Abstract
Background:
A small proportion of physicians adhere to tuberculosis (TB) notification regulations, particularly in the private sector. In most developing countries, the private sector has dominance over delivering services in big cities. In such circumstances deviation from the TB treatment protocol is frequently happening. This study sought to estimate TB notification in the private sector and settle on determinants of TB notification by private sector physicians.
Methods:
A population-based study has been conducted; private physicians at their clinics were interviewed. The total number of 443 private sectors’ physicians has been chosen by the stratified random sampling method. Appropriate descriptive analysis was used to describe the study's participants. Logistic regression was used for bivariable and multivariable analysis.
Results:
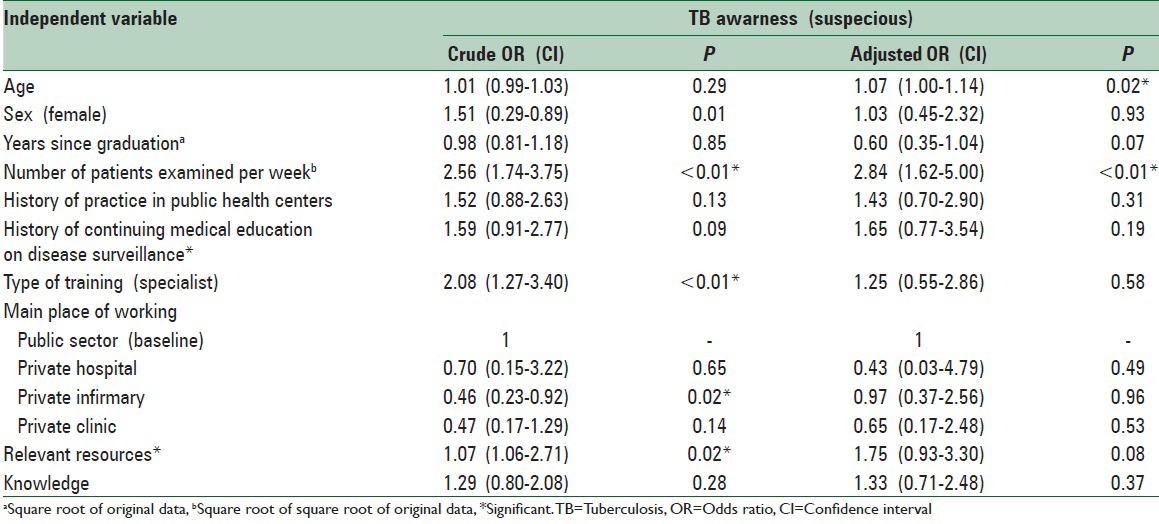
The response rate of the study was 90.06 (399%). Among responders, who had stated that they were suspicious of TB over the recent year, 62 (16.45%) stated that they reported cases of TB at least once during the same period. Having reporting requirements and the number of visited patients was significantly related to TB suspicious (odds ratio = 2.84, confidence interval: 1.62–5, P < 0.01). Workplace and access to relevant resources are associated with TB notification (P < 0.05).
Conclusions:
In poor resource settings with a high burden of TB, the public health administration can promote notification activities in the private sector by simple and quick interventions. It seems that a considerable fraction of private sector physicians, not all of them, will notify TB if they are provided with primary information and primary resources. To optimize the TB notification, however, intersectoral interventions are more likely to be successful.
Keywords: Mandatory reporting, private practice, public health
INTRODUCTION
Components of the stop tuberculosis (TB) strategy steers an array of activities that are mainly performed by national TB programs and surveillance systems.[1] A successful TB surveillance system is trying to detect all new TB patients in a reasonable time and launching the standardized treatment under supervision.[2,3] In doing so, TB surveillance system requires the existence of a reliable “TB notification system” for timely detection and rightly managing the TB patients.[4]
In the passive type of disease surveillance system, physicians are those who first encounter new cases of different diseases, so their reports contribute a considerable extent to the diseases notification system.[5] In most countries reporting notifiable diseases is considered as a lawful duty of medical professions.[3] However, studies conducted in various countries show that a small percentage of physicians feel the obligation toward adherence to disease reporting, and many do not report diseases, even communicable ones. This underreporting is even worse among physicians engaged in the private sector.[3,6,7,8,9,10]
In case of TB, in most resource-poor countries with a high TB-burden, patients with symptoms indicative of TB mostly ask for care from private health-care providers, particularly in big cities. Owing to the greater complexities of the private sector with regards to communications with the surveillance system, problems of early case detection are more palpable in populous settings in poor and middle-income countries.[8,11]
In addition, there are higher incidences of multidrug-resistant-TB in patients diagnosed in the private sector who have not been reported to the surveillance system. In fact, private practitioners are more susceptible to deviate from recommended TB management practices.[2,3,6,11,12,13,14] Furthermore, the low collaboration of the private sector reduce the sensitivity of the surveillance system and owing to the fact that this underestimation is not equally distributed across different sub-groups of the society, detected cases are not representative of total TB cases.[15]
Incidence and prevalence of TB in Iran were last measured at 21 and 32 per 100,000 people, respectively (WHO report).[16] Iran's surveillance system is considering TB as a notifiable disease, though it is in a not urgent manner. In rural areas and county districts with a limited population, most TB cases are registered in the NTP and are receiving standard treatments under supervision. However, a major proportion of TB patients in big cities is under the coverage of the private sector and the TB surveillance system has many problems in early detection and well-accepted managing of such patients.[17,18] It has been shown about 67.5% of Iranian patients prefer to refer to the private sector when they have symptoms indicative of TB and among diagnosed patients. About 70% of positive sputum pulmonary TB patients had chosen private doctor's offices as the primary desired clinical unit. Furthermore, 50% of TB patients had been visited at least twice by physicians prior to the diagnosis of their disease.[19] Despite the fact that private sector is playing a very important role in TB program, their involvement in reporting smear-positive TB is extremely lesser than the public sector.[6] Although it is clear that the rate of TB notification in the private sector is low in urban settings, the determinants of this problem are not evidently cleared. This study aims to estimate the status of TB notification in the private sector and seeks to determine the factors which can potentially have an effect on notifying suspected TB cases by private sector physicians. The result of this study may act as a guide for low-cost and rapid interventions to promote TB notification among physicians engaged in the private sector.
METHODS
Study design and participant
A population-based study was conducted. Based on the density of private section physicians in different municipal divisions, 443 physicians were randomly chosen out of 23,307 physicians whose names were registered in Iran's Medical Council as private engaging physicians. These physicians have been selected from special majorities which were more likely to have met the TB cases (general physicians, pediatrics, infectious disease surveillance, and internists).
Procedure and variable assessment
The data collection tool was a structured questionnaire with closed questions which were designed on the basis of findings of similar studies accomplished by a qualitative study.[18] In addition to demographic data and physician's knowledge about notification for different diseases.[19,20,21] Professional variables such as average number of patients, having any history of working in public sector (past or current),[18] having any history of participation in continuous medical education containing surveillance and notification topics,[22] the main place of doing clinical affairs as a job[17,18,21] and accessibility to some facilities (access to the contact number for reporting, access to the list of reportable diseases and reporting form)[17] were considered as independent variables. As a dependent variable, the participants were also asked whether they had suspected TB in any of their examined patients in a recent year. If physicians had suspected TB, at least one instance of notification within the recent year was considered as their notification history of TB [Figure 1]. The questionnaires were delivered to each physician at their clinics in person. If the physician was absent or the address was wrong, the questioner would visit a substitute predetermined physician. In cases where a physician was not willing to complete the questionnaire, the subject was marked as a case of nonresponse. Physicians were interviewed in their clinics and informed consent was taken verbally. They were assured that their answers would affect them neither professionally nor personally and a present was given to them to compensate for their time allocated to complete the questionnaire. All identification data were kept in the research institute with limited access.
Figure 1.
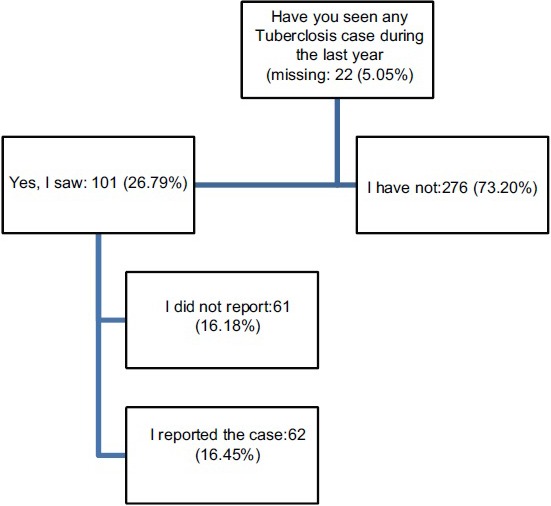
Distribution of physicians’ answers about tuberculosis notification
Statistical analysis
Probable errors in data entry were corrected by double entry method. For assessing crude and adjusted associations among different independent variables and the main outcomes, awareness and notification behavior, bivariable and multivariable logistic regression models, were used, respectively. The significance level was considered at 0.05.
RESULTS
Characteristics of 399 physicians who agreed to participate in the study are illustrated in Table 1 (90.06% response rate). Among nonresponders 37 persons (84.04%) were male and 21 persons (47.73%) were general practitioner while others were specialist (n = 23, 52.27%). The percentage of respondents who were aware of the method of notification of TB was 33.33 (n = 133). Participants were asked their history of notification of other notifiable diseases as well as TB. Notification history of HIV and fever plus rash syndrome were comparable with TB's notification status (HIV: 20.46%, fever plus rash: 29.4%), while it was higher than TB for other diseases (syphilis: 40.63%, animal bites: 60.63%, malaria: 65.62%, swine flu: 85.45%, and AFP: 87.37%). Two hundred seventy-six participants (73.20%) stated that they had not suspected TB within the last year; on the contrary, 101 (26.79%) said that they had. Table 2 illustrates the crude and adjusted relationship between different independent factors and suspecting TB.
Table 1.
Characteristics of study participants
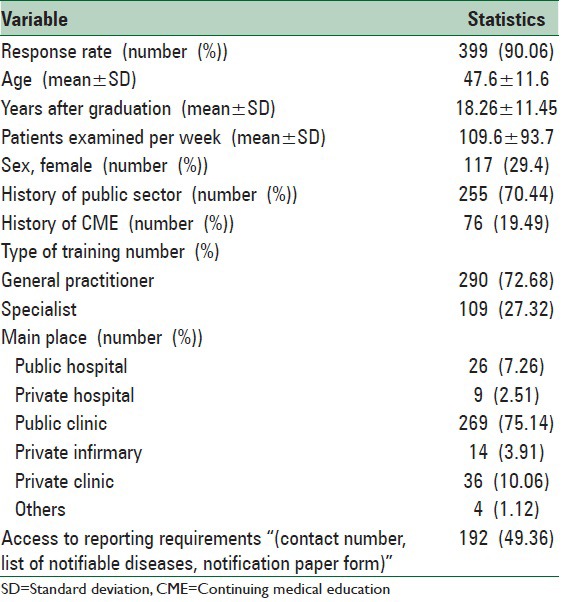
Table 2.
Participants’ characteristic associations with TB awarness (suspecious) in bivariable and multivariable analysis
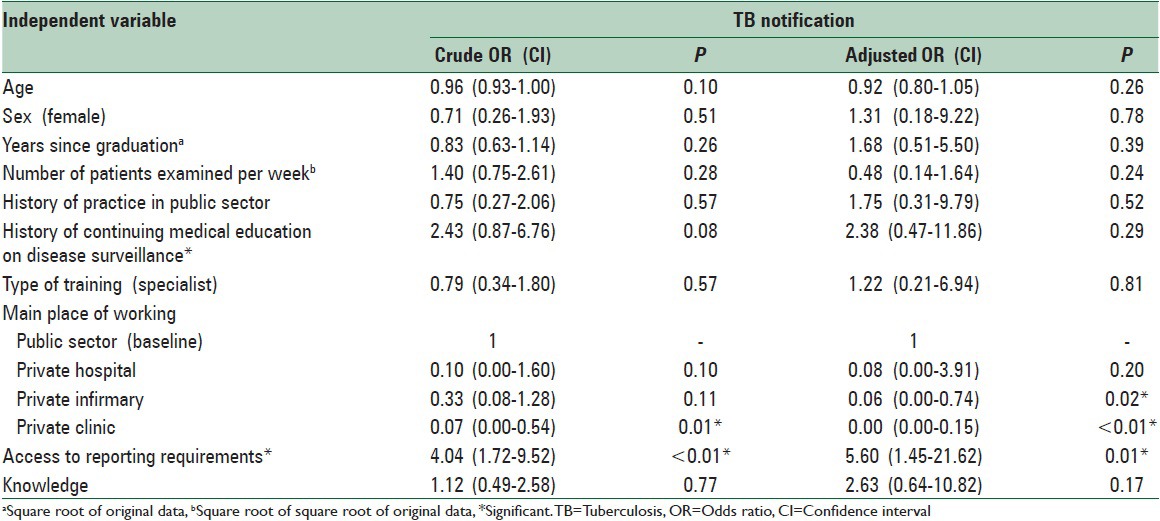
The overall ratio of notifying TB by the study's participants at least once within the recent year was 16.45% (n = 62). This ratio was 61.39% (n = 62) among physicians who had suspected TB (n = 101) [Figure 1]. Table 3 shows the crude and adjusted relationship between independent factors and TB notification among physicians who had suspected TB.
Table 3.
Participants’ characteristic associations with TB notification among physicians suspected to TB, in bivariable and multivariable analysis
DISCUSSION
The ratio of TB notification over a year, among physicians who are engaged in the private sector in Tehran was 16.45%. Although this result is bolding the great deficiency in cooperation of private section physicians with a surveillance system,[6,11] however, it was 61.39% among physicians who suspected to TB in our study. Considering this result, it can be concluded, potentially, that the lack of physician's awareness of TB in their routine practice is an important reason of under notification. Therefore, a great potential improvement in private sector physician's notification might be achieved through making physicians more sensitive, by emphasizing on TB burden and its priority in their region. Despite the fact that there might be many challenges in this conclusion, it seems accessible to a great extent, because regarding the sensitive definition of suspected TB case in Iran's surveillance system, it is expected to much more than 25% of physicians (by considering majorities we included in our study) observe a suspected TB case during a year. In addition, knowing TB notification route is even lesser than most of other diseases which were asked about in this study. It seems that the importance of reporting diseases that have to be notified urgently is more attended by private sector physicians.
Although the effects of demographic variables on notification have been investigated in similar studies, the association between these variables and notification has controversy and cannot be directly interpreted. However, they can be taken into consideration as predisposing factors of notification behavior in physicians.[20,21,22]
In this study, no significant association was observed between the “history of practice in public health centers” and physicians’ notification activities; on the other hand, “history of continuing medical education (CME) about disease surveillance” has an insignificant correlation with TB reporting. However, the recent relationship diminished in multivariable analysis. The absence of follow-up and sustainability programs after the CME courses can be considered as an important reason behind the little influence of the CME on physician's behavior.[22]
There are several solutions which have been put forth by some studies to promote the status of TB notification in the private sector. Among them, training, feedback, managerial interventions, incentives, and financial fines are frequently repeated.[15] The findings of our study, also, show access to the primary tools of TB notification (access to a contact number for notification, list of notifiable diseases, and notification form) is associated with physicians’ TB awareness and also strongly associated with the TB notification. Although, this positive association can result from the availability of notification facilities, the more probable explanation is the effect of communications between surveillance system and private physicians, in which the availability of notification facilities is a consequence of these communications. Such assessments can be greatly influenced by surveillance system units’ activities to draw physicians’ collaboration to the TB notification, along with arranging the required facilities for willing physicians. It is important to put emphasis any solution for attracting private sector physicians for participation in surveillance cannot be solely applied[3] and private physicians must be considered as an active component in an intersectoral collaboration. It is quite appropriate to emphasize, also, that the private sector’ physician are quite deserved to receive feedback from their reported cases, as well as other data providers of the surveillance system.[3,6,7,8,9,10,11,12,14,18]
Limitations
The major limitation of this study measures the behavior (notification) through a self-statement manner that makes the results prone to social desirability bias. Without this bias the notification ratio might be lower than what has been shown in this study.
CONCLUSIONS
With respect to the TB notification, some physicians are considering TB notification as a futile attempt and do not corporate in TB notification. On the other hand, most physicians have a positive view of TB notification, but they might have neither required facilities nor enough motivation to do so. The low ratio of notification among private physicians in urban settings makes the recent group as a suitable target group for implementation of quick and simple interventions, in compare to the first group, whose may need complex interventions. Based on our findings, it seems that access to primary tools of TB notification, such as form and forum of TB reporting can be helpful in achieving a large volume of data on the distribution of TB in big cities. This access can relatively be considered as a quick and cost-effective intervention to identify, almost, a large number of people with symptoms of TB and managing the confirmed cases in a right way to be cured.
ACKNOWLEDGEMENTS
Authors would like to acknowledge Iranian Medical Council, Tehran University of Medical sciences and Iran University of Medical sciences for providing the list of private physicians.
Footnotes
Source of Support: This work was supported by the Tehran University of Medical Sciences under Grant No: 12086-102-04-89 and with the support of the “Knowledge Utilization Research Center”
Conflict of Interest: None declared.
REFERENCES
- 1.Global Tuberculosis Control 2011. World Health Organization. 2012. [Last accessed on 2015 Aug 10]. Available from: http://www.whqlibdoc.who.int/publications/2011/9789241564380_eng.pdf .
- 2.Nagpal M. Tuberculosis Notification: Issues and Challenges. Online J Health Allied Sci. 2013;12:26, 27, 35. [Google Scholar]
- 3.World Health Organization. Tuberculosis services in partnership; The case of Egypt. WHO-EM/TUB/243/E. Eastern Mediterranean Region/Royal Tropical Institute. 2004 [Google Scholar]
- 4.Huaman MA, Araujo-Castillo RV, Soto G, Neyra JM, Quispe JA, Fernandez MF, et al. Impact of two interventions on timeliness and data quality of an electronic disease surveillance system in a resource limited setting (Peru): A prospective evaluation. BMC Med Inform Decis Mak. 2009;9:16. doi: 10.1186/1472-6947-9-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sadrizadeh B. Communicable Disease control programs in the eastern mediterra-nean region of the World Health Organization. Arch Iran Med. 1999;2:28–37. [Google Scholar]
- 6.Hassan Zadeh J, Nasehi M, Rezaianzadeh A, Tabatabaee H, Rajaeifard A, Ghaderi E. Pattern of reported tuberculosis in Iran 2009-2010. Iran J Public Health. 2013;42:72–8. [PMC free article] [PubMed] [Google Scholar]
- 7.Allen CJ, Ferson MJ. Notification of infectious diseases by general practitioners: A quantitative and qualitative study. Med J Aust. 2000;172:325–8. doi: 10.5694/j.1326-5377.2000.tb123979.x. [DOI] [PubMed] [Google Scholar]
- 8.Pethani A, Zafar M, Khan AA, Rabbani Sana U, Ahmed S, Fatmi Z. Engaging general practitioners in public-private mix tuberculosis DOTS program in an urban area in Pakistan: Need for context-specific approach. Asia Pac J Public Health. 2015;27:NP984–92. doi: 10.1177/1010539513483828. [DOI] [PubMed] [Google Scholar]
- 9.Uplekar M, Pathania V, Raviglione M. Private practitioners and public health: Weak links in tuberculosis control. Lancet. 2001;358:912–6. doi: 10.1016/S0140-6736(01)06076-7. [DOI] [PubMed] [Google Scholar]
- 10.Wells WA, Ge CF, Patel N, Oh T, Gardiner E, Kimerling ME. Size and usage patterns of private TB drug markets in the high burden countries. PLoS One. 2011;6:e18964. doi: 10.1371/journal.pone.0018964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Global Tuberculosis Report 2013. World Health Organization. [Last accessed on 2015 Aug 10]. Available from: http://www.apps.who.int/iris/bitstream/10665/91355/1/9789241564656_eng.pdf .
- 12.Lönnroth K, Thuong LM, Linh PD, Diwan VK. Utilization of private and public health-care providers for tuberculosis symptoms in Ho Chi Minh City, Vietnam. Health Policy Plan. 2001;16:47–54. doi: 10.1093/heapol/16.1.47. [DOI] [PubMed] [Google Scholar]
- 13.Singla N, Sharma PP, Singla R, Jain RC. Survey of knowledge, attitudes and practices for tuberculosis among general practitioners in Delhi, India. Int J Tuberc Lung Dis. 1998;2:384–9. [PubMed] [Google Scholar]
- 14.Khan AJ, Khowaja S, Khan FS, Qazi F, Lotia I, Habib A, et al. Engaging the private sector to increase tuberculosis case detection: An impact evaluation study. Lancet Infect Dis. 2012;12:608–16. doi: 10.1016/S1473-3099(12)70116-0. [DOI] [PubMed] [Google Scholar]
- 15.Doyle TJ, Glynn MK, Groseclose SL. Completeness of notifiable infectious disease reporting in the United States: An analytical literature review. Am J Epidemiol. 2002;155:866–74. doi: 10.1093/aje/155.9.866. [DOI] [PubMed] [Google Scholar]
- 16.Global Tuberculosis Report 2014. World Health Organization. [Last accessed on 2015 Aug 10]. Available from: http://www.who.int/countries/irn/en/
- 17.Nader F, Askarian M. How do Iranian physicians report notifiable diseases?. The first report from Iran. Am J Infect Control. 2009;37:500–4. doi: 10.1016/j.ajic.2008.09.014. [DOI] [PubMed] [Google Scholar]
- 18.Ahmadi A, Nedjat S, Gholami J, Majdzadeh R. Disease surveillance and private sector in the metropolitans: A troublesome collaboration. Int J Prev Med. 2013;4:1036–44. [PMC free article] [PubMed] [Google Scholar]
- 19.Geneva: World Health Organization; 2006. [Last accessed on 2015 Aug 10]. World Health Organization. Diagnostic and Treatment Delay in Tuberculosis; p. 23. Available from: http://www.applications.emro.who.int/dsaf/dsa710.pdf . [Google Scholar]
- 20.Ofili AN, Ugwu EN, Ziregbe A, Richards R, Salami S. Knowledge of disease notification among doctors in government hospitals in Benin City, Edo State, Nigeria. Public Health. 2003;117:214–7. doi: 10.1016/S0033-3506(02)00021-5. [DOI] [PubMed] [Google Scholar]
- 21.Gauci C, Gilles H, O’Brien S, Mamo J, Calleja N. General practitioners role in the notification of communicable diseases-study in Malta. Euro Surveill. 2007;12:E5–6. doi: 10.2807/esm.12.11.00745-en. [DOI] [PubMed] [Google Scholar]
- 22.Davis D, O’Brien MA, Freemantle N, Wolf FM, Mazmanian P, Taylor-Vaisey A. Impact of formal continuing medical education: Do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA. 1999;282:867–74. doi: 10.1001/jama.282.9.867. [DOI] [PubMed] [Google Scholar]


