Description
A 22-year-old woman (body mass index of 40 kg/m2) repeatedly presented to her general practitioner (GP), with a diffusely tender and distended abdomen. She was told the reason for her symptoms was obesity. Eventually her GP referred her to A&E department when she reported left-sided flank pain, to rule out renal calculi.
Ultrasonography revealed a large cyst extending from the symphysis to the xiphisternum, measuring approximately 26 cm×26 cm×21 cm (figure 1). Owing to previous pulmonary emboli in the patient's medical history, she was at high risk for malignancy,1 so a CT scan was performed, which confirmed a 27 cm (craniocaudal)×27 cm (transverse)×17 cm (anterposterior) low-density (Hounsfield unit 9) cystic lesion (figures 2–4). The scan showed a single septa along the right lateral aspect of the cyst. There was a small area of soft tissue along the left lateral wall with a slightly thicker wall. There was no internal calcification or fat. The left adnexal origin of the cyst represented a large left-sided abdominopelvic ovarian cyst. A whirled appearance of the broad ligament/fallopian on the left suggested possible torsion. There was no free fluid, pelvic or para-aortic adenopathy. There was no evidence of peritoneal/omental or metastatic disease. All tumour markers were normal.
Figure 1.
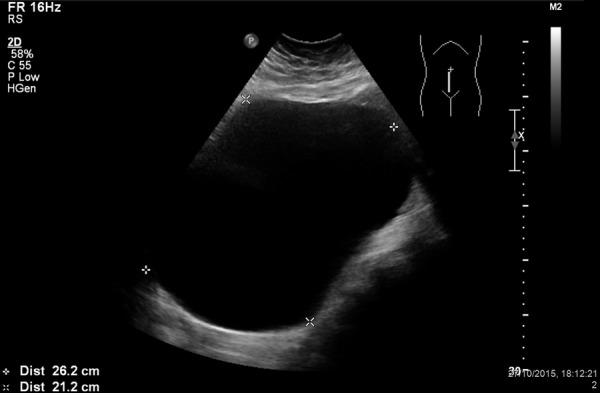
Ultrasound scan of the cyst measuring approximately 26 cm×26 cm×21 cm.
Figure 2.
Coronal CT scan showing 27 cm (craniocaudal)×27 cm (transverse) low-density cystic lesion.
Figure 3.
Sagittal CT scan showing 27 cm (craniocaudal)×17 cm (anterposterior) low-density cystic lesion.
Figure 4.
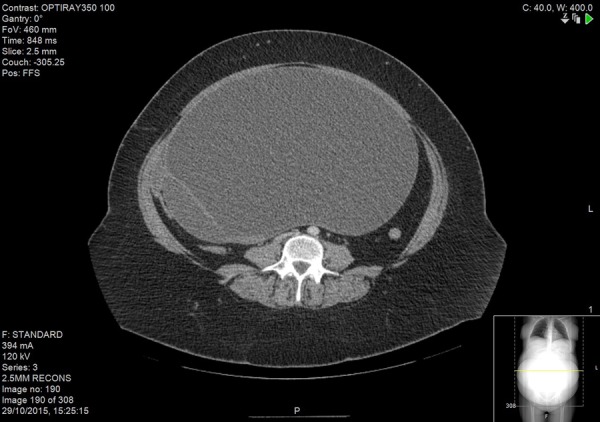
Transverse CT scan showing 27 cm (transverse)×17 cm (anterposterior) low-density cystic lesion.
The patient eventually became septic. She was started on empirical antibiotics and expedited to theatre for laparotomy, cyst removal and left oophorectomy. The cyst was multilocular and filled with 6 L of blood-stained fluid. There was no evidence of malignancy. The patient completed the course of intravenous and oral antibiotics.
Learning points.
Patients with history of pulmonary embolism or deep venous thrombosis are at higher risk of malignancy.1
Repeated general practitioner visits with recurring symptoms should warrant specialist opinion to rule out occult diagnoses. A simple ultrasound scan is a very useful tool when investigating acute abdominal pain and is a safe imaging modality in young female patients.2
The management of obesity is complex because it has an underlying genetic basis that can be exacerbated by lifestyle and eating habits.3
Footnotes
Contributors: JTP was responsible for the patient's care. PR and AKMP looked after the patient during her stay as an inpatient. All the authors contributed to the writing of the case report.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Sørensen HT, Mellemkjaer L, Steffensen FH et al. . The risk of a diagnosis of cancer after primary deep venous thrombosis or pulmonary embolism. N Engl J Med 1998;338:1169–73. 10.1056/NEJM199804233381701 [DOI] [PubMed] [Google Scholar]
- 2.Mazzei MA, Guerrini S, Squitieri NC et al. . The role of US examination in the management of acute abdomen. Crit Ultrasound J 2013;5(Suppl 1):S6. 10.1186/2036-7902-5-S1-S6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kassir R, Blanc N, Tiffet O et al. . Obesity and the stool concept. Obes Surg 2015;25:129–30. 10.1007/s11695-014-1405-9 [DOI] [PubMed] [Google Scholar]




