Abstract
Background:
Today, beside immunization coverage the age appropriate vaccination is another helpful index in public health. Evidences have shown that high immunization coverage rates do not necessarily imply age-appropriate vaccination status. The current study aimed to show the predictive factors of delayed vaccination by survival models.
Methods:
A historical cohort study conducted on 3610 children aged between 24 and 47 months who was living in the suburbs of five big cities of Iran. Time of delay in vaccination of first dose of mumps-measles-rubella (MMR) was calculated from date of vaccination minus age appropriate time according to vaccine card. Kaplan–Maier and Log rank tests were used for comparison the median of delay time. For controlling of confounding variables, multivariate cox model was used and hazard ratio with 95% confidence interval (95%) was reported.
Results:
The mean ± standard deviation and median interquartile range of delay time was 38.34 ± 73.1 and 16 (11–31) days in delayed group. The Log rank test showed that city of living, nationality, parents’ education, and birth order are related with prolonged delay time in MMR vaccination (P < 0.05). Nevertheless, child sex, prior living place (rural or city) and parent's job are not related with delay time of vaccination (P > 0.05). Cox regression showed that city of living, mother education, and nationality are the most predictive factors of delay time duration in MMR vaccination.
Conclusions:
Delay time duration of vaccination increased by faring from capital to the east south. Moreover, concentration of foreign immigrants in big cities and low level of mother education are the most predictors of delayed vaccination. Educational intervention should focus on immigrants and mothers with low education level.
Keywords: Children, delay vaccination, Iran, mumps-measles-rubella, risk factors, survival analysis
INTRODUCTION
Immunization is a proven as one of the most cost effective child survival interventions. It is a public health tools leading to decreased infant and childhood morbidity and mortality from vaccine preventable diseases,[1,2] that are worldwide responsible for three million death in children annually.[3,4] Vaccination coverage is measured worldwide by estimation of the third dose of diphtheria tetanus and pertussis vaccine – DTP-3 and this index has been on an upward trend. So, increasing from 74% in 2000 to a record 85% in 2010.[3] Iran is a developing country and the immunization coverage is higher than 95% based on recent studies.[5,6,7] Moreover, according to our recent study the immunization coverage in children of suburbs of big Iranian cities was as 96.8% fully immunized, 3.2% partially immunized, and 0.1% not immunized.[8] Todays another index is more helpful regarding immunization that considered as age appropriate vaccination.[9,10,11] Available evidence has shown that high immunization coverage rates do not necessarily imply age-appropriate vaccination status.[12]
The implication of delay in receiving of vaccines is that a pool of children with incomplete or no immunization swiftly builds up at appropriate time.[3] Immunization is considered timely when received at the earliest appropriate age, defined as within 7–30 days of the recommended age appropriate.[11,13,14] Although high childhood immunization in the 1st year of life is beneficiary, but it is considerable that children who are not (or are inadequately) immunized are at risk of illness; death, and long-term disability continually due to vaccine preventable diseases until future years of life.[3] High rates of untimely vaccinations reveal inadequate consideration about the immunization program during the vaccination delivery process; and limited recording of immunization on vaccination cards.[3] Recent studies showed that duration of delay in immunization is related to some sociodemographic factors.[12,15,16] The coverage of first dose of mumps-measles-rubella (MMR) is reported by WHO and UNICEF as one of the immunization program monitoring indicators and it is one of the milestones for measles elimination programs by 2015.[17,18] Therefore, due to the high immunization coverage in suburbs of Iranian big cities,[8] the current study aimed to show the delay of immunization in MMR and related factors that were prolonged immunization by survival models.
METHODS
A historical cohort study conducted on the children aged 24–47 months as the target population who are living in the suburbs of five big cities of Iran (Tehran, Esfahan, Arak, Mashhad, and Zahedan) in June 2013. Suburbs areas of each city were defined by local health authorities based on concentration of migrants and some socioeconomic criteria. Immunization history of children was assessed by immunization card plus history of vaccination according to the mother memory.
In each city proportional cluster sampling method was used for selection of eligible children. Clusters were defined as any area highlighted by local health officers owing to lower social class, population density of low health indicators, and high density of migrants. The daily time of delay in vaccination was the first outcome and calculated from date of vaccination minus age appropriate time for each subject. However, only children with vaccination cards were included in the analysis. Regarding to sampling method, 4502 eligible children assessed for immunization status and after excluding children without vaccination card 3610 children were included in analysis. Details of sample size and sampling method explored in our recent study.[8]
Data collection was conducted using a standard instrument that designed according to the questionnaire offered by WHO for the estimation of vaccination coverage.[9] Interviewers were trained university students and data gathering conducted by house-to-house interview method. The questionnaires were completed based on the vaccination card information. The study protocol was approved by the ethical committee of Arak University of Medical Sciences. Moreover, informed consent was filled by each of the study subjects before administration of the questionnaire.
Data analysis
Data analysis was performed using SPSS software (version 18) (Chicago Inc). Descriptive statistics including mean, standard deviation (SD), and median were used. After calculating time of delay for MMR 1, daily delay time used as dependent variable and the mean and median of delay time compared according to the independent variables including child sex, parent's education and job, city, and nationality. Kaplan–Meier and Log rank test was used for comparison the median of delay time. Delay time more than 7 days defined as without timeliness in vaccination and used in Kaplan–Meier for status. For controlling of confounding variables, multivariate cox model was used and hazard ratio (HR) with 95% of confidence interval (95% CI) was reported.
RESULTS
Overall 3610 children included in statistical analysis that 87.7% (3166/3610) were Iranian and 51.3% (1518/3610) were male. The on-time vaccination prevalence (vaccination in <7 days from recommended age) was 68%. The mean ± SD and median interquartile range (IQR) of delay time in on-time group was 2.56 ± 2.18 and 2 (1–4) days, respectively. The mean ± SD and median (IQR) of delay time was 38.34 ± 73.1 and 16 (11–31) days in delayed group.
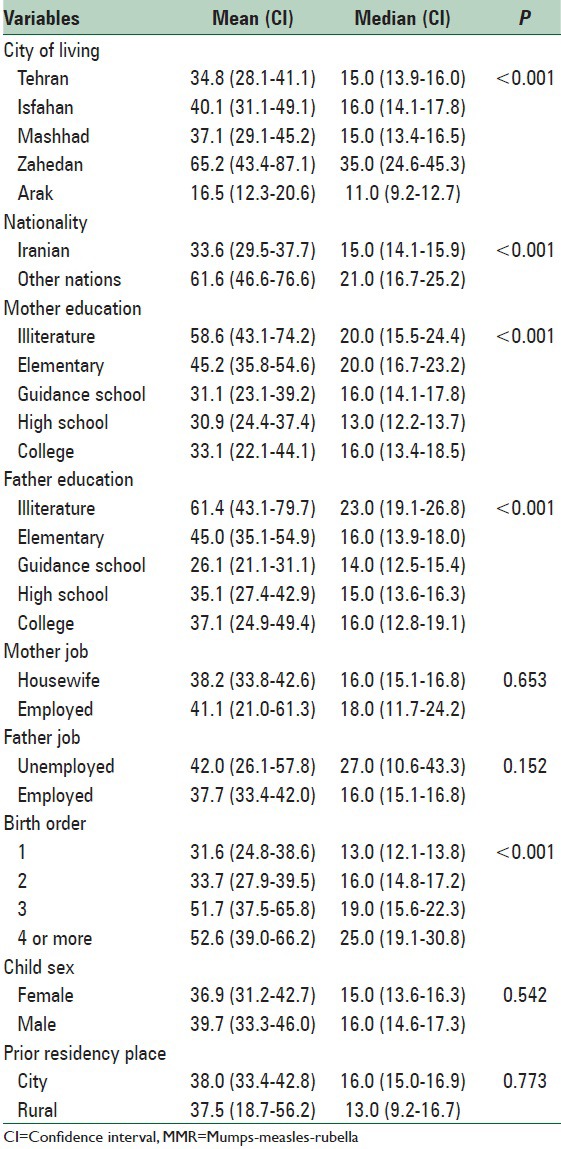
The Log rank test in Kaplan–Maier method showed [Table 1] that city of living, nationality, parents education, and birth order are related with prolonged delay time in MMR vaccination (P < 0.05). However, child sex, prior living place (rural or city), and parent's job are not related with delay time of vaccination (P > 0.05). Pair-wise comparison showed that the median of delay time in Zahedan is more than and in Arak less than other cities (P < 0.001). Also, the median of delay time in Iranian children is less than other nations. Moreover, the delay time duration was decreased with increasing of parent's educations, however increased by birth order of children (P < 0.05).
Table 1.
The mean (95% CI for mean) and median (95% CI for median) for delay time in vaccination of MMR according to city of living, child sex and nationality, parents job, and education level
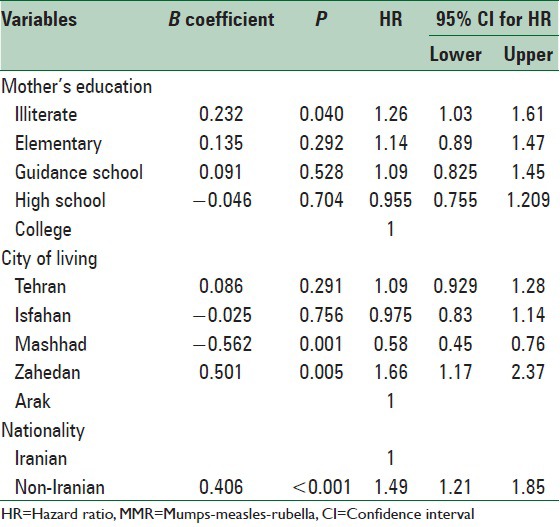
According to Cox regression results [Table 2], after controlling the effect of child sex, birth order, parent's job and education, nationality and city of living, showed that city of living, mother education and nationality are the most predictive factors of delay time duration in MMR vaccination. On the other hand, high education of mother (low school literature) increased the hazard of delay vaccination to 26% (HR: 1.26, CI 95%; 1.03–1.61). Also, living in Zahedan increasing the hazard of delay vaccination to 66% (HR: 1.66, CI 95%; 1.17–2.37) while living in Mashhad decrease this risk to 42% (HR: 0.58, CI 95%; 0.45–0.76). Moreover, non-Iranian children are in 49% higher risk for delay vaccination (HR: 1.49, CI 95%; 1.21–1.85).
Table 2.
The Cox regression results for predictive factors of delay time duration of MMR vaccination
DISCUSSION
The mean and median of delay time of first dose of MMR vaccination in 12-month-year old is very late. Fifty percent of children received the first dose of MMR vaccine with more than 1-month delay approximately. On the other hand, 32% of children immunized against MMR after 7 days of recommended age. Although the immunization coverage in suburbs of big Iranian cities was higher 95%, however, the delay time in these areas is a significant problem.[8] Other studies also showed that the prevalence of delayed vaccination increased by age of infant.[12]
Another studies showed the effect of place and geographic variation on immunization coverage and vaccination delay.[3,19] Also, other studies showed that there are different access to care and inequity in health care utilization.[20,21] However, according to log rank test in Kaplan–Meier analysis, did not observe any significant difference between prior residencies in rural or city areas. This finding suggested that in suburbs of big cities the vaccination delay time duration is higher than who were lived in rural areas, recently. In the cox multivariate analysis declared that city of living is one the important predictive factors for delayed vaccination, Zahedan is placed in east south of Iran and very far from Tehran (the capital of Iran), so, living in Zahedan increased the hazard of delayed vaccination to 66% while living in Mashhad decreased the delayed vaccination to 42%. In another study variation showed among different administrative states.[19] However, the variation due to the state or place of residency may be as different ethnicity and culture.[22] Since, the immigrants in Zahedan are more than other central cities of Iran. Nationality was another significant predictor for delayed vaccination. Non-Iranian children were in higher hazard for delayed immunization. In another study by Pavlopoulou et al. showed that immigrant and foreign ethnicity are predictors of incomplete and delayed administration of all vaccines.[1] This finding approved the different social and cultural aspects of people in studied cities. Due to some legal and political issues the immigrants have less access and less utilized to health care. Moreover, strong geographic differences in health services quality and health outcomes can cause inequity in timely vaccination.[23] So, the delay time of vaccination increase.
Mother education was another significant predictor in cox model. Therefore, mother with low school education are at risk for delayed vaccination for their children. It is showed that levels of education negatively impact health seeking behavior.[2] In another study showed that illiterate mothers are less willing for seeking care than other mothers.[20] However, it seems that the matter of on-time vaccination did not conceptualized by low educated mothers. However, another studies showed the effect of mother education with vaccination delay of coverage.[3,4,24] However, this relationship is not fix in all studies.[22,25] Some studies showed that housewife's children are in more risk for delayed vaccination.[26] However, the association of low education of mothers with untimely vaccination of children can confounded by mother work. Although this relationship did not observe in our study as other studies.[27,28]
This national survey was one of the first studies conducted in suburbs of big Iranian cities regarding timeliness of vaccination. Nevertheless, since the vaccine card of 18% of children was not accessible, it may be the delay time of vaccination has been underestimated. Nevertheless, the goodness of fit of cox model evaluated as good and the precision of hazard ratio estimates were high.
CONCLUSIONS
The median of time delay in first dose of MMR vaccine is more than 1-month. Delay time duration of vaccination increased by faring from capital to the east south. Moreover, concentration of foreign immigrants in big cities and low level of mother education are the most predictors of delayed vaccination. Therefore, increasing the knowledge of families regarding to timely vaccination benefits and protective effect of on-time vaccination is helpful. Especially, educational intervention should be focused on immigrants and mothers with low education level.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Pavlopoulou ID, Michail KA, Samoli E, Tsiftis G, Tsoumakas K. Immunization coverage and predictive factors for complete and age-appropriate vaccination among preschoolers in Athens, Greece: A cross - Sectional study. BMC Public Health. 2013;13:908. doi: 10.1186/1471-2458-13-908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lahariya C. A brief history of vaccines and vaccination in India. Indian J Med Res. 2014;139:491–511. [PMC free article] [PubMed] [Google Scholar]
- 3.Sanou A, Simboro S, Kouyaté B, Dugas M, Graham J, Bibeau G. Assessment of factors associated with complete immunization coverage in children aged 12-23 months: A cross-sectional study in Nouna district, Burkina Faso. BMC Int Health Hum Rights. 2009;9(Suppl 1):S10. doi: 10.1186/1472-698X-9-S1-S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Odusanya OO, Alufohai EF, Meurice FP, Ahonkhai VI. Determinants of vaccination coverage in rural Nigeria. BMC Public Health. 2008;8:381. doi: 10.1186/1471-2458-8-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Esteghamati A, Gouya MM, Zahraei SM, Dadras MN, Rashidi A, Mahoney F. Progress in measles and rubella elimination in Iran. Pediatr Infect Dis J. 2007;26:1137–41. doi: 10.1097/INF.0b013e3181462090. [DOI] [PubMed] [Google Scholar]
- 6.Esteghamati A, Keshtkar AA, Nadjafi L, Gouya MM, Salaramoli M, Roshandel G, et al. Hepatitis B vaccination coverage among Iranian children aged 15-26 months in 2006. East Mediterr Health J. 2011;17:93–100. [PubMed] [Google Scholar]
- 7.Majdzadeh R, Moradi A, Zeraati H, Sepanlou SG, Zamani G, Zonobi V. Evaluation of the measles-rubella mass vaccination campaign in the population covered by Tehran University of Medical Sciences. East Mediterr Health J. 2008;14:810–7. [PubMed] [Google Scholar]
- 8.Zahraei SM, Eshrati B, Gouya MM, Mohammadbeigi A, Kamran A. Is there still an immunity gap in high-level national immunization coverage, Iran? Arch Iran Med. 2014;17:698–701. [PubMed] [Google Scholar]
- 9.Dannetun E, Tegnell A, Hermansson G, Törner A, Giesecke J. Timeliness of MMR vaccination - Influence on vaccination coverage. Vaccine. 2004;22:4228–32. doi: 10.1016/j.vaccine.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 10.Hull BP, McIntyre PB. Timeliness of childhood immunisation in Australia. Vaccine. 2006;24:4403–8. doi: 10.1016/j.vaccine.2006.02.049. [DOI] [PubMed] [Google Scholar]
- 11.Sadoh AE, Eregie CO. Timeliness and completion rate of immunization among Nigerian children attending a clinic-based immunization service. J Health Popul Nutr. 2009;27:391–5. doi: 10.3329/jhpn.v27i3.3381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Poorolajal J, Khazaei S, Kousehlou Z, Bathaei S, Zahiri A. Delayed vaccination and related predictors among infants. Iran J Public Health. 2012;41:65–71. [PMC free article] [PubMed] [Google Scholar]
- 13.Abbott P, Menzies R, Davison J, Moore L, Wang H. Improving immunisation timeliness in Aboriginal children through personalised calendars. BMC Public Health. 2013;13:598. doi: 10.1186/1471-2458-13-598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lernout T, Theeten H, Hens N, Braeckman T, Roelants M, Hoppenbrouwers K, et al. Timeliness of infant vaccination and factors related with delay in Flanders, Belgium. Vaccine. 2014;32:284–9. doi: 10.1016/j.vaccine.2013.10.084. [DOI] [PubMed] [Google Scholar]
- 15.Dombkowski KJ, Lantz PM, Freed GL. Risk factors for delay in age-appropriate vaccination. Public Health Rep. 2004;119:144–55. doi: 10.1177/003335490411900207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rejali M, Mohammadbeigi A, Mokhtari M, Zahraei SM, Eshrati B. Timing and delay in children vaccination; evaluation of expanded program of immunization in outskirt of Iranian cities. J Res Health Sci. 2015;15:54–8. [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention (CDC). Global routine vaccination coverage, 2010. MMWR Morb Mortal Wkly Rep. 2011;60:1520–2. [PubMed] [Google Scholar]
- 18.Perry RT, Gacic-Dobo M, Dabbagh A, Mulders MN, Strebel PM, Okwo-Bele JM, et al. Progress toward regional measles elimination – Worldwide, 2000-2013. MMWR Morb Mortal Wkly Rep. 2014;63:1034–8. [PMC free article] [PubMed] [Google Scholar]
- 19.Mbabazi W, Lako AK, Ngemera D, Laku R, Yehia M, Nshakira N. Maiden immunization coverage survey in the republic of South Sudan: A cross-sectional study providing baselines for future performance measurement. Pan Afr Med J. 2013;16:110. doi: 10.11604/pamj.2013.16.110.3164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hassanzadeh J, Mohammadbeigi A, Eshrati B, Rezaianzadeh A, Rajaeefard A. Determinants of inequity in health care services utilization in markazi province of Iran. Iran Red Crescent Med J. 2013;15:363–70. doi: 10.5812/ircmj.3525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mohammadbeigi A, Hassanzadeh J, Eshrati B, Rezaianzadeh A. Decomposition of inequity determinants of healthcare utilization, Iran. Public Health. 2013;127:661–7. doi: 10.1016/j.puhe.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 22.Ettarh RR, Mutua MK, Kyobutungi C. Ethnicity and delay in measles vaccination in a nairobi slum. Trop Med Health. 2012;40:59–62. doi: 10.2149/tmh.2012-09s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fadnes LT, Jackson D, Engebretsen IM, Zembe W, Sanders D, Sommerfelt H, et al. Vaccination coverage and timeliness in three South African areas: A prospective study. BMC Public Health. 2011;11:404. doi: 10.1186/1471-2458-11-404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fadnes LT, Nankabirwa V, Sommerfelt H, Tylleskär T, Tumwine JK, Engebretsen IM, et al. Is vaccination coverage a good indicator of age-appropriate vaccination. A prospective study from Uganda? Vaccine. 2011;29:3564–70. doi: 10.1016/j.vaccine.2011.02.093. [DOI] [PubMed] [Google Scholar]
- 25.Gidado S, Nguku P, Biya O, Waziri NE, Mohammed A, Nsubuga P, et al. Determinants of routine immunization coverage in Bungudu, Zamfara State, Northern Nigeria, May 2010. Pan Afr Med J. 2014;18(Suppl 1):9. doi: 10.11694/pamj.supp.2014.18.1.4149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wiysonge CS, Uthman OA, Ndumbe PM, Hussey GD. Individual and contextual factors associated with low childhood immunisation coverage in sub-Saharan Africa: A multilevel analysis. PLoS One. 2012;7:e37905. doi: 10.1371/journal.pone.0037905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mathew JL. Inequity in childhood immunization in India: A systematic review. Indian Pediatr. 2012;49:203–23. doi: 10.1007/s13312-012-0063-z. [DOI] [PubMed] [Google Scholar]
- 28.Etana B, Deressa W. Factors associated with complete immunization coverage in children aged 12-23 months in Ambo Woreda, Central Ethiopia. BMC Public Health. 2012;12:566. doi: 10.1186/1471-2458-12-566. [DOI] [PMC free article] [PubMed] [Google Scholar]


