Abstract
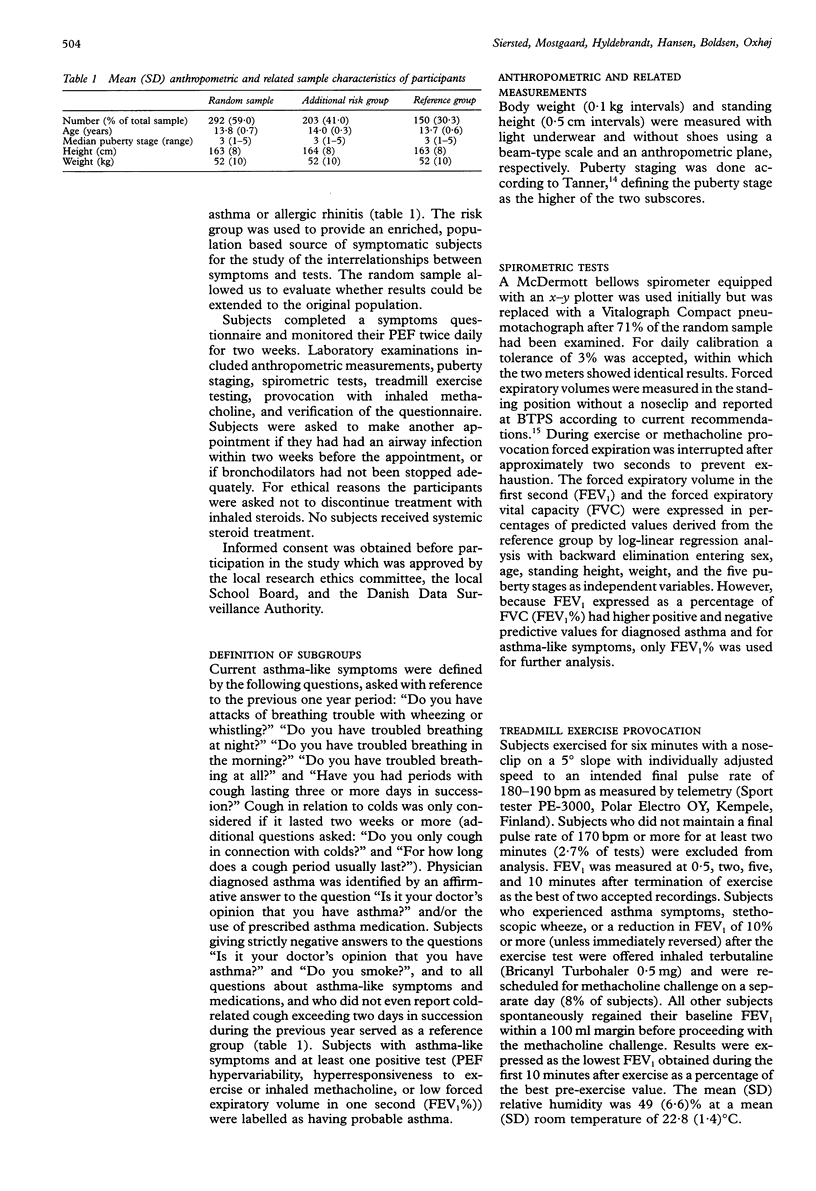
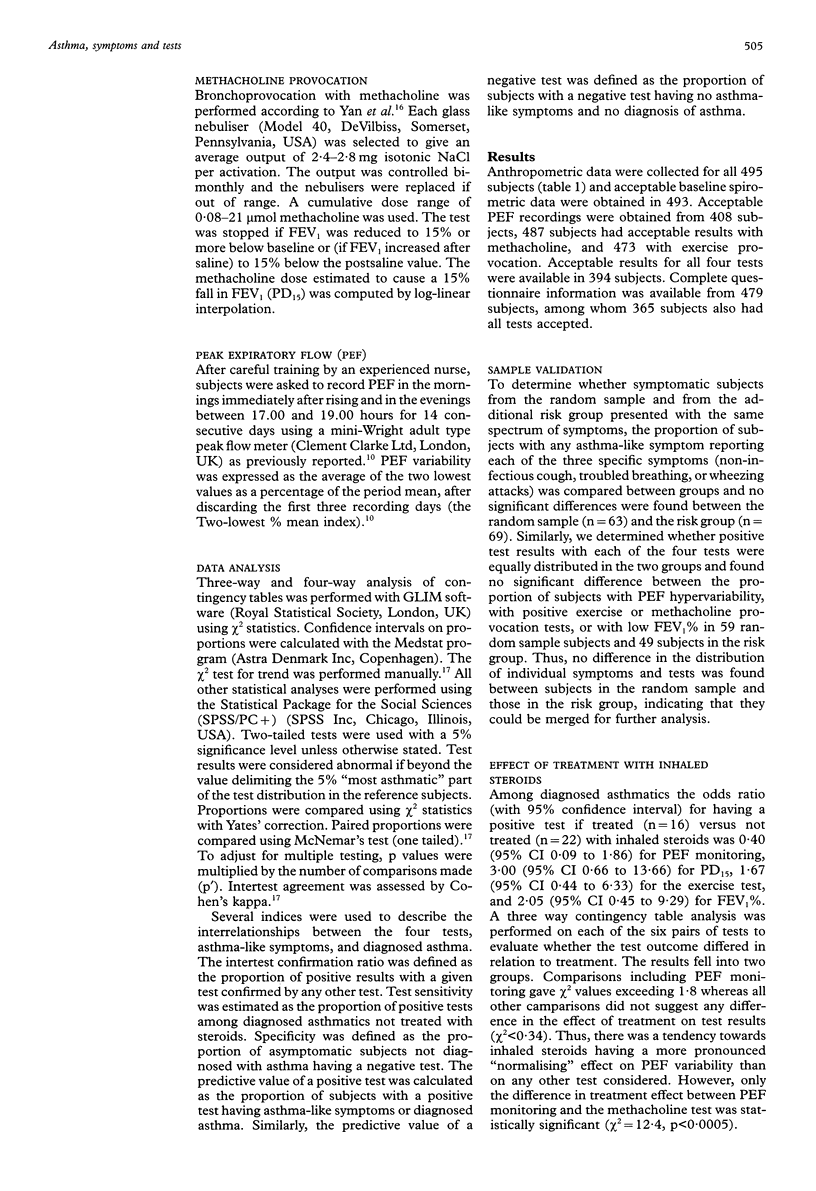
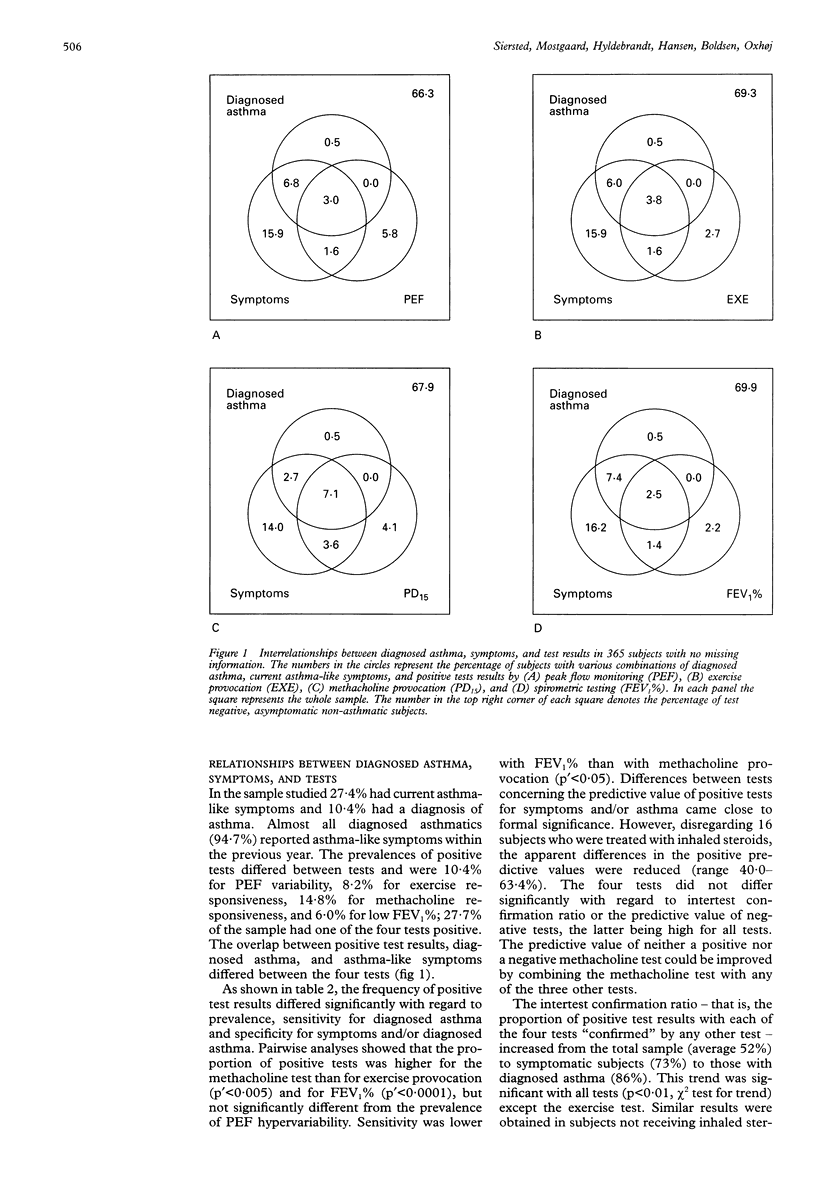
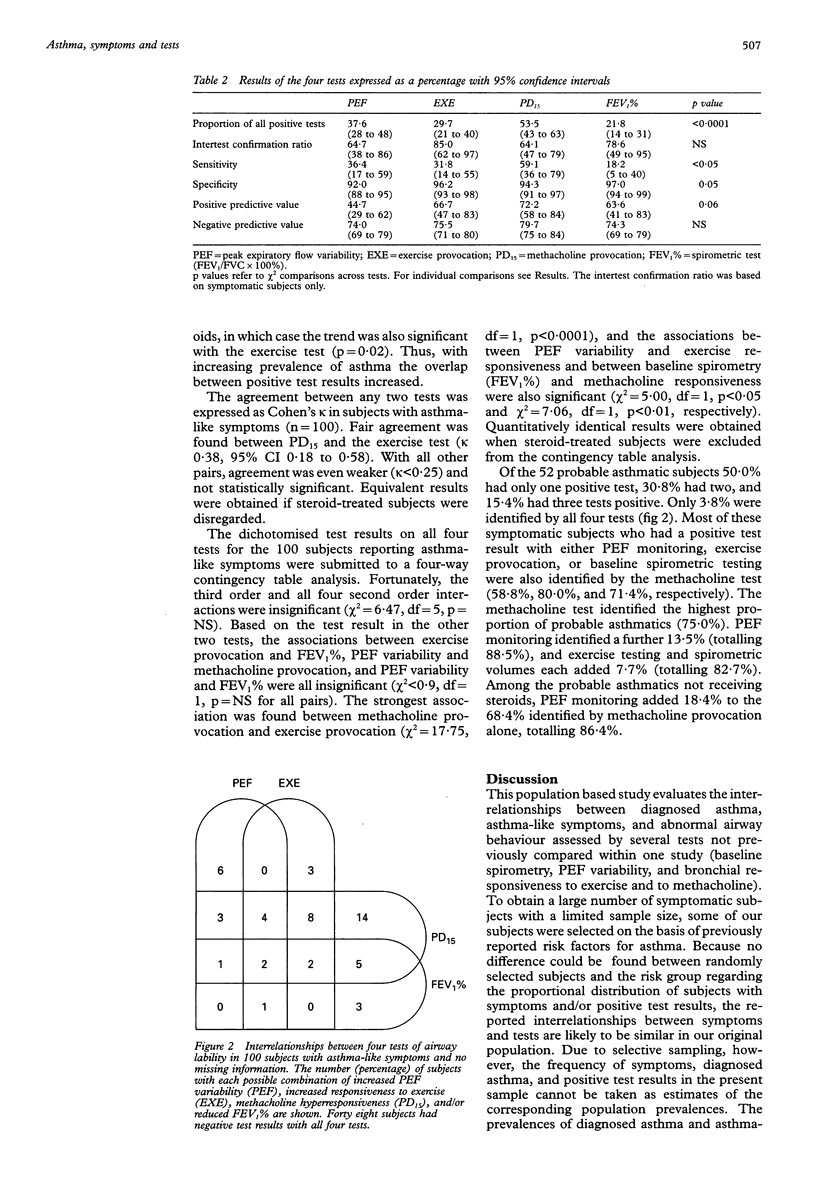
BACKGROUND: The diagnosis of asthma is based on several characteristics including symptoms and suitable tests of airway lability. However, it is neither clear to what degree various tests and symptoms identify the same subjects, nor how these characteristics are best combined to diagnose asthma. The interrelationships between physician-diagnosed asthma, asthma-like symptoms, and abnormal airway function, as defined by four commonly used tests, have therefore been assessed. METHODS: A population based sample of 495 Danish schoolchildren aged 12-15 years, comprising 292 randomly selected subjects and 203 subjects considered at risk of having or developing asthma, was examined. Symptoms and background information were recorded by questionnaire. The test panel consisted of baseline forced expiratory volume in one second (FEV1%), provocation with treadmill exercise (EXE) and with inhaled methacholine (PD15), and monitoring of peak expiratory flow (PEF) twice daily for two weeks. RESULTS: The sensitivity for diagnosed asthma was highest for PD15 followed by PEF monitoring, whereas specificity for asthma or asthma-like symptoms was marginally higher with the other two tests. Most symptomatic subjects with any positive test were identified by PD15 alone (75%) or in combination with PEF monitoring (89%). PEF variability was more susceptible to treatment with inhaled steroids than the PD15 index. Although inter-test agreement was weak (kappa < 0.40 for all pairs), significant associations were found between PD15 and EXE, PEF and EXE, and FEV1% and PD15. CONCLUSIONS: The agreement between the four tests was weak. In particular, PEF variability and methacholine responsiveness seem to identify different varieties of airway pathophysiology. The combined use of methacholine provocation testing and PEF monitoring may be helpful as an epidemiological screening tool for asthma.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Asher M. I., Keil U., Anderson H. R., Beasley R., Crane J., Martinez F., Mitchell E. A., Pearce N., Sibbald B., Stewart A. W. International Study of Asthma and Allergies in Childhood (ISAAC): rationale and methods. Eur Respir J. 1995 Mar;8(3):483–491. doi: 10.1183/09031936.95.08030483. [DOI] [PubMed] [Google Scholar]
- Bardagi S., Agudo A., Gonzalez C. A., Romero P. V. Prevalence of exercise-induced airway narrowing in schoolchildren from a Mediterranean town. Am Rev Respir Dis. 1993 May;147(5):1112–1115. doi: 10.1164/ajrccm/147.5.1112. [DOI] [PubMed] [Google Scholar]
- Brand P. L., Postma D. S., Kerstjens H. A., Koëter G. H. Relationship of airway hyperresponsiveness to respiratory symptoms and diurnal peak flow variation in patients with obstructive lung disease. The Dutch CNSLD Study Group. Am Rev Respir Dis. 1991 May;143(5 Pt 1):916–921. doi: 10.1164/ajrccm/143.5_Pt_1.916. [DOI] [PubMed] [Google Scholar]
- Burney P. G., Luczynska C., Chinn S., Jarvis D. The European Community Respiratory Health Survey. Eur Respir J. 1994 May;7(5):954–960. doi: 10.1183/09031936.94.07050954. [DOI] [PubMed] [Google Scholar]
- Fowler M. G., Davenport M. G., Garg R. School functioning of US children with asthma. Pediatrics. 1992 Dec;90(6):939–944. [PubMed] [Google Scholar]
- Frischer T., Kühr J., Meinert R., Karmaus W., Forster J., Urbanek R. Relation between response to exercise and diurnal variability of peak expiratory flow in primary school children. Thorax. 1993 Mar;48(3):249–253. doi: 10.1136/thx.48.3.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen H. S., Hyldebrandt N., Nielsen J. R., Froberg K. Blood pressure distribution in a school-age population aged 8-10 years: the Odense Schoolchild Study. J Hypertens. 1990 Jul;8(7):641–646. doi: 10.1097/00004872-199007000-00007. [DOI] [PubMed] [Google Scholar]
- Haugaard L., Iversen M., Dahl R. A comparative study of four different bronchial challenge tests. Allergy. 1992 Apr;47(2 Pt 2):138–142. doi: 10.1111/j.1398-9995.1992.tb00954.x. [DOI] [PubMed] [Google Scholar]
- Higgins B. G., Britton J. R., Chinn S., Cooper S., Burney P. G., Tattersfield A. E. Comparison of bronchial reactivity and peak expiratory flow variability measurements for epidemiologic studies. Am Rev Respir Dis. 1992 Mar;145(3):588–593. doi: 10.1164/ajrccm/145.3.588. [DOI] [PubMed] [Google Scholar]
- Kerstjens H. A., Brand P. L., de Jong P. M., Koëter G. H., Postma D. S. Influence of treatment on peak expiratory flow and its relation to airway hyperresponsiveness and symptoms. The Dutch CNSLD Study Group. Thorax. 1994 Nov;49(11):1109–1115. doi: 10.1136/thx.49.11.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neville R. G., Bryce F. P., Robertson F. M., Crombie I. K., Clark R. A. Diagnosis and treatment of asthma in children: usefulness of a review of medical records. Br J Gen Pract. 1992 Dec;42(365):501–503. [PMC free article] [PubMed] [Google Scholar]
- Nish W. A., Schwietz L. A. Underdiagnosis of asthma in young adults presenting for USAF basic training. Ann Allergy. 1992 Sep;69(3):239–242. [PubMed] [Google Scholar]
- Perin P. V., Weldon D., McGeady S. J. Objective indicators of severity of asthma. J Allergy Clin Immunol. 1994 Sep;94(3 Pt 1):517–522. doi: 10.1016/0091-6749(94)90208-9. [DOI] [PubMed] [Google Scholar]
- Siersted H. C., Hansen H. S., Hansen N. C., Hyldebrandt N., Mostgaard G., Oxhøj H. Evaluation of peak expiratory flow variability in an adolescent population sample. The Odense Schoolchild Study. Am J Respir Crit Care Med. 1994 Mar;149(3 Pt 1):598–603. doi: 10.1164/ajrccm.149.3.8118624. [DOI] [PubMed] [Google Scholar]
- Tanner J. M., Whitehouse R. H. Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch Dis Child. 1976 Mar;51(3):170–179. doi: 10.1136/adc.51.3.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toelle B. G., Peat J. K., Salome C. M., Mellis C. M., Woolcock A. J. Toward a definition of asthma for epidemiology. Am Rev Respir Dis. 1992 Sep;146(3):633–637. doi: 10.1164/ajrccm/146.3.633. [DOI] [PubMed] [Google Scholar]
- Weiss K. B., Gergen P. J., Hodgson T. A. An economic evaluation of asthma in the United States. N Engl J Med. 1992 Mar 26;326(13):862–866. doi: 10.1056/NEJM199203263261304. [DOI] [PubMed] [Google Scholar]
- Weiss K. B. Seasonal trends in US asthma hospitalizations and mortality. JAMA. 1990 May 2;263(17):2323–2328. [PubMed] [Google Scholar]
- Yan K., Salome C., Woolcock A. J. Rapid method for measurement of bronchial responsiveness. Thorax. 1983 Oct;38(10):760–765. doi: 10.1136/thx.38.10.760. [DOI] [PMC free article] [PubMed] [Google Scholar]



