Abstract
Background
Technical faults leading to coracoid fractures during screw insertion and coracoid graft osteolysis are concerns with standard screw fixation techniques in Latarjet procedure. The purpose of this study is to share our experience using Arthrex wedge profile plate with mini-open technique for graft fixation, that ensures better load distribution between coracoid graft and glenoid.
Methods
We did retrospective analysis of 24 patients with recurrent anterior shoulder instability after failed arthroscopic Bankart's repair. Arthroscopic examination of affected shoulder was done in lateral position before making patient supine for open Latarjet. A low profile wedge plate (Arthrex) with two screws was used for the procedure. CT analysis was performed post-operatively at 6 months to see graft union and results were evaluated using the Rowe and Walch Duplay score.
Results
Mean follow-up time was 26 months. Postoperatively, mean forward elevation was 170.6 + 4.6° (loss of average 5.9°) and mean external rotation was 42.5 + 5.3° (loss of average 3.1°). All patients returned to their previous occupation. None reported to be having any recurrent subluxation. Functional assessment done using Rowe score and Walch Duplay score showed statistically significant improvement (p value 0.034). There were no implant-related complications and no case of coracoid graft osteolysis.
Conclusions
Mini-open Latarjet with graft fixation with Arthrex mini-plate provides satisfactory outcome in patients who require reoperation due to dramatic bone loss and failed soft tissue reconstruction. The modified incision improves exposure enabling plate fixation and the secure fixation accelerates rehabilitation.
Keywords: Shoulder instability, Bankarts, Reoperation, Mini-open Latarjet, Wedge profile plate
1. Introduction
Almost 97% of traumatic shoulder dislocations are associated with an underlying Bankart's lesion.1 With the advent of latest arthroscopic techniques and implants, arthroscopic Bankart's repair has become the standard surgical method for primary anterior instability.2, 3, 4, 5, 6 However, in cases with irreparable damage to labrum or significant bony defects of glenoid or humeral head, the arthroscopic Bankart's repair is insufficient to adequately stabilize the shoulder joint.2, 3, 4, 5, 6, 7 Hence, recurrent instability after Bankart's repair is the most frequently reported complication.8 Recurrence rates of open procedures are about 10% whereas those of arthroscopic procedures vary from 0% to 43%.7 Significant amount of these treatment failures are associated with failure to recognize and treat the full extent of pathologic process or bone loss. Major factors associated with failure of Bankart's surgery are significant gleno-humeral bone defects (>25% loss of inferior glenoid diameter or an inverted pear shaped glenoid) and an engaging Hill Sach's lesion.8 The gold standard answer to these failures remains the Latarjet procedure, developed and reported first in 1954, where a large segment of the coracoid (2.5–3 cm in length) was transferred as bone graft to the anterior inferior glenoid rim and fixed with cancellous screws.9
Over time, this procedure has seen a plethora of modifications and changes in an attempt to improve the outcome. We recommend a Modified Latarjet procedure with a slightly medially placed incision that betters the exposure and allows fixation of coracoid with a low profile wedged plate (Arthrex, Naples, FL, USA) through a mini-skin incision. Plate fixation of coracoid would better compression and provide uniform load distribution between the graft and the glenoid bone surface and hence hasten union of graft, apart from enabling accelerated rehabilitation because of more secure fixation. Hence, this study aimed to assess the results of our modified mini-open Latarjet technique in patients with failed arthroscopic Bankart's repair. There are very few studies in literature that have described this procedure where coracoid fixation has been performed with a plate.
2. Material and methods
This prospective study conducted at our institute from June 2011 to May 2013 initially involved 30 patients (29 males and 1 female) who had presented with persistent anterior instability due to failed Bankart's repair. Six patients went out of contact and 24 patients (23 males and 1 female) were eventually available for final follow-up. Mean age of patients was 31.8 years (range 21–37 years) and mean follow-up was 26 months (range 24–30 months). Inclusion criteria involved a positive apprehension test or an occurrence of repeat episode of dislocation in patients who already underwent an arthroscopic Bankart's repair. Patients in whom a primary Latarjet procedure had been performed for instability were excluded from the study.
For assessment of reasons for failure of Bankart's repair, a thorough pre-operative assessment was performed that included documentation of a detailed history and a meticulous clinical examination in every patient. Radiographs of the affected shoulder were performed that included antero-posterior (internal rotation and external rotation) and axillary views. Since radiographs provide only qualitative analysis of bone loss, a three-dimensional computed tomography was additionally obtained in each patient for quantitative measurement of both glenoid (pico method10) and humeral head bone defects. Failed Bankart's repair (positive apprehension test) was found to be attributable to a repeat traumatic episode in 8 patients, significant humeral head bone defect in 7 and significant glenoid bone loss in 9 patients. 12 of these patients had bipolar lesions involving both glenoid and humeral head. All these candidates, after an informed consent, underwent the intended surgical procedure, the details of which have been described below.
2.1. Surgical technique
2.1.1. Positioning
Patients are prepared and draped in lateral position initially and a diagnostic arthroscopy is performed. Size of glenoid bone loss and Hill Sach's lesion are evaluated. The open Latarjet procedure is then performed after making the patient supine. A folded sheet is placed under the scapula to make coracoid more prominent.
2.1.2. Incision
Conventionally, for Latarjet procedure, a standard delto-pectoral approach is employed.9 The incision begins one centimeter proximal to the coracoid process and extends around eight centimeters distally toward the anterior axillary fold. We use mini-open Latarjet technique in which a limited delto-pectoral approach is used. The skin incision begins from 1 cm above the tip of the coracoid extending 4–5 cm toward the axillary fold (Fig. 1). We keep our incision slightly medial to coracoid, so that anterior inferior glenoid neck is easily and better exposed and no vigorous retraction is required, thereby minimizing the chances of any neuro-vascular injury.
Fig. 1.

Photograph showing the modified skin incision for our mini-open Latarjet technique.
2.1.3. Approach
The cephalic vein is protected and retracted laterally. The anterior deltoid is split in order to reach the coracoid process and the conjoined tendon. The coracoid process is exposed from its tip to the insertion of the coraco-clavicular ligaments at its base (Fig. 2A). The coraco-acromial ligament is incised as distally as possible from lateral aspect of the coracoid to aid later in capsular repair and the pectoralis minor tendon insertion on the medial side of the coracoid is visualized.
Fig. 2.

(A) Photograph depicting adequate exposure of coracoid for harvest via our modified Latarjet mini-incision. (B) Coracoid graft harvested and ready to undergo preparation. (C) Photograph showing coracoid graft fixed to antero-inferior glenoid neck with Arthrex mini-plate via mini-open incision.
2.1.4. Harvesting coracoid graft
The pectoralis minor tendon insertion is released with electrocautery from the coracoid process. 70° angled sagittal saw-blade is used to osteotomize the coracoid at its base just distal to attachment of coraco-clavicular ligaments (Fig. 2B). The bone block usually measures 2–3 cm in length. The coracoid graft with attached conjoined tendons is turned over to remove the periosteum and to smooth over its undersurface. We prepare underside of graft by using a reciprocating saw, so as to establish bleeding raw surface to enhance union.
2.1.5. Subscapularis split and glenoid preparation
We split horizontally the subscapularis tendon at its middle-lower third junction and a self-retaining retractor is applied to maintain the exposure of underlying glenoid neck. A vertical capsular incision is performed with the electrocautery. Then, the anterior–inferior glenoid neck is prepared with an osteotome to decorticate the anterior surface.
2.1.6. Coracoid positioning and fixation
Proper positioning of the coracoid bone graft relative to the glenoid is critical. Care is taken not to place the graft too far laterally or medially. It is not intended to be a bone block, and therefore it is placed so that it functions as an extension of the glenoid articular arc. We used a specially designed, wedged profile plate for coracoid fixation (Arthrex, Naples, FL, USA) with two 4 mm cannulated cancellous screws (Arthrex, Naples, FL, USA). Fixation of the graft at the same level as the glenoid preventing lateral overhang or medialization is an important step (Fig. 2C).
2.2. Postoperative protocol
Patient's arm was kept in a shoulder immobilizer up to 2 weeks to protect the healing process of subscapularis and to enhance the osseous union between coracoid graft and anterior glenoid neck. Shoulder pendulum exercises were started from day 1. Passive abduction up to 90° and External rotation up to 30° was initiated from 2nd week with suture removal at end of second week. Strengthening exercises on the biceps were delayed until 3 months postoperatively to protect the coracoid healing. At this time, the bone graft usually would show early radiographic evidence of consolidation with the glenoid. Contact sports and heavy labor work were allowed only after 3 months.
2.3. Follow-up assessment
Follow-up examination was performed at 2 weeks, 6 weeks, 3 months, 6 months, 1 year, and 2 years. Post-operative radiograph assessment was done with true antero-posterior and scapular Y radiographs at every follow-up (Fig. 3). Three-dimensional CT scan was performed after 6 months to confirm union of coracoid graft with glenoid (Fig. 1B–D) and again after 2 years for CT densitometry to study osteolysis in graft if any.
Fig. 3.

AP view right shoulder of a 32-year-old male at 1-year follow-up showing fixation of coracoid graft with Arthrex mini-plate.
Two functional scores were employed to assess the functional status of patients during follow-up – the Rowe score and the Walch Duplay score.11 Pre-operative and post-operative range of motion were recorded by same author during every follow-up and expressed in terms of mean active forward elevation and external rotation with arm by side.
Data were analyzed statistically using the Mann–Whitney student's T-test with statistical significance set at p value <0.05.
3. Results
Out of 24 patients available at final follow-up, 23 were males. The mean follow-up was 26 months (range 24–30 months). The right shoulder was involved in 13 cases (54.17%), and the dominant arm was affected in 11 of these patients (45.83%). All patients had reported at least one episode of frank antero-inferior shoulder dislocation after arthroscopic Bankart's repair (average 1–3 dislocations). However, mean episodes of dislocations before first surgery were 7 (range 2–14). Mean duration between Bankart's repair and mini-open Latarjet procedure was 14.3 months.
Glenoid bone loss was quantified by Pico method.10 Average glenoid bone loss was 21% (range from 16% to 29%).
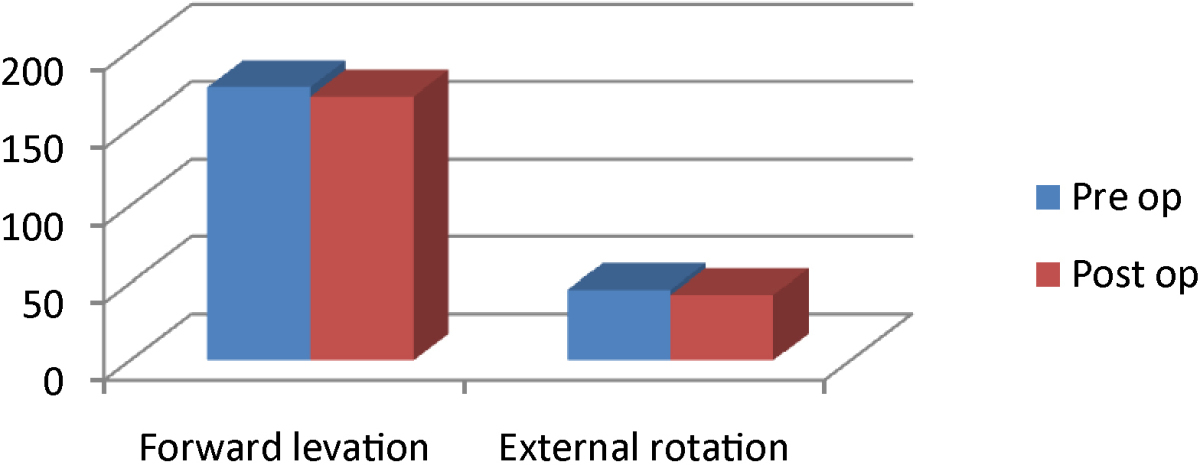
On range of motion assessment (Table 1), preoperatively mean active forward elevation was found to be 176.5 ± 2.5° and mean external rotation with the arm at the side 45.6 ± 10.4°. Post-operative range of motion was comparable to preoperative values with mean active forward elevation 170.6 ± 4.6° (loss of average 5.9°) and mean external rotation with arm by side 42.5 ± 5.3° (loss of average 3.1°).
Table 1.
Outcome after assessment of range of motion (Note that loss in external rotation after surgery was only 3.1°).
Functional assessment using Rowe score showed improvement from average preoperative value of 65 (range from 55 to 75) to average postoperative value of 95 (range from 70 to 100). According to Rowe score, 16 (66.67%) patients had an excellent result (90–100 points), 7 (29.17%) patients had good result (75–89 points), and only 1 (4.17%) patient had fair result (51–74 points). No patient had a poor result. According to Walch Duplay score, 13 (54.17%) patients had an excellent result (91–100 points), 9 (37.5%) patients had a good result (76–90 points), and 2 (8.33%) patients had medium result (51–75 points). The improvement in both scales was statistically significant (p value 0.034). There was no evidence of scapular dyskinesis or static scapular mal-positioning in any patient at final follow-up examination.
The average length of the coracoid graft harvested for surgery was 22.4 ± 2.5 mm. Union of this graft was evaluated radiologically at every follow-up and was achieved in all patients after 7 months (mean: 5 months, range 3–7 months). To assess graft union, a three-dimensional computed tomography was performed at 3 months, 6 months, and 2 years follow-up (Fig. 4A–C). Graft osteolysis was also assessed by CT densitometry at the same time. No case with non-union or significant osteolysis was identified.
Fig. 4.
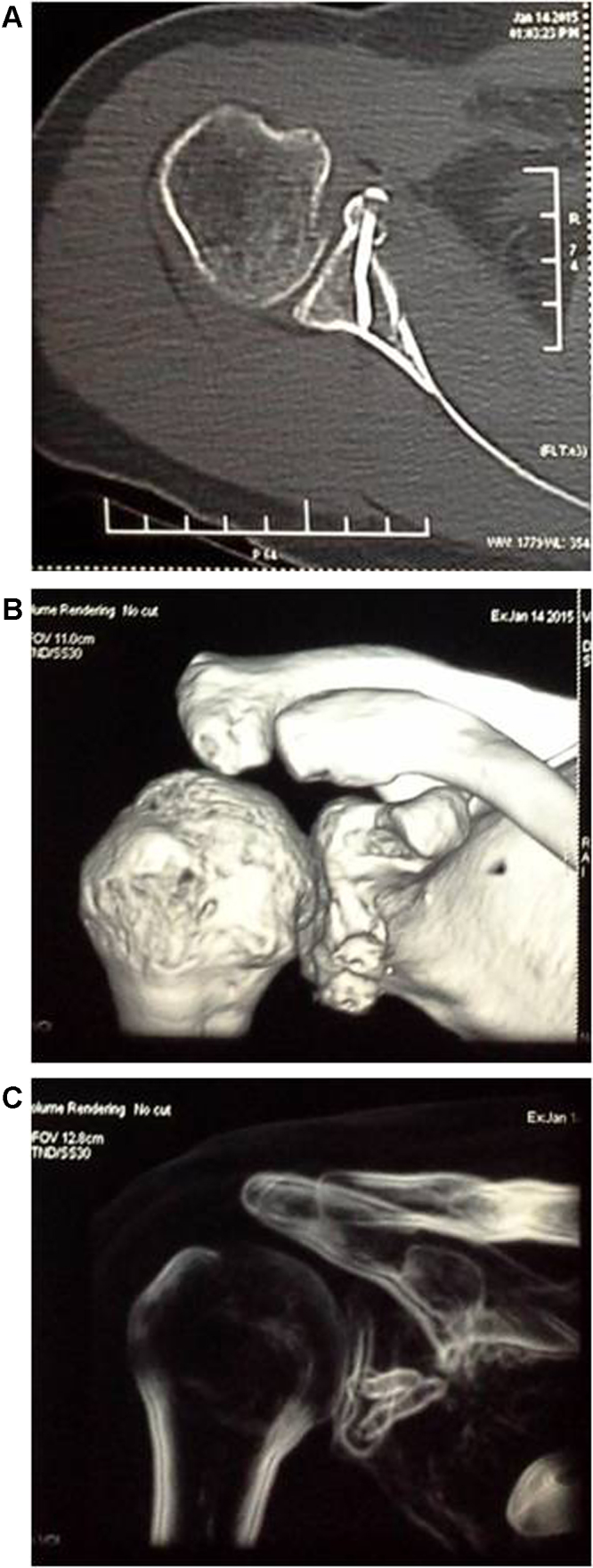
(A–C) CT scan right shoulder of a 26-year-old male at 2-year follow-up showing union after fixation of coracoid graft to glenoid with Arthrex mini-plate.
As far as complications are concerned, only one patient reported a positive apprehension test post-surgery though no episode of dislocation occurred even in that patient till 2 years post-surgery. Residual shoulder pain was reported by six patients (32%) but four had only mild pain while two had moderate pain as per VAS scale. Only patients with superficial wound infection responded to irrigation and oral antibiotics. No neurovascular complication was encountered during surgery or at any follow-up. There were neither hardware related complications nor was any degenerative arthritis encountered till final possible follow-up in any patient.
4. Discussion
Recurrent instability after arthroscopic Bankart repair is often due to unattended bony defects either in glenoid or in humeral head. Burkhart and De Beer,7 who defined the inverted pear shape glenoid, reported that glenoid defects increase recurrence rates to as high as 68% from 4%.
Stability after a Hill-Sachs injury is, however, more dependent upon the location of the bony humeral head defect.13 The track that the humerus glides within the glenoid has been identified as an important factor concerned with shoulder instability.14 When the humerus is in a position of function, Yamamoto and colleagues have demonstrated that the humeral head is seated in 84% of the glenoid cavity as the posterior rim of the glenoid abuts the cuff tendons.3 Any anterior defect to the glenoid reduces the perch that the humeral head has upon the glenoid to less than 84%, decreasing the width of the glenoid track. When a Hill-Sachs lesion rotates outside the glenoid rim and engages the anterior rim of the glenoid, an unstable position for the shoulder occurs.13 If there is less than a normal glenoid bone stock, this ratio becomes increasingly more important as the humeral head may engage easier and become symptomatic when it would not have been symptomatic if the glenoid was fully intact. Thus, the importance of the status of the glenoid defect in the setting of a Hill-Sachs injury cannot be overemphasized, as even small amounts of glenoid bone loss may make a humeral head Hill-Sachs deficiency much more important. Although the exact amount of defects leading to failure is unclear, in the literature, it is accepted that defects of less than 15–20% can be tolerated with soft tissue repair and those over 20–25% require osseous reinforcements.14, 15
The Latarjet procedure with its “Triple effect” (Patte) is the standard surgical procedure for most such patients with significant bony defects.12 Since its first description, the original Latarjet procedure has been modified extensively based on various technical differences like sectioning of lower 1/3 of subscapularis, fixation of coracoid after rotating on its longitudinal axis and fixation of its anterior surface to the glenoid, the extra capsular placement of graft, and the use of anchors for capsulo-labral repair.7, 15, 16 We advocate a mini-open modified Latarjet technique employing smaller incision of 4–5 cm, given slightly medial to coracoid so that antero-inferior glenoid neck is exposed better thereby enabling fixation of coracoid graft with a low profile wedged plate.
Medial placement of the incision has distinct advantages. It enables a relatively easier exposure of antero-inferior glenoid neck without undue retraction so that coracoid graft can be fixed at the desired place. Ghadodra et al.17 stated that fixation of graft level with glenoid may lead to glenohumeral pressures closest to normal. Contact pressures increase by fixing graft laterally by more than 2 mm. Medial placement of graft increases the likelihood of degenerative gleno-humeral arthritis. Through this modified incision, we were able to place coracoid graft at level with glenoid with great accuracy. Also, better exposure allowed us to go for a plate fixation.
Most conventional techniques that have been described in the literature for fixation of coracoid graft with glenoid use screws and washers.11, 12, 16 We have used a wedged low profile plate with 4 mm cannulated cancellous screws for fixation. The mini-plate design has specific characteristics that enhance the compression, stability, and concordance, making it better suited for its desired biomechanical function. It has a wedged profile. The wedge plate if placed medially on the slope on the medial scapular neck under compression, makes the coracoid bone graft rotate medially, thereby improving the bone match between the coracoid bone graft and the glenoid bone surface. It has a figure of eight (Fig. 5) configuration that allows a better torsional orientation of the plate on the dorsal-sloped coracoid surface. Four spikes are there on its undersurface for an improved stabilization of the plate-bone block and it has two appropriately distanced screw holes for lag screws insertion. These features allow the plate to distribute the load more evenly to the bone than the conventional screw and washer combination.
Fig. 5.

Arthrex low profile wedge mini-plate with figure of eight configuration.
On analyzing our results, we found the satisfaction level of patients (based on Walch Duplay and Rowe scores) to be similar to other studies suggesting significant improvements postoperatively. However, most authors (Table 2) have reported a mean loss of 9–12° of external rotation and some have reported external rotation losses of up to 20°.16, 17, 18, 19, 20, 21 Postoperative range of motion has been reported as abduction of 42 ± 17° and external rotation of 48 ± 18° by Allain et al.16 and flexion of 179.6 ± 2.0° and external rotation of 50.2 ± 12.6° by Burkhart and De Beer.22 In our study, loss of external rotation was 6.4° which is less as compared to other studies. Mean forward elevation was 170.6 ± 4.6° (range 158–174°; mean loss of 5.9°) and external rotation with the arm at the side 42.5 ± 5.3° (range 35–60°; mean loss of 3.1°). This is probably because we protect the subscapularis tendon during surgery. An accelerated postoperative rehabilitation enabled by a more secure plate fixation, is another reason to explain these good results, especially that lesser loss in external rotation, which is especially vital for the elite throwing athletes.
Table 2.
| Allain et al. | Burkhart and De beer | Our study |
|---|---|---|
| Mean abduction 42 ± 17° |
Mean forward elevation 179.6 ± 2° |
Mean forward elevation 170.6 ± 4.6° |
| Mean external rotation 48 ± 18° |
Mean external rotation 50.2 ± 12.6° |
Mean external rotation 42.5 ± 5.3° |
Complications reported in literature in context of this procedure mostly pertain to an inadequate surgical technique. Redislocation and glenohumeral arthrosis appear to be the most common complications.22, 23 There are varying reports in literature (Table 3) with regard to recurrent instability with values varying from 1% to 6%.16, 20, 23 In our study, only one patient had a positive apprehension sign after surgery but even he did not report any dislocation till final follow-up. None of our patient developed gleno-humeral arthritis, though follow-up of our study was too short to actually assess it. Allain et al.16 retrospectively reviewed 56 patients at an average of 14.3 years after the Latarjet procedure to determine the prevalence of gleno-humeral arthritis and factors related to its development. Eleven patients (20%) were thought to demonstrate significant gleno-humeral arthritis. The authors concluded that the development of gleno-humeral arthritis is most closely related to a preoperative tear of the rotator cuff and too lateral placement of the coracoid graft.16 Insufficient contact or inconvenient preparation of the surfaces may lead to non-union. Fortunately, none of our patients had graft fracture or developed non-union. The main drawbacks of our study were a small sample size and a short follow-up period.
Table 3.

5. Conclusion
Recurrent instability in a patient with a previously failed shoulder stabilization procedure can be a significant surgical challenge considering patient's expectations from a revision repair. The mini-open Latarjet procedure with wedge plate fixation provides satisfactory outcome and stabilization in this extremely challenging category of patients who present with dramatic bone loss and failed soft tissue reconstruction. We recommend this treatment for young active patients with recurrent anterior shoulder instability after failed arthroscopic Bankart's repair which is associated with the inverted-pear configuration of glenoid bone deficiency or an engaging Hill-Sachs lesion.
Conflict of interest
The authors have none to declare.
References
- 1.Lazarus M., Harryman D. Complications of open anterior stabilization of the shoulder. J Am Acad Orthop Surg. 2000;8:1222–1232. doi: 10.5435/00124635-200003000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Walch G., Boileau P., Levigne C., Mandrino A., Neyret P., Donell S. Arthroscopic stabilization for recurrent anterior shoulder dislocation: results of 59 cases. Arthroscopy. 1995;11:173–179. doi: 10.1016/0749-8063(95)90063-2. [DOI] [PubMed] [Google Scholar]
- 3.Kim S.H., Ha K.I., Cho Y.B., Ryu B.D., Oh I. Arthroscopic anterior stabilization of the shoulder: two to six-year follow-up. J Bone Joint Surg Am. 2003;85:1511–1518. [PubMed] [Google Scholar]
- 4.Westerheide K.J., Dopirak R.M., Snyder S.J. Arthroscopic anterior stabilization and posterior capsular plication for anterior glenohumeral instability: a report of 71 cases. Arthroscopy. 2006;22:539–547. doi: 10.1016/j.arthro.2005.12.033. [DOI] [PubMed] [Google Scholar]
- 5.Mohtadi N.G., Bitar I.J., Sasyniuk T.M., Hollinshead R.M., Harper W.P. Arthroscopic versus open repair for traumatic anterior shoulder instability: a meta-analysis. Arthroscopy. 2005;21:652–658. doi: 10.1016/j.arthro.2005.02.021. [DOI] [PubMed] [Google Scholar]
- 6.Cole B.J., Warner J.J. Arthroscopic versus open Bankart repair for traumatic anterior shoulder instability. Clin Sports Med. 2000;19:19–48. doi: 10.1016/s0278-5919(05)70294-5. [DOI] [PubMed] [Google Scholar]
- 7.Burkhart S.S., De Beer J.F. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16:677–694. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
- 8.Stein D.A., Jazrawi L., Bartolozzi A.R. Arthroscopic stabilization of anterior shoulder instability: a review of the literature. Arthroscopy. 2002;18:912–924. doi: 10.1053/jars.2002.36148. [DOI] [PubMed] [Google Scholar]
- 9.Latarjet M. Traitement de la luxation récidivante de l’épaule. Treatment of recurrent dislocation of the shoulder. Lyon Chirurgical. 1954;49:994–997. [PubMed] [Google Scholar]
- 10.Bois A.J., Fening S.D., Polster J., Jones M.H., Miniaci A. Quantifying glenoid bone loss in anterior shoulder instability reliability and accuracy of 2-dimensional and 3-dimensional computed tomography measurement techniques. Am J Sports Med. 2012;40(11) doi: 10.1177/0363546512458247. [DOI] [PubMed] [Google Scholar]
- 11.Edouard P., Beguin L., Fayolle-Minon I., Degache F., Farizon F., Calmels P. Relationship between strength and functional indexes (Rowe and Walch-Duplay scores) after shoulder surgical stabilization by the Latarjet technique. Ann Phys Rehabil Med. 2010;53(October (8)):499–510. doi: 10.1016/j.rehab.2010.07.033. [Epub 2010 Aug 27] [DOI] [PubMed] [Google Scholar]
- 12.Mercier N., Saragaglia D. Mini-open latarjet procedure for recurrent anterior shoulder instability. Adv Orthop. 2011;2011 doi: 10.4061/2011/656205. AN Article ID 656205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yamamoto N., ltol E., Abe H. Contact between the glenoid and the humeral head in abduction, external rotation and horizontal extension: a new concept of glenoid track. J Shoulder Elbow Surg. 2007;16(5):649–656. doi: 10.1016/j.jse.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 14.Burkhart S.S., Danaceau S.M. Articular arc length mismatch as a cause of failed Bankart repair. Arthroscopy. 2000;16(7):740–744. doi: 10.1053/jars.2000.7794. [DOI] [PubMed] [Google Scholar]
- 15.Provencher M.T., Bhatia S., Ghodadra N.S., Grumet R.C., Bach B.R., Dewing C.B. Recurrent shoulder instability: current concepts for evaluation and management of glenoid bone loss. J Bone Joint Surg Am. 2010;92(2):133–151. doi: 10.2106/JBJS.J.00906. [DOI] [PubMed] [Google Scholar]
- 16.Allain J., Goutallier D., Glorion C. Long-term results of the latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg A. 1998;80(6):841–852. doi: 10.2106/00004623-199806000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Ghadodra N., Gupta A., Romeo A.A., Bach B.R., Verma N., Shewman E. Normalization of glenohumeral articular contact pressures after Latarjet or iliac crest bone grafting. J Bone Joint Surg Am. 2010;92:1478–1489. doi: 10.2106/JBJS.I.00220. [DOI] [PubMed] [Google Scholar]
- 18.Weng P.W., Shen H.C., Lee H.H., Wu S.S., Lee C.H. Open reconstruction of large bony glenoid erosion with allergenic bone graft for recurrent anterior shoulder dislocation. Am J Sports Med. 2009;37(9):1792–1797. doi: 10.1177/0363546509334590. [DOI] [PubMed] [Google Scholar]
- 19.Banas M.P., Dalldorf P.G., Sebastianelli W.J., DeHaven K.E., Warren R.F. Long-term follow up of the modified Bristow procedure. Am J Sports Med. 1993;21(5):666–671. doi: 10.1177/036354659302100505. [DOI] [PubMed] [Google Scholar]
- 20.Hovelius L.K., Sandström B.C., Rösmark D.L., Saebö M., Sundgren K.H., Malmqvist B.G. Long-term results with the Bankart and Bristow-Latarjet procedures: recurrent shoulder instability and arthropathy. J Shoulder Elbow Surg. 2001;10(5):445–452. doi: 10.1067/mse.2001.117128. [DOI] [PubMed] [Google Scholar]
- 21.Singer G.C., Kirkland P.M., Emery R.J.H. Coracoid transposition for recurrent anterior instability of the shoulder. A 20-year follow-up study. J Bone Joint Surg B. 1995;77(1):73–76. [PubMed] [Google Scholar]
- 22.Burkhart S., De Beer J., Barth J. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy. 2007;23(10):1033–1041. doi: 10.1016/j.arthro.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 23.Hill J.A., Lombardo S.J., Kerlan R.K. The modified Bristow-Helfet procedure for recurrent anterior shoulder subluxations and dislocations. Am J Sports Med. 1981;9(5):283–287. doi: 10.1177/036354658100900501. [DOI] [PubMed] [Google Scholar]


