Abstract
Hypertension has been suggested to be one possible risk factor of tinnitus, but the association between hypertension and tinnitus remains uncertain. The authors performed a meta-analysis of the existing studies on the association between hypertension and tinnitus. We performed literature search of studies using SinoMed, CNKI, WanFang, PubMed, Scopus, Web of Science, and Google Scholar. Studies reported the odds ratio and 95% confidence interval (CI) (or provided sufficient information for calculation) of the association between hypertension and tinnitus were included. A total of 19 eligible studies with 20 effect estimates were used in this study. They included 63,154 participants with age ranging from 14 to 92. The pooled OR, which was pooled using a random effects model, was 1.37 (95% CI: 1.16 to 1.62). There was no evidence of publication bias (p = 0.11 for Begg's test, p = 0.96 for Egger's test). By meta-regression, we found that study design may be one possible factor of heterogeneity. Sensitivity analysis found that the result was stable. This study suggests that hypertension might be one risk factor of tinnitus, and hypertension prevention and control might be helpful in preventing tinnitus.
1. Introduction
Tinnitus is the perceived sensation of sound in the absence of a corresponding external acoustic stimulus [1]. It is a very bothersome symptom for many patients as it can affect the physical and mental health in different degree. The patients suffering from serious tinnitus may even commit suicide [2].
Hypertension has been suggested as one potential risk factor of tinnitus in some studies, but some other studies showed different results. Thirunavukkarasu and Geetha's retrospective study [3] showed that hypertension and giddiness were high risk factors for the occurrence of tinnitus. Nondahl et al.'s study [4] of ten-year incidence of tinnitus showed that hypertension was not associated with the incidence of tinnitus. Negrila-Mezei et al.'s case-control study [5] based on 471 ear-nose-throat department patients showed that hypertension was significantly associated with tinnitus, but de Moraes Marchiori's case-control study [6] did not find any significant association between hypertension and tinnitus. Some cross-sectional surveys [7, 8] showed that hypertension was a risk of tinnitus, but some other cross-sectional surveys [9, 10] did not find any significant association. It is important to elucidate and quantify the association between hypertension and tinnitus. If the association holds, prevention and control of hypertension should then be included in the prevention measures of tinnitus.
In this study, we provided a meta-analysis of the tinnitus risk associated with hypertension. We also performed a meta-regression to examine possible sources of heterogeneity between the studies and examined the influence of single study on the overall meta-estimate.
2. Methods
2.1. Literature Search
Eligible studies were searched via databases. The databases included SinoMed, CNKI, WanFang, PubMed, Scopus, Web of Science, and Google Scholar. Search strategies used subject headings and key words and did not have language and time restrictions. The presence of tinnitus was defined as answering “yes” to the question “In the past 12 months, have you ever heard a sound (buzzing, hissing, ringing, humming, roaring, machinery noise) originating in your ears?” or similar question in different phrase. Hypertension (high blood pressure) was defined as a systolic blood pressure (SBP) ≥ 140 mmHg or diastolic blood pressure (DBP) ≥ 90 mmHg or reported use of antihypertensive medication [11].
The studies were identified by combining the term “tinnitus” with several terms, such as hypertension, blood pressure, prevalence, risk factors, epidemiology, and characterization, which indicated that the study might provide the relevant information on the association between hypertension and tinnitus, such as OR (odds ratio) and 95% confidence intervals (95% CIs) or relevant information to calculate OR and 95% CIs. We also examined reference lists of the all identified studies and reviewed the cited literatures to identify any other relevant studies.
2.2. Inclusion and Exclusion Criteria
Studies were included in the current meta-analysis if they provided the information to examine the association between hypertension and tinnitus (OR and 95% CIs or relevant data to calculate OR and 95% CIs). Studies which reported one specific type of tinnitus (such as left ear tinnitus and pulsatile tinnitus) were excluded.
2.3. Meta-Analysis
To estimate the quantitative relationship between hypertension and tinnitus, we obtained estimates of the OR and 95% CIs from relevant studies. We used a random-effects model to combine estimates from the identified studies, which allowed between-study heterogeneity to contribute to the variance [12]. We assessed homogeneity of ORs with I 2 value which represented the estimated percent of total variance that could be explained by between-study heterogeneity [13]. Publication bias was assessed using Begg's test [14] and Egger's test [15]. Begg's funnel plot and Egger's publication bias plot were created to provide a visual investigation of possible publication bias. Meta-regression was used to explore whether the inconsistency in results across individual studies could be explained by variations in publication year, region (American and others), sample size, study design (case-control study and cross-sectional study), and confounder adjustment (the sets of potential confounders for which adjustment was made varied by study; we just assessed the difference between studies with adjusted ORs and studies with crude ORs) [16]. We performed both univariate and multivariate meta-regression analysis. Finally, we performed sensitivity analysis to examine the influence of individual studies, in which the meta-analysis estimates were derived by omitting one study at a time. The whole analyses were conducted using STATA software (v12.1).
3. Results
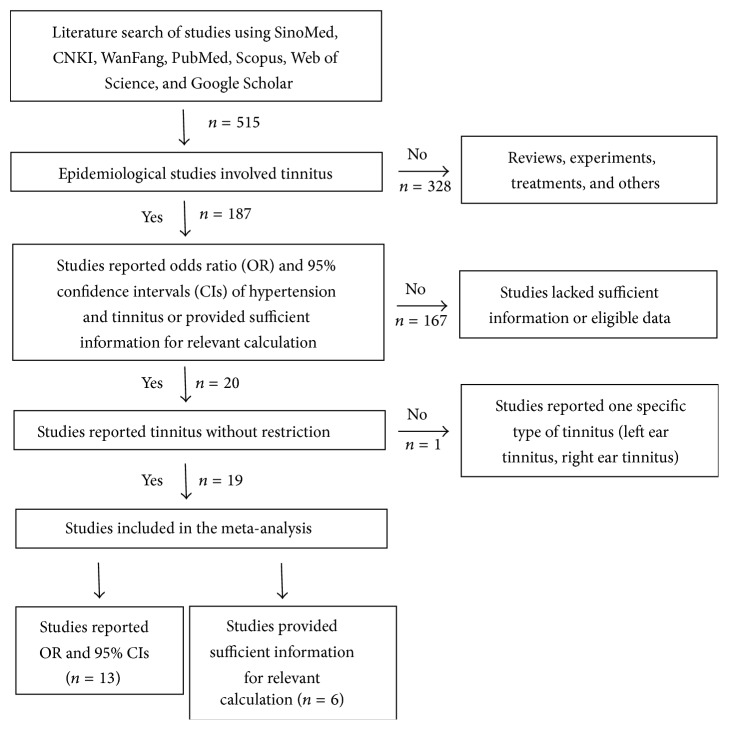
Of a total of 515 studies identified from the search strategy, 187 were epidemiological studies and 328 studies were literature reviews, experimental studies, clinical treatments, or others and were excluded from the analysis. We chose 20 studies reporting OR and 95% CIs of the association between hypertension and tinnitus or providing sufficient data for relevant calculation. Of the 20 studies, one study reported one specific type of tinnitus (left ear tinnitus, right ear tinnitus) and was excluded. Finally, we included a total of 19 studies which provided suitable information for the subsequent analysis (Figure 1).
Figure 1.
Flow diagram on the search process.
We identified 3 case-control studies and 16 cross-sectional studies. Twenty population samples from 19 studies (Fujii et al.'s study [8] provided both men and women information) provided sufficient data for a meta-analysis. Details of the included studies were summarized in Table 1. Overall, this study included 63,154 participants from Italy, South Korea, China, Nigeria, USA, Brazil, Japan, Romania, Turkey, Australian, and Chile, the age of the subjects ranged from 14 to 92 years, sample size of the studies ranged between 120 and 14,178, and OR ranged between 0.73 (95% CI: 0.35 to 1.53) and 12.14 (95% CI: 5.04 to 29.23).
Table 1.
Description of the study populations included in the meta-analysis (n = 63154).
| First author | Year | Country | Study design | Sample size (n) | Age (years) |
|---|---|---|---|---|---|
| Martines [17] | 2015 | Italy | Case-control | 120 | 14–85 |
| Park [18] | 2014 | South Korea | Cross-sectional | 5140 | ≥40 |
| ∗Park [9] | 2014 | South Korea | Cross-sectional | 10061 | 20–97 |
| Chen [19] | 2014 | China | Case-control | 204 | NA |
| Sogebi [20] | 2013 | Nigeria | Cross-sectional | 127 | ≥41 |
| ∗Mahboubi [21] | 2013 | American | Cross-sectional | 3520 | 12–19 |
| ∗Loprinzi [22] | 2013 | American | Cross-sectional | 473 | 70–85 |
| ∗Melo [23] | 2012 | Brazil | Cross-sectional | 498 | ≥60 |
| ∗Fujii [8] | 2011 | Japan | Cross-sectional | 6450 (men) | 45–79 |
| ∗Fujii [8] | 2011 | Japan | Cross-sectional | 7973 (women) | 45–79 |
| ∗Nondahl [24] | 2011 | American | Cross-sectional | 3267 | 21–84 |
| Negrila-Mezei [5] | 2011 | Romania | Case-control | 471 | ≥60 |
| ∗Günay [7] | 2011 | Turkey | Cross-sectional | 879 | 18–64 |
| Shargorodsky [25] | 2010 | American | Cross-sectional | 14178 | NA |
| Michikawa [26] | 2010 | Japan | Cross-sectional | 1286 | ≥65 |
| Gopinath [27] | 2010 | Australian | Cross-sectional | 1214 | NA |
| ∗Lasisi [10] | 2010 | Nigeria | Cross-sectional | 1302 | ≥65 |
| de Moraes Marchiori [6] | 2009 | Brazil | Cross-sectional | 154 | 45–64 |
| Nondahl [28] | 2002 | American | Cross-sectional | 3737 | 48–92 |
| Fasce [29] | 2002 | Chile | Cross-sectional | 2100 | NA |
∗OR was adjusted; NA: not available.
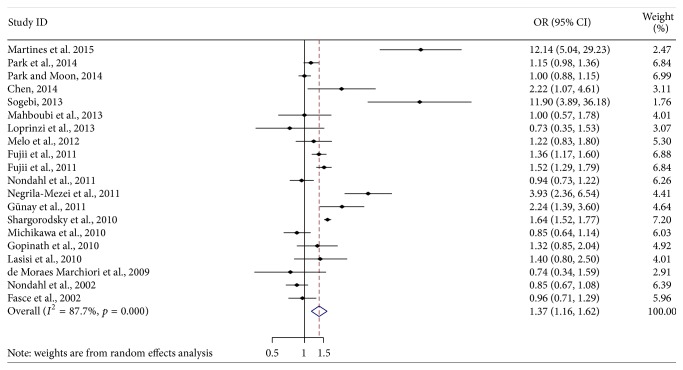
Figure 2 showed the forest plot of 20 effect estimates from 19 studies. Of them, eight studies showed a significant positive association between hypertension and tinnitus. The overall pooled OR was 1.37 (95% CI: 1.16 to 1.62).
Figure 2.
Forest plot of the associations between hypertension and tinnitus (OR and 95% CI indicate odds ratio and 95% confidence interval).
Publication bias was not detected by Begg's test (p = 0.11) (Figure 3) and Egger's test (p = 0.96) (Figure 4). The heterogeneity test was significant (Q = 155.06, p < 0.001, I 2 = 87.7%, and Tau-squared = 0.103). Meta-regression (I 2 = 85.1%, Tau-squared = 0.090, and adjusted R-square = 73.6%) showed that, among various variables, study design was one significant contributor (p = 0.002) (Table 2).
Figure 3.
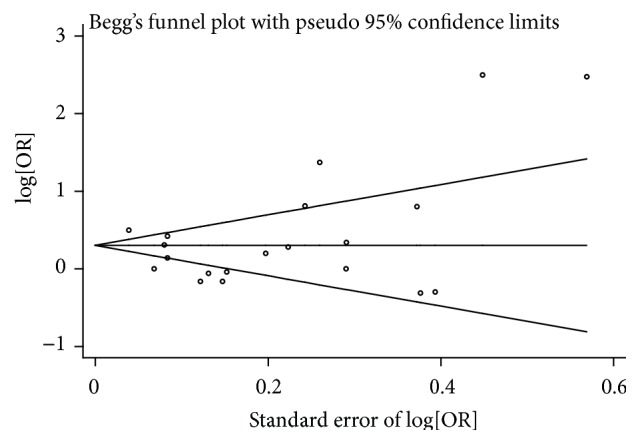
Begg's funnel plot for meta-analysis.
Figure 4.
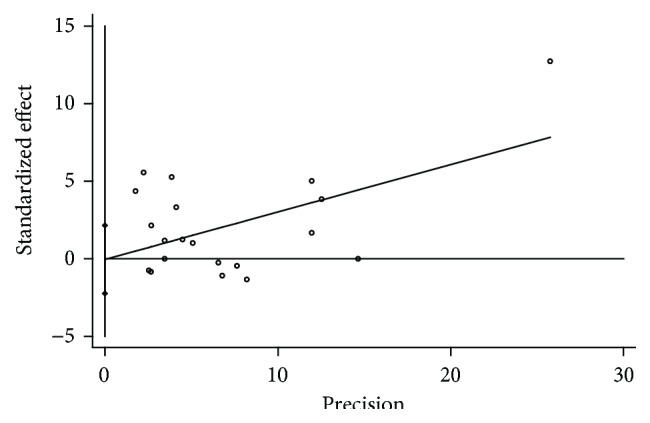
Egger's publication bias plot for meta-analysis.
Table 2.
Parameter estimation of meta-regression.
| Variable | Univariate | Multivariate | ||
|---|---|---|---|---|
| Coefficient | 95% CI | Coefficient | 95% CI | |
| Publication year | 0.07 | (−0.02, 0.16) | 0.04 | (−0.06, 0.13) |
| Region | −0.49 | (−1.23, 0.25) | −0.21 | (−0.86, 0.43) |
| Sample size | −3.46e − 5 | (−12.14e − 5, 5.23e − 5) | 7.06e − 6 | (−6.71e − 5, 8.12e − 5) |
| Study design | 1.28 | (0.54, 2.02) | 1.10 | (0.07, 2.14) |
| Confounder adjustment | 0.34 | (−0.32, 1.01) | 0.10 | (−0.53, 0.73) |
95% CI indicates 95% confidence interval.
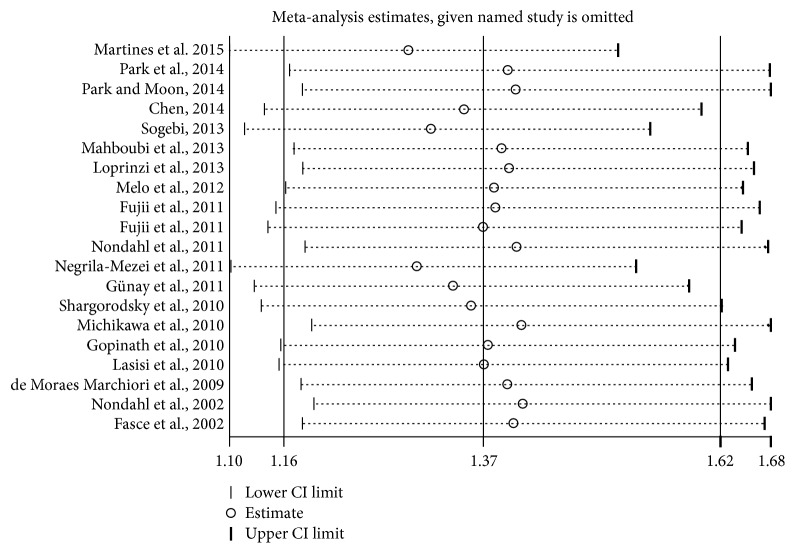
The sensitivity analysis indicated that the omission of any of the studies led to changes in estimates between 1.29 (95% CI: 1.10 to 1.51) and 1.41 (95% CI: 1.19 to 1.68) (Figure 5).
Figure 5.
Sensitivity analysis.
4. Discussion
Tinnitus involves a large proportion of the general population and affects the quality of life and work efficiency. Most of tinnitus prevalence studies in Western Europe and USA have reported prevalence rates between 10% and 15% in the adult population [30]. For example, the largest study (n = 48313), which was undertaken as part of the National Study of Hearing in England, showed a prevalence of 10.1% among adults, with 2.8% of respondents describing it as moderately annoying, 1.6% as severely annoying, and 0.5% at a level severely affecting their normal life [31]. The mechanism of occurrence of tinnitus remains largely unknown; although several treatment strategies for tinnitus patients have been proposed, such as the tinnitus masking technique, pharmacological therapy, and surgery, no single effective cure exists for tinnitus [32]. It is necessary and important to study the risk factors of tinnitus, which will be helpful for formulating specific prevention measures for its prevention. This study provided a quantitative meta-analysis of the association between hypertension and tinnitus. The pooled OR was 1.37 (95% CI: 1.16 to 1.62), which supports that hypertension is significantly associated with tinnitus.
Hypertension has been suggested as one potential risk factor of tinnitus in some studies. There are some studies about hypertension in patients with tinnitus; for example, Nowak et al.'s study [33] included 1200 patients getting treated in the Laryngological Rehabilitation Centre in Poznań due to tinnitus, in the examined group 34% suffered from systemic diseases, and among them the highest percentage (47%) suffered from hypertension; Sogebi's study [20] showed that, among 79 patients having complaints of tinnitus, 15.2% were suffering from hypertension. There are also some studies about tinnitus in patients with hypertension; for instance, Borghi et al.'s study [34] showed that 17.6% patients (aged 18 to 75 years, with uncontrolled hypertension) reported occasional or prolonged spontaneous tinnitus and suggested that systemic blood pressure might have played a prominent role in some tinnitus patients; Chávez-Delgado et al. conducted a cross-sectional study of 385 patients with hypertension, type 2 diabetes mellitus, and dyslipidemia with symptoms of hearing loss, vertigo, and tinnitus; the prevalence of tinnitus was 32% in patients with hypertension [35].
The pathophysiological mechanisms of tinnitus are still not clear. There are several possible mechanisms including increased spontaneous firing rate of neurons in the central auditory system, increased neural synchrony in the firing pattern across neurons in primary auditory cortex, and map reorganisation in the auditory modality [30]. The mechanisms underlying the relationship between hypertension and tinnitus are poorly understood. There are animal experiments [36, 37] indicating that hypertension may induce the occurrence of tinnitus or aggravate preexisting tinnitus through two principle mechanisms, high blood pressure might cause damage to the cochlear microcirculation, and diverse antihypertensive drugs might lead to ototoxicity. Tachibana et al. [37] suggested that the primary target of hypertensive damage in the rat cochlea is the stria vascularis, which feeds the organ of Corti. Przewoźny et al. [38] suggested that the subclinical damage to the stria vascularis includes the decrease in the cochlear oxygen partial pressure and disturbance of the ionic K+ recycling. Borghi et al. [34] suggested that the presence of tinnitus is the consequence of toxic damage of the labyrinth in most patients, which means that the onset of tinnitus might be an adverse event in patients treated with antihypertensive drugs. Another possibility pointed to the fact that when antihypertensive action exceeded the desired effects, subsequent abrupt hypotension would lead to cochlear hypoperfusion and circulatory impairment, which could disturb the sensorineural response, leading to the onset of tinnitus [34]. Clinical evidence also indicated an association between hypertension and tinnitus, which reinforces the hypothesis that alterations in the cochlear microcirculation, as causal or adjuvant factors in tinnitus pathophysiology, occur [39].
There is widespread recognition that consistency between research centers in the ways that patients with tinnitus are assessed and outcomes following interventions are measured would facilitate more effective cooperation and more meaningful evaluations and comparisons of outcomes [40]. But many studies still have methodological drawbacks, especially with production of an unambiguous definition of tinnitus and phrasing of appropriate epidemiological questions, which may be one of the main causes for the heterogeneity in the present study [30]. The other cause for heterogeneity of this research may include socioeconomic condition, ethnic differences, and public health service. Although the meta-analysis detected significant heterogeneity between studies, further sensitivity analyses and the exclusion of publication bias are in favor of a similar effect across the populations.
Hypertension is an important public health concern worldwide. Globally, the overall prevalence of hypertension in adults aged 18 years and over was around 22% in 2014 [41]. Kearney et al.'s study [42] estimated that 29% (about 1.56 billion) of the world's adult population would have hypertension by 2025. Since hypertension is one of the high incidence chronic diseases and has large numbers of patients, we must pay attention to the fact that tinnitus may be caused by hypertension and consider the ototoxicity of drugs for hypertension patients, which means that we may make a choice for hypertension medication to prevent tinnitus.
A few limitations should be noted. First, the included studies for this meta-analysis varied in the degree of controlling for potential confounders, such as age, gender, ethnicity, income, smoking, ear infecting, noise exposure, BMI, anemia, and hearing loss, only a few of the ORs were adjusted, and the adjusted ORs did not adjust for all the same factors. Second, the study design was either cross-sectional or case-control study; therefore it cannot determine temporal sequence and causality [43]. Third, our study did not investigate any causal mechanism of tinnitus and simply did quantitative analysis of the association between hypertension and tinnitus, this association may not be the direct causal role, and further studies are needed.
In conclusion, this meta-analysis suggests that hypertension might be a risk factor of tinnitus and should be considered in its prevention strategy.
Acknowledgment
This research was supported by Science and Technology Program of Guangzhou, China (no. 2014Y2-00511).
Conflict of Interests
The authors have no competing interests regarding the publication of this paper.
References
- 1.Langguth B., Kreuzer P. M., Kleinjung T., De Ridder D. Tinnitus: causes and clinical management. The Lancet Neurology. 2013;12(9):920–930. doi: 10.1016/s1474-4422(13)70160-1. [DOI] [PubMed] [Google Scholar]
- 2.Lewis J. E., Stephens S. D. G., McKenna L. Tinnitus and suicide. Clinical Otolaryngology & Allied Sciences. 1994;19(1):50–54. doi: 10.1111/j.1365-2273.1994.tb01147.x. [DOI] [PubMed] [Google Scholar]
- 3.Thirunavukkarasu K., Geetha C. One-year prevalence and risk factors of tinnitus in older individuals with otological problems. The International Tinnitus Journal. 2013;18(2):175–181. doi: 10.5935/0946-5448.20130023. [DOI] [PubMed] [Google Scholar]
- 4.Nondahl D. M., Cruickshanks K. J., Wiley T. L., et al. The ten-year incidence of tinnitus among older adults. International Journal of Audiology. 2010;49(8):580–585. doi: 10.3109/14992021003753508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Negrila-Mezei A., Enache R., Sarafoleanu C. Tinnitus in elderly population: clinic correlations and impact upon QoL. Journal of Medicine and Life. 2011;4(4):412–416. [PMC free article] [PubMed] [Google Scholar]
- 6.de Moraes Marchiori L. L. Tinnitus complaint and blood hypertension in the aging process. Revista Brasileira de Hipertensão. 2009;16(1):5–8. [Google Scholar]
- 7.Günay O., Borlu A., Horoz D., Gün I. Tinnitus prevalence among the primary care patients in Kayseri, Turkiye. Erciyes Tip Dergisi. 2011;33(1):39–46. [Google Scholar]
- 8.Fujii K., Nagata C., Nakamura K., et al. Prevalence of tinnitus in community-dwelling Japanese adults. Journal of Epidemiology. 2011;21(4):299–304. doi: 10.2188/jea.JE20100124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Park R. J., Moon J. D. Prevalence and risk factors of tinnitus: the Korean National Health and Nutrition Examination Survey 2010-2011, a cross-sectional study. Clinical Otolaryngology. 2014;39(2):89–94. doi: 10.1111/coa.12232. [DOI] [PubMed] [Google Scholar]
- 10.Lasisi A. O., Abiona T., Gureje O. Tinnitus in the elderly: profile, correlates, and impact in the Nigerian study of ageing. Otolaryngology: Head and Neck Surgery. 2010;143(4):510–515. doi: 10.1016/j.otohns.2010.06.817. [DOI] [PubMed] [Google Scholar]
- 11.Tesfaye F., Byass P., Wall S. Population based prevalence of high blood pressure among adults in Addis Ababa: uncovering a silent epidemic. BMC Cardiovascular Disorders. 2009;9(1, article 39) doi: 10.1186/1471-2261-9-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.DerSimonian R., Laird N. Meta-analysis in clinical trials. Controlled Clinical Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 13.Higgins J. P. T., Thompson S. G., Deeks J. J., Altman D. G. Measuring inconsistency in meta-analyses. British Medical Journal. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Begg C. B., Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–1101. doi: 10.2307/2533446. [DOI] [PubMed] [Google Scholar]
- 15.Peters J. L., Sutton A. J., Jones D. R., Abrams K. R., Rushton L. Comparison of two methods to detect publication bias in meta-analysis. Journal of the American Medical Association. 2006;295(6):676–680. doi: 10.1001/jama.295.6.676. [DOI] [PubMed] [Google Scholar]
- 16.Song F., Sheldon T. A., Sutton A. J., Abrams K. R., Jones D. R. Methods for exploring heterogeneity in meta-analysis. Evaluation & the Health Professions. 2001;24(2):126–151. doi: 10.1177/01632780122034849. [DOI] [PubMed] [Google Scholar]
- 17.Martines F., Sireci F., Cannizzaro E., et al. Clinical observations and risk factors for tinnitus in a Sicilian cohort. European Archives of Oto-Rhino-Laryngology. 2015;272(10):2719–2729. doi: 10.1007/s00405-014-3275-0. [DOI] [PubMed] [Google Scholar]
- 18.Park K. H. O., Lee S. H. W., Koo J.-W., et al. Prevalence and associated factors of tinnitus: data from the Korean national health and nutrition examination survey 2009–2011. Journal of Epidemiology. 2014;24(5):417–426. doi: 10.2188/jea.je20140024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen Y. Analysis on Risk Factors of Idiopathic Tinnitus. Shanxi Medical University; 2014. [Google Scholar]
- 20.Sogebi O. A. Characterization of tinnitus in Nigeria. Auris Nasus Larynx. 2013;40(4):356–360. doi: 10.1016/j.anl.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 21.Mahboubi H., Oliaei S., Kiumehr S., Dwabe S., Djalilian H. R. The prevalence and characteristics of tinnitus in the youth population of the United States. The Laryngoscope. 2013;123(8):2001–2008. doi: 10.1002/lary.24015. [DOI] [PubMed] [Google Scholar]
- 22.Loprinzi P. D., Lee H., Gilham B., Cardinal B. J. Association between accelerometer-assessed physical activity and tinnitus, NHANES 2005-2006. Research Quarterly for Exercise and Sport. 2013;84(2):177–185. doi: 10.1080/02701367.2013.784840. [DOI] [PubMed] [Google Scholar]
- 23.Melo J. J., Meneses C. L., Marchiori L. L. D. M. Prevalence of tinnitus in elderly individuals with and without history of occupational noise exposure. International Archives of Otorhinolaryngology. 2012;16(2):222–225. doi: 10.7162/s1809-97772012000200011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nondahl D. M., Cruickshanks K. J., Huang G.-H., et al. Tinnitus and its risk factors in the Beaver Dam Offspring study. International Journal of Audiology. 2011;50(5):313–320. doi: 10.3109/14992027.2010.551220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shargorodsky J., Curhan G. C., Farwell W. R. Prevalence and characteristics of tinnitus among US adults. The American Journal of Medicine. 2010;123(8):711–718. doi: 10.1016/j.amjmed.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 26.Michikawa T., Nishiwaki Y., Kikuchi Y., et al. Prevalence and factors associated with tinnitus: a community-based study of Japanese elders. Journal of Epidemiology. 2010;20(4):271–276. doi: 10.2188/jea.je20090121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gopinath B., McMahon C. M., Rochtchina E., Karpa M. J., Mitchell P. Risk factors and impacts of incident tinnitus in older adults. Annals of Epidemiology. 2010;20(2):129–135. doi: 10.1016/j.annepidem.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 28.Nondahl D. M., Cruickshanks K. J., Wiley T. L., Klein R., Klein B. E. K., Tweed T. S. Prevalence and 5-year incidence of tinnitus among older adults: the epidemiology of hearing loss study. Journal of the American Academy of Audiology. 2002;13(6):323–331. [PubMed] [Google Scholar]
- 29.Fasce E., Flores M., Fasce F. Prevalence of symptoms associated with blood pressure in normal and hypertensive population. Revista Medica de Chile. 2002;130(2):160–166. [PubMed] [Google Scholar]
- 30.Baguley D., McFerran D., Hall D. Tinnitus. The Lancet. 2013;382(9904):1600–1607. doi: 10.1016/s0140-6736(13)60142-7. [DOI] [PubMed] [Google Scholar]
- 31.Davis A., Rafaie E. A. Epidemiology of tinnitus. In: Tyler R. S., editor. Tinnitus Handbook. San Diego, Calif, USA: Singular; 2000. pp. 1–23. [Google Scholar]
- 32.Ahmad N., Seidman M. Tinnitus in the older adult. Drugs & Aging. 2004;21(5):297–305. doi: 10.2165/00002512-200421050-00002. [DOI] [PubMed] [Google Scholar]
- 33.Nowak K., Banaszewski J., Dabrowski P., Szymiec E., Szyfter W. Tinnitus in systemic diseases. Otolaryngologia Polska. 2002;56(2):213–216. [PubMed] [Google Scholar]
- 34.Borghi C., Brandolini C., Prandin M. G., Dormi A., Modugno G. C., Pirodda A. Prevalence of tinnitus in patients withhypertension and the impact of different anti hypertensive drugs on the incidence of tinnitus: a prospective, single-blind, observational study. Current Therapeutic Research. 2005;66(5):420–432. doi: 10.1016/j.curtheres.2005.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chávez-Delgado M. E., Vázquez-Granados I., Rosales-Cortés M., Velasco-Rodríguez V. Cochleovestibular dysfunction in patients with diabetes mellitus, hypertension and dyslipidemia. Acta Otorrinolaringologica Espanola. 2012;63(2):93–101. doi: 10.1016/j.otorri.2011.09.001. [DOI] [PubMed] [Google Scholar]
- 36.Borg E., Moller A. R. Noise and blood pressure: effect of lifelong exposure in the rat. Acta Physiologica Scandinavica. 1978;103(3):340–342. doi: 10.1111/j.1748-1716.1978.tb06223.x. [DOI] [PubMed] [Google Scholar]
- 37.Tachibana M., Yamamichi I., Nakae S., Hirasugi Y., And M. M., Mizukoshi O. The site of involvement of hypertension within the cochlea: a comparative study of normotensive and spontaneously hypertensive rats. Acta Oto-Laryngologica. 1984;97(3-4):257–265. doi: 10.3109/00016488409130987. [DOI] [PubMed] [Google Scholar]
- 38.Przewoźny T., Gójska-Grymajło A., Kwarciany M., Gąsecki D., Narkiewicz K. Hypertension and cochlear hearing loss. Blood Pressure. 2015;24(4):199–205. doi: 10.3109/08037051.2015.1049466. [DOI] [PubMed] [Google Scholar]
- 39.Figueiredo R. R., de Azevedo A. A., de Oliveira Penido N. Tinnitus and arterial hypertension: a systematic review. European Archives of Oto-Rhino-Laryngology. 2015;272(11):3089–3094. doi: 10.1007/s00405-014-3277-y. [DOI] [PubMed] [Google Scholar]
- 40.Langguth B., Goodey R., Azevedo A., et al. Consensus for tinnitus patient assessment and treatment outcome measurement: tinnitus research initiative meeting, regensburg, July 2006. Progress in Brain Research. 2007;166:525–536. doi: 10.1016/s0079-6123(07)66050-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.World Health Organization. Global Status Report on Noncommunicable Diseases 2014. Geneva, Switzerland: World Health Organization; 2014. http://apps.who.int/iris/bitstream/10665/148114/1/9789241564854_eng.pdf. [Google Scholar]
- 42.Kearney P. M., Whelton M., Reynolds K., Muntner P., Whelton P. K., He J. Global burden of hypertension: analysis of worldwide data. The Lancet. 2005;365(9455):217–223. doi: 10.1016/s0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 43.Cappuccio F. P., Taggart F. M., Kandala N.-B., et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31(5):619–626. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]