Abstract
Primary lymphoid neoplasms of the urinary tract are exceedingly rare, with only 21 cases being reported and comprising less than 5% of all primary extranodal lymphomas. We report a case of a 45-year-old man who presented with right flank pain and weight loss, and who was found to have a stricture in the right lower ureter causing ureteral obstruction. Histopathology revealed lower ureteric non-Hodgkin lymphoma, which, on further evaluation, was found to be isolated ureteric lymphoma. The patient was doing well after six cycles of R-CHOP chemotherapy. This case is being reported as a rare cause of distal ureteric obstruction.
Background
Primary lymphoid neoplasms of the urinary tract are rare, comprising less than 5% of all primary extranodal lymphomas.1 Involvement of the ureter in lymphomas could be a result of ureteric wall involvement, direct extension or compression from retroperitoneal lymph nodes. Primary ureteric lymphomas are exceedingly rare, with only 21 cases reported in the literature so far.2 We report a case of a 45-year-old man who presented with right flank pain and weight loss, and who was found to have a stricture in the right lower ureter causing ureteral obstruction, diagnosed to be due to lower ureteric non-Hodgkin lymphoma (NHL).
Case presentation
A 45-year-old man presented with dull aching right flank pain of 2 months duration, associated with neither haematuria nor dysuria, nor with lower urinary tract symptoms. He had lost around 10 kg in the past 6 months and had loss of appetite, with low grade fever and malaise. He had no comorbidities, no prior surgeries and no tuberculosis. He was moderately built, poorly nourished and pale, with no generalised lymphadenopathy, no loin tenderness and no hepatosplenomegaly.
Investigations
The patient had anaemia (haemoglobin: 9 g/dL) and his serum creatinine was 1.7 mg/dL. Non-contrast CT of the abdomen and pelvis revealed right moderate right hydroureteronephrosis (HUN) to the lower ureter (figure 1). The left kidney, ureter and urinary bladder were normal. There was no retroperitoneal lymphadenopathy and no hepatosplenomegaly.
Figure 1.
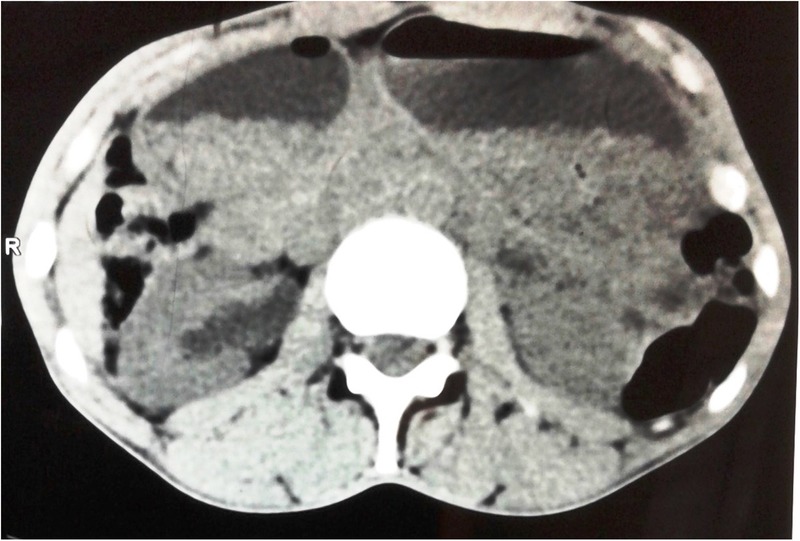
Non-contrast computed tomogram of the abdomen showing right hydroureteronephrosis.
Differential diagnosis
Tuberculosis ureter; ureteric stricture.
Treatment
The patient was planned for right double J stenting with consent for open exploration. Cystoscopy revealed a normal lower urinary tract. As the guidewire could not be passed beyond the distal ureter, a retrograde ureteropyelogram was performed. It revealed a lower ureteric stricture approximately 5 cm long (figure 2). On exploration through a right Gibson incision, the distal ureter was found to be indurated for 6 cm with enlarged periureteric lymph nodes. The proximal ureter was normal. These intraoperative findings led to a strong suspicion of tuberculosis, as it is endemic to India. Right distal ureterectomy and lymph node biopsy were carried out and ureteric reimplantation with psoas hitch was performed over a 5.5F DJ stent. A retroperitoneal drain was placed. Histopathology of the ureterectomy and lymph node specimens revealed diffuse NHL. The wall of the ureter showed diffuse infiltrate of large cells with vesicular nuclei and prominent nucleoli (figure 3). Immunohistochemistry was positive for CD 20 (figure 4), Bcl 6 and Mum1, and negative for ALK, Cyclin D1 and Cyclin D10, favouring a diagnosis of non-GCB (germinal centre B-cell-like) diffuse large B cell lymphoma (DLBCL). Ki-67 proliferation index was 90%. After postoperative recovery, bone marrow biopsy was performed to rule out disseminated disease. CT of the thorax was negative for lymphadenopathy. Bone marrow biopsy was negative, following which the patient was started on rituximab, cyclophosphamide, doxorubicin, vincristine and methyl prednisolone (R-CHOP) regimen; at writing, he has completed six cycles.
Figure 2.

Retrograde pyelogram of right ureter showing a filling defect in the lower ureter.
Figure 3.
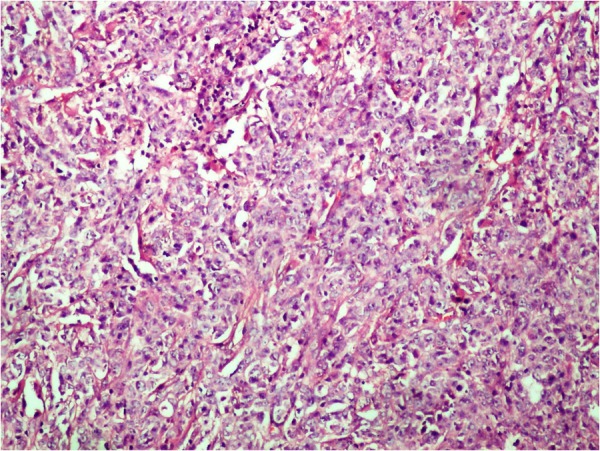
Photomicrograph. Histopathology (H&E, ×10) showing diffuse infiltrate of large cells with vesicular nuclei and prominent nucleoli.
Figure 4.

Photomicrograph. Immunohistochemistry with CD20.
Outcome and follow-up
The patient's B symptoms have improved and he is on follow-up. His serum creatinine is 1.4 mg/dL 2 months after stent removal.
Discussion
Among the various causes of distal ureteric obstruction, primary lymphomas are rarely thought of as a cause, especially in countries endemic for tuberculosis, such as ours. Primary or isolated lymphoma involving the ureter is exceedingly rare, with only 21 cases being reported in the literature so far. The median age at presentation is 56 years and the disease has a male preponderance. The most common presentation is flank pain. NHL is the commonest subtype, including DLBCL, follicular B-cell, small cell and mucosa associated lymphoid tissue varieties.3 NHL has a greater propensity to disseminate to extranodal sites than does HL. The gastrointestinal tract is the most common extranodal site. Lymphoma involving the genitourinary tract is very rare, constituting less than 5% of all extranodal lymphomas. Involvement of the ureter could be due to primary mural affliction or due to spread from retroperitoneal lymph nodes.4 As discussed, ureteral lymphomas are rarely considered as an aetiology for ureteric obstruction. Diagnosis is always performed by histopathological examination after partial ureterectomy or nephroureterectomy. In the previously reported series, 13 of the 21 cases underwent surgery: partial ureterectomy in six cases and nephroureterectomy in seven cases, and one patient underwent ureteroscopic mucosal biopsy.3 Our patient underwent a partial ureterectomy (distal) and this intraoperative decision of distal ureterectomy was made in view of a high index of suspicion for urinary tract tuberculosis in an endemic setting versus any malignant process. Imaging has a limited role in specific preoperative diagnosis of ureteral lymphoma. The role of ureteral mucosal biopsy has been mentioned by Hashimoto et al.5 However, other reports have denied the adequacy of mucosal biopsy, as vessels and lymphatics are longitudinally oriented in the adventitia, which determine longitudinal spread of the tumour. Ni et al3 reported a case of a patient where ureteroscopic biopsy revealed granuloma; subsequent nephroureterectomy, performed for a non-functioning kidney, revealed ureteral lymphoma. Hence in cases where strong suspicion of a malignant process exists, resection may be necessary to establish the final diagnosis. The determination of primary versus secondary involvement of extranodal sites by lymphoma is a pertinent issue. Krol et al6 proposed criteria stating that any lymphoma with initial presentation at an extranodal site should be considered extranodal, even if disseminated disease is discovered, in cases where the extranodal component is clinically dominant. Since the incidence of isolated ureteric lymphoma is rare, treatment guidelines are not established. The majority of these reported cases (table 1) underwent chemotherapy after diagnosis was established on histopathology.7–15 To assess extent of disease, patients should be subjected to FDG-PET scan and bone marrow biopsy, as these patients may have bone marrow involvement.16 Our patient only had isolated distal ureteral lymphoma with contiguous lymph node involvement as evidenced by histopathology. He is doing well after six cycles of R-CHOP chemotherapy.
Table 1.
| Sl No | Author | Age/sex | Lymphoma type | Presentation | Location | Treatment | Follow-up (in months) |
|---|---|---|---|---|---|---|---|
| 1 | Jaeger4 | 16/M | DLBCL | FP | MU | Chemo (CHOP) | NA |
| 2 | Ni3 | 38/M | Follicular | FP | MU | RNU+Chemo (R-CHOP) | 7 |
| 3 | Otsuki7 | 69/M | MALT | FP | UU | RNU+R | 78 |
| 4 | Asgari8 | 74/F | MALT | FP, H | UU+Pelvis | RNU | NA |
| 5 | Naranji9 | 78/F | Mantle cell | FP, UTI | PUJ | DP+R-CHOP | NA |
| 6 | Haitani10 | 59/M | Follicular | FP | NA | Chemo (RCOP) | NA |
| 7 | Ruth11 | 50/M | DLBCL | FP | MU | Chemo | NA |
| 8 | Kubota12 | 68/M | Follicular | OU | UU | RNU+Chemo | NA |
| 9 | Kawashima13 | 71/M | Follicular | H | MU | PUT+Chemo | NA |
| 10 | Fujisawa14 | 58/M | DLBCL | FP | MU | RNU+Chemo | 15 |
| 11 | Tozzini15 | 54/M | HL | FP, UTI | DU | RNU+ABVD | NA |
| 12 | Our patient | 45/m | DLBCL | FP | DU | DUT+R-CHOP | 6 |
*Ni et al reported 20 cases of ureteric lymphoma but, due to lack of references, only available cases have been tabulated.
A, adriamycin; B, bleomycin; C, cyclophosphamide; Chemo, chemotherapy; D, dacarbazine; DLBCL, diffuse large B cell lymphoma; DU, distal ureter; DUT, distal ureterectomy; FP, flank pain; H, adriamycin; H, haematuria; HL, hodgkins Lymphoma; MALT, mucosa associated lymphoid tissue; MU, mid-ureter; O, vincristine; OU, obstructive uropathy; P, prednisolone; PUT, partial ureterectomy; R, rituximab; RNU, radical nephroureterectomy; UTI, urinary tract infection; UU, upper ureter; V, vinblastine.
Learning points.
Isolated non-Hodgkin lymphoma of the ureter is a rare cause of hydroureteronephrosis.
In patients with flank pain, this condition is to be suspected, especially in the presence of fever, loss of appetite and significant loss of weight.
Definitive diagnosis is possible only on histopathology and chemotherapy with R-CHOP appears to be effective based on limited available literature.
Footnotes
Contributors: JS, AM and VSK performed the literature search, and conceived of and drafted the manuscript; they also gave their approval of the final manuscript. UA provided the pathological aspects, was involved in the drafting of the manuscript and gave approval of the final manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Schniederjan SD, Osunkoya AO. Lymphoid neoplasms of the urinary tract and male genital organs: a clinicopathological study of 40 cases. Mod Pathol 2009;22:1057–65. 10.1038/modpathol.2009.65 [DOI] [PubMed] [Google Scholar]
- 2.Foote C, Henderson S, Reddy S et al. Primary ureteral lymphoma presenting with acute flank pain. Curr Urol 2014;7:210–13. 10.1159/000365679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ni BW, Zhong L, Wang T et al. Malignant lymphoma of the ureter: a case report and literature review. Exp Ther Med 2014;7:1521–4. 10.3892/etm.2014.1658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jaeger CD, McAlvany KL, Zingula SN et al. Diffuse large B-cell lymphoma in an adolescent male presenting as ureteral stricture. Case Rep Radiol 2014;2014:239345 10.1155/2014/239345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hashimoto H, Tsugawa M, Nasu Y et al. Primary non-Hodgkin lymphoma of the ureter. BJU Int 1999;83:148–9. 10.1046/j.1464-410x.1999.00856.x [DOI] [PubMed] [Google Scholar]
- 6.Krol AD, le Cessie S, Snijder S et al. Primary extranodal non-Hodgkin's lymphoma (NHL): the impact of alternative definitions tested in the Comprehensive Cancer Centre West population-based NHL registry. Ann Oncol 2003;14:131–9. 10.1093/annonc/mdg004 [DOI] [PubMed] [Google Scholar]
- 7.Otsuki H, Ito K, Sato K et al. Malignant lymphoma of mucosa-associated lymphoid tissue involving the renal pelvis and the entire ureter: a case report. Oncol Lett 2013;5:1625–8. 10.3892/ol.2013.1221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Asgari SA, Aval HB, Asgari SA et al. A unique case of kidney's collecting system MALT lymphoma. Can Urol Assoc J 2014;8:E172–5. 10.5489/cuaj.1452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Naranji I, Zakri RH, Liston T. Mantle cell lymphoma presenting as a pelvi-ureteric junction obstruction: a case report. J Med Case Rep 2013;7:105 10.1186/1752-1947-7-105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haitani T, Shimizu Y, Inoue T et al. A case of ureteral malignant lymphoma with concentric thickening of the ureteral wall. Hinyokika Kiyo 2012;58:209–13. [PubMed] [Google Scholar]
- 11.Ruth K, El-Amm J, Sotelo T et al. Primary diffuse large B-cell lymphoma of the ureter in a patient with HIV: a case report and review of literature. Clin Lymphoma Myeloma Leuk 2013;13:324–6. 10.1016/j.clml.2012.12.009 [DOI] [PubMed] [Google Scholar]
- 12.Kubota Y, Kawai A, Tsuchiya T et al. Bilateral primary malignant lymphoma of the ureter. Int J Clin Oncol 2007;12:482–4. 10.1007/s10147-007-0685-7 [DOI] [PubMed] [Google Scholar]
- 13.Kawashima A, Shiotsuka Y, Nin M et al. Malignant lymphoma of the ureter: a case report. Hinyokika Kiyo. 2005;51:269–72. [PubMed] [Google Scholar]
- 14.Fujisawa H, Takagane H, Shimosegawa K et al. Primary malignant lymphoma of the ureter: a case report. Hinyokika Kiyo 2004;50:721–4. [PubMed] [Google Scholar]
- 15.Tozzini A, Bulleri A, Orsitto E et al. Hodgkin's lymphoma: an isolated case of involvement of the ureter. Eur Radiol 1999;9:344–6. 10.1007/s003300050677 [DOI] [PubMed] [Google Scholar]
- 16.Shi YF, Li XH, Song YQ et al. Involvement of bone marrow in lymphoma: pathological investigation in a single-center from northern China. Int J Clin Exp Pathol 2015;8:7102–11. [PMC free article] [PubMed] [Google Scholar]


