1. Introduction
Recurrent posterior dislocation of the shoulder (RPDS) due to trauma is extremely rare, with few cases reported to date.1, 2, 3, 4, 5 Here, we report a case of RPDS associated with the Buford complex. The Buford complex is a normal anatomical variant of the anterosuperior part of the glenoid.6, 7 To date, all reports mention axial forces applied to the shoulder during anterior elevation, horizontal adduction, and mild inner rotation as the causes of posterior dislocation.4, 8, 9 However, the dislocation position of RPDS reported here was completely different from those reported to date. The dislocation occurred when the patient forcibly extended and horizontally abducted his arm with internal rotation, without any direct external force being applied to the shoulder joint. Rao et al. suggested that the range of passive internal rotation during 90° shoulder abduction is strongly associated with anterosuperior labral variations including the Buford complex, which may predispose the shoulder to lesions of the superior glenohumeral ligament and the anterosuperior portion of the labrum. Our case was believed to be associated with the Buford complex because the dislocation occurred without major trauma.10 Surgery was performed for treatment because of some daily life disturbances reported by the patient. Repair of RPDS includes repair of the posteroinferior labrum injury (posterior Bankart lesion), plaication,8 and bone–block procedures to repair the bone defect of the humeral head (reverse Hill–Sachs lesion)11, 12, 13 or strengthening the subscapularis tendon.2, 14, 15, 16 The patient was informed that data from this case would be submitted for publication, and consent was obtained. This report was approved by our institutional review board.
2. Case
The patient is a 34-year-old male company employee with a history of RPDS, and the anxiety regarding repeated dislocations was affecting his activities of daily living. The patient had no remarkable medical history, but he almost fell with his shoulder in the extended position while carrying a 2-kg blueprint at the age of 28 years. The first dislocation occurred when he forcibly extended and horizontally abducted his arm with internal rotation, without any direct external force being applied to the shoulder joint. The patient was diagnosed with an acute posterior dislocation of the shoulder, and reduction was performed. The second dislocation occurred 3 years after the first dislocation, when the patient reached back with his hand to support a fire door that was closing behind him in a similar position to that during the first dislocation. The third and final dislocation occurred approximately 3 years after the second dislocation while “stretching” with both hands for clasping them behind him, with chest out and shoulders extended. In each case, self-reduction was difficult, and the patient required reduction during hospitalization.
2.1. Findings on initial examination
Range of motion was slightly restricted with pain and anxiety. No muscle weakness was detected, and the anterior apprehension sign was positive. In addition, dislocation anxiety was observed when forced horizontal abduction was attempted at 45° abduction, which became more prominent with internal rotation. The posterior jerk test during forward flexion and horizontal adduction, which reveals posterior instability, was completely negative. In addition, the sulcus sign and general joint laxity were negative.
2.2. Image findings
The humeral head was posterior to the glenoid fossa on a plain X-ray taken by the previous doctor prior to reduction. Computed tomography revealed an anterior bone defect in the humeral head (defect size, approximately 15%; Fig. 1). Magnetic resonance imaging (MRI) confirmed the anterior bone defect in the humeral head (Fig. 2), and contrast agent flowed between the posteroinferior labrum and the glenoid. In addition, the medial glenohumeral ligament (MGHL) was highly developed, and the anterosuperior labrum was not visualized. Based on these observations, the patient was diagnosed with RPDS caused by minor trauma. This result had a negative impact on his activities of daily living, as dislocation occurred easily, and surgery was consequently performed under arthroscopy.
Fig. 1.
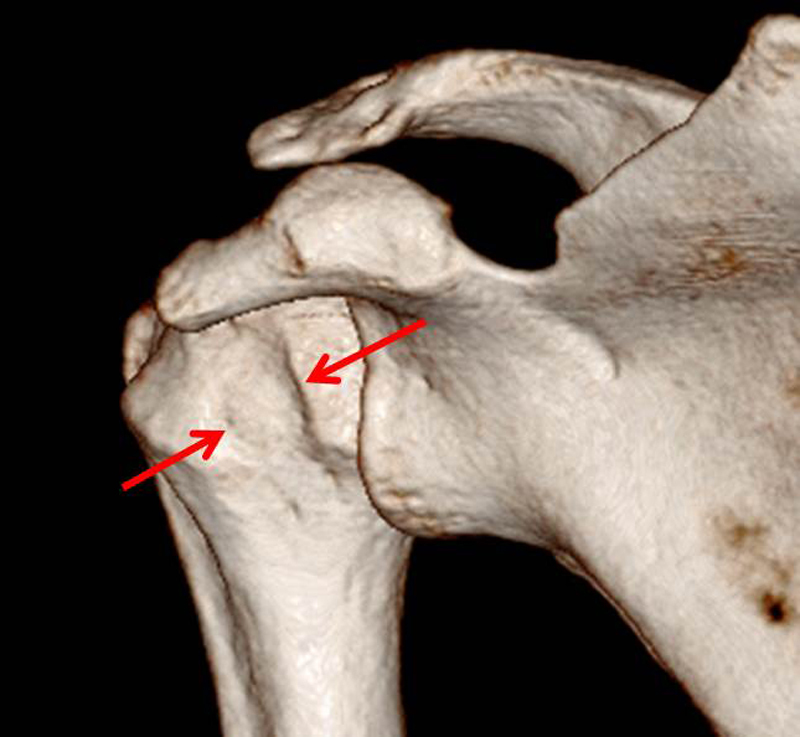
Three-dimensional computed tomography scan. The reverse Hill–Sachs lesion of the posteriorly dislocated shoulder is shown (arrow).
Fig. 2.

Preoperative magnetic resonance arthrography images. We confirmed an osteochondral defect of the humeral head (arrow) on a T2-weighted axial image. Excess internal rotation may have caused engagement of the defect to the posterior edge of the glenoid (bold arrow).
2.3. Surgical findings
During an examination under anesthesia, instability was noted in both the anterior and posterior directions. The Buford complex was observed as the absence of the anterosuperior labrum and presence of a cord-like middle glenohumeral ligament. Findings suggestive of synovitis were observed in the rotator interval (Fig. 3). Delamination damage to the posterior labrum was observed. No Hill–Sachs lesion was found in the posterosuperior humeral head, but an anterior reverse Hill–Sachs lesion was observed (Fig. 4). No posterior subluxation was observed during anterior flexion or horizontal abduction while performing the posterior jerk test. However, subluxation was observed when the reverse Hill–Sachs lesion and detached posteroinferior labrum collided during internal rotation and horizontal abduction (Fig. 5, Fig. 6). Arthroscopic repair of the posterior Bankart lesion was performed similarly to the anteroinferior stabilization (Fig. 5b). Next, we performed surgery on the posteriorly dislocated shoulder by transferring the subscapularis tendon from its insertion at the lesser tuberosity and suturing it into the reverse Hill–Sachs lesion using suture anchors (modified McLaughlin procedure) because the bone defect easily engaged the glenoid with internal rotation (Fig. 6b).
Fig. 3.

Arthroscopic findings. (a) Right shoulder. Arthroscopic view from the posterior portal with the patient in the lateral position, showing the Buford complex with the cord-like medial glenohumeral ligament (MGHL). (b) Absence of the anterosuperior labrum. (c) Inflammation of the rotator interval. G, Glenoid; HH, Humeral head; L, Labrum; LHB, Long head of biceps tendon; MGHL, Middle glenohumeral ligament; RI, Rotator interval; SSC, Subscapularis tendon.
Fig. 4.
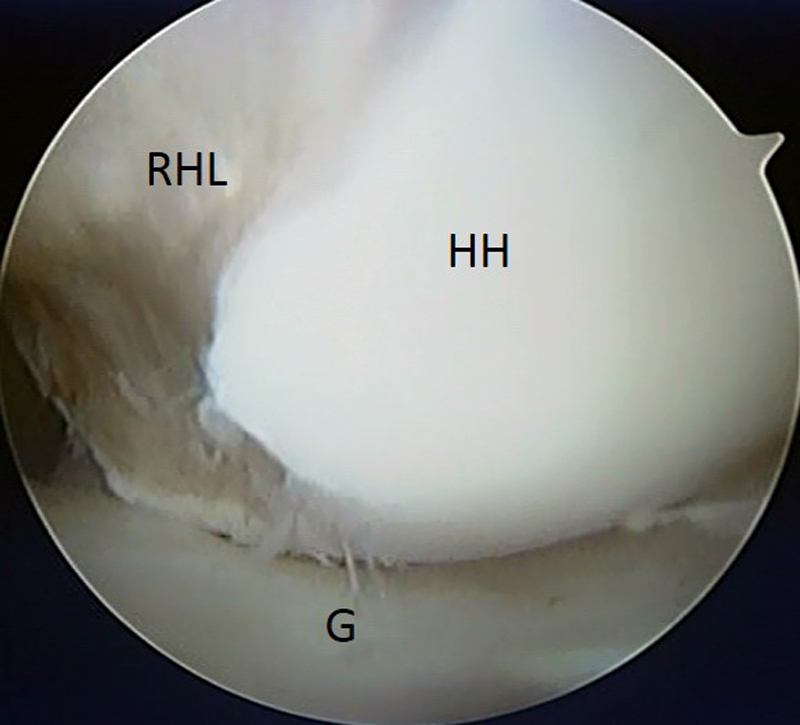
Arthroscopic view from the anterior portal with the patient in the lateral position, showing the reverse Hill–Sachs lesion. Internal rotational position, indicating the reverse Hill–Sachs lesion closer to the posterior injured labrum. G, Glenoid; HH, Humeral head; RHL, Reverse Hill–Sachs lesion.
Fig. 5.

Intraoperative arthroscopic images with a posterior labral detachment, as observed from the anterosuperior viewing portal. (a) Avulsion plus torn posterior labrum. (b) The suture was tied after elevating the labrum from the glenoid neck, and the labral tissue was approximated to the glenoid rim using one bioabsorbable suture and two suture anchors. The posteroinferior glenohumeral ligament (PIGHL) was restored. G, Glenoid; HH, Humeral head; PIGHL, Posteroinferior glenohumeral ligament.
Fig. 6.

Arthroscopic McLaughlin procedure. (a) Reverse Hill–Sachs defect with cartilage lesion and subchondral bone impression fractures. (b) We performed the arthroscopic McLaughlin procedure to attach the subscapularis tendon to the humeral head with one bioabsorbable suture and two suture anchors. The subscapularis tendon was tied into the bony defect to provide stability for the glenohumeral joint. HH, Humeral head; MGHL, Middle glenohumeral ligament; RHL, Reverse Hill–Sachs lesion; RI, Rotator interval; SSC, Subscapularis tendon.
2.4. Postoperative treatment and results
A sling was worn for 3 weeks. From the third day post-surgery, under the physical therapy, the patient started trunk-functional, scapulothoracic, and stooping exercises for the shoulder joint. The glenohumeral joint was also actively exercised within a confirmed range of motion after surgery. The difference between the range of motion on the healthy side and the affected side was −10° flexion, −10° abduction, and −20° external rotation, and no difference in internal rotation at 2 years after the surgery, with no major restrictions, was observed. No further dislocation anxiety has occurred, and the patient is following a favorable course. The postoperative MRI control image after surgery showed perfect integration of the subscapularis tendon into the reverse Hill–Sachs defect, preventing repetitive dislocation (Fig. 7).
Fig. 7.

Axial section magnetic resonance (MR) image after modified arthroscopic McLaughlin procedure. The postoperative MR control image after 24 weeks shows perfect integration of the subscapularis tendon into the reverse Hill–Sachs defect, which prevented repetitive dislocation.
3. Discussion
RPDS is extremely rare. Robinson et al. reported that the prevalence of acute posterior dislocation was 1.1 per 100,000 per year, and only 20 (23 shoulders) of 112 patients develop recurrent instability.4 To the best of our knowledge, no cases of RPDS associated with the Buford complex have been reported. All reports to date mention axial forces applied to the shoulder during anterior elevation, horizontal adduction, and mild inner rotation as the causes of posterior dislocation because these positions are close to those that induce dislocation.4, 8, 9 Our patient experienced dislocation when internal rotation was applied during mild abduction and horizontal abduction, and dislocation anxiety occurred in the same arm position, which is completely different from reports to date (Fig. 8).
Fig. 8.
Assumed mechanism of posterior dislocation associated with the Buford complex. Internal rotation increased further during horizontal abduction and abduction due to the influence of the Buford complex. The reverse Hill–Sachs lesion engaged with the posterior glenoid edge when internal rotation was applied.
The Buford complex was first described by Williams et al. in 1994.7 It is a normal anatomical variant of anterosuperior shoulder anatomy consisting of an absent anterosuperior labrum with a cord-like structure called the MGHL. Although widely described as a normal variant, the Buford complex and the sublabral foramen can predispose patients to develop intra-articular lesions. Rao et al. found that a study group of these patients had a significantly greater range of motion in active (p = 0.001) and passive (p = 0.003) internal rotation of shoulder abduction than the standard anatomy group. They suggested that variations in the anterosuperior portion of the labrum, as in the Buford complex, are associated with increased internal rotation, which may predispose the shoulder to lesions in the superior glenohumeral ligament and anterosuperior portion of the labrum. Abnormal findings were clearly observed in the rotator interval under arthroscopy in our case, and we assumed that chronic stimuli had been applied to the same area. Moreover, no report has considered the possible relationship between instability and the Buford complex without trauma. They also mentioned that these variations do not appear to contribute to instability. However, the present case revealed excess translation to both the anterior and posterior directions. The labrum provides a point of attachment for the soft tissue stabilizers, the glenohumeral ligaments, and the capsule.10 In our case, detachment of the complete posteroinferior labrum appeared to be due to posterior dislocation; therefore, half of the labrum disappeared. We speculate that this loss of a part of the anterior labrum was related to the reduced effective depth of concavity, reduced concavity compression stability, and reduced resistance to translating forces in the glenohumeral joint.17
Surgical treatment for RPDS is indicated if a manipulative reduction is performed for the first dislocation and if the dislocation recurs during conservative therapy.18, 19 Although few studies are available on RPDS, the algorithm of Paul et al. provides guidelines for decision making including minimally invasive treatment options according to the available literature.16 In this review, they describe that the gold standard is operative stabilization using the McLaughlin procedure2 or a modified technique for patients with unstable shoulders after RPDS and impression fractures of <33–50% of the humeral head. One modification is plication of the subscapularis tendon into the reverse Hill–Sachs defect using suture anchors to secure the subscapularis tendon into the humeral defect, thereby preventing further engagement of the anterior part of the humeral head with the posterior part of the glenoid rim.
In the present case, surgery was indicated because the shoulder was dislocating easily during activities of daily living. In addition, the reverse Hill–Sachs lesion easily engaged with the delaminated posterior labrum during arthroscopy, and subluxation was observed in the same arm position. Therefore, we performed the arthroscopic McLaughlin procedure in this case to prevent translation to the superior anterior direction.
Conflicts of interest
We affirm that we have no financial affiliation (including research funding) or involvement with any commercial organization that has a direct financial interest in any matter included in this manuscript. There is no conflict of interest.
References
- 1.Hawkins R.J., Neer C.S., 2nd, Pianta R.M., Mendoza F.X. Locked posterior dislocation of the shoulder. J Bone Joint Surg Am. 1987;69(1):9–18. [PubMed] [Google Scholar]
- 2.McLaughlin L.H. Posterior dislocation of the shoulder. J Bone Joint Surg Am. 1952;24-A(3):584–590. [PubMed] [Google Scholar]
- 3.Robinson C.M., Aderinto J. Posterior shoulder dislocations and fracture-dislocations. J Bone Joint Surg Am. 2005;87(3):639–650. doi: 10.2106/JBJS.D.02371. [DOI] [PubMed] [Google Scholar]
- 4.Robinson C.M., Seah M., Akhtar M.A. The epidemiology, risk of recurrence, and functional outcome after an acute traumatic posterior dislocation of the shoulder. J Bone Joint Surg Am. 2011;93(17):1605–1613. doi: 10.2106/JBJS.J.00973. [DOI] [PubMed] [Google Scholar]
- 5.Walch G., Boileau P., Martin B., Dejour H. Unreduced posterior luxations and fractures-luxations of the shoulder, Apropos of 30 cases. Rev Chir Orthop Reparatrice Appar Mot. 1990;76(8):546–558. [PubMed] [Google Scholar]
- 6.Tirman P.F., Feller J.F., Palmer W.E., Carroll K.W., Steinbach L.S., Cox I. The Buford complex—a variation of normal shoulder anatomy: MR arthrographic imaging features. Am J Roentgenol. 1996;166(4):869–873. doi: 10.2214/ajr.166.4.8610565. [DOI] [PubMed] [Google Scholar]
- 7.Williams M.M., Snyder S.J., Buford D., Jr. The Buford complex—the cord-like middle glenohumeral ligament and absent anterosuperior labrum complex: a normal anatomic capsulolabral variant. Arthroscopy. 1994;10(3):241–247. doi: 10.1016/s0749-8063(05)80105-7. [DOI] [PubMed] [Google Scholar]
- 8.Lenart B.A., Sherman S.L., Mall N.A., Gochanour E., Twigg S.L., Nicholson G.P. Arthroscopic repair for posterior shoulder instability. Arthroscopy. 2012;28(10):1337–1343. doi: 10.1016/j.arthro.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 9.Shah A.A., Butler R.B., Fowler R., Higgins L.D. Posterior capsular rupture causing posterior shoulder instability: a case report. Arthroscopy. 2011;27(9):1304–1307. doi: 10.1016/j.arthro.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 10.Rao A.G., Kim T.K., Chronopoulos E., McFarland E.G. Anatomical variants in the anterosuperior aspect of the glenoid labrum: a statistical analysis of seventy-three cases. J Bone Joint Surg Am. 2003;85-A(4):653–659. doi: 10.2106/00004623-200304000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Assom M., Castoldi F., Rossi R., Blonna D., Rossi P. Humeral head impression fracture in acute posterior shoulder dislocation: new surgical technique. Knee Surg Sports Traumatol Arthrosc. 2006;14(7):668–672. doi: 10.1007/s00167-005-0001-x. [DOI] [PubMed] [Google Scholar]
- 12.Bock P., Kluger R., Hintermann B. Anatomical reconstruction for reverse Hill–Sachs lesions after posterior locked shoulder dislocation fracture: a case series of six patients. Arch Orthop Trauma Surg. 2007;127(7):543–548. doi: 10.1007/s00402-007-0359-y. [DOI] [PubMed] [Google Scholar]
- 13.Khayal T., Wild M., Windolf J. Reconstruction of the articular surface of the humeral head after locked posterior shoulder dislocation: a case report. Arch Orthop Trauma Surg. 2009;129(4):515–519. doi: 10.1007/s00402-008-0762-z. [DOI] [PubMed] [Google Scholar]
- 14.Krackhardt T., Schewe B., Albrecht D., Weise K. Arthroscopic fixation of the subscapularis tendon in the reverse Hill–Sachs lesion for traumatic unidirectional posterior dislocation of the shoulder. Arthroscopy. 2006;22(2):227. doi: 10.1016/j.arthro.2005.10.004. e1–e6. [DOI] [PubMed] [Google Scholar]
- 15.Paul J., Buchmann S., Beitzel K., Solovyova O., Imhoff A.B. Posterior shoulder dislocation: systematic review and treatment algorithm. Arthroscopy. 2011;27(11):1562–1572. doi: 10.1016/j.arthro.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 16.Paul J.H.S., Wörtler K., Imhoff A.B. Arthroscopic transfer of the M. subscapularis in the reverse Hill–Sachs defect. Arthroskopie. 2008;21:188–191. [Google Scholar]
- 17.Lippitt S., Matsen F. Mechanisms of glenohumeral joint stability. Clin Orthop Relat Res. 1993;291:20–28. [PubMed] [Google Scholar]
- 18.Bradley J.P., Baker C.L., 3rd, Kline A.J., Armfield D.R., Chhabra A. Arthroscopic capsulolabral reconstruction for posterior instability of the shoulder: a prospective study of 100 shoulders. Am J Sports Med. 2006;34(7):1061–1071. doi: 10.1177/0363546505285585. [DOI] [PubMed] [Google Scholar]
- 19.Savoie F.H., 3rd, Holt M.S., Field L.D., Ramsey J.R. Arthroscopic management of posterior instability: evolution of technique and results. Arthroscopy. 2008;24(4):389–396. doi: 10.1016/j.arthro.2007.11.004. [DOI] [PubMed] [Google Scholar]



