provider barriers to post-fracture secondary prevention. Osteoporos Int 2014;25:2581–9. 10.1007/s00198-014-2804-4 [DOI] [PubMed] [Google Scholar]
- 52.Roberge D, Beaulieu MD, Haddad S et al. Loyalty to the regular care provider: patients’ and physicians’ views. Fam Pract 2001;18:53–9. 10.1093/fampra/18.1.53 [DOI] [PubMed] [Google Scholar]
- 53.Pratt L, Seligmann A, Reader G. Physicians’ views on the level of medical information among patients. Am J Public Health Nations Health 1957;47:1277–83. 10.2105/AJPH.47.10.1277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Greenfield G, Pliskin JS, Feder-Bubis P et al. Patient-physician relationships in second opinion encounters—the physicians’ perspective. Soc Sci Med 2012;75:1202–12. 10.1016/j.socscimed.2012.05.026 [DOI] [PubMed] [Google Scholar]
- 55.Guest G, Bunce A, Johnson L. How many interviews are enough? Field Methods 2006;18:59–82. 10.1177/1525822X05279903 [DOI] [Google Scholar]