Abstract
An otherwise healthy 37-year-old man was admitted to hospital with uncontrollable vomiting and abdominal pain. Lithiasic acute pancreatitis was diagnosed on the basis of clinical symptoms along with raised serum amylase levels and compatible findings in ultrasonography and CT scan. Two Ranson criteria (lactate dehydrogenase over 350 U/L and aspartate aminotransferase over 250 U/L) were present at admission. The patient was transferred to an intensive care unit (ICU); intravenous crystalloids were prescribed and analgaesics were administered for pain relief. Unexpectedly, 10 h after ICU admission, he presented a cardiac arrest with a non-defibrillate rhythm and died after 40 min of advanced life support. An autopsy was performed and revealed acute necrohaemorrhagic pancreatitis with massive intraperitoneal and retroperitoneal haemorrhage. This case report summarises the epidemiology, pathophysiology and risk factors for fatal bleeding acute pancreatitis.
Background
Acute pancreatitis presents a wide spectrum of clinical manifestations, ranging from a mild, self-limited disorder (consisting of acute interstitial inflammation and oedema) to a severe and sometimes fatal necrohaemorrhagic form. Acute pancreatitis may rarely present with haemorrhagic complications, generally due to erosion of major pancreatic or peripancreatic vessels, with catastrophic massive bleeding into the gastrointestinal tract or abdominal cavity. While mild retroperitoneal haemorrhage is a common early feature of acute severe pancreatitis, life-threatening haemorrhagic complications following pancreatitis are rarely encountered. Massive bleeding has been reported to occur in 1.2–14.5% of patients with pancreatitis, with an overall mortality rate estimated at 34–52%.1
We report an unusual and atypical presentation of acute pancreatitis, represented by sudden death due to exsanguination related to necrohaemorrhagic pancreatitis.
Case presentation
An otherwise healthy 37-year-old man with a history of obesity and a smoking habit was admitted to a district general hospital with uncontrollable vomiting and epigastric abdominal pain with dorsal radiation that had started 3 h before admission.
At admission, he was conscious, with a regular blood pressure (BP 119/79 mm Hg), heart rate 64 bpm, SpO2 100%, sweaty skin, painful abdomen with abdominal bloating and decreased bowel sounds. Laboratory results (table 1) revealed high levels of serum amylase (2309 UI/L), serum transaminases (aspartate aminotransferase (AST) 251 UI/L; alanine transaminase (ALT) 253 UI/L) and serum lactic dehydrogenase (LDH 1003 UI/L).
Table 1.
Laboratory values at admission and 12 h after
| Admission | 12 h After admission | |
|---|---|---|
| Haemoglobin (g/dL) | 16.9 | 18.9 |
| Haematocrit (%) | 48 | 56.1 |
| Platelets (IU/L) | 215 000 | 215 000 |
| Leucocytes (IU/L) | 14 700 | 25 000 |
| Neutrophils (%) | 77 | 81 |
| Creatinine (mg/dL) | 1.1 | |
| Urea (mg/dL) | 30 | |
| Sodium (mmol/L) | 141 | |
| Potassium (mmol/L) | 3.7 | |
| Calcium (mg/dL) | 8.5 | |
| Phosphorus (mg/dL) | 4.3 | |
| Blood glucose (mg/dL) | 145 | |
| Total bilirubin (mg/dL) | 1.77 | |
| Conjugated bilirubin (mg/dL) | 0.79 | |
| Alkaline phosphatase (IU/L) | 43 | |
| γ-glutamyltransferase (IU/L) | 380 | |
| Aspartate aminotransferase(IU/L) | 251 | 116 |
| Alanine transaminase (IU/L) | 253 | 251 |
| Serum amylase (IU/L) | 2309 | |
| Serum lipase (IU/L) | 5913 | |
| Serum lactic dehydrogenase (IU/L) | 1003 | 887 |
| C reactive protein (mg/dL) | <0.5 |
Abdominal ultrasonography revealed a gallbladder with slight parietal prominence and millimetric lithiasic shadows on its contents without distension of the bile ducts, and an enlarged and heterogeneous pancreas with peripancreatic fluid. Abdominal CT scan revealed a swollen pancreas, with densification of adjacent fat, with no signs of pancreatic necrosis, and slight peritoneal effusion with no organised collections, leading to a Balthazar Score of 2 (figure 1). The diagnosis of lithiasic acute pancreatitis with 2 Ranson criteria (LDH over 350 U/L and AST over 250 U/L) was reached. Twelve hours after admission, the patient was transferred to a Central Hospital. At the admission, he had a sinus tachycardia (102 bpm) with no relevant changes in arterial blood gas analysis, except light hyperlactatemia (3.1 mmol/L).
Figure 1.
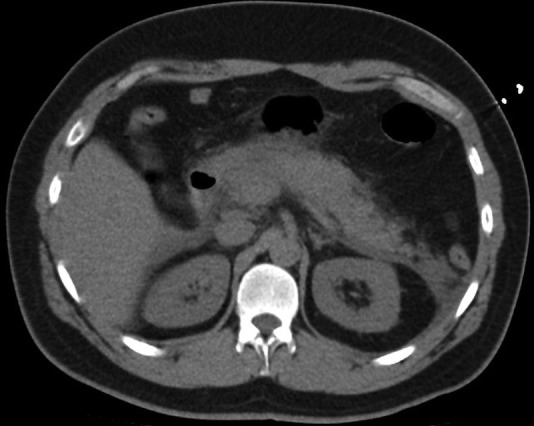
Abdominal CT scan revealing a swollen pancreas with densification of adjacent axial section.
Treatment
The patient was promptly transferred to the intensive care unit (ICU) and intravenous crystalloids were provided; analgaesics (tramadol and alphentanil) were administered for pain relief.
Despite initial respiratory and haemodynamic stability, with diuresis >0.5 mL/kg/h and no analytic worsening in renal function, 10 h after admission to ICU, unpredictably, the patient presented cardiac arrest in a non-defibrillate rhythm and died after 40 min of advanced life support.
Outcome and follow-up
An autopsy was performed and revealed acute necrohaemorrhagic pancreatitis with massive intraperitoneal and retroperitoneal haemorrhage, possibly related to involvement of the splenic vein and artery in the necrotic process.
Discussion
Acute pancreatitis is a common disease associated with acute inflammation of the pancreas tissue. Frequently, it involves the peripancreatic tissue and may affect other organs. The most common causes of pancreatic injury are gallstones and alcohol abuse. Only 15% of acute pancreatitis episodes are related to other aetiologies.2
Abdominal pain and vomiting are the most frequent symptoms in acute pancreatitis. Usually, it is a mild disease, associated with recovery in few days, nevertheless, severe acute pancreatitis could be a fatal condition due to the involvement of various organs, leading to multisystem organ failure, such as irreversible pulmonary oedema and acute renal failure.3
In acute necrotising pancreatitis, the peripancreatic vascular tissues are affected and destroyed by the autodigestive action of the pancreatic enzymes. This mechanism is responsible for the formation of pseudoaneurysms, vascular and intestinal erosions, and consequent haemorrhage.4 The retroperitoneum and peritoneal cavity are the most affected areas.5 Massive bleeding can occur within a few days after an episode of pancreatitis, nevertheless, it usually occurs as a late complication of repeated severe attacks or in patients with chronic pancreatitis.
The literature on bleeding complications of acute pancreatitis is sparse. Most of the available data are known due to few case reports and most studies include patients with acute pancreatitis as well as those with chronic pancreatitis. Nevertheless, some studies show incidence rate ranging from 1.2% to 14.5%1 6 7 with a higher mortality rate.1 Frequent reports of haemorrhage associated with postacute pancreatitis have usually involved rupture of pseudo-aneurysms.8 Other mechanisms of bleeding include compression by pseudocysts or pancreatic abscess.
Gastrointestinal and intra-abdominal bleeding have different degrees of severity. Gastrointestinal haemorrhage is usually a non-fatal condition, while intra-abdominal haemorrhage, as seen in our patient, is frequently associated with death.9
Various risk factors have been described as being responsible for bleeding in acute pancreatitis, namely: vasculitis, long-term anticoagulation therapy, history of pancreatic necrosectomy, pseudocyst and pancreatic abscess. Nevertheless, our patient had an acute necrohaemorrhagic pancreatitis in absence of any risk factor at presentation and the haemorrhage took place in the first 24–36 h of diagnosis.
The haemorrhagic complication of the present case, leading to sudden death, has rarely been reported. Therefore, massive intraperitoneal bleeding must be considered in the differential diagnosis for sudden death in patients with acute pancreatitis.
Learning points.
Massive bleeding is more frequent in patients with chronic pancreatitis and not so common in cases of acute pancreatitis.
Rarely, acute pancreatitis may present with haemorrhagic complications, which may lead to death.
Massive intraperitoneal bleeding should be kept in mind as a possible diagnosis for patients with acute pancreatitis leading to sudden death.
Footnotes
Contributors: SQ contributed to data collection, data analysis and drafting the article. IC, FM contributed to concept/design and critical revision of the article. PP contributed to concept/design, data analysis/interpretation, drafting the article, critical revision of the article and approval of the article.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Flati G, Andrén-Sandberg A, La Pinta M et al. Potentially fatal bleeding in acute pancreatitis: pathophysiology, prevention, and treatment. Pancreas 2003;26:8–14. 10.1097/00006676-200301000-00002 [DOI] [PubMed] [Google Scholar]
- 2.Steinberg W, Tenner S. Acute pancreatitis. N Eng J Med 1994;330:1198–210. 10.1056/NEJM199404283301706 [DOI] [PubMed] [Google Scholar]
- 3.Pastor CM, Matthay MA, Frossard JL. Pancreatitis-associated acute lung injury: new insights. Chest 2003;124:2341–51. 10.1378/chest.124.6.2341 [DOI] [PubMed] [Google Scholar]
- 4.Vujic I. Vascular complications of pancreatitis. Radiol Clin North Am 1989;27:81–91. [PubMed] [Google Scholar]
- 5.Bradley EL., III A clinically based classification system for acute pancreatitis. Summary of the International Symposium on Acute Pancreatitis, Atlanta, Ga, September 11 through 13, 1992. Arch Surg 1993;128:586–90. 10.1001/archsurg.1993.01420170122019 [DOI] [PubMed] [Google Scholar]
- 6.Imrie CW. Observations on acute pancreatitis. Br J Surg 1974;61:539–44. 10.1002/bjs.1800610710 [DOI] [PubMed] [Google Scholar]
- 7.Sharma PK, Madan K, Garg PK. Hemorrhage in acute pancreatitis: should gastrointestinal bleeding be considered an organ failure? Pancreas 2008;36:141–5. 10.1097/MPA.0b013e318158466e [DOI] [PubMed] [Google Scholar]
- 8.de Perrot M, Barney T, Buhler L et al. Management of bleeding pseudoaneurysm in patients with pancreatitis. Br J Sug 1999;86:29–32. 10.1046/j.1365-2168.1999.00983.x [DOI] [PubMed] [Google Scholar]
- 9.Andersson E, Ansari D, Andersson R. Major haemorrhagic complications of acute pancreatitis. Br J Surg 2010;97:1379–84. 10.1002/bjs.7113 [DOI] [PubMed] [Google Scholar]


