Abstract
Objectives
To describe implementation of a new national preventive programme to reduce cardiovascular morbidity.
Design
Observational study over 4 years (April 2009—March 2013).
Setting
655 general practices across England from the QResearch database.
Participants
Eligible adults aged 40–74 years including attendees at a National Health Service (NHS) Health Check.
Intervention
NHS Health Check: routine structured cardiovascular check with support for behavioural change and in those at highest risk, treatment of risk factors and newly identified comorbidity.
Results
Of 1.68 million people eligible for an NHS Health Check, 214 295 attended in the period 2009–12. Attendance quadrupled as the programme progressed; 5.8% in 2010 to 30.1% in 2012. Attendance was relatively higher among older people, of whom 19.6% of those eligible at age 60–74 years attended and 9.0% at age 40–59 years. Attendance by population groups at higher cardiovascular disease (CVD) risk, such as the more socially disadvantaged 14.9%, was higher than that of the more affluent 12.3%. Among attendees 7844 new cases of hypertension (38/1000 Checks), 1934 new cases of type 2 diabetes (9/1000 Checks) and 807 new cases of chronic kidney disease (4/1000 Checks) were identified. Of the 27 624 people found to be at high CVD risk (20% or more 10-year risk) when attending an NHS Health Check, 19.3% (5325) were newly prescribed statins and 8.8% (2438) were newly prescribed antihypertensive therapy.
Conclusions
NHS Health Check coverage was lower than expected but showed year-on-year improvement. Newly identified comorbidities were an important feature of the NHS Health Checks. Statin treatment at national scale for 1 in 5 attendees at highest CVD risk is likely to have contributed to important reductions in their CVD events.
Keywords: PRIMARY CARE, Health check, cardiovascular risk prevention, cardiovascular risk
Strengths and limitations of this study.
This is the first national study describing implementation of the new National Health Service (NHS) Health Check programme 2009–2012.
It is based on a large representative sample of 655 general practices in England with 1.68 million people aged 40–74 years eligible for an NHS Health Check of whom 214 295 attended.
Of those eligible, 70% had ethnic group recorded and 99% socioeconomic group recorded. In attendees, recording of ethnic group and major risk factors was over 90%.
Non-attendees were younger, more likely to smoke and recording of cardiovascular risk was less complete.
There is no information available about attendance for support for behavioural change following general practitioner (GP) referral.
Introduction
The English National Health Service (NHS) Health Checks programme started in 2009, aiming to reduce cardiovascular disease (CVD) risks and events. Internationally, it is the first of its kind, aiming to provide a routine structured clinical assessment and management for adults aged 40–74 years without pre-existing diabetes or CVD. The NHS Health Check includes review of CVD risks, behavioural change support and treatment of newly identified risk factors or comorbidity through integration with routine clinical provision in general practice. We describe an evaluation of the first 4 years of this national programme.
The NHS Health Check is a 5-year rolling programme which targets one-fifth of the eligible population each year, aiming to invite 3 million people at an annual cost of £165 million.1–3 The Department of Health report that 2.4 million NHS Health Checks were undertaken in the 2 years (2011–2012).4 Nationally, uptake is reported at around 50% of the eligible target population with considerable variability between provider organisations.4–6 The NHS Health Check programme is now supported by NHS England and Public Health England following major changes in the NHS in 2013 when Primary Care Trusts (PCTs) were replaced by Clinical Commissioning Groups (CCGs) and responsibility for commissioning the programme was transferred to the Local Authorities.7 8
Stratification of CVD risk for the purposes of therapeutic intervention is a key component of the NHS Health Check. Attendees receive personal advice to support behaviour change and treatment informed by CVD risk stratification. When the programme was introduced, National Institute for Health and Care Excellence (NICE) guidance and the NHS Health Check programme,9 10 recommended statin treatment at a 10-year CVD risk of 20% or more and antihypertensive treatment with blood pressure sustained at 140/90 mm Hg or more. Comorbidities, including diabetes and chronic kidney disease (CKD), are identified through blood testing in the high CVD risk group with appropriate management. Familial propensity to premature ischaemic heart disease is also identified.
There is robust trial and observational evidence of benefit from statins and antihypertensives in high-risk people with and without established CVD.11–16 In people at higher CVD risk, primary prevention of CVD using multiple risk factor intervention including treatment with statins and antihypertensives has been shown to be of benefit.17 However, this has not been demonstrated in entire populations including people at lower CVD risk. For people at lower CVD risk (ie, a 10-year risk of <10%) for whom behavioural change is the main intervention, the most effective prevention strategy remains unclear.16
Primary prevention based on assessment of cardiovascular risk is a topic of international interest and debate.18–20 The study was commissioned by the Department of Health to provide an early view of implementation of the national programme. This study describes the results from the first 4 years of the NHS Health Check programme, the population coverage and characteristics of those who attended, their recorded CVD risks, new comorbidity and treatment. Available information on non-attendees is also reported.
Methods
The study plan and this report conform to the STROBE recommendations for observational studies.21
QResearch is a large, nationally representative and validated primary care electronic database containing the health records of 13 million patients registered from 655 general practices using the Egton Medical Information System (EMIS) computer system for at least a year.
For the 4 years (1 April 2009 to 31 March 2013), we included in the study all eligible adults aged 40–74 years if they had been registered for at least a year. We excluded people ineligible for an NHS Health Check, defined by the Department of Health as people with pre-existing vascular disease including hypertension, ischaemic heart disease, stroke or transient ischaemic attack, atrial fibrillation, heart failure, peripheral arterial disease, CKD, familial hypercholesterolaemia, diabetes and those already on statins.22
Read codes are used to code clinical data in primary care. NHS Health Check attendance was identified by Read codes for CVD risk assessment or NHS Health Check completed. We were unable to distinguish NHS Health Checks conducted in general practice from those conducted by a third party such as a community pharmacy. For people with an NHS Health Check, we used the date of the Check as the index date for analysis. For those without an NHS Check during the study period, we allocated an index date of 1 April in each year. The NHS Health Check is a rolling 5-year programme, and the total eligible population each year was divided by five to estimate the number eligible in any 1 year. Coverage was defined as the number of attendees in the year, as a proportion of one-fifth of the population eligible in that year.
The total eligible population and people who attended an NHS Health Check were described according to sex, age group (40–49, 50–59, 60–74) and ethnic group. Ethnic groups were combined into Office of National Statistics categories: white (British, Irish, other Caucasian); South Asian (Bangladeshi, Indian, Pakistani); black African; black Caribbean; Chinese; other Asian; other (any other recorded ethnic group including mixed ethnic groups) and ethnic group not recorded.23
Deprivation was assessed using the Townsend score based on 2001 census-derived measures of overcrowding, car ownership and education available at lower super output area.24 This was obtained by linking the individuals’ postcode to lower super output area (approximately 150 households). Townsend score was accessible for 99% of patients. We grouped individuals into fifths of deprivation, with quintile 1 indicating least deprived and quintile 5 most deprived.
Information on smoking status, alcohol intake and risk factor recording was described for attendees and non-attendees. This included the latest information recorded up to and including the date of the NHS Health Check for attendees or the index date for non-attendees. Family history of ischaemic heart disease was coded as positive if a first-degree relative had angina or a heart attack under age 60 years. Information on alcohol consumption was categorised by units consumed per day (non-drinker, <1, 1–2, 3–6, 7–9, >9+) although it was not nationally part of the NHS Health Check during the study period. Information was also extracted on whether a recorded CVD risk score was estimated by either Framingham or QRisk2 using the same time frame as specified above. Where a score was recorded we used it to identify people at high CVD risk, defined as a 10-year CVD risk of 20% or more.
In people who attended a Health Check, information was extracted on medications, new morbidities, risk factor recording and referrals on the date of the check or in the following 12 months. The equivalent information was extracted for non-attendees for the 12 months from their index date. New medication was defined as at least two statin or antihypertensive prescriptions within 12 months. New comorbidities, including diagnosed hypertension, CKD categories 3–5 and diabetes, were included if newly recorded within 12 months of an NHS Health Check. Abnormal measurements were not classified as a diagnosis unless a diagnostic code was recorded. For example, a raised blood pressure was not classified as hypertension unless the diagnostic code for hypertension was recorded.
The data were analysed using STATA V.13 (STATA Corps). We calculated proportions of people who attended by categories of age, sex and ethnic group. We calculated proportions according to levels of smoking status, alcohol intake and risk factors in those who did and did not attend an NHS Health check. We also described CVD risk levels and outcomes in attendees following the NHS Health Check. We did not carry out statistical comparisons of NHS Health Check attendees with non-attendees, as data were incomplete in the latter.
Results
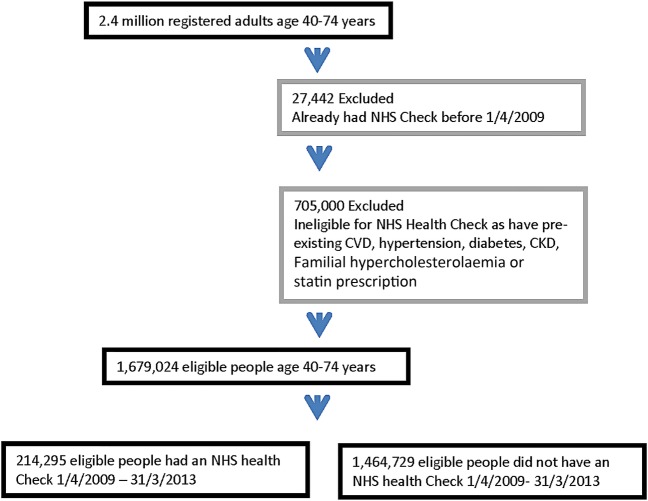
Over the 4-year study period (1 April 2009–31 March 2013) 1 679 024 people were eligible for an NHS Health Check. Of these, 12.8% (214 295) patients were recorded as having had an NHS Health Check (see figure 1).
Figure 1.
Flow-chart showing inclusion and exclusion of people eligible for an NHS Health Check and attendance. CKD, chronic kidney disease; CVD, cardiovascular disease; NHS, National Health Service.
One-fifth of the eligible population was considered available for attendance each year.
Table 1 shows coverage by financial year. In 2009/2010, there were a total 1 430 174 people eligible of whom 286 035 (one-fifth) were considered eligible in the year, and of these, 5.8% (16 613/286 035) attended an NHS Health Check. In 2010/11, 14.6% attended; in 2011/12, 24.4% attended; and in 2012/13, 30.1% attended.
Table 1.
Coverage of National Health Service (NHS) Health Check programme in each year
| Financial years | Patients with health check in financial year | 20% of the eligible population on 1 April | Percentage of coverage attendance/one-fifth of eligible population |
|---|---|---|---|
| 2009/2010 | 16 613 | 286 035 | 5.8 |
| 2010/2011 | 41 832 | 286 383 | 14.6 |
| 2011/2012 | 69 978 | 286 669 | 24.4 |
| 2012/2013 | 86 042 | 285 784 | 30.1 |
Table 2 shows NHS Health Check coverage for different eligible population subgroups during the entire 4-year study period. Of those eligible aged 60–74 years, 19.6% attended, and at age 40–59 years, 9.0% attended. In the most deprived quintile, 14.9% attended, and in the least deprived quintile, 12.3% attended.
Table 2.
Characteristics of people aged 40–74 years eligible for a National Health Service (NHS) Health Check between April 2009 and March 2013 and those who attended
| Total eligible people | NHS Health Check attendees | Percentage of total eligible population with NHS Health Check | |
|---|---|---|---|
| Total | 1 679 024 | 214 295 | 12.8 |
| Female | 846 797 | 111 740 | 13.2 |
| Male | 832 227 | 102 555 | 12.3 |
| Age band (years) | |||
| 40–49 | 806 199 | 72 903 | 9.0 |
| 50–59 | 499 725 | 68 428 | 13.7 |
| 60–74 | 373 100 | 72 964 | 19.6 |
| Townsend quintile of deprivation | |||
| 1 (most affluent) | 336 174 | 41 423 | 12.3 |
| 2 | 334 996 | 40 342 | 12.0 |
| 3 | 335 706 | 40 897 | 12.2 |
| 4 | 335 302 | 41 557 | 12.4 |
| 5 (most deprived) | 334 652 | 49 974 | 14.9 |
| Townsend not recorded | 2194 | 102 | 4.7 |
| Ethnicity | |||
| White | 1 065 171 | 185 082 | 17.4 |
| Indian | 16 842 | 2987 | 17.7 |
| Pakistani | 8472 | 1362 | 16.1 |
| Bangladeshi | 4925 | 1460 | 29.6 |
| Other Asian | 13 471 | 1966 | 14.6 |
| Caribbean | 12 908 | 2531 | 19.6 |
| Black African | 19 899 | 3128 | 15.7 |
| Chinese | 6913 | 1059 | 15.3 |
| Other | 26 045 | 4059 | 15.6 |
| Not recorded | 504 378 | 10 661 | 2.1 |
Seventy per cent (1 174 646/1 679 024) of the eligible population had ethnic group recorded. There was low attendance, 2.1% among the 30% of the eligible population without ethnicity recorded. Among those with ethnic group recorded, coverage was highest among South Asians (Indian, Pakistani, Bangladeshi, other Asian) of whom 19.2% of the eligible population attended, and black Caribbeans 19.6%, and lowest in black Africans 15.7% and Chinese 15.3%. In white people, 17.4% attended compared with 16.9% in all other recorded ethnic groups.
Table 3 shows information on risk factor recording and CVD risk score recording among attendees and non-attendees prior to or at the NHS Health Check or the equivalent index date for non-attendees. Smoking status was recorded in 99.9% of attendees and 94.5% of non-attendees. Non-attendees were more likely to be smokers. In total, 17.7% of attendees were smokers, and 22.4% of non-attendees were smokers. Alcohol consumption was recorded for 95.9% of attendees and 80.3% for non-attendees. Among those in whom alcohol consumption was recorded, heavy drinking (>9 units/day) was reported by 2.5% of attendees and 2.2% of non-attendees.
Table 3.
Characteristics of eligible people who did and did not attend for a NHS Health Check recorded prior to or on the date of the NHS Health Check or relevant index date
| NHS Health Check N (%) |
No NHS Health Check N (%) |
|
|---|---|---|
| Total | 214 295 | 1 464 729 |
| Smoking status recorded | 214 020 (99.9) | 1 384 707 (94.5) |
| Non-smoker | 117 968 (55.1) | 768 276 (55.5) |
| Ex-smoker | 58 244 (27.2) | 306 397 (22.1) |
| Light smoker (1–9/day) | 19 589 (9.2) | 167 592 (12.1) |
| Moderate smoker (10–19/day) | 11 052 (5.2) | 83 585 (6.0) |
| Heavy smoker (20+/day) | 7167 (3.3) | 58 857 (4.3) |
| Alcohol intake | ||
| Alcohol status recorded | 205 506 (95.9) | 1 175 900 (80.3) |
| Non-drinker | 53 485 (26.0) | 292 289 (24.9) |
| Trivial <1 units/day | 66 780 (32.5) | 421 139 (35.8) |
| Light 1–2 units/day | 37 398 (18.2) | 205 572 (17.5) |
| Moderate 3–6 units/day | 42 467 (20.7) | 227 987 (19.4) |
| Heavy 7–9 units/day | 3235 (1.6) | 17 169 (1.5) |
| Very heavy >9 units/day | 1866 (0.9) | 8842 (0.8) |
| Drinker—amount not recorded | 275 (0.1) | 2902 (0.2) |
| Risk factor recording | ||
| Body mass index recorded | 210 062 (98.0) | 1 176 819 (80.3) |
| Systolic blood pressure recorded | 213 690 (99.7) | 1 316 926 (89.9) |
| Cholesterol recorded | 195 994 (91.5) | 633 548 (43.3) |
| Cholesterol/HDL recorded | 174 345 (81.4) | 433 594 (29.6) |
| Positive family history CHD | 46 466 (21.7) | 156 604 (10.7) |
| Mean body mass index (SD) | 27.1 4.5) | 26.4 (4.6) |
| Mean cholesterol (SD) | 5.5 (1.0) | 5.4 (1.0) |
| Mean cholesterol/HDL (SD) | 4 (1.3) | 4 (1.2) |
| Mean SBP (SD) | 130.8 (16.9) | 128.4 (15.6) |
| Mean DBP (SD) | 79.4 (10.0) | 78.6 (9.4) |
| QRisk2 recorded | 171 441 (80.0) | 424 523 (29.0) |
| QRisk2 not recorded | 42 854 (20.0) | 1 040 206 (71.0) |
| QRisk2 score | ||
| <5% | 47 794 (22.3) | 195 253 (13.3) |
| 5–9.99% | 43 687 (20.4) | 114 706 (7.8) |
| 10–14.99% | 32 452 (15.1) | 55 306 (3.8) |
| 15–19.99% | 22 639 (10.6) | 31 356 (2.1) |
| 20+% | 24 869 (11.6) | 27 902 (1.9) |
| Framingham score recorded | 33 260 (15.5) | 76 051 (5.2) |
| Not recorded | 181 035 (84.5) | 1 388 679 (94.8) |
| Framingham score | ||
| <5% | 7152 (3.3) | 20 532 (1.4) |
| 5–9.99% | 10 196 (4.8) | 25 898 (1.8) |
| 10–14.99% | 6896 (3.2) | 15 286 (1.0) |
| 15–19.99% | 4283 (2.0) | 7787 (0.5) |
| 20+% | 4733 (2.2) | 6547 (0.4) |
| 20+ QRisk2 or Framingham | 27 624 (12.9) | 32 481 (2.2) |
CHD, coronary heart disease; DBP, diastolic blood pressure; HDL, high-density lipoprotein; NHS, National Health Service; SBP, systolic blood pressure.
CVD risk using QRisk2 was assessed in 80.0% (171 441/214 295) of attendees and in 29.0% (424 523/1 464 729) of non-attendees and versions of Framingham were used in 15.5% (33 260/214 295) of attendees and 5.2% (76 051/1 464 729) of non-attendees.
Of those attendees with QRisk2 scores recorded, 14.5% (24 869/171 441) were at high CVD risk (10-year risk of 20% or more), and 20.7% (4733/33 260) of those with Framingham scores recorded were at high CVD risk. In total, 12.9% (27 624/214 295) of all attendees were recorded at high CVD risk (20% or more 10-year risk) using either QRisk2 or Framingham. Among non-attendees with QRisk2 recorded, 6.6% (27 902/424 523) were at high CVD risk and 8.6% of non-attendees were at high CVD risk (6547/76 051) using Framingham.
Of those attendees with a QRisk2 score recorded, 46.6% (79 960/171 441) had a CVD risk of 10% or more. In the non-attendees with a recorded QRisk2 score, 27.0% (114 564/424 523) were at 10% or more CVD risk.
New comorbidity
Table 4 records new comorbidity identified at or in the 12 months after the NHS Health Check from 2009 to 2012. This included 7844 new cases of hypertension (1 case per 27 NHS Health Checks), 1934 new cases of diabetes (1 new case for every 110 Checks) and 807 new cases of CKD (1 new case in every 265 Checks).
Table 4.
Outcomes for people who did and did not have an NHS Health Check (number, %) recorded at NHS Health Check, relevant index date or in 12 months following these dates
| NHS Health Check N (%) |
No NHS Health Check N (%) |
|
|---|---|---|
| Total patients | 214 295 | 1 464 729 |
| New diagnoses | ||
| Chronic kidney disease (eGFR <60 mL/min/) | 807 (0.4) | 2310 (0.2) |
| Type 2 diabetes | 1934 (0.9) | 5647 (0.4) |
| Hypertension | 7844 (3.7) | 16 184 (1.1) |
| Risk factor recording | ||
| Body mass index recorded | 151 480 (70.7) | 144 756 (9.9) |
| Positive family history of premature CHD recorded | 14 760 (6.9) | 4720 (0.3) |
| Blood pressure recorded | 140 995 (65.8) | 242 928 (16.6) |
| eGFR recorded | 59 021 (27.5) | 160 843 (11.0) |
| Fasting glucose | 35 801 (16.7) | 78 934 (5.4) |
| Random glucose | 64 439 (30.1) | 102 568 (7.0) |
| Total cholesterol recorded | 123 342 (57.6) | 137 207 (9.4) |
| Cholesterol/HDL ratio recorded | 118 930 (55.5) | 115 011 (7.9) |
| Smoking status recorded | 188 282 (87.9) | 410 301 (28.0) |
| Risk factors identified (as % recorded) | ||
| Fasting glucose≥7 mmol/L | 954 (2.7) | 2983 (3.7) |
| Random glucose≥11 mmol/L | 421 (0.6) | 1291 (1.3) |
| Raised BP: SBP ≥140mmHg or DBP ≥90mmHg | 26 126 (18.5) | 52 236 (21.5) |
| Obesity BMI≥30 kg/m2 | 32 133 (21.2) | 39 774 (27.5) |
| New referrals (as % recorded) | ||
| Current smokers referred to smoking cessation clinic | 2571 (6.8) | 9944 (3.2) |
| Weight referrals: BMI ≥30 kg/m2 | 12 430 (38.7) | 4441 (11.2) |
| Exercise referrals: BMI ≥30 kg/m2 | 13 309 (41.4) | 4082 (10.3) |
| Alcohol referrals: >6 units/day | 1823 (33.9) | 1459 (5.1) |
| New medication | ||
| 2+ prescriptions for statins | 10 900 (5.1) | 15 086 (1.0) |
| 2+ prescriptions for antihypertensives | 8457 (3.9) | 26 178 (1.8) |
BMI, body mass index; CHD, coronary heart disease; DBP, diastolic blood pressure; eGFR, estimated glomerular filtration rate; HDL, high-density lipoprotein; NHS, National Health Service; SBP, systolic blood pressure.
Recording of new comorbid conditions in the year after an NHS Check was higher in people attending NHS Health Checks than recording in the year after the index date in non-attendees. However, in non-attendees, missing data are a major issue which precludes simple direct comparison between attendees and non-attendees. Risk factors requiring further follow-up were recorded in more than one in five attendees. Raised blood pressure (≥140/90 mm Hg; but not recorded as a diagnosis of hypertension) was identified in 18.5% (26 126/140 995), obesity (body mass index (BMI) ≥30 kg/m2) in 15.0% (32 133/151 480) and raised fasting blood sugar (but not recorded as a diagnosis of diabetes) in 2.7% (954/35 801).
In total, 33.9% of heavy and very heavy alcohol drinkers (1823/5376) were referred for further advice, and in people who were obese (BMI ≥30 kg/m2), 38.7% (12 430/32 133) received advice on weight reduction and 41.4% (13 309/32 133) on physical activity. In total, 6.8% (2571/37 808) of smokers were referred to dedicated smoking cessation services.
New recurrent prescriptions for statins (two or more prescriptions within 12 months) were provided for 5.1% (10 900) of attendees and new recurrent prescriptions for antihypertensives for 3.9% (8497) of attendees. Equivalently 1 in 20 attendances resulted in recurrent statin prescriptions, and 1 in 25 attendances resulted in recurrent antihypertensive prescriptions.
Attendees at high CVD risk
Table 5 shows the characteristics of those at high CVD risk (≥20% risk) who attended for an NHS Health Check. In total, 12.9% (27 624/214 295) attendees were recorded at high CVD risk. As expected, those at high CVD risk were older, with 81.0% of high-risk attendees in the 60–74-year age group compared with 34.0% of all attendees. Men comprised 78.3% in the high-risk group and 47.9% among all attendees.
Table 5.
Characteristics of people at high CVD risk who attended an NHS Health Check 1 April 2009 to 31 March 2013 recorded at or prior to the date of the NHS Health Check
| NHS Health Check risk ≥20% N (%) |
|
|---|---|
| Total patients all CVD risks | 214 295 |
| Total with CVD risk ≥20% | 27 624 |
| Females | 5992 (21.7) |
| Males | 21 632 (78.3) |
| Age band (years) | |
| 40–49 | 778 (2.8) |
| 50–59 | 4475 (16.2) |
| 60–74 | 22 371 (81.0) |
| Townsend quintile | |
| 1 (most affluent) | 5135 (18.6) |
| 2 | 5356 (19.4) |
| 3 | 5301 (19.2) |
| 4 | 5284 (19.1) |
| 5 (most deprived) | 6539 (23.7) |
| Ethnicity | |
| Ethnicity recorded | 26 392 (95.5) |
| White | 25 037 (90.6) |
| Indian | 376 (1.4) |
| Pakistani | 264 (1.0) |
| Bangladeshi | 276 (1.0) |
| Other Asian | 135 (0.5) |
| Caribbean | 89 (0.3) |
| Black African | 27 (0.1) |
| Chinese | 17 (0.1) |
| Other | 171 (0.6) |
| Not recorded | 1232 (4.5) |
| Smoking status recorded | 27 611 (100.0) |
| Non-smoker | 10 517 (38.1) |
| Ex-smoker | 9351 (33.9) |
| Light smoker (1–9/day) | 4024 (14.6) |
| Moderate smoker (10–19/day) | 2199 (8.0) |
| Heavy smoker (20+/day) | 1520 (5.5) |
| Alcohol intake prior to or at NHS Health Check | |
| Alcohol status recorded | 26 765 (96.9) |
| Non-drinker | 6897 (25.0) |
| Trivial <1 units/day | 7919 (28.7) |
| Light 1–2 units/day | 4684 (17.0) |
| Moderate 3–6 units/day | 6322 (22.9) |
| Heavy 7–9 units/day | 601 (2.2) |
| Very heavy >9 units/day | 304 (1.1) |
| Drinker: amount not recorded | 38 (0.1) |
| Risk factor recording prior to or at NHS Health Check | |
| Body mass index recorded | 27 243 (98.6) |
| Systolic blood pressure recorded | 27 600 (99.9) |
| Cholesterol recorded | 26 241 (95.0) |
| Positive family history of premature CHD | 9503 (34.4) |
| Mean body mass index (SD) | 27.6 (4.2) |
CHD, coronary heart disease; CVD, cardiovascular disease; NHS, National Health Service.
As expected, all other risk factors were more prevalent in those at high CVD risk. Of the high CVD risk attendees, 23.2% (4222/18 203) were obese and 28% (7743/27 611) were smokers. Blood pressure was ≥140/90mm Hg in 30.0% (4772/15 905) at high CVD risk compared with 18.5% (26 126/140 995) in all attendees. Of those NHS Health Check attendees at high CVD risk, 19.3% (5325/27 624) were prescribed recurrent statins and 8.8% (2438/27 624) were prescribed recurrent antihypertensive therapy.
Referrals to behavioural support
Online supplementary appendix table shows referrals for behavioural interventions in people at high CVD risk. Using data from tables 3 and 4, it can be shown that most referrals took place in people at lower CVD risk (<20% over 10 years). Of those people with behaviourally mediated risk factors recorded—smoking, obesity and high alcohol consumption—who were referred for further support during an NHS Health Check, 80.0% were not in the high CVD risk group. Of the smoking cessation referrals made in smokers, 17.1% (439/2571) were in smokers at high CVD risk and 82.9% were in people at lower risk. Of the dietary referrals made in people with BMI ≥30 kg/m2, 13.6% (1691/12 430) were in people at high CVD risk and 86.4% were in people at lower risk. Similarly of the referrals for physical activity, 13.4% (1780/13 309) were in people at high CVD risk and 86.6% were in people at lower risk. Of the total referrals for alcohol reduction support for heavy or very heavy drinkers, 16.5% (300/1823) were in people at high CVD risk and 83.5% were in people at lower risk.
In total, 5.7% (1139/7743) of smokers at high CVD risk were referred to accredited level 2 or 3 smoking cessation services. In people at high CVD risk with BMI ≥30 kg/m2, 40.0% (1691/4222) were referred to dietary and 42.2% (1780/4222) to physical activity support services, and 33.1% (300/905) of those at high CVD risk recorded as drinking seven or more units of alcohol per day were referred to alcohol reduction services.
These proportions of people at high CVD risk referred to smoking cessation, dietary, physical activity and alcohol services were very similar to the proportions of all attendees (tables 3 and 4) who were referred, of whom 6.8% (2571/37 808) of smokers were referred to smoking cessation, 38.7% (12 430/32 133) of BMI ≥30 to dietary and 41.4% (13 309/32 133) of BMI ≥30 to physical activity support services, and 35.7% (1823/5101) of heavy drinkers were referred to alcohol reduction services.
Discussion
This is the first study to describe national results from the NHS Health Check programme. In 2012, the most recent year reported, 30.1% of the eligible population attended. Attendance was more likely over age 65 years 19.6% than in those under 65 years (9.0%) and among those people in the most deprived quintile (14.9%) versus the least deprived (12.3%). In total, 12.9% of all attendees were recorded at high CVD risk (20% or more 10-year risk). There were differences in attendance between ethnic groups, though these could be due to missing data. Attendance in white people was similar to those with non-white ethnic group recorded.
New comorbidity identified in the 4-year period included 7844 new cases of hypertension (1 case per 27 NHS Health Checks), 1934 new cases of diabetes (1 new case for every 110 Checks) and 807 new cases of CKD (1 new case in every 265 Checks). Records of risk factors were more incomplete in non-attendees who had a different CVD risk profile to those who attended. Non-attendees were younger and more likely to be smokers than attendees. Because of differences in the characteristics and recording of risk factors between attendees and non-attendees, we have not made formal statistical comparisons of new morbidity between these groups.
In addition to those people with new comorbidities diagnosed, risk factors such as raised blood pressure, raised blood sugar and obesity requiring further follow-up were recorded in more than one in five of attendees. Most referrals for behavioural interventions took place in people at lower CVD risk. Of those people with behaviourally mediated risk factors recorded—smoking, obesity and alcohol consumption—who were referred for further support during an NHS Health Check, 80% were not in the high CVD risk group. The proportion of people in the high CVD risk group referred because of risk factors was similar to the proportion referred among all attendees.
One in 20 attendances resulted in recurrent statin prescription and 1 in 25 attendances resulted in recurrent antihypertensive prescription. Of those NHS Health Check attendees at high CVD risk, 19.3% were prescribed recurrent statins and 8.8% were prescribed recurrent antihypertensive therapy.
This is a large and nationally representative study including records of social deprivation and ethnicity. Coverage of 30% was lower than expected, though attendance quadrupled during the course of the study reflecting the early phase of implementation. There was no evidence that older people, or those in the more deprived quintile were less likely to attend than other groups. South Asians who have higher CVD risks were more likely to attend than other ethnic groups. Though missing data might account for this, similar differences have been found in other studies.25 Currently attendance at NHS Health Checks is reported as uptake in response to invitation rather than coverage, defined as attendance as a proportion of the eligible population as reported in this paper.4
The NHS Health Check programme is an example of systematic implementation at national scale, of a stratified approach to advice and effective treatment in people at increased CVD risk. QRisk2 was used in 80% of NHS Checks reported in this study and is fully integrated with the EMIS computer systems used by general practitioners in this study and has since been recommended as the risk algorithm of choice in the 2014 NICE guidance;26 an example of successful translation of clinical decision support at scale.27 28 This algorithm is fully integrated with the electronic primary care record, a key enabling factor for implementation.29
Limitations of the study
There is no nationally available data on the extent of provision of the NHS Health Check outside of general practices. However, these were likely to represent less than 10% of NHS Health Checks undertaken, as in most PCTs the NHS Health Check was conducted almost entirely in general practice with limited use of community programmes targeting hard-to-reach groups or, with the exception of a few areas, community pharmacies. Completeness of NHS Health Checks was not ascertained, but taking measurement of cholesterol recording of 91.5% as a proxy measure, risk ascertainment was generally well conducted.
Of the people referred with behavioural risk factors, 80% were at lower CVD risk, which indicates the wide distribution of risk factors and the potential for behaviour change if programmes can be shown to be effective. Like other recent studies, referral rates were generally low,30 and little is known about attendance at, or quality of behavioural programmes even for those at higher CVD risk. Lack of consistent coding of referrals in earlier years of the NHS Health Check programme and the availability of local services for behavioural change may have contributed to low referral rates. The impact of the NHS Health Check programme on people at lower risk is unknown and further research is required.31
The study is descriptive and was not designed to determine variability between practices or CCGs. The study has not assessed changes in risk factors or cardiovascular events between comparable groups. These comparisons are difficult in a non-randomised study, especially if one group is at higher risk than the other or information is incomplete. For these reasons, we have not directly compared attendees with non-attendees. Communication of results and patient behaviours following NHS Health Checks remains an under-researched area.32–34
Implications for practice
A number of local studies suggest that the programme has been better implemented in some areas with coverage of 80% and statin prescription of up to 50% in high-risk individuals in some CCGs.25 35 Nationally, uptake in 2011–2012 was reported as 45%, with high levels of variability and better uptake in more deprived areas.6 5 There is limited evidence of effectiveness35 or comorbidities identified36 and statin uptake in those at high risk was reported to be between 20% and 50%,5 25 which accords with national surveys of 32%.37
Despite a statin treatment rate of only 19% in high-risk attendees in this study, this is likely to have had an important impact on CVD events in those treated. Assuming that 1.2 million people attended a NHS Check each year in the 5 years since 2010, of whom 10% (120 000) were at high CVD risk averaging 2.5% per year, and 19.3% (23 160) of these people were treated with statins over this period and 8.8% (10 560) were treated with antihypertensives; if each treatment reduces cardiovascular risk by 20%, it is estimated that 2529 people would avoid a major CVD event over a 5-year period.11 12 Higher uptake in recent years and additional treatment in people at both high CVD risk and at lower CVD risk make this a conservative estimate and behavioural change will have further impact.37 These estimates assume that patients who are prescribed medications take them for a 5-year period and that the impact on outcomes is similar to that described in the trial meta-analyses cited.
The NHS Health Check programme has had a difficult birth. The efficacy of the programme has been challenged,38–41 based largely on a review of 16 trials of health checks, of which 12 trials were undertaken more than 20 years ago before 1994,42–52 the year in which the landmark 4S trial established statin effectiveness.53 This means that 12 out of 16 of the reported studies were conducted before statins or modern antihypertensive drugs were used. Of the trials since 1994, only one52 specifically recommended drug treatment for CVD risk, the other three offering advice but no drug treatment.54–56 The results of the Inter99 study of intensive lifestyle counselling published subsequent to this review57 showed no reduction in CVD. Despite high-quality review of trial evidence showing net benefit,11 statins have continued to received considerable adverse publicity58 59 which has been refuted.60
There have also been organisational factors that have impacted on implementation of the programme. Major organisational change in the NHS in the context of financial austerity61 62 led to one-third of staff leaving many PCTs in the transition to CCGs in April 201363 and commissioning responsibility for NHS Checks passed to Local Authorities. It is perhaps not surprising that in 2013, 27/151 PCTs nationally offered NHS Health Checks to fewer than 10% of eligible individuals and uptake could be substantially improved.64 The most efficient means to deliver this programme including delivery through pharmacies and likely economic impact, remain subjects for further research and debate. A range of infrastructural issues and new research are currently being addressed by Public Health England.65 66
This study indicates limited though improving success in the early years of a major new national preventive programme. Coverage of 30% and statin treatment of 19% of attendees at high CVD risk leave considerable room for improvement. New comorbidity and abnormal risk factors were frequently identified in people who attended an NHS Health Check. The majority of referrals for abnormal risk factors were among people at lower CVD risk. This modest start to a major new programme at scale is likely to have made an important impact on CVD events in people who have been treated with statins and antihypertensives or who improved adverse risk factors.
Acknowledgments
The authors thank EMIS practices, EMIS and the University of Nottingham for the use of QResearch for this study.
Footnotes
Contributors: JR initiated the study and has contributed to its design and implementation. JH-C contributed to the research question, design, data extraction, data analysis, interpretation and comments on the manuscript. CC advised on the statistical analysis and interpretation. ID conducted a preliminary investigation in one CCG that informed the study design, preparation of the code sets and study specification. SE and VM supported the statistical analysis and interpretation and all authors including CG and AS contributed to the study design and all authors contributed to the manuscript. The views expressed in this publication are those of the authors and do not necessarily represent those of those of the Department of Health or institutions that fund or support the authors.
Funding: This study is independent research commissioned and funded by the Department of Health Policy Research Programme (as the NHS Health Check Programme evaluation 009/0052). AS is supported by a Harkness Fellowship in Health Care Policy and Practice from The Commonwealth Fund. All other authors are funded by their host organisation.
Competing interests: All authors have completed the Unified Competing Interests form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare that (1) JR, JH-C, CC and AS are authors of QRisk, one of the CVD Scores widely used in the NHS Health Check programme. JR was Chair of a National Institute for Health and Care Excellence Guideline that recommended systematic use of CVD scores in 2008. JH-C is also the director of ClinRisk Ltd which produces open and closed source software to ensure the reliable and updatable implementation of clinical risk algorithms (including QRISK) within clinical computer systems to help improve patient care. CC is an associate professor of Medical Statistics at the University of Nottingham and a consultant statistician for ClinRisk Ltd. The NIHR grant which funded this project provided funds to SE, JR, ID, JH-C and CC for their contribution to the study.
Ethics approval: The Trent Research Ethics committee has approved use of the QResearch database for anonymised use of primary care data (http://www.qresearch.org).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Public Health England. NHS Health Check programme standards. NHS England, 2014. http://www.healthcheck.nhs.uk/commissioners_and_healthcare_professionals/national_guidance/ (accessed 12 Mar 2015). [Google Scholar]
- 2.Kerr M. NHS Health Check costs, benefits and savings. Department of Health, 2012. http://www.nhshealthcheck.nhs.uk/default.aspx?aID=18 (accessed 12 Mar 2015). [Google Scholar]
- 3.Public Health England. NHS Health Check programme best practice guidance, 2013. http://www.healthcheck.nhs.uk/commissioners_and_healthcare_professionals/national_guidance/ (accessed 12 Mar 2015).
- 4.Department of Health. NHS Health Checks 2011–13, 2013. http://www.england.nhs.uk/statistics/integrated-performance-measures-monitoring/nhs-health-checks-data/ (accessed 12 Mar 2015).
- 5.Nicholas JM, Burgess C, Dodhia H et al. Variations in the organization and delivery of the ‘NHS health check’ in primary care. J Public Health (Oxf) 2013;35:85–91. 10.1093/pubmed/fds062 [DOI] [PubMed] [Google Scholar]
- 6.Artac M, Dalton AR, Babu H et al. Primary care and population factors associated with NHS Health Check coverage: a national cross-sectional study. J Public Health (Oxf) 2013;35:431–9. 10.1093/pubmed/fdt069 [DOI] [PubMed] [Google Scholar]
- 7.Department of Health. Living well for longer: a call to action on avoiding premature mortality. London, 2013. [Google Scholar]
- 8.Department of Health. Improving outcomes for people with or at risk of cardiovascular disease. London, 2013. https://www.gov.uk/government/publications/cardiovascular-disease-outcomes-strategy-improving-outcomes-for-people-with-or-at-risk-of-cardiovascular-disease (accessed 12 Mar 2015). [Google Scholar]
- 9.Department of Health. Putting prevention first: NHS Health check: vascular risk assessment and management. Best practice guidance. London, 2009. http://www.healthcheck.nhs.uk/document.php?o=227 (accessed 12 Mar 2015). [Google Scholar]
- 10.NICE. Lipid modification: cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease. CG67. London: National Institute of Health and Clinical Excellence, 2008. [PubMed] [Google Scholar]
- 11.Mihaylova B, Emberson J, Blackwell L et al. , Cholesterol Treatment Trialists (CTT) Collaborators. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet 2012;380:581–90. 10.1016/S0140-6736(12)60367-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taylor F, Huffman MD, Macedo AF et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev 2013;(1):CD004816 10.1002/14651858.CD004816.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Czernichow S, Zanchetti A, Turnbull F et al. The effects of blood pressure reduction and of different blood pressure-lowering regimens on major cardiovascular events according to baseline blood pressure: meta-analysis of randomized trials. J Hypertens 2011;29:4–16. 10.1097/HJH.0b013e32834000be [DOI] [PubMed] [Google Scholar]
- 14.Baigent C, Keech A, Kearney PM et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005;366:1267–78. 10.1016/S0140-6736(05)67394-1 [DOI] [PubMed] [Google Scholar]
- 15.Jackson R, Wells S, Rodgers A. Will screening individuals at high risk of cardiovascular events deliver large benefits? Yes. BMJ 2008;337:a1371 10.1136/bmj.a1371 [DOI] [PubMed] [Google Scholar]
- 16.Capewell S, Lloyd-Jones DM. Optimal cardiovascular prevention strategies for the 21st century. JAMA 2010;304:2057–8. 10.1001/jama.2010.1641 [DOI] [PubMed] [Google Scholar]
- 17.Ebrahim S, Taylor F, Ward K et al. Multiple risk factor interventions for primary prevention of coronary heart disease. Cochrane Database Syst Rev 2011;(1):CD001561 10.1002/14651858.CD001561.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berger JS, Jordan CO, Lloyd-Jones D et al. Screening for cardiovascular risk in asymptomatic patients. J Am Coll Cardiol 2010;55:1169–77. 10.1016/j.jacc.2009.09.066 [DOI] [PubMed] [Google Scholar]
- 19.Mehta S, Wells S, Grey C et al. Initiation and maintenance of cardiovascular medications following cardiovascular risk assessment in a large primary care cohort: PREDICT CVD-16. Eur J Prev Cardiol 2014;21:192–202. 10.1177/2047487312462150 [DOI] [PubMed] [Google Scholar]
- 20.Ioannidis JP. More than a billion people taking statins? Potential implications of the new cardiovascular guidelines. JAMA 2014;311:463–4. 10.1001/jama.2013.284657 [DOI] [PubMed] [Google Scholar]
- 21.von Elm E, Altman DG, Egger M et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008;61:344–9. 10.1016/j.jclinepi.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 22.Health and Social Care Information Centre. NHS Health Check secondary use dataset, 2014. http://www.hscic.gov.uk/nhshealthcheck (accessed 13 Mar 2014).
- 23.Office of National Statistics. Presentation of ethnic group data, 2015. http://www.ons.gov.uk/ons/guide-method/measuring-equality/equality/ethnic-nat-identity-religion/ethnic-group/presentation-of-ethnic-group-data.html (accessed 28 Aug 2015).
- 24.Townsend P, Phillimore P, Beattie A. Health and Deprivation: Inequality and the North. London: Croom Helm, 1988. [Google Scholar]
- 25.Robson J, Dostal I, Madurasinghe V et al. The NHS Health Check programme: implementation in east London 2009–2011. BMJ Open 2015;5:e007578 10.1136/bmjopen-2015-007578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.NICE. Lipid modification: cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease. CG181. London: National Institute for Health and Care Excellence, 2014. [PubMed] [Google Scholar]
- 27.Sheikh A, Nurmatov UB, Cresswell K et al. Investigating the cost-effectiveness of health information technologies: a systematic review protocol. BMJ Open 2013;3:e003737 10.1136/bmjopen-2013-003737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hippisley-Cox J, Coupland C, Vinogradova Y et al. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ 2008;336:1475–82. 10.1136/bmj.39609.449676.25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wells S, Furness S, Rafter N et al. Integrated electronic decision support increases cardiovascular disease risk assessment four fold in routine primary care practice. Eur J Cardiovasc Prev Rehabil 2008;15:173–8. 10.1097/HJR.0b013e3282f13af4 [DOI] [PubMed] [Google Scholar]
- 30.Coffey C, Cooper AM, Brown T et al. Vascular health checks in Salford. Manchester: University of Salford, 2014. http://usir.salford.ac.uk/35581/1/final_farsite_report.pdf (accessed 20 Aug 2015). [Google Scholar]
- 31.Chipchase L. An insight into the NHS health Check programme in Birmingham: NHS Health Checks national learning network, 2012. http://www.nhshealthcheck.nhs.uk/default.aspx?aID=45 (accessed 13 Mar 2014).
- 32.Hill S, Spink J, Cadilhac D et al. Absolute risk representation in cardiovascular disease prevention: comprehension and preferences of health care consumers and general practitioners involved in a focus group study. BMC Public Health 2010;10:108 10.1186/1471-2458-10-108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liew SM, Blacklock C, Hislop J et al. Cardiovascular risk scores: qualitative study of how primary care practitioners understand and use them. Br J Gen Pract 2013;63:e401–7. 10.3399/bjgp13X668195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krska J, du Plessis R, Chellaswamy H. Views and experiences of the NHS Health Check provided by general medical practices: cross-sectional survey in high-risk patients. J Public Health (Oxf) 2015;37:210–17. 10.1093/pubmed/fdu054 [DOI] [PubMed] [Google Scholar]
- 35.Artac M, Dalton AR, Majeed A et al. Effectiveness of a national cardiovascular disease risk assessment program (NHS Health Check): results after one year. Prev Med 2013;57:129–34. 10.1016/j.ypmed.2013.05.002 [DOI] [PubMed] [Google Scholar]
- 36.Smith S, Waterall J, Burden AC. An evaluation of the performance of the NHS Health Check programme in identifying people at high risk of developing type 2 diabetes. BMJ Open 2013;3:pii: e002219.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van Staa TP, Smeeth L, Ng ES et al. The efficiency of cardiovascular risk assessment: Do the right patients get statin treatment? Heart 2013;99:7 10.1136/heartjnl-2013-303698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Prochazka AV, Lundahl K, Pearson W et al. Support of evidence-based guidelines for the annual physical examination: a survey of primary care providers. Arch Intern Med 2005;165:1347–52. 10.1001/archinte.165.12.1347 [DOI] [PubMed] [Google Scholar]
- 39.Krogsboll LT, Jorgensen KJ, Gronhoj Larsen C et al. General health checks in adults for reducing morbidity and mortality from disease: Cochrane systematic review and meta-analysis. BMJ 2012;345:e7191 10.1136/bmj.e7191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Krogsboll LT, Jørgensen KJ, Gøtzsche PC. Health checks. Letter to the editor. The Times 20/08/2013.
- 41.Krogsboll LT, Jorgensen KJ, Gotzsche PC. Universal health checks should be abandoned. BMJ 2013;347:f5227 10.1136/bmj.f5227 [DOI] [PubMed] [Google Scholar]
- 42.Shapiro S, Fink R, Rosenberg C. A program to measure the impact of multiphasic health testing on health differentials between poverty and nonpoverty groups. Med Care 1972;10:207–14. 10.1097/00005650-197205000-00003 [DOI] [PubMed] [Google Scholar]
- 43.Thorner RM, Djordjevic D, Vuckmanovic C et al. A study to evaluate the effectiveness of multiphasic screening in Yugoslavia. Prev Med 1973;2:295–301. 10.1016/0091-7435(73)90072-8 [DOI] [PubMed] [Google Scholar]
- 44.South-East London Screening Study Group. A controlled trial of multiphasic screening in middle-age: results of the South-East London Screening Study. The South-East London Screening Study Group. Int J Epidemiol 1977;6:357–63. 10.1093/ije/6.4.357 [DOI] [PubMed] [Google Scholar]
- 45.Bennett AE, Fraser IG. Impact of a screening programme in general practice: a randomized controlled trial. Int J Epidemiol 1972;1:55–60. 10.1093/ije/1.1.55 [DOI] [PubMed] [Google Scholar]
- 46.Tibblin G, Welin L, Larsson B et al. The influence of repeated health examinations on mortality in a prospective cohort study, with a comment on the autopsy frequency. The study of men born in 1913. Scand J Soc Med 1982;10:27–32. [DOI] [PubMed] [Google Scholar]
- 47.Lannerstad O, Sternby NH, Isacsson SO et al. Effects of a health screening on mortality and causes of death in middle-aged men. A prospective study from 1970 to 1974 of mean in Malmo, born 1914. Scand J Soc Med 1977;5:137–40. [DOI] [PubMed] [Google Scholar]
- 48.Olsen DM, Kane RL, Proctor PH. A controlled trial of multiphasic screening. N Engl J Med 1976;294:925–30. 10.1056/NEJM197604222941705 [DOI] [PubMed] [Google Scholar]
- 49.Wilhelmsen L, Berglund G, Elmfeldt D et al. The multifactor primary prevention trial in Goteborg, Sweden. Eur Heart J 1986;7:279–88. [DOI] [PubMed] [Google Scholar]
- 50.Friedman GD, Collen MF, Fireman BH. Multiphasic health checkup evaluation: a 16-year follow-up. J Chronic Dis 1986;39:453–63. 10.1016/0021-9681(86)90112-8 [DOI] [PubMed] [Google Scholar]
- 51.World Health Organization European Collaborative Group. WHO European collaborative trial in the multifactorial prevention of coronary heart disease. WHO, 1989. [PubMed] [Google Scholar]
- 52.No authors listed]. Effectiveness of health checks conducted by nurses in primary care: final results of the OXCHECK study. Imperial Cancer Research Fund OXCHECK Study Group. BMJ 1995;310:1099–104. 10.1136/bmj.310.6987.1099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet 1994;344:1383–9. [PubMed] [Google Scholar]
- 54.Theobald H, Bygren LO, Carstensen J et al. Effects of an assessment of needs for medical and social services on long-term mortality: a randomized controlled study. Int J Epidemiol 1998;27:194–8. 10.1093/ije/27.2.194 [DOI] [PubMed] [Google Scholar]
- 55.Jorgensen T, Borch-Johnsen K, Thomsen TF et al. A randomized non-pharmacological intervention study for prevention of ischaemic heart disease: baseline results Inter99. Eur J Cardiovasc Prev Rehabil 2003;10:377–86. 10.1097/01.hjr.0000096541.30533.82 [DOI] [PubMed] [Google Scholar]
- 56.Thomsen JL, Parner ET, Karlsmose B et al. Effect of preventive health screening on long-term primary health care utilization. A randomized controlled trial. Fam Pract 2005;22:242–8. 10.1093/fampra/cmi007 [DOI] [PubMed] [Google Scholar]
- 57.Jorgensen T, Jacobsen RK, Toft U et al. Effect of screening and lifestyle counselling on incidence of ischaemic heart disease in general population: Inter99 randomised trial. BMJ 2014;348:g3617 10.1136/bmj.g3617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Daily Mail. Why statins might be pointless and even bad for you 2008. http://www.dailymail.co.uk/health/article-1340299/Why-taking-statins-pointless--bad-you.html
- 59.Godlee F. Statins and the BMJ. BMJ 2014;349:g5038 10.1136/bmj.g5038 [DOI] [PubMed] [Google Scholar]
- 60.Collins R. Doctors fears over statins may cost lives. The Guardian 21/3/2014.
- 61.Appleby J. Is general practice in trouble? BMJ 2014;349:g6814 10.1136/bmj.g6814 [DOI] [PubMed] [Google Scholar]
- 62.Majeed A, Rawaf S, De Maeseneer J. Primary care in England: coping with financial austerity. Br J Gen Pract 2012;62:625–6. 10.3399/bjgp12X659150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.National Audit Office. Delivering efficiency savings in the NHS, 2011. http://www.nao.org.uk/wp-content/uploads/2011/12/NAO_briefing_Delivering_efficiency_savings_NHS.pdf (accessed 12 Mar 2015).
- 64.NHS England. NHS Health Checks Data, 2011. http://www.england.nhs.uk/statistics/statistical-work-areas/integrated-performance-measures-monitoring/nhs-health-checks-data (accessed 12 Mar 2015).
- 65.Research Works Limited. Understanding the implementation of NHS Health Checks: Research Report: Public Health England, 2013. http://www.healthcheck.nhs.uk/document.php?o=351 (accessed 20 Feb 2014).
- 66.Public Health England. NHS Health Check implementation plan review and action plan, 2013. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/224805/NHS_Health_Check_implementation_review_and_action_plan.pdf (accessed 13 Mar 2015).