Background
Fusion anomalies of the kidney are uncommonly encountered in clinical practice. These are broadly divided into two distinct varieties: horseshoe kidney (most common) and crossed fused renal ectopia (second most common).1 Crossed fused renal ectopia has an incidence of 1:1000 to 1:7500 and is more common in males (2:1), with left to right ectopia being three times more common than right to left ectopia.2 According to Türkvatan et al,3 the most common variant of crossed fused renal ectopia forms when the upper pole of the inferiorly positioned crossed-ectopic kidney is fused to the lower pole of the superior, normally placed kidney. The presence of chyluria in the setting of crossed fused ectopic kidney is uncommonly reported. We report a unique case of chyluria in a middle-aged man with crossed fused renal ectopia associated with a large calculus in the middle one-third of the crossed ureter.
Case presentation
A 35-year-old man presented with intermittent mild left flank pain and milky urine, with no history of urinary tract infections, trauma or instrumentation.
Investigations
Chyluria was confirmed by the presence of chyle and triglycerides in postprandial urine. A plain X-ray KUB and intravenous pyelography (IVP) showed non-opacification of the right kidney and a malrotated left kidney with mid-ureteric calculus in the crossed ureter (figure 1). On ultrasonography of the kidney, ureter and urinary bladder, the right kidney was present on the left side, fused at its upper pole with the lower pole of the left, normally located kidney (figure 2). Contrast-enhanced CT of the kidney, ureter and urinary bladder showed a slightly smaller sized right kidney (crossed to the left side and fused with the lower pole of the normal placed left kidney at its upper pole), revealing moderate hydroureteronephrosis as a result of 17 mm calculus present in the middle one-third of the crossed right ureter. The left kidney was present in the normal position and slightly malrotated, with an extrarenal pelvis with multiple small calculi in all calices. The urinary bladder was normal in contour with normal wall thickening and the prostate was normal (figures 3–5).
Figure 1.
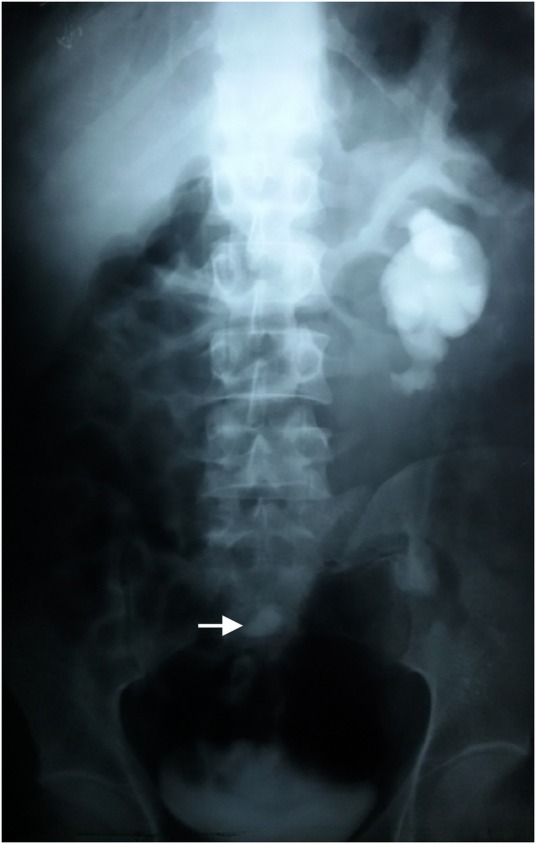
Intravenous pyelogram (delayed film) showing malrotated normally placed left kidney (non-visualised crossed right kidney) with a radiopaque shadow (ureteric calculus) in the crossed right ureter (arrow).
Figure 2.
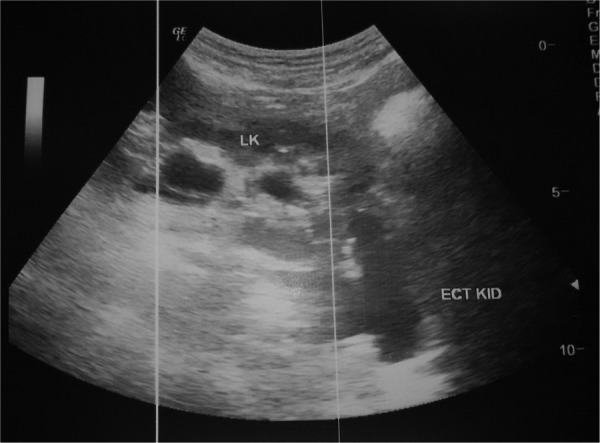
Ultrasonography of the kidney, ureter and urinary bladder (KUB) showing right kidney crossed to the left side, fused at its upper pole with lower pole of left normal placed kidney.
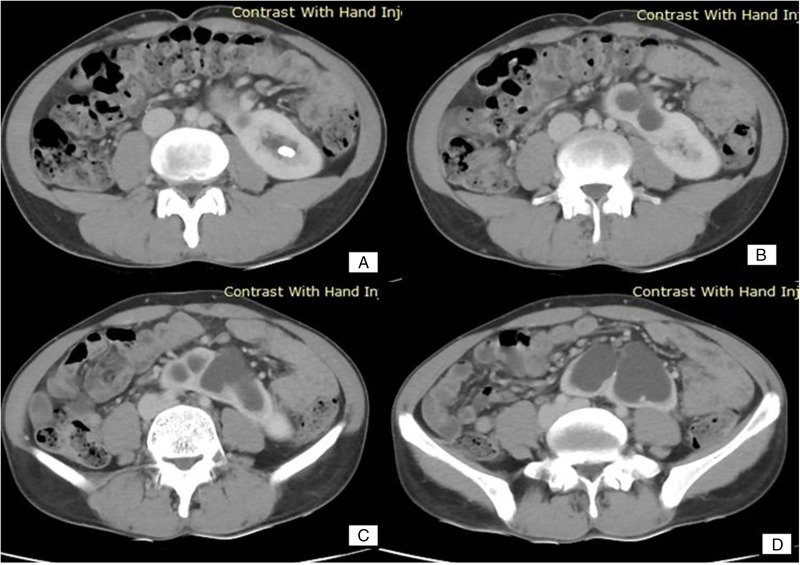
Figure 3.
Contrast-enhanced CT scan of the kidney, ureter and urinary bladder showing small contracted right kidney with anterior directed pelvicalyceal system crossed to the left and present in left lumbar region extending towards midline anterior to the spine with upper pole of right kidney attached to lower pole of normal placed left kidney.(arrow).
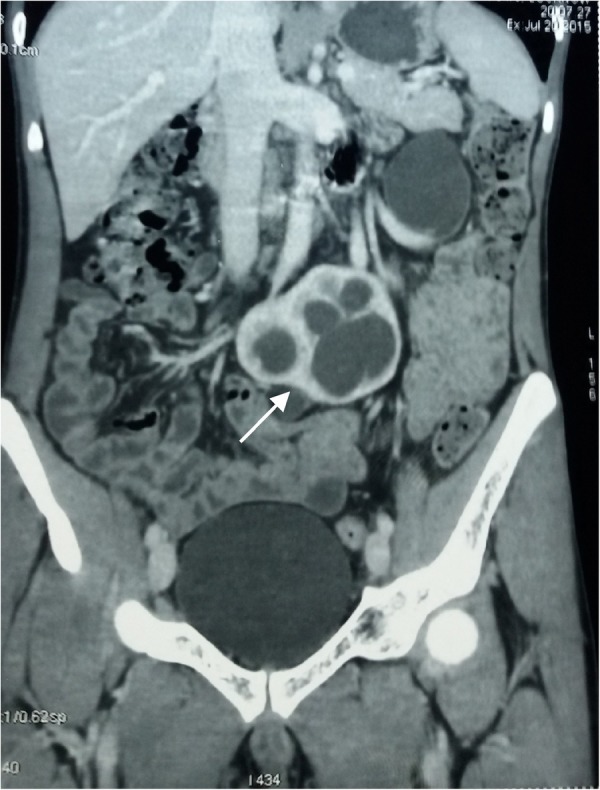
Figure 4.
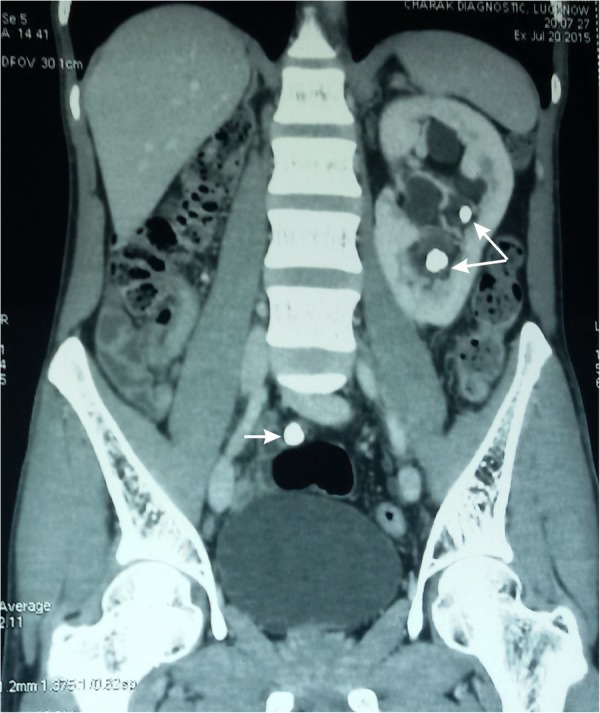
Contrast-enhanced CT scan of the kidney, ureter and urinary bladder showing left kidney present in normal position, enlarged in size, slightly malrotated and having an extrarenal pelvis with multiple small calculi in all calices (double arrow) with a large calculus present in mid-ureter region of right crossed ureter (single arrow).
Figure 5.
Contrast-enhanced CT scans of the kidney, ureter and urinary bladder region showing: (A) normal placed left kidney having normal contrast uptake and cortical thickness; (B–D) crossed right kidney fused at its upper pole with lower pole of left kidney with moderate hydroureteronephrosis.
Differential diagnosis
The possible differential diagnosis of chyluria can be based on its aetiology, that is, parasitic (most common—Wuchereria bancrofti, taenia echinococcus, Ankylostomiasis, trichiniasis and malarial parasites) and non-parasitic (congenital, lymphangioma of urinary tract, megalymphatics and urethral/vesicle fistulae, stenosis of thoracic duct, retroperitoneal lymphangiecatasia, traumatic lymphangiourinary fistulae, obstruction of thoracic duct/lymphatics, pregnancy, diabetes, abscess and nephrotic syndrome.4
Treatment
Postprandial cystoscopy (after 100 g oral butter) was performed under local anaesthesia, revealing chylous efflux from the left ureteric orifice, with normally located openings of bilateral ureters (figure 6). Retrograde pyelography revealed a right crossed ectopic kidney fused at its upper pole to a normal left kidney at its lower pole, with the right ureter crossing anterior to the sacral spine, opening at its normal location at trigone and containing a large calculus at the middle one-third of the ureter (figures 7–9). The patient was managed with renal pelvis instillation sclerotherapy (instillation of 1% silver nitrate directly in the left renal pelvis through a ureteric catheter), under strict aseptic conditions.
Figure 6.
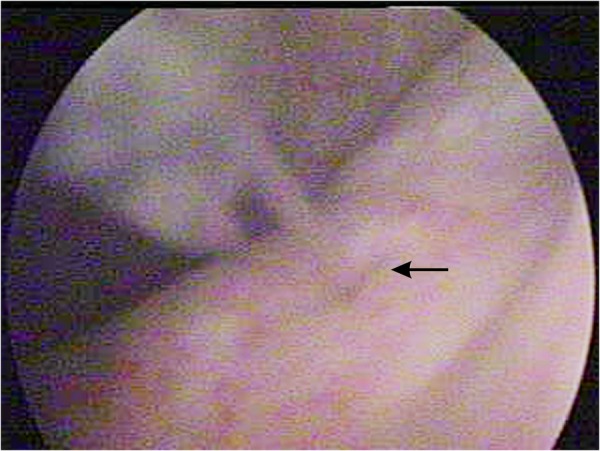
Cystoscopy view of urinary bladder showing chylous efflux from the left ureteric orifice.
Figure 7.
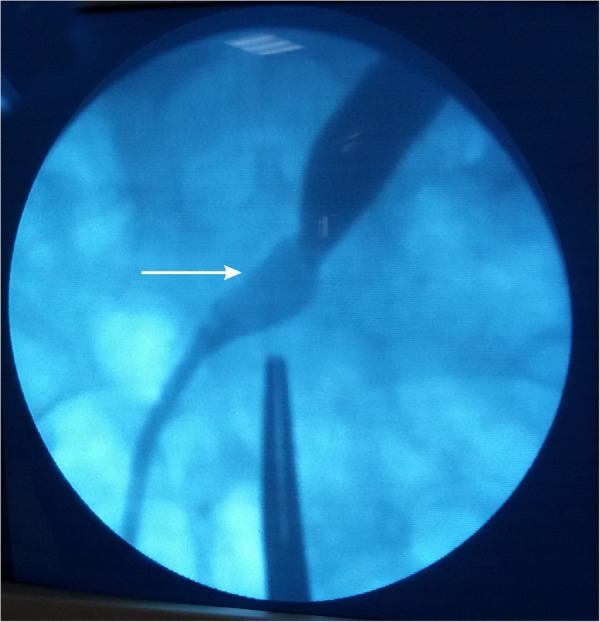
Retrograde pyelography view showing a large ureteric calculus in the crossed right ureter (arrow) with proximal dilatation.
Figure 8.

Retrograde pyelography view showing the pelvicalyceal system of small, malrotated and crossed right kidney (arrow).
Figure 9.
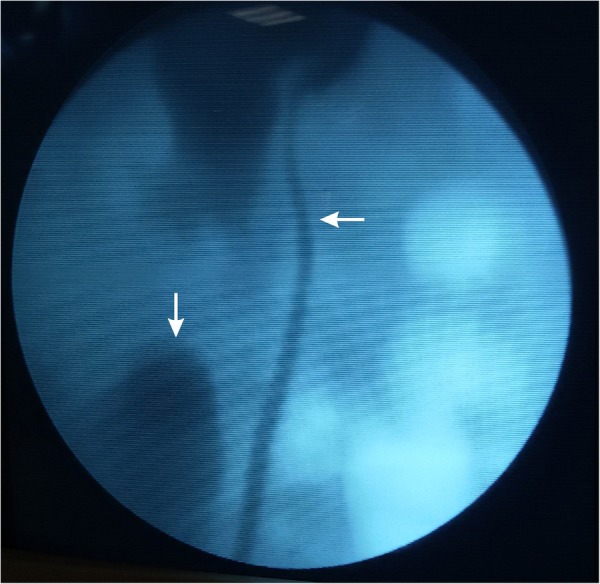
Retrograde pyelography view showing the pelvicalyceal system of malrotated crossed right kidney (vertical arrow) fused at its upper pole with the lower pole of normally located, malrotated left kidney (horizontal arrow showing the left ureter).
Outcome and follow-up
The chyluria subsided after sclerotherapy. We first tried rigid ureteroscopy for the removal of mid-ureteric calculus but found difficulty in negotiating the scope through this crossed, tortuous ureter, hence the procedure was abandoned. Since flexible ureteroscopy is not available in our institution, the patient underwent laparoscopic ureterolithotomy. Small renal calculi in the left kidney were treated with extracorporeal shockwave lithotripsy, following which the patient recovered well; he is at present doing fine in routine follow-up.
Discussion
Crossed fused renal ectopia is a rare condition, first described by Pamarolus in 1654.5 To date, only a limited number of cases have been reported in the literature. Most cases of crossed fused renal ectopia are asymptomatic, diagnosed incidentally and renal function is usually normal.6 Symptomatic patients most commonly present with flank or lower abdomen pain, abdominal lump, haematuria, dysuria, hypertension, urinary tract infections and fever. Chyluria in crossed fused renal ectopia is rarely reported. The chyluria can be of parasitic or non-parasitic origin. Parasitic infestation by W. bancrofti is most commonly responsible for chyluria in India. Mature parasites cause the blockade of retroperitoneal lymphatics and thoracic duct resulting in retrograde flow of lymph from abdomen and pelvis into the lumen of the genitourinary tract and subsequent development of urinary fistulae, which are most commonly located at the caliceal fornix.7 In this patient, although eosinophilia was absent and microfilariae were not found on peripheral smear, the presence of filariasis could not be ruled out because the patient belonged to a zone endemic for filariasis; confirmatory IgG ELISA (95% sensitivity and 85% specificity)8 against filarial antigens was not carried out and the patient had a history of no response of chyluria to a full course of diethylcarbamazine. Since this case was the first of its kind reported at our institute, we were left in a great dilemma about the ideal management sequence of this patient—which entity was to be treated first—the chyluria or ureteric calculus? The patient was advised on the management options for both his conditions in detail, but he was bothered more by the chyluria (rather than the mild intensity left flank pain) and wanted it to be managed first. As this patient had a history of failed medical treatment for chyluria, the only management options left were sclerotherapy and surgery. Therefore we decided to initially perform intrapelvic sclerotherapy according to the patient's preference. Different sclerotherapy agents reported in the literature include silver nitrate (0.1–3.0%), povidone iodine (0.2%), sodium iodide (15–25%), potassium iodide (10–25%), dextrose (50%), hypertonic saline (76%) or a combination of these agents. Silver nitrate is the most commonly used sclerosant and is tolerated well by most patients, with a reported response rate of around 80%. Common side effects (usually subsiding within 24 h) of sclerotherapy are flank pain, nausea/vomiting and, occasionally, haematuria. Certain uncommon side effects, though rarely reported, include anaphylactic reactions, pelviureteric junction or ureteric stricture,9 renal papillary necrosis and acute renal failure.10 Different surgical options are available for chyluria, postsclerotherapy failure, such as lymphovenous disconnection, omental wrapping, renal autotransplantation, microsurgical procedures and lymph node–saphenous vein anastomosis. Fortunately, this patient responded well to sclerotherapy, without any serious side effects.11 The ureteric calculus was managed with laparoscopic ureterolithotomy (in the same hospital sitting) after the exhaustion of other management options such as extracorporeal shockwave lithotripsy (the larger stone size with proximal hydroureteronephrosis, sacral promontory location and tortuous course of the ureter would have shown poor results), flexible ureteroscopy (non-availability of the instrument) and rigid ureteroscopy (difficulty in negotiating the tortuous nature of the crossed ureter).
This case is unique in many aspects. The patient had a less frequently occurring crossed renal ectopia from right to left (left to right is more common), also, the findings of crossed fused renal ectopia with ureteric calculus and chyluria are rarely reported together. Despite the initial dilemma of which entity to manage first—the chyluria or ureteric calculus—the patient had a thorough work up, was managed appropriately with the available resources and recovered well. Thus the message behind reporting this case is to try and build a consensus on the ideal management of such rarely reported cases.
Learning points.
Crossed fused renal ectopia is an uncommon entity and its association with chyluria is exceedingly rare.
A thorough work up of these patients is necessary for timely diagnosis and management.
There is a paucity of literature on the ideal management of patients presenting with such uncommon entities.
There is urgent need to develop a consensus on the ideal management of such rare cases.
Acknowledgments
The authors would like to acknowledge their family, friends and teachers, for their constant support in writing this manuscript.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Glodny B, Petersen J, Hofmann KJ et al. Kidney fusion anomalies revisited: clinical and radiological analysis of 209 cases of crossed fused ectopia and horseshoe kidney. BJU Int 2009;103:224–35. 10.1111/j.1464-410X.2008.07912.x [DOI] [PubMed] [Google Scholar]
- 2.Rinat C, Farkas A, Frishberg Y. Familial inheritance of crossed fused renal ectopia. Pediatr Nephrol 2001;16:269–70. 10.1007/s004670000540 [DOI] [PubMed] [Google Scholar]
- 3.Türkvatan A, Ölçer T, Cumhur T et al. Multidetector computed tomographic urography for evaluation of crossed fused renal ectopia. Ankara Üniversitesi Tip Fakültesi Mecmuasi 2008;61:149–54. 10.1501/Tipfak_0000000666 [DOI] [Google Scholar]
- 4.Sharma S, Hemal AK. Chyluria—an overview. Int J Nephrol Urol 2009;1:14–26. [Google Scholar]
- 5.Hochwald O, Shaoul R. Crossed fused ectopic left kidney. Arch Dis Child 2004;89:704 10.1136/adc.2003.047647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bauer SB. Anomalies of the upper urinary tract. In: Wein AJ, Kavoussi LR, Novick AC et al., eds Campbell–Walsh Urology. 9th edn Philadelphia: Saunders–Elsevier, 2007:3269–304. [Google Scholar]
- 7.Diamond E, Schapira HE. Chyluria—a review of the literature. Urology 1985;26:427–31. 10.1016/0090-4295(85)90147-5 [DOI] [PubMed] [Google Scholar]
- 8.Mehta VK, Lohar H, Banerjee GK et al. Surgical filariasis: immunoscreening for filarial IgG antibodies using Wuchereria bancrofti microfilarial excretory-secretory antigen. J Commun Dis 1999;31:35–40. [PubMed] [Google Scholar]
- 9.Garg M, Dalela D, Goel A. Devastating complication of silver nitrate instillation for the treatment of chyluria. BMJ Case Rep 2013;2013:pii: bcr2013201270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singh I, Dargan P, Sharma N. Chyluria a clinical and diagnostic stepladder algorithm with review of literature. Indian J Urol 2004;20:79–85. [Google Scholar]
- 11.Suri A, Kumar A. Chyluria—SGPGI experience. Indian J Urol 2005;21:59–62. 10.4103/0970-1591.19554 [DOI] [Google Scholar]