Abstract
Objectives
To describe the beliefs and attitudes to organ donation in the Arabic-speaking community.
Design
Arabic-speaking participants were purposively recruited to participate in 6 focus groups. Transcripts were analysed thematically.
Participants
53 participants, aged 19–77 years, and originating from 8 countries, participated in 1 of 6 focus groups. Participants identified as Christian (73%), Islam (26%), Buddhist (2%) or did not identify with any religion (2%).
Results
6 themes (with subthemes) were identified; religious conviction; invisibility of organ donation; medical suspicion; owning the decision; and reciprocal benefit.
Conclusions
Although organ donation is considered a generous life-saving ‘gift’, representative members of the Arabic-speaking community in Australia were unfamiliar with, unnerved by and sceptical about the donation process. Making positive decisions about organ donation would likely require resolving tensions between respecting family, community and religious values versus their individual autonomy. Providing targeted education about the process and benefits of organ donation within the Arabic community may clarify ambiguities surrounding cultural and religious-based views on organ donation, reduce taboos and suspicion towards donation, and in turn, lead to increased organ donation rates.
Keywords: TRANSPLANT MEDICINE, QUALITATIVE RESEARCH, PUBLIC HEALTH
Strengths and limitations of this study.
First known qualitative study to elicit the perspectives on organ donation in the Arabic-speaking community in a country where they are an ethnic minority group.
Researcher triangulation and multiple coding were used to strengthen the rigour of the research.
Participants were recruited using market research companies, which may have introduced a potential selection bias.
Introduction
Deceased organ donation rates fall short of demand in the great majority of advanced countries, principally because of low rates of conversion of potential donors to actual donors.1–3 This is despite concerted and directed efforts to increase deceased donation by promoting the benefits of transplantation to the general population.4 The challenge is greater in ethnic minority populations, with rates of deceased donation markedly lower than their respective wider community. This is reflected in their limited proportion of organ donor registrations and family consent when organ donation is discussed in the acute hospital setting.5–9
In the USA, the deceased organ donation consent rate between 2008 and 2011 for the white population was 77.0%, compared with 67.5% for Hispanics, 54.9% for African-Americans and 48.1% for Asians.6 Similar trends have also been noted in the UK where ethnic minority groups account for 8% of the population, but constitute 24% of the waiting list for kidneys,10 and only 3% of deceased donors.11 A recent systematic review suggested that these differences may be explained by the lack of awareness about transplantation within their communities, dominant influences of older family members, religious myths and misconceptions, fear of premature death, concerns about bodily disfigurement, distrust of the medical system, and concerns of racial discrimination in organ allocation.12
In Australia, the Arabic language is the fourth most common spoken at home, spoken by 1.4% of the national population,13 Arabic speakers accounted for 0.07% of deceased donors, and only one donor between 2007 and 2011.14 In the Sydney Local Area Health District as at 31 December 2014, 10% of the kidney transplant waiting list (n=150) identified as Arabic speaking. Moreover, between 2010 and 2014 inclusively, 11% of deceased donor kidney transplant recipients in this Health District identified as Arabic speaking. In contrast, there were no deceased donations from within this population.15 The reasons for these observations are largely unknown with few studies having been conducted on community perspectives on organ donation in the Arabic-speaking population.16 17 This is the first known qualitative study to elicit the perspectives on organ donation in the Arabic-speaking community in a country where they are an ethnic minority group. It aims to describe the attitudes and beliefs of this population towards deceased organ donation and to assist development of education and other strategies and policies that might potentially lead to an overall increase in deceased organ donation rates.
Patients and methods
This reporting of this study is based on the Consolidated Criteria for Reporting Qualitative Health Research (COREQ) as shown in online supplementary file 1.18
Participant selection
A market research company was used to purposively select Arabic-speaking participants residing in Sydney, Australia, to achieve a range of sociodemographic characteristics including gender, age, employment status, marital status, nationality and migration status (first or second generation). The market research company recruited participants through their databases, advertising and snowball sampling. Participants were eligible if they were aged over 18 years, spoke both Arabic and English language, and able to provide informed consent. Focus groups were convened by age groups (18–30, 31–50, 51 years and over) to encourage rapport. Participants were reimbursed A$90 to cover their transportation and incidental costs.
Data collection
The focus group topic guide was based on a systematic review19 and discussion among the research team, and included questions on awareness, attitude and beliefs about deceased organ donation (see online supplementary table S2). Towards the end of the focus group, Australian organ donation and transplantation rates (see online supplementary table S3) were provided to participants who were asked to suggest reasons for the lower rates of donation in ethnic minority groups and provide suggestions to improve community awareness and willingness to donate. One of the investigators (AFR/AA/RDMA/AT) facilitated one or two, 2 h, focus groups during June 2014. All focus group sessions were conducted in English in absence of resources to support a trained Arabic-speaking researcher to facilitate all groups. Groups were held in hired meeting rooms. Field notes were recorded by a second investigator (AFR/AA/RDMA/AT/KH). Focus groups ceased when theoretical saturation was reached, that is, when few or no new concepts or topics were raised in subsequent group discussions. All focus groups were digitally audio-taped and video-taped, and transcribed.
Analysis
The transcripts were entered into HyperRESEARCH qualitative data management software (ResearchWare Inc, V.3.5.2, Randolph, Massachusetts, USA). One author (AFR) coded the transcripts following the principles of grounded theory20 and thematic analysis where concepts were identified inductively from the data and new codes were created when necessary. HyperRESEARCH was used to generate a report of all codes with the corresponding text allowing similar concepts to be grouped into themes. Conceptual links and patterns among themes and subthemes were identified and mapped into a thematic schema. Researcher triangulation was conducted whereby AFR discussed the preliminary themes with three other researchers (AA, AT, RDMA) who read the transcripts independently and confirmed that the themes captured the full range of participants’ perspectives.
Results
We conducted six focus groups with 53 participants (95% attendance rate) during June 2014. The participant characteristics are provided in table 1 and the focus group composition in online supplementary table S4. The age of participants ranged from 19 to 77 years (mean 40.7, SD 14.5) and 45% of participants were male. Notably, 14 (26%) participants were born in Lebanon. In terms of religion, participants identified as Christian (n=37 (70%)), Islam (n=14 (26%)), Buddhist (n=1 (2%)) or no religion (n=1 (2%)). The participants’ intention to donate and registration status are shown in table 2. Approximately half (51%) of the participants were unsure whether they were willing to donate their organs after death, while 38% and 11% would and would not, respectively, intend to be a deceased organ donor.
Table 1.
Participant characteristics (N=53)
| Characteristic | N (%) |
|---|---|
| Gender | |
| Male | 24 (45) |
| Female | 29 (55) |
| Age (years) | |
| 18–20 | 2 (4) |
| 21–30 | 13 (25) |
| 31–40 | 12 (23) |
| 41–50 | 11 (21) |
| 51–60 | 11 (21) |
| 61–70 | 4 (8) |
| Marital status | |
| Married/de facto | 26 (49) |
| Divorced/separated | 3 (6) |
| Partner (not living with) | 5 (9) |
| Widowed | 1 (2) |
| Single | 15 (28) |
| Country of birth | |
| Australia | 21 (40) |
| Lebanon | 14 (26) |
| Egypt | 5 (9) |
| Jordan | 3 (6) |
| Saudi Arabia | 2 (4) |
| Other | 5 (9) |
| Mother's country of birth | |
| Australia | 2 (4) |
| Lebanon | 28 (53) |
| Egypt | 7 (13) |
| Jordan | 4 (8) |
| Syria | 2 (4) |
| Other | 8 (15) |
| Father's country of birth | |
| Australia | 1 (2) |
| Lebanon | 26 (49) |
| Egypt | 7 (13) |
| Jordan | 5 (9) |
| Syria | 4 (8) |
| Other | 8 (15) |
| Religion | |
| Christianity | 37 (70) |
| Islam | 14 (26) |
| Buddhism | 1 (2) |
| No religion | 1 (2) |
| Language/s spoken at home | |
| English and Arabic | 39 (74) |
| Arabic only | 10 (19) |
| English only | 3 (6) |
| English, French and Arabic | 1 (2) |
Table 2.
Donation and registration characteristics (N=53)
| Characteristic | n (%) |
|---|---|
| Registration status | |
| Registered organ donor | 10 (19) |
| Registered intent to not donate | 0 (0) |
| Not registered | 42 (79) |
| Registration method | |
| Drivers licence | 10 (19) |
| Australian Organ Donor Register | 0 (0) |
| Intention to be an organ donor | |
| Yes | 20 (38) |
| No | 6 (11) |
| Unsure | 27 (51) |
| Communicated intent with family member | |
| Yes | 18 (34) |
| No | 34 (64) |
| View on organ donation | |
| Very much against organ donation | 1 (2) |
| Against organ donation | 4 (8) |
| Neither for nor against organ donation | 27 (51) |
| In favour of organ donation | 8 (16) |
| Very much in favour of organ donation | 13 (25) |
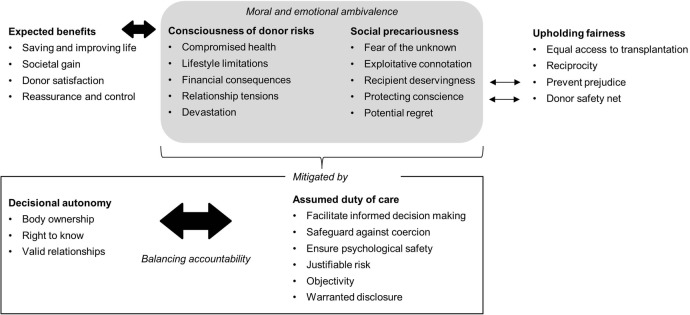
Six themes were identified: protecting family and community cohesiveness, religious conviction, invisibility of organ donation, medical suspicion, owning the decision, and reciprocal benefit; which are described in the following section. Selected quotations for each theme are provided in table 3. The conceptual links relationships among themes are portrayed in figure 1.
Table 3.
Illustrative quotations
| Theme | Illustrative quotations |
|---|---|
| Protecting family and community cohesiveness | |
| Respecting parental authority | I would say while my mum is alive and if I die first, I wish to do whatever to please her. So if she wants me in one piece, I'm in one piece. (FG5, woman, 20s) I think my family has a large influence on what I do and my decisions so I respect their opinion. What they think about what I do is very important to me and it always has been. So my mother being totally against it is probably the only reason I haven't really changed my mind about it as yet. (FG4, woman, 30s) |
| Intense emotionality | You've got to use emotions to get to the community. We're highly emotional people. (FG3, woman, 30s) |
| Avoiding taboo | It's a bit like jinxing yourself if you talk about death and what's going to happen, you might bring it on. So they don't want to talk about it. (FG6, woman, 50s) I can't even bring up the subject…you don't discuss it with your parents or your child because they will just go insane. (FG3, woman, 30s) |
| Fearing judgement | We live in an environment where you are not allowed to do this…that…no. No. No. No. If I do something bad everyone talks about me. The community, we are not individuals. If I do something wrong they put a black spot on me and say alright she is a so and so…and we don't accept organ donation. (FG1, woman, 50s) |
| Religious conviction | |
| Clarifying ambiguity | You have to be generous and help people out no matter what. But then it comes back to that grey area, saying ‘No. No. No. No. No.’ (FG3, woman, 30s) I'm going to go and ask my priest…I don't know if it's a sin or not to donate your body parts. Right? So there's a lot of things that aren't touched upon. (FG4, woman, 40s) |
| Adhering to religious requirements | From my belief, if you do something like that you would go straight to heaven. From my religion. (FG4, woman, 30s) Religiously, you're burying someone, in like Islam, straightaway. So for someone, for a culture that's big on making sure you're burying someone straightaway last funeral I went to was like, within hours of the person passing away. That is a barrier in itself. (FG5, man, 40s) |
| Invisibility of organ donation | |
| Proximity and direct relevance | I'm not aware of anyone in our little community, from our village and so forth, that has had a transplant, but if they had, I know, for a fact that everyone would rally around them and change their opinion. But I think because it's not an immediate threat to (my family), they're not really considering it—‘cause they only considering it from the giving perspective, not from the receiving perspective as well. (FG5, woman, 20s) |
| Lack of conceptual familiarity | They are not educated…Like my parents, like my dad didn't even go to high school. He doesn't know anything about organs. (FG2, woman, 20s) They just have to hear it over and over until it's normal ‘cause if you come up with someone that hasn't heard of that who is like, “Are you normal? What are you talking about? Why I wanna remove and organ from my family member? Yeah, I'm afraid of it.” (FG2, man, 20s) |
| Apathy for registration | A lot of people from our community don't vote. It's just like that. They don't wanna know about it and they don't do it. So I think this is very similar, like they're just not interested at all. (FG4, man, 30s) |
| Medical suspicion | |
| Visceral fear of organ removal | When I think of organ donation, I just think it's scary. I don't want to think about it. It scares me. (FG4, woman, 30s) |
| Wary about less effort to save donors | What if I'm not completely dead and they decide to save someone else's life and so they're making a decision about who to be saved. (FG6, woman, 50s) If they know you're an organ donor, and you're dying, they will make you die. (FG2, woman, 20s) |
| Losing body dignity | You become a nobody. From being someone with a name and shape, and stuff, you become just a number. Especially the idea of donating tissue is really scary ‘cause they chop everything and take the bones, and they put tubes inside you. (FG4, man, 40s) |
| Transferring historical scepticism | It happened in Lebanon where they took this guy…made him sign this paper saying, ‘In case you die, would you allow us to donate your organs?’ And he agreed…and what they did is they actually killed him. (FG5, man, 40s) We paid 25 000 dollars for my cousin's kidney in Lebanon. (FG3, man, 30s) |
| Questioning differential allocation | The worst part is you're doing it out of generosity, but actually there is someone who's a billionaire living out of you. Benefitting out of your parts. (FG4, man, 50s) I'm worried that somebody's gonna get hold of that register and there's gonna be some financial transactions, I think. (FG4, man, 40s) |
| Owning the decision | |
| Saving lives | If we can save others’ lives then why not? It's a beautiful thing. (FG3, man, 30s) I wanna donate…especially give a child sight or somebody a liver. That gives me so much pleasure to know that I would be doing that. (FG4, woman, 40s) |
| Gaining independence | I think the older generation have this really old view, but I think a lot of us, younger Lebanese, have moved away, broken away from tradition and we've become our own individuals now and we're raising kids Australianised, totally different to what our parents raised us. We're not as strict. We still have Lebanese values, but we love this country so we're trying to embrace it. So in my opinion, family's opinion does not count. (FG4, woman, 30s) |
| Anticipating family resistance | Even if I say yes, I would like to donate my organ…If I was to pass away and family was to take the decision, I'm sure mum's decision would stand. So really, I've got no say. (FG5, woman, 20s) |
| Reciprocal benefit | |
| The Arab community go, What's in it for me? That's the mentality thing…If someone in my family say, “I expect to get paid for this.” (FG5, man, 40s) I think there's just no motivation. Why should I put my mum's body through trauma although she's passed away, when really I don't even know what's gonna happen with her—that organ, do you know what I mean? I don't even know whether or not that is gonna be used. (FG5, woman, 20s) |
|
FG, focus group.
Figure 1.
Thematic schema. Participants believed in the life-saving act of donation; however, this was in conflict with the need to adhere and respect their family and community values. Participants were largely unfamiliar with organ donation and thus desired to turn to their religion as a form of guidance, requiring their religion's stance on the issue. Participants were sceptical of donation and the donation process and questioned the impartiality of medical practitioners.
Protecting family and community cohesiveness
Respecting parental authority: Participants believed that family opinion was the dominant influence in their own decision about being an organ donor, with some stating that parental authority held the most sway. They placed emphasis on wishing to please their parents. Their guidance and approval was seen to be important, particularly for the younger participants, even for those who were married and had children of their own. If their parents were deceased, then participants perceived that their own decision would carry more weight.
Intense emotionality: Some participants expressed that Arabic-speaking people were ‘highly emotional’ and would avoid discussing organ donation to minimise negative reactions and responses from their relatives, such as, acting ‘hysterically’, ‘crazily’ and ‘illogically’. Hence, they suggested that campaigns to increase donation rates within their community would need to ‘tug at the heartstrings’ and tap into their emotions, for example, by portraying images of sick children from within their own Arabic-speaking community in need of an organ transplant.
Avoiding taboo: Discussing topics relating to ‘death’, such as organ donation, life insurance and writing a will, was seen as ‘jinxing’ death. Hence, the subject of organ donation was rarely broached within the focus group participants’ families and their community. Many noted that the older generation were the most reluctant to discuss such topics. Some participants felt too ‘unnerved’ and were unable to discuss hypothetical scenarios where they were asked to make a decision whether or not to donate their family member's organs for purposes of life-saving transplantation.
Fearing judgement: Arabic-speaking people were believed to live in close-knit and enmeshed communities, which meant that participants felt that they had to adhere to accepted social and cultural norms. If not, they feared that they would be judged adversely by their community. Some participants were afraid that their community could regard organ donation as being unacceptable and therefore believed that they would be vulnerable to criticism or disapproval if they should register to be an organ donor, or consented for a family member's organs to be removed.
Religious conviction
Clarifying ambiguity: Some participants were unsure if their religion defined organ donation as ‘good’ or ‘bad’, stating that they had received mixed messages. They claimed that there were ‘grey areas’ in religious texts, and that leaders in their church or mosque had not raised the topic of organ donation. They desired education and clarification on deceased organ donation from religious leaders as they wanted to be ‘100% sure’ before registering their intent to donate. Participants also felt conflicted between the religious values of being charitable and helping people (such as saving a life) and not being ‘allowed to donate’ for religious reasons such as the need to avoid cutting the body after declaration of death. Equally, for some it was difficult to differentiate between religious values and perceived cultural norms.
Adhering to religious requirements: Some believed that their religion encouraged donation and that the organ donor would be rewarded by going ‘straight to heaven’ for helping others. However, others believed that their religion prevented them from donating. For example, participants were under the impression that Islam emphasised the importance of returning one's body to the earth intact and as soon as possible after death and feared that organ donation would interfere with both of these requirements.
Invisibility of organ donation
Proximity and direct relevance: Organ donation was believed to be ‘out of sight, out of mind’ by some participants. They felt that it was irrelevant to their community as they were unaware of donations occurring in their country of origin or in their community within Australia. Despite being unable to direct a deceased organ to a specific individual, they believed they would consider being a deceased donor if they knew someone within their own community who needed an organ as this would hold more personal meaning. Others who had relatives that had either needed or received a transplant, maintained that they were entirely supportive towards donation and would ‘approach and tell people’ about it.
Lack of conceptual familiarity: Organ donation was viewed as a foreign concept that participants knew little about due to lack of exposure. Raising awareness, particularly in schools was considered to be important. Also, participants believed that having knowledge regarding the organ donation process (including timing and length of the potential surgery, what it involves and how the donation affects the appearance of the deceased), as well as organ matching and success rates, would assist them in deciding whether or not to donate their own or their family member's organs. Participants believed that the older generation in Arabic-speaking communities who had less education would struggle to understand organ donation due to their difficulties with the English language and lack of education and knowledge about disease processes and the human body.
Apathy for registration: Some participants ‘had not been bothered’ to register their decision to donate, did not know how to register or indicated that the register was not easily accessible. Participants believed that for Arabic-speaking people, the ‘disinterest’ in registering to donate was similar to voting, that is, unless one was extremely passionate about making a particular decision “they don't want to know about it and they don't do it…they're just not interested at all.”
Medical suspicion
Visceral fear of organ removal: The topic of organ donation was considered by participants to be inherently confronting. Some felt more uncomfortable with the notion of removing particular organs such as the heart and eyes.
Wary about less effort to save donors: Some participants suspected that physicians might not strive to save the life of a registered donor if their organs were needed for another patient. Participants had heard many and read about such stories through television, movies, books and by word of mouth. Physicians were seen to have the power to make a decision about whose life should be saved.
Losing body dignity: Organ donation was viewed by some participants as tampering with the body. The process of cutting the dead body was seen as disrespecting the deceased person. Protecting the physical appearance of an intact-body postdonation was important to participants, especially as many families conducted viewings of the deceased prior to burial.
Transferring historical scepticism: Participants, specifically first-generation migrants, believed that their understanding of the medical system from their country of origin influenced their view of the Australian medical system, and thus organ donation. For example, some feared that their organs could potentially be sold on the black market, that their organs could be removed before they were declared dead or that they could be killed for their organs. They had either personally witnessed or heard stories of these practices ‘happening over there—in the Arab world or the Middle East’. Furthermore, they felt that money was essential to access healthcare and that there were ‘no rules or protection for the human’, thus only the wealthy would be able to access medical care and be able to benefit from organ donation. Some younger participants, educated in Australia, had trust in and respect for the Australian healthcare system. However, they believed that older Arabic-speaking people held on to their traditional ways of thinking and suspicion.
Questioning differential allocation: Some participants distrusted the allocation system and suspected that the wealthy or well-connected individuals were more likely to receive a deceased donor organ for transplantation. Some suggested that financial transactions, such as bribes and ‘kick-backs’, took place. They acknowledged that the current national allocation system in Australia was equitable as long as it was based on blood type, age and medical urgency. However, they also thought that having health insurance might guarantee ‘priority’ on the waitlist and this they considered to be unfair. However, others assumed correctly, or trusted, that Australia had a transparent, fair and ethical system of deceased donor organ allocation.
Owning the decision
Saving lives: Organ donation was perceived by some participants as a ‘noble’ and ‘humane’ act. A strong potential motivator to donate their own or their family member's organs was the idea that such organs were no longer needed in the deceased and could be used to ‘help someone else live’. Some participants believed that donating their family member's organs would bring them a sense of satisfaction from ‘changing someone's life’ as well as reducing the recipient's family from feeling the loss and grief that they would be experiencing.
Gaining independence: Personal opinion and choice was believed to be the most important factor by some participants, particularly among the younger aged focus groups. They believed that intrinsic autonomy was more important in deciding whether to be a deceased organ donor than external family or religious influences. Second-generation and third-generation immigrants felt that they had ‘broken away from tradition’ and had become ‘Australianised’, and could therefore make an autonomous decision about organ donation.
Anticipating family resistance: Of the participants who would consent to be an organ donor, some believed that their decision to donate would cause tension within their family, particularly if a decision had to be made if they died. Because they anticipated that their family would argue and ultimately veto their decision to donate due to their strong resistance against the concept of organ donation, participants felt they had ‘no say’ in their donation decision. One participant had registered to donate her organs through her driver's licence until an older brother found out and escorted her back to the local office of the Road and Traffic Authority (the government body responsible for issuing drivers licences and where registration for donation previously took place) to reverse her decision.
Honouring donor wishes: Many participants felt that their decision to either donate or not donate their organs should be binding. They believed that it would be ‘selfish’ for their family to over-rule their decision, and would themselves respect the deceased's wishes if known or if they were a registered donor. Legislating against the family right to veto the deceased's decision to donate was believed by some participants to be beneficial to the family as it would take this decision out of their hands at a very difficult and emotional time and thus avoid worsening their grief.
Reciprocal benefit
Organ donation was considered to be a significant gift, and some believed that families should gain mutual benefit from their decision to donate. They also believed that the Arabic-speaking community may question ‘What's in it for me? I would expect to be paid for this’. Others suggested that families should receive a reward such as money for their family, better future access to medical assistance in the form of free private health insurance, or financial assistance with funeral costs.
Discussion
This focus group study confirmed that the Arabic-speaking community in Australia were aware of the life-saving benefits of transplantation using deceased donor organs. While the participants, a mixture of first-generation, second-generation and third-generation migrants to Australia, universally applauded the generosity of donor families in Australia, they were collectively ambivalent about the prospects of improvement of the deceased organ donation rate in their own Arabic-speaking community in the short to medium term. Individual values and attitudes to deceased organ donation were seen to be in conflict with the desire to respect and abide by family and community cultures and traditions. These values were not explicitly discouraging organ donation, but rather caused them to feel vulnerable and uneasy about the act of donation. Religious ambiguities about the virtue of organ donation were evident, with confusion expressed as to their family religion's stance on organ donation, particularly by those identifying to be of Islamic faith. For some, these ambiguities may have provided an easy ‘opt-out’ clause to justify their own negative attitudes to deceased organ donation that were, in turn, principally based on cultural norms and family expectations.
The majority of the focus group participants were of Christian faith from Lebanon, Egypt and Syria, and very likely representative of the Arabic-speaking community living at present in metropolitan Sydney, a city of almost five million inhabitants. From a global perspective, 85% of Arabic speakers are of Islamic faith. Prior to 1975 and the civil war in Lebanon, the majority of Arabic-speaking migrants to Sydney came to Australia for economic reasons and were of Christian faith. Subsequently, and on humanitarian grounds, migration of both Christians and Muslims became easier, particularly if extended family members were already established in Australia, and for those from poorer and less well-educated rural areas. Recently, the majority of Arabic-speaking migrants to Australia have been of Islamic faith and from war-torn countries of Iraq, Iran, Afghanistan and Syria. Irrespective of their faith, they were likely to come from communities where healthcare was sparse and governments could not be trusted. Further, such countries have little or no access to deceased organ donation with rates per million population (PMP) falling below five for many countries in the Middle East (Lebanon: 2 PMP; Saudi Arabia: 2.5 PMP; Kuwait: 4 PMP).21
Also in common and deeply embedded within the structure of Arab identity, is the role community and family.22 Understandably, respect for the elderly members of the family is paramount, and traditionally, parents act as gate keepers who make the important decisions, such as organ donation. Some second-generation and third-generation immigrants, who considered themselves more socially integrated into the dominant ‘Australian’ culture, contend with dissonance between their individual positive beliefs about organ donation and the Australian healthcare system, and the suspicions and fears held by members of their family and the Arabic-speaking community. Similarly, in the USA, greater acculturation of immigrants is associated with greater odds of believing organ donation to be justified.17 This tension between migrant generations, referred to as an intergenerational acculturation gap,23–25 has been linked to family and social conflict and adjustment.26–29 Thus, it is not surprising that our study found that many were concerned about negative appraisal by their family and community, and anticipated family resistance and conflict if they are registered as an organ donor. It is also consistent with a recent systematic review: while younger generations in minority communities held more westernised views and were more likely to support organ donation, the beliefs of older family members who were less likely to support donation had dominant influence.12
Our study confirms findings from previous research conducted in both the general community30 and ethnic minority groups12 that have consistently identified that a lack of trust in doctors and the healthcare profession is a major barrier to deceased organ donation. Participants in our study also expressed fears that doctors would not try as hard to save the life of an organ donor with physicians holding the power to decide whose life to save, as well as the belief that the wealthy and ‘well connected’ were more likely to obtain a transplant. It appears these suspicions and fears were transferred from their countries of origin, because they observed the lack of mechanisms to protect the needs and interests of vulnerable members of the community in the country from which they originated. Similar anxieties have been expressed in other ethnic minority populations including Chinese-Canadians;31 Hispanics, African-Americans and Asian-Americans in the USA;32–35 and black Caribbean and black Africans in the UK.5 While these beliefs may be easily dismissed as misconceptions in the Western context, our study provides new insights as members of the Arabic-speaking community explained their origin of beliefs to be based on publicised healthcare practices reportedly occurring in the Middle East, for example, black market trading of organs, bribery for organs and removal of organs before being declared deceased.
The importance of religion was evident across all age groups. Many participants looked to their religion's view on donation as a benchmark for their own beliefs, however were unaware or confused on their religion's stance and desired guidance by religious leaders. This appeared to apply to a greater extent to those of Muslim faith rather than those identifying as Christian, many of who believed Christianity encouraged donation. A recent Turkish study revealed that Mosque Imams had little knowledge of organ donation and were unwilling to donate their organs.36 In the USA, a study found that people of African, Hispanic, black Caribbean and South Asian heritage were more likely to regard organ donation as unacceptable to their religious beliefs compared with the general population.12 Notably, the European Council for Fatwa and Research has issued three fatwas permitting organ donation37 and the Pope and other religious leaders of people of Hindu, Jewish, Orthodox, Buddhist faiths have all issued statements encouraging followers to donate.38–40 It is plausible that the lower rates of donation among ethnic minorities are not be explained by specific religious factors in and of themselves, but rather, lack of awareness of their faith's position on deceased donation.41
This is the first known qualitative study to elicit the perspectives on organ donation in the Arabic-speaking community in a country where they are an ethnic minority group. However, we acknowledge some potential limitations. Recruiting participants registered with market research companies may have introduced a potential selection bias. However, we were able to capture the range of demographic characteristics that match the migration patterns of Arabic speakers to Australia, and in particular to Sydney, where according the 2011 national population census, up to 60% of households in some suburban areas within the Sydney Local Health District report Arabic as the principal language spoken at home (13). We were not able to measure the proficiency of Arabic speaking among participants, which may have strengthened our study. It was also not feasible to include participants from all ethnic/demographic groups, and also the majority of participants were Australia-born who may have different views to migrant community members. The Arabic-speaking community in Australia is heterogeneous, as is our sample, with participants originating from nine countries (including first-generation and second-generation migrants) and identifying with one of three religions, or with no religion. Owing to lack of resources for interpretation and translation, this study was restricted to English-speaking participants. Some cultural nuances or concepts that may be more readily expressed in Arabic language may not have been captured, and the transferability to non-English-speaking populations is uncertain. While we were unable to send preliminary findings to participants for member checking due to strict confidentiality between the market research company and participants, researcher triangulation was used with researchers debriefing after each focus group, and multiple investigators were involved in coding the data and development of emerging themes. Also, author AA is Arabic speaking and was involved in the data collection and analysis to ensure that ethnic and cultural nuances were identified.
Few studies have assessed the effect of a community-based educational intervention with regard to improving willingness to donate one's organs.16 42–44 One study targeting the Muslim American community found that a brief educational intervention focusing on an explanation for organ donation as well as evidence for Islam's support or organ donation increased willingness to donate.16 Further, community-based media and educational programme in the Hispanic community significantly increased people's awareness of and knowledge about organ donation as well as their intent to donate.42 The intervention was delivered in English and Spanish through media, schools and churches and addressed culturally sensitive issues regarding donation in the Hispanic community and corrected common religious misconceptions. Participants in our study suggested that an intervention targeting the Arabic-speaking population should ideally come from within their own communities, in the Arabic language, through local Arabic radio stations and through institutions such as churches and Mosques where members of their community frequent. ‘Pulling at the heart strings’, as suggested by one participant, should be achievable using local recipients of transplants and Arabic-speaking medical professionals trained in Australia. However, the authors’ experience gained when talking to patients on transplant waiting lists, and particularly those of Islamic faith, is a general reluctance of patients and relatives to voice their situation and transplant need to those outside their immediate family unit.
To raise awareness and correct religious misconceptions about organ donation, other participants were of the view that a targeted grass roots campaign, involving members of the community, including religious and cultural leaders, is likely to be perceived as more credible, particularly for first-generation migrants, the elderly family decision makers, and those with limited educational background and English language skills. Provision of the targeted education is likely to be a role for a team of intensivists and transplant professionals that would ideally include an Arabic-speaking clinician. In the case of the Sydney Local Health District, transplant professionals could point to local data demonstrating the equity of access to deceased donor organs, a process that is driven by nationwide protocols and computer allocation.45 The marked disparity between the willingness of Arabic speakers to receive a transplant, and the absence of deceased organ donors from the Arabic-speaking community, would need to be discussed. Whether Christian or Islamic, the explanation for the disparity may not be religious in nature.
A significant cultural challenge and one that is likely to be difficult to change by targeted campaigns is the taboo surrounding any discussion of the subject of death in the setting of family and friends, particularly before a death has occurred. However, after death has been declared, trained donation practitioners have been found to increase consent rates.46 Of importance is the need for specialised training for practitioners to cover cultural and religious issues that may influence the family during donation, in particular to negate familial tension between generations and fear of negative societal appraisal. An understanding and appreciation of such issues is considered vital to ensure culturally sensitive approaches can be implemented when making a donation request.
Research by others has predominately considered ethnic minority groups as a generally homogenous population. In common in this study of migrant Arabic speakers and their descendants in Australia, were the economic, political or civil turmoil in their country of origin that prompted them to migrate. However, there were also notable differences in our study with some younger participants identifying themselves as more socially integrated into the dominant ‘Australian’ culture. Participants, who intended to donate their organs, regarded anticipated resistance from their family and culture and worried that such views could cause familial conflict. Future research could focus on identifying ways to best support those within ethnic minorities who wish to donate the organs after death, as well as identifying culturally appropriate ways to raise the topic of organ donation with family members. For the foreseeable future, the ultimate decision to donate organs after death in Australia for purposes of transplantation is likely to remain with the next-of-kin and be irrespective of the individual's positive wishes stated prior to death. Thus, it is important to include all family members in community and educational interventions.
In summary, members of the heterogeneous Arabic-speaking community in Australia considered organ donation to be a life-saving act, however were unaccustomed with the donation process. To better understand the attitudes towards organ donation and the reasons for the disparity between the preparedness to accept a transplant and negativity towards deceased organ donation, six themes were identified. These themes would likely benefit from research by sociologists and/or ethnographers. Our suggested approach to modify the negative attitudes associated with medical suspicion and religious ambiguity is targeted, grass roots media and language-compatible educational campaigns at the community level. Breaking down cultural taboo and the need for protecting family cohesiveness may be achievable with appropriately trained and culturally sensitive designated organ donor requestors. A task for the general community and government is to determine the means by which an individual can ‘own their decision’ about organ donation after their death.
Footnotes
Contributors: All authors contributed to the study concept and design. AFR, AA, RDMA, KH and AT collected and coded the data. AFR, AA, RDMA, KH, JCC and AT contributed to the analysis and interpretation of the data. All authors reviewed and revised the article critically for important intellectual content.
Funding: This study is funded by the Sydney Local Health District and the Transplant Australia ‘Mark Cocks Transplant Research Scholarship’. AFR is supported by an NHMRC scholarship (GNT1093101).
Competing interests: None declared.
Ethics approval: University of Sydney Ethics Committee (ID: 2013/937).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Rudge C, Matesanz R, Delmonico F et al. International practices of organ donation. Br J Anaesth 2012;108(Suppl 1):i48–55. 10.1093/bja/aer399 [DOI] [PubMed] [Google Scholar]
- 2.Klein A, Messersmith E, Ratner L et al. Organ donation and utilization in the United States, 1999–2008. Am J Transplant 2010;10(4 pt 2):973–86. 10.1111/j.1600-6143.2009.03008.x [DOI] [PubMed] [Google Scholar]
- 3.Wynn JJ, Alexander CE. Increasing organ donation and transplantation: the U.S. experience over the past decade. Transpl Int 2011;24:324–32. 10.1111/j.1432-2277.2010.01201.x [DOI] [PubMed] [Google Scholar]
- 4.International Registry in Organ Donation and Transplantation (IroDaT). IRoDaT Preliminary Numbers 2013. IRoDaT, 2014. [Google Scholar]
- 5.Morgan M, Hooper R, Mayblin M et al. Attitudes to kidney donation and registering as a donor among ethnic groups in the UK. J Public Health 2006;28:226–34. 10.1093/pubmed/fdl045 [DOI] [PubMed] [Google Scholar]
- 6.Goldberg DS, Halpern SD, Reese PP. Deceased organ donation consent rates among racial and ethnic minorities and older potential donors. Crit Care Med 2013;41:496 10.1097/CCM.0b013e318271198c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brown CV, Foulkrod KH, Dworaczyk S et al. Barriers to obtaining family consent for potential organ donors. J Trauma 2010;68:447–51. 10.1097/TA.0b013e3181caab8f [DOI] [PubMed] [Google Scholar]
- 8.Salim A, Berry C, Ley EJ et al. The impact of race on organ donation rates in Southern California. J Am Coll Surg 2010;211:596–600. 10.1016/j.jamcollsurg.2010.06.390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Siminoff LA, Gordon N, Hewlett J et al. Factors influencing families’ consent for donation of solid organs for transplantation. JAMA 2001;286:71–7. 10.1001/jama.286.1.71 [DOI] [PubMed] [Google Scholar]
- 10.Randhawa G. Achieving equality in organ donation and transplantation in the UK—challenges and solutions. Better Health Briefing. Achieving equality in organ donation and transplantation in the UK—challenges and solutions. Better Health Briefing, Paper 23: Race Equality Foundation & Department for Communities and Local Government 2011.
- 11.Summers D, Johnson R, Hudson A et al. Standardized deceased donor kidney donation rates in the UK reveal marked regional variation and highlight the potential for increasing kidney donation: a prospective cohort study. Br J Anaesth 2014;113:83–90. 10.1093/bja/aet473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morgan M, Kenten C, Deedat S et al. Attitudes to deceased organ donation and registration as a donor among minority ethnic groups in North America and the UK: a synthesis of quantitative and qualitative research. Ethn Health 2013;18:367–90. 10.1080/13557858.2012.752073 [DOI] [PubMed] [Google Scholar]
- 13.Australian Bureau of Statistics. Census of population and housing. Canberra, Australia: Australian Bureau of Statistics, 2011. [Google Scholar]
- 14.Australian and New Zealand Organ Donation Registery (ANZOD). ANZOD Registry Report 2012. In: Excell L, Marion V, Russ G, eds. Adelaide, South Australia: ANZOD, 2012, p 12. [Google Scholar]
- 15.Transplantation Services. 2014 Annual report kidney transplantation Sydney, Australia: Royal Prince Alfred Hospital, 2015. [Google Scholar]
- 16.Hafzalah M, Azzam R, Testa G et al. Improving the potential for organ donation in an inner city Muslim American community: the impact of a religious educational intervention. Clin Transplant 2014;28:192–7. 10.1111/ctr.12296 [DOI] [PubMed] [Google Scholar]
- 17.Padela AI, Rasheed S, Warren GJ et al. Factors associated with positive attitudes toward organ donation in Arab Americans. Clin Transplant 2011;25:800–8. 10.1111/j.1399-0012.2010.01382.x [DOI] [PubMed] [Google Scholar]
- 18.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 19.Irving MJ, Tong A, Jan S et al. Factors that influence the decision to be an organ donor: a systematic review of the qualitative literature. Nephrol Dial Transplant 2012;27:2526–33. 10.1093/ndt/gfr683 [DOI] [PubMed] [Google Scholar]
- 20.Strauss A, Corbin J. Basics of qualitative research. Techniques and procedures for developing grounded theory. California: Sage Publications, 1998. [Google Scholar]
- 21.IRoDaT. Donation Activity Database 2013. Secondary Donation Activity Database 2013, 2013. http://www.irodat.org/?p=database
- 22.Beitin BK, Allen KR. Resilience in Arab American couples after September 11, 2001: a systems perspective. J Marital Fam Ther 2005;31:251–67. 10.1111/j.1752-0606.2005.tb01567.x [DOI] [PubMed] [Google Scholar]
- 23.Birman D, Trickett EJ. Cultural transitions in first-generation immigrants acculturation of Soviet Jewish refugee adolescents and parents. J Cross Cult Psychol 2001;32:456–77. 10.1177/0022022101032004006 [DOI] [Google Scholar]
- 24.Szapocznik J, Kurtines W. Acculturation, biculturalism and adjustment among Cuban Americans. Acculturation: theory, models, and some new findings. 1980:139–59. [Google Scholar]
- 25.Szapocznik J, Kurtines WM. Family psychology and cultural diversity: opportunities for theory, research, and application. Am Psychol 1993;48:400 10.1037/0003-066X.48.4.400 [DOI] [Google Scholar]
- 26.Morse JM. The significance of saturation. Qual Health Res 1995;5:147–9. 10.1177/104973239500500201 [DOI] [Google Scholar]
- 27.Birman D. Measurement of the “acculturation gap” in immigrant families and implications for parent-child relationships. Bornstein MH, Cote LR (eds). Acculturation and parent-child relationships: Measurement and development. Mahwah, NJ, US: Lawrence Erlbaum Associates Publishers. 2006; pp 113–34.
- 28.Ho J, Birman D. Acculturation gaps in Vietnamese immigrant families: impact on family relationships. Int J Intercult Relat 2010;34:22–33. 10.1016/j.ijintrel.2009.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Costigan CL, Dokis DP. Relations between parent–child acculturation differences and adjustment within immigrant Chinese families. Child Dev 2006;77:1252–67. 10.1111/j.1467-8624.2006.00932.x [DOI] [PubMed] [Google Scholar]
- 30.Irving MJ, Tong A, Jan S et al. Community attitudes to deceased organ donation: a focus group study. Transplantation 2012;93:1064–9. 10.1097/TP.0b013e31824db997 [DOI] [PubMed] [Google Scholar]
- 31.Molzahn AE, Starzomski R, McDonald M et al. Chinese Canadian beliefs toward organ donation. Qual Health Res 2005;15:82–98. 10.1177/1049732304270653 [DOI] [PubMed] [Google Scholar]
- 32.McNamara P, Guadagnoli E, Evanisko MJ et al. Correlates of support for organ donation among three ethnic groups. Clin Transplant 1999;13:45–50. 10.1034/j.1399-0012.1999.t01-2-130107.x [DOI] [PubMed] [Google Scholar]
- 33.Morgan SE, Miller JK, Arasaratnam LA. Similarities and differences between African Americans’ and European Americans’ attitudes, knowledge, and willingness to communicate about organ donation. J Appl Soc Psychol 2003;33:693–715. 10.1111/j.1559-1816.2003.tb01920.x [DOI] [Google Scholar]
- 34.Edwards TM, Essman C, Thornton JD. Assessing racial and ethnic differences in medical student knowledge, attitudes and behaviors regarding organ donation. J Natl Med Assoc 2007;99:131–00. [PMC free article] [PubMed] [Google Scholar]
- 35.Siminoff LA, Burant CJ, Ibrahim SA. Racial disparities in preferences and perceptions regarding organ donation. J Gen Intern Med 2006;21:995–1000. 10.1111/j.1525-1497.2006.00516.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Keten HS, Keten D, Ucer H et al. Knowledge, attitudes, and behaviors of mosque imams regarding organ donation. Ann Transplant 2014;19:598–603. 10.12659/AOT.891370 [DOI] [PubMed] [Google Scholar]
- 37.Ghaly M. Religio-ethical discussions on organ donation among Muslims in Europe: an example of transnational Islamic bioethics. Med Health Care Philos 2012;15:207–20. 10.1007/s11019-011-9352-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kinnaert P. [Christian religions and organ transplantation]. Rev Med Brux 2007;29:187–91. [PubMed] [Google Scholar]
- 39.Organ and Tissue Authority. Statements of Support. Secondary Statements of Support 2014. http://www.donatelife.gov.au/statements-support.
- 40.Randhawa G, Brocklehurst A, Pateman R et al. Faith leaders united in their support for organ donation: findings from the UK organ donation taskforce study. Transpl Int 2010;23:140–6.. 10.1111/j.1432-2277.2009.00952.x [DOI] [PubMed] [Google Scholar]
- 41.Aslam M, Hameed W. UK Muslim graduates need more information about organ donation and transplant. Transpl Int 2008; 21:92–3. 10.1111/j.1432-2277.2007.00558.x [DOI] [PubMed] [Google Scholar]
- 42.Salim A, Ley EJ, Berry C et al. Increasing organ donation in Hispanic Americans: the role of media and other community outreach efforts. JAMA Surg 2014;149:71–6. 10.1001/jamasurg.2013.3967 [DOI] [PubMed] [Google Scholar]
- 43.Callender CO, Hall MB, Branch D. An assessment of the effectiveness of the Mottep model for increasing donation rates and preventing the need for transplantation—adult findings: program years 1998 and 1999. Semin Nephrol 2001; 21:419–28. 10.1053/snep.2001.23778 [DOI] [PubMed] [Google Scholar]
- 44.Andrews AM, Zhang N, Magee JC et al. Increasing donor designation through black churches: results of a randomized trial. Prog Transplant 2012;22:161–7. 10.7182/pit2012281 [DOI] [PubMed] [Google Scholar]
- 45.Transplantation Society of Australia and New Zealand. Organ transplantation from deceased donors: consensus statement on eligibility criteria and allocation protocols. Transplantation Society of Australia and New Zealand, 2015. [Google Scholar]
- 46.Jansen NE, van Leiden HA, Haase-Kromwijk BJ et al. Appointing ‘trained donation practitioners’ results in a higher family consent rate in the Netherlands: a multicenter study. Transpl Int 2011;24:1189–97. 10.1111/j.1432-2277.2011.01326.x [DOI] [PubMed] [Google Scholar]