Abstract
Introduction
Sleep deprivation has a potentially deleterious effect on postoperative recovery. The aim of our prospective study was to identify the factors contributing to postoperative sleep deprivation and disturbance in order to recommend improvements in postoperative care.
Methods
102 consecutive patients attending for elective general and orthopaedic surgery were interviewed preoperatively (baseline) and postoperatively on their duration of sleep, number of wakenings during the night, factors contributing to sleep loss and the use of analgesia and night sedation.
Results
Patients woke up a median of 5 times in the first postoperative night compared to a median of 3 times preoperatively (p = 0.01). Pain was the predominant factor preventing sleep, affecting 39% of patients preoperatively and 48% of patients on the first postoperative day. Other factors included noise from other patients and nursing staff, and using the toilet. Analgesia was taken by more than 90% of patients in the first two days, this number gradually reducing over the postoperative period. On the other hand, in the first two postoperative days, only about 5% of patients had night sedation.
Discussion and conclusions
Apart from highlighting the need for effective pain management postoperatively, we believe that our study supports the drive towards single bed bays, where steps can be taken to minimize the impact of environmental factors on sleep.
Keywords: Sleep disturbance, Sleep deprivation, Surgery, Postoperative analgesia, Postoperative sedation
Highlights
-
•
This study is a prospective questionnaire survey of 102 surgical patients who procedures over a set time period.
-
•
The aim of the study was to determine factors contributing to sleep deprivation postoperatively on a surgical ward.
-
•
Unexpectedly, patients were not sleep deprived postoperatively but slept more during the daytime.
-
•
Pain and noise were the main factors contributing to sleep deprivation.
-
•
The authors then conclude that their study supports a drive towards single bed bays.
1. Introduction
The sleep wake cycle occurs over a period of approximately 24 h. Normal sleep forms part of the circadian rhythm of the body which is accompanied by many bodily changes, such as variations in the levels of glucagon, cortisol and catecholamines which inhibit protein synthesis and are at their highest during the day [1]. During sleep the levels of growth hormone increases leading to the physiologically plausible theory that wakefulness causes tissue catabolism and sleep induces anabolism [2].
Sleep deprivation is defined as the reduction in the total sleep time relative to one's usual baseline during a 24-h period. It can have potentially dangerous multi-systemic effects in the critically ill, including surgical patients [3], [4], [5], [6], [7], [8]. The need for adequate sleep must therefore be taken into account in both the preoperative and the postoperative care of surgical patients. The stress of poor sleep when coupled with surgical stress can lead to increased catabolic activity and tissue breakdown as well as reduced anabolic activity, which will affect post operative recovery [1], [5], [7] Indeed animal models have shown that sleep deprivation leads to the depletion of glycogen stores and increases in oxidative stress and free radical production as well as the production of pro-inflammatory cytokines all implicated in poor post operative recovery [9], [10].
Hospital wards have been shown to be particularly difficult places to get a good night's sleep [3], [4], [5], [6], [7], [8], [11]. By their very nature surgical wards are very noisy often with noise levels in excess of 70 dB [3]. Surgical wards are also bright with a lot of night time activity and patient interventions occurring. Indeed it is not uncommon for painful and distressing procedures such as urinary catheterisation and cannulation to occur between 2am and 5am [3], [4], [5], [6], [7], [8], [11]. Nursing interventions while often necessary have also been reported as causing disturbance [12].
In general, studies into sleep in an inpatient setting tended to focus on the intensive care units [13]. Few studies have been done on sleep in the postoperative setting in a surgical ward [8], with one study comparing sleep disturbances between laparoscopic and open surgery [7].
Using a large cohort of patients, the aim of this study was to identify those factors that were contributing to sleep deprivation and disturbance in the postoperative patient on a surgical ward. By identifying and critically analyzing these factors, recommendations to improve the quality of sleep in the postoperative patient may be made in the future but these interventions are not the main focus of this study.
2. Patients and methods
Patients admitted to a Teaching General Hospital over a 3 month period for routine elective major orthopaedic and general surgery were identified preoperatively. A questionnaire was administered to the patients on a daily basis by the authors, starting from the day of their admission and continuing until discharge home for up to the sixth postoperative day. Questions were asked on the number of hours of sleep, the number of wakenings during the night, factors contributing to sleep loss and disturbance, and the use of analgesia and night sedation. The duration of patients' sleep was divided into two periods: nocturnal sleep (hours of sleep between 9pm and 7am) and daytime/afternoon sleep (hours of sleep between 7am and 9pm). The patients' baseline sleep pattern was taken to be the sleep pattern for the day and night prior to surgery spent at home. Patients were then asked to declare if they had any underlying sleep disorders or a history of chronic sleep disturbance.
Patients were nursed in six-bedded bays postoperatively in general surgical or orthopaedic wards. Those who required High Dependency or Intensive Therapy Unit care postoperatively were excluded.
Clinical data were entered into a Microsoft Excel database and analysed using a Wilcoxon signed rank test (Microsoft, Redmond, Washington, USA). A p value less than 0.05 was considered statistically significant.
The study was approved and registered as Quality Improvement Project E453 with the NHS Forth Valley Quality Improvement board.
3. Results
A total of one hundred and two patients (58 women, median age (range) 69 (21–87) years) participated in the study. A power calculation produced an ideal sample size of 84 so this study is well powered. Sixty four had orthopaedic operations (28 had a Total Hip Replacement and 36 had a Total Knee Replacement) whilst the other 38 patients had various abdominal operations (5 right hemicolectomy, 3 sigmoid colectomy, 5 anterior resection, 4 closure of ileostomy, 3 open repair of abdominal wall hernia, 2 cholecystectomy, 2 fundoplication, 6 rectopexy and 8 other abdominal operations). The total length of stay was 7 days (one pre op and six post op), 102 patients were present on day 1 post op, 88 of day 2, 68 on day 3, 47 on day 4, 34 on day 5 and 23 on day 6 post operatively.
No patients reported a history of sleep disorders or of chronic sleep disturbances other than reduced sleep due to pain. There was no significant difference in the mean number of hours of sleep before and after surgery (Table 1). In the postoperative period, however, the patients reported more sleep during the daytime and afternoon.
Table 1.
Mean hours of sleep both before and after surgery.
| Day | Mean hours (range) of sleep in a 24 h period | Mean hours (range) of daytime/afternoon sleep |
|---|---|---|
| 1 (Pre-Op) | 7.43 (2.0–10.5) | 0.25 (0.0–2.0) |
| 2 | 7.16 (1.0–14.0) | 0.75 (0.0–5.0) |
| 3 | 7.8 (3.0–11.0) | 0.67 (0.0–3.0) |
| 4 | 6.71 (3.0–11.0) | 0.75 (0.0–4.0) |
| 5 | 6.28 (3.5–10.0) | 0.50 (0.0–3.0) |
| 6 | 6.97 (1.25–13.0) | 0.50 (0.0–2.5) |
| 7 | 6.05 (1.0–9.0) | 0.50 (0.0–1.5) |
Night-time sleep at hospital was more disturbed postoperatively when compared to the preoperative night. Patients reported waking up a median of 5 times in the first postoperative night, compared to a median of 3 times preoperatively (p = 0.01).
A number of factors disturbing nocturnal sleep were cited by patients (Table 2). Pain was identified as the predominant factor, with 48.0% and 47.7% of patients giving this as the main reason for their interrupted sleep (this was quantified using a standard numerical 1–10 score) in the first and second post operative days respectively. Environmental factors were identified as significant factors disturbing patients' sleep over the course of the study. These factors included noise and disturbances from other patients, and nursing staff.
Table 2.
Numbers of patients and the reasons for disturbed nocturnal sleep across the seven days of the study. (N/A, not applicable).
| Cause of disturbed nocturnal sleep | Pre-operative (N = 102) | PostOp day 1 (N = 102) | PostOp day 2 (N = 88) | PostOp day 3 (N = 68) | PostOp day 4 (N = 47) | PostOp day 5 (N = 34) | PostOp day 6 (N = 23) |
|---|---|---|---|---|---|---|---|
| Pain | 33 | 49 | 42 | 29 | 23 | 17 | 9 |
| Nausea | 10 | 10 | 13 | 11 | 9 | 5 | 3 |
| Anxiety | 13 | 11 | 5 | 9 | 7 | 4 | 4 |
| Fever | 2 | 5 | 2 | 3 | 0 | 0 | 2 |
| Dressing change | N/A | 4 | 7 | 2 | 2 | 3 | 1 |
| Drips | N/A | 8 | 6 | 1 | 2 | 1 | 1 |
| Catheter | N/A | 5 | 1 | 0 | 0 | 0 | 0 |
| Drains | N/A | 3 | 2 | 2 | 1 | 0 | 2 |
| Noise | N/A | 19 | 16 | 12 | 12 | 7 | 8 |
| Lights on the ward | N/A | 5 | 5 | 2 | 3 | 5 | 1 |
| Disturbances from Nursing Staff | N/A | 29 | 11 | 9 | 5 | 6 | 3 |
| Disturbances from Medical Staff | N/A | 6 | 4 | 4 | 0 | 2 | 2 |
| Blood Tests | N/A | 1 | 7 | 1 | 1 | 0 | 0 |
| Other Tests eg ECG Xray | N/A | 3 | 3 | 0 | 0 | 1 | 0 |
| Disturbances from other patients | N/A | 16 | 21 | 13 | 11 | 4 | 6 |
| Room Temperature | N/A | 7 | 6 | 3 | 3 | 4 | 1 |
| Needing to use toilet facilities | 44 | 39 | 32 | 24 | 10 | 14 | 9 |
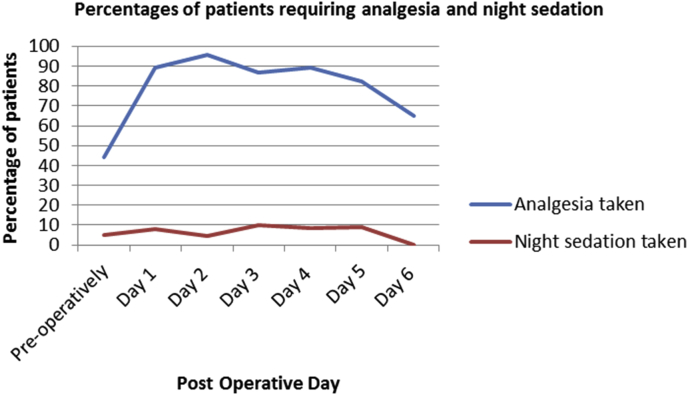
Analgesia was taken by more than 90% of patients in the first two postoperative days, this number decreasing over time. A much lower percentage of patients used night sedation over the course of this study (Fig. 1).
Fig. 1.
Percentage of patients requiring analgesia and night sedation on the pre-operative and six concurrent post operative days.
4. Discussion
The aim of this prospective study was to identify those factors that disturb nocturnal sleep in postoperative patients in general surgical and orthopaedic wards. These patients underwent major abdominal and orthopaedic surgery and were nursed in general orthopaedic or surgical wards. It is hoped that identifying these factors in a surgical ward in particular as opposed to ITU would allow for intervention methods to be developed to help aid patient sleep in the ward setting to be formulated with future studies.
Although there was no significant difference in the total number of hours slept in a 24 h period before and after surgery, we observed that postoperatively the patients were sleeping more in the daytime and afternoon. This disturbance in the circadian sleep rhythm has also been observed by Gogenur et al. in their study on patients undergoing cholecystectomy [7].
Preoperatively, with the patient at home, pain was the main factor responsible for sleep disturbance at night (Table 2). Often patients were not taking adequate analgesia at home which exacerbated this problem. The need to use toilet facilities was also a main contributing factor. Postoperatively however, this pattern changed. Pain was the predominant factor yet again, although environmental factors became more apparent. These factors include disturbance from nursing staff and noise; unsurprising given that these patients were nursed within bays typically accommodating between 4 and 6 patients. Additional factors such as need to use the toilet decreased post-operatively, possibly due to postoperative sedation or the use of urinary catheters.
The presence of pain as an important factor in both the pre and post operative periods is an interesting finding. It is to be expected particularly in orthopaedic patients who are having elective joint replacement for severe arthritis with associated resting pain. However this should not be used as a means to discount the importance of post operative pain control and its impact of patients sleeping patterns [11]. While there is a change in the type of painful stimulus, the initial cause of the joint pain has been removed and our ability to manage post operative pain is essential to aid patients' recovery.
Pain was controlled with oral and IV medication with all patients receiving a baseline of paracetamol and tramadol or another weak opioid. Oxycontin, Oxynorm and MST were used if pain became difficult to control however no patient controlled analgesia (PCA) systems or epidurals were used. Patients received appropriate pain relief in accordance with the standards of the WHO pain ladder and when needed strong opioids were used when required, however there were some time delays in the administration of pain relief noted.
Recent studies have shown that post operative pain perception can be affected by sleep disturbance producing a hyperalgesic state [14], [15]. However from our observation particularly in the pre-operative period where pain was the predominant cause of sleep disturbance it is pain which leads to sleep disturbance and that while a hyperalgesic state may be exacerbated by poor sleep it is the initial pain that starts this process and must be addressed.
Ward structure is of high importance in this study especially with the move towards more single occupancy beds in modern hospitals. We postulate that this move to more single occupancy rooms could reduce noise and as a result improve patients' sleep and this is a factor, which we will be looking directly at in follow up research. However in a recent study in the Netherlands single occupancy rooms have been shown to improve sleep quality and duration [16].
Other studies confirm that environmental factors have an important and compounding effect on sleep deprivation, in conjunction with pain [2], [11]. A study of sleep deprivation in post operative orthopaedic patients highlighted that 45% and 23% of patients cited pain and noise respectively as accounting for loss of sleep [17]. Noise levels can reach as high as 85 dB with alarm noises and conversations between medical staff in particular being highlighted by patients as being disturbing [13]. The negative impact of noise was also noted from a UK based study which noted amplitudes as high as 70 dB within wards [3]. Nausea was an identified cause of sleep loss, but did not contribute to the extent that we expected, particularly in general surgical patients.
Surgical patients are commonly troubled by post operative pain which can markedly and adversely affect their ability to get quality sleep [18]. When asked directly many surgical patients admitted to perceiving their pain to be worse at night [19]. However this is precisely the time when, due to reduced staffing numbers or other structural arrangements on the ward that the fewest doses of analgesics are prescribed, or that analgesia is not administered on time. The majority of patients took analgesia, but nonetheless pain was a main factor disturbing sleep. The use of effective analgesia has previously been demonstrated to be the single most reliable factor for promoting sleep [6], [11]. In addition, our study has shown that night sedation is under prescribed. The judicious use of night sedation in selected patients may improve the quality of nocturnal sleep. These findings warrant further investigation into patients' pain control and night sedation in hospital.
The re-establishment of physiological, circadian sleep rhythm by way of sedatives has been proven as effective at least with the use of benzodiazepines post operatively [7], [8]. Furthermore, patient stress levels would only be increased by sleep deprivation, leading to delayed wound healing that in turn would feedback to cause increased stress [1], [20], [21]. This originates from persistently elevated cortisol levels throughout the day that do not conform to normal physiological intervals [20].
There are several strategies to promote sleep in hospital including the reduction of environmental noise and the promotion of daytime activities as well as the use of sedation which can often be effective but which must be used with caution. Sleep hygiene refers to measures or interventions used to promote sleep and a person-centered approach is necessary to achieve this. Medications are used extensively in hospital settings to aid in sleep, with benzodiazepines and other sedating agents often being used. Unfortunately the potential addictive nature and risk of tolerance of these drugs makes many practitioners wary of using them excessively which can result in under sedation and increased physiological stress [19], [22].
We feel that one of the most topical ways of improving quality of postoperative sleep is to be a move away from multi-bedded bays and dormitories in favour of single bed rooms. This could lead to reduced environmental disturbance and supports the drive for this form of nursing and hospital structure that is currently occurring in the UK. It should be noted that such a change confers additional benefits to patients' wellbeing and safety in the form of better infection control, and more privacy for families [16].
There are some deficiencies in the study, which we would like to highlight. The potential for individuals to tolerate lack of sleep particularly over a short time period varies widely and is a potential confounding factor. However, the duration of this study which is a maximum of 7 days means that over the course of this elongated time period that the physiological potential of some individuals to tolerate reduced sleep can normalize and we believe this reduces this potential confounding factor.
Another potentially important confounding factor with the use of sleep questionnaires is the potential for recall bias. As patients are not objectively monitored during the sleeping process, we are relying on the accuracy of what they remember. While minor disturbances may not be recalled these can have an important impact on quality of sleep. Some studies have used sleep diaries or sterile sleep laboratories in order to ascertain patients' baseline sleep patterns. We believe that the use of sleep labs would not be possible in surgical patients. However, sleep diaries supported by direct observation of patients within the ward setting could be used in any future studies. Another potential way to introduce a more objective element to this study would be to fit patients with wrist actigraphy or another form of portable monitoring device.
The patient cohort was heterogenous, with most orthopaedic patients having arthroplasties and the general surgical patients having both open and also laparoscopic operations. We acknowledge that the type of surgery is related to postoperative sleep, mainly due to differences in postoperative pain [7], [23]. The aim of the study was not, however, to compare patient groups, but to analyse sleep disturbance across the surgical floor. Sub-group analyses may identify patterns in sleep disturbance specific to particular operations. Finally, it would be interesting to follow these patients up with a sleep based questionnaire to ascertain their sleep patterns 1–2 months after surgery which could provide an interesting further study moving forward.
5. Conclusion
We conclude that post-operative pain is the most significant and detrimental factor impacting upon sleep in surgical patients nursed in general surgical and orthopaedic wards. It is therefore essential to optimize analgesia to reduce this effect. Other factors contributing to sleep deprivation include noise from other patients and from nursing staff, factors that have their stem in multi-patient bays.
We believe that our study, apart from highlighting the need for effective pain management add further support the drive towards single-bed bays. This would have to be confirmed with an additional study in the setting of single occupancy beds compared to multiple bays however we believe such a change confers additional benefits to patients' wellbeing and safety in the form of better infection control and more privacy for families [16].
Ethical approval
Forth Valley Ethics Committee.
Funding
None.
Author contribution
Ross Dolan designed the project and completed the data collection with the help of Jae Huh, Neil Tiwari and Tom Sproat. Mr John Brennan was the supervising consultant.
Conflicts of interest
None.
Guarantor
Mr Ross Dolan.
Declarations
This paper was presented at the ASIT conference in Cardiff in March 2012 and published in abstract form in the International Journal of Surgery 10 (2012) S46, abstract number 0426.
References
- 1.Adam K., Oswald I. Sleep helps healing. Br. Med. J. Clin. Res. Ed. 1984;289(6456):1400–1401. doi: 10.1136/bmj.289.6456.1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wood A.M. A review of literature relating to sleep in hospital with emphasis on the sleep of the ICU patient. Intensive Crit. Care Nurs. 1993;9(2):129–136. doi: 10.1016/0964-3397(93)90054-2. [DOI] [PubMed] [Google Scholar]
- 3.Christensen M. Noise levels in a general surgical ward: a descriptive study. J. Clin. Nurs. 2005;14(2):156–164. doi: 10.1111/j.1365-2702.2004.01040.x. [DOI] [PubMed] [Google Scholar]
- 4.Tembo A.C., Parker V. Factors that impact on sleep in intensive care patients. Intensive Crit. Care Nurs. 2009;25(6):314–322. doi: 10.1016/j.iccn.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 5.Knutson K.L., Spiegel K., Penev P., Van C.E. The metabolic consequences of sleep deprivation. Sleep. Med. Rev. 2007;11(3):163–178. doi: 10.1016/j.smrv.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lane T., East L.A. Sleep disruption experienced by surgical patients in an acute hospital. Br. J. Nurs. 2008;17(12):766–771. doi: 10.12968/bjon.2008.17.12.30306. [DOI] [PubMed] [Google Scholar]
- 7.Gogenur I., Rosenberg-Adamsen S., Kiil C., Kjaersgaard M., Kehlet H., Rosenberg J. Laparoscopic cholecystectomy causes less sleep disturbance than open abdominal surgery. Surg. Endosc. 2001;15(12):1452–1455. doi: 10.1007/s004640090086. [DOI] [PubMed] [Google Scholar]
- 8.Rosenberg-Adamsen S., Kehlet H., Dodds C., Rosenberg J. Postoperative sleep disturbances: mechanisms and clinical implications. Br. J. Anaesth. 1996;76(4):552–559. doi: 10.1093/bja/76.4.552. [DOI] [PubMed] [Google Scholar]
- 9.McEwen B.S., Karatsoreos I.N. Sleep deprivation and circadian disruption: stress, allostasis, and allostatic load. Sleep. Med. Clin. 2015;10(1):1–10. doi: 10.1016/j.jsmc.2014.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McEwen B.S. Sleep deprivation as a neurobiologic and physiologic stressor: allostasis and allostatic load. Metabolism. 2006;55(10 Suppl 2):S20–S23. doi: 10.1016/j.metabol.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 11.Closs S.J. Patients' night-time pain, analgesic provision and sleep after surgery. Int. J. Nurs. Stud. 1992;29(4):381–392. doi: 10.1016/0020-7489(92)90016-a. [DOI] [PubMed] [Google Scholar]
- 12.Le A., Friese R.S., Hsu C.H., Wynne J.L., Rhee P., O'Keeffe T. Sleep disruptions and nocturnal nursing interactions in the intensive care unit. J. Surg. Res. 2012;177(2):310–314. doi: 10.1016/j.jss.2012.05.038. [DOI] [PubMed] [Google Scholar]
- 13.Xie H., Kang J., Mills G.H. Clinical review: the impact of noise on patients' sleep and the effectiveness of noise reduction strategies in intensive care units. Crit. Care. 2009;13(2):208. doi: 10.1186/cc7154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chouchou F., Khoury S., Chauny J.M., Denis R., Lavigne G.J. Postoperative sleep disruptions: a potential catalyst of acute pain? Sleep. Med. Rev. 2014;18(3):273–282. doi: 10.1016/j.smrv.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 15.Schuh-Hofer S., Wodarski R., Pfau D.B., Caspani O., Magerl W., Kennedy J.D. One night of total sleep deprivation promotes a state of generalized hyperalgesia: a surrogate pain model to study the relationship of insomnia and pain. Pain. 2013;154(9):1613–1621. doi: 10.1016/j.pain.2013.04.046. [DOI] [PubMed] [Google Scholar]
- 16.van dG I., de RS, Goossensen A. Do patients in hospitals benefit from single rooms? A literature review. Health Policy. 2007;84(2–3):153–161. doi: 10.1016/j.healthpol.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 17.Celik S., Oztekin D., Akyolcu N., Issever H. Sleep disturbance: the patient care activities applied at the night shift in the intensive care unit. J. Clin. Nurs. 2005;14(1):102–106. doi: 10.1111/j.1365-2702.2004.01010.x. [DOI] [PubMed] [Google Scholar]
- 18.Meltzer L.J., Mindell J.A., Owens J.A., Byars K.C. Use of sleep medications in hospitalized pediatric patients. Pediatrics. 2007;119(6):1047–1055. doi: 10.1542/peds.2006-2773. [DOI] [PubMed] [Google Scholar]
- 19.Brown G., Scott W. An assessment of a sedative algorithm for sleep in an intensive care unit. Off. J. Can. Assoc. Crit. Care Nurs. 1998;9(4):20–24. [PubMed] [Google Scholar]
- 20.Vileikyte L. Stress and wound healing. Clin. Dermatol. 2007;25(1):49–55. doi: 10.1016/j.clindermatol.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 21.Gay P.C. Sleep and sleep-disordered breathing in the hospitalized patient. Respir. Care. 2010;55(9):1240–1254. [PubMed] [Google Scholar]
- 22.Treggiari-Venzi M., Borgeat A., Fuchs-Buder T., Gachoud J.P., Suter P.M. Overnight sedation with midazolam or propofol in the ICU: effects on sleep quality, anxiety and depression. Intensive Care Med. 1996;22(11):1186–1190. doi: 10.1007/BF01709334. [DOI] [PubMed] [Google Scholar]
- 23.Bisgaard T., Klarskov B., Kehlet H., Rosenberg J. Recovery after uncomplicated laparoscopic cholecystectomy. Surgery. 2002;132(5):817–825. doi: 10.1067/msy.2002.127682. [DOI] [PubMed] [Google Scholar]