Abstract
Background
The global burden of cardiovascular mortality is increasing, as is the number of large-scale humanitarian emergencies. The interaction between these phenomena is not well understood. This review aims to clarify the relationship between humanitarian emergencies and cardiovascular morbidity and mortality.
Methods
With assistance from a research librarian, electronic databases (PubMed, Scopus, CINAHL, Global Health) were searched in January 2014. Findings were supplemented by reviewing citations of included trials. Observational studies reporting the effect of natural disasters and conflict events on cardiovascular morbidity and mortality in adults since 1997 were included. Studies without a comparison group were not included. Double-data extraction was utilized to abstract information on acute coronary syndrome (ACS), acute decompensated heart failure (ADHF), and cardiac death (SCD). Review Manager 5.0 was used to create figures for qualitative synthesis (Version 5.2, Copenhagen Denmark, The Nordic Cochrane Centre).
Results
The search retrieved 1697 unique records; 24 studies were included (17 studies of natural disasters, 7 studies of conflict). These studies involved 14,583 cardiac events. All studies utilized retrospective designs: 4 were population-based, 15 were single-center, and 5 were multicenter studies. 23 studies utilized historical controls in the primary analysis, and 1 utilized primarily geographical controls. Conflicts are associated with an increase in long-term morbidity from ACS; the short-term effects of conflict vary by study. Natural disasters exhibit heterogeneous effects including increased occurrence of ACS, ADHF, and SCD.
Conclusions
In certain settings, humanitarian emergencies are associated with increased cardiac morbidity and mortality that may persist for years following the event. Humanitarian aid organizations should consider morbidity from non-communicable disease when planning relief and recuperation projects.
Introduction
In the last century, non-communicable diseases have become a leading cause of morbidity and mortality worldwide; ischemic heart disease (IHD) is the world’s leading cause of death.1 This increased burden of non-communicable disease alters the vulnerability of populations to disaster as persons with chronic disease may be more greatly impacted by disruptions to the healthcare system that result from large-scale emergencies.2 In addition to direct injury from disaster events, affected persons are at risk of communicable disease, malnutrition, and exacerbations of underlying disease. There is a growing body of evidence to suggest that the acute stress of these events may trigger cardiac events as well.3 Chronic stressors such as low socioeconomic status, work stress, and depression have been associated with increased IHD;3 acute stressors such as sporting events, earthquakes, and war have all been associated with acute coronary syndrome.4. 5. 6 Increased arrhythmia, blood pressure lability, coagulopathy, and sympathetic dysregulation have been posited as mediating factors in this phenomenon.3
This review aims to clarify the relationship between humanitarian emergencies and cardiovascular morbidity and mortality. Specifically, this review seeks to quantify the effect of natural and man-made disasters on the prevalence of acute coronary syndrome (ACS), acute decompensated heart failure (ADHF), and sudden cardiac death (SCD).
Methods
The full protocol for this review has been published in the PROSPERO International prospective register of systematic reviews (Registration number CRD420140007056).
PubMed, Scopus, CINAHL, and Global Health databases were searched in January 2014 using two main concepts; humanitarian emergencies and cardiovascular morbidity and mortality. The search terms utilized are listed in Appendix 1. The bibliographies of included studies were manually reviewed to identify studies missed using our initial search strategy.
Inclusion criteria were as follows:
Reports of adult patients directly affected by humanitarian emergency, including natural disaster (e.g. hurricane, tornado) and/or conflict (e.g. war, acts of terror)
Reported outcomes occurring within 5 years of the disaster event, with some cases occurring in the first year after the event
At least one of: ACS, ADHF, SCD quantified in the study
Observational studies with a comparison population (historical or geographic)
Reports in all languages published after 1997
Exclusion criteria:
As this review sought to quantify changes in the population prevalence of cardiac events following disasters, studies of subsets of patients not representative of the entire population, such as those with implantable cardiac devices, were excluded
Reports of occupational emergencies not triggered by a natural disaster
Geographically remote exposure, such that those studied were unlikely to have been injured by the disaster or incurred damage to their residence as a result of the disaster
Exposures greater than five years prior to the initial outcome measurements
No comparison population
Two investigators independently reviewed all titles and abstracts for studies that met the inclusion criteria, and two investigators reviewed all potentially relevant full text reports. A modified version of the Newcastle-Ottawa Scale was used to assess the risk of bias in studies.7
The numbers of admissions for ACS, ADHF, and SCD (as defined by the study authors), as well as corresponding odds ratios or relative risks, were abstracted for each study and input into Review Manager 5.0 (Version 5.2, Copenhagen Denmark, Nordic Cochrane Centre).8 Admissions for ACS included unstable angina (UA), ST-segment myocardial infarction (STEMI), and non-ST segment myocardial infarction (NSTEMI). When reported separately by the authors, these values were pooled to obtain totals. Admissions for chest pain that did not result in a diagnosis of ACS were excluded. When only graphical data was presented in the published study, authors were contacted to obtain numerical results. If authors did not respond within two weeks, numerical results were estimated from graphs using freely available software.
A summary ratio of events in the exposed vs. unexposed (control) periods was calculated for each study. If the authors did not provide measures of variance, the standard error was estimated using Poisson assumptions for the purposes of visual representation in Forest plots. Our unit of analysis was number of events. These studies were clinically and methodologically heterogeneous. In an exploratory analysis of statistical heterogeneity, I2 measure of heterogeneity ranged from 50–80%. Given the marked heterogeneity between studies, only a qualitative synthesis of results has been provided.
Results
Study selection
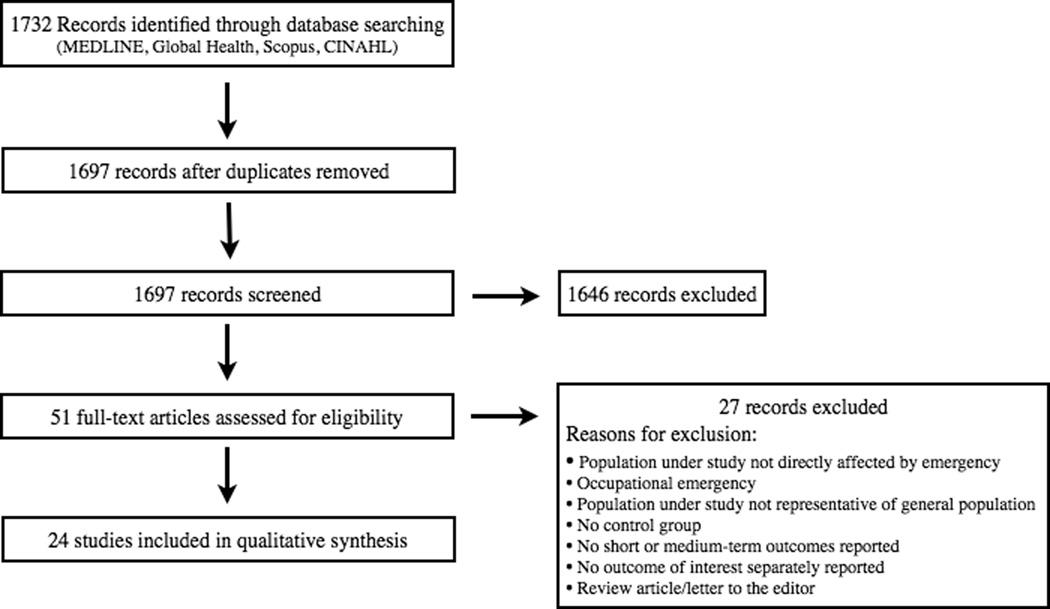
In total, 1732 records were identified through database searching, 1697 of which remained after duplicates were excluded. 51 studies were assessed in full text for eligibility, 24 of which were included in the final review. Backward citation screening of included papers identified no further relevant studies. A PRISMA flow diagram is provided in Figure 1.
Figure 1.
PRISMA Flow Diagram
Of the 24 included studies, 7 reported on conflict events, and the remainder reported findings following natural disasters. A detailed summary of the patient and exposure characteristics of included studies is provided in Tables 1a and 1b.
Studies of conflict events
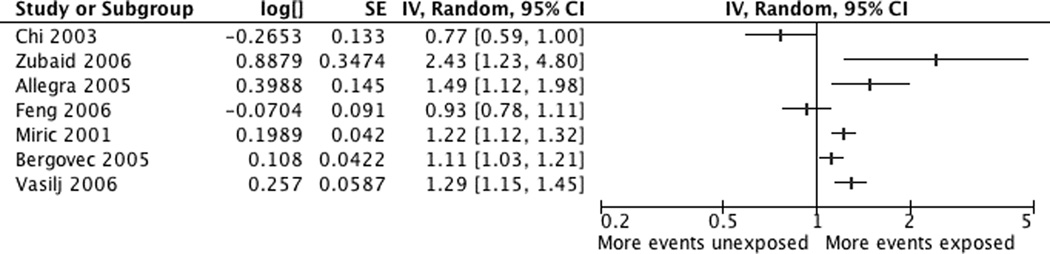
4 studies report on the rates of myocardial infarction (AMI) during active conflict compared to periods of relative stability.6, 9–11 One study reported the acute effects of air raids in Kuwait on AMI, finding that the incidence of admission for AMI increased during the first 5 days of attacks (IRR 2.43; 95% CI 1.23–4.26).11 3 studies identified a long-term increase in ACS in prolonged conflict settings.6, 9, 10 Studying 3,454 consecutive admissions for ACS over a 9-year period including the Middle Dalmatia War, Miric et. al. found that significantly more patients were admitted with ACS in the three-year period during the war than the preceding 3-year period (1,257 vs. 1,024 patients, p<0.05).10 Two separate studies also found a statistically significant increase in the number of patients with wartime ACS in Bosnia and Herzegovina compared to the pre-war period.6, 9 A summary of the estimated effect of each conflict event is provided in Figure 2, with results ordered by length of follow-up.
Figure 2.
Incidence rate ratio for ACS following conflict exposure (Ordered by length of study period)
3 included studies report on the effects of the September 11th terrorist attacks on the World Trade Center.12–15 A study of coronary care unit admissions at 8 centers in New York City did not find a significant change in the number of admissions for ACS, ADHF, or chest pain in the week following the attacks.12 Two studies examined outcomes to 60-days; a study of 16 hospitals in New Jersey found a 49% increase (p=0.01) in the incidence of AMI in the 60 days following the event (42% when the number of patients presenting to the ED was controlled for).14 A study of admissions to the telemetry and coronary care units at a single center in Brooklyn also identified an increase in the overall occurrence of cardiac events in the post-exposure period compared to the corresponding period in 2010 (p=0.008).13 Interestingly, the incidence of AMI and tachyarrhythmia was increased following the event, however, the incidence of admission for unstable angina did not change.
Studies of natural disasters
Seventeen relevant studies on cardiovascular morbidity and mortality following natural disasters were identified, reporting on a variety of cardiac outcomes with widely varying follow-up.
Acute coronary syndrome
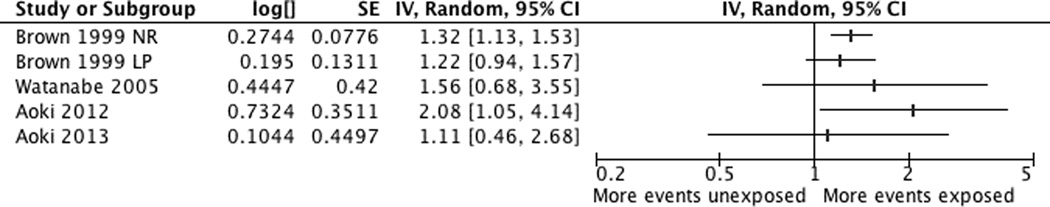
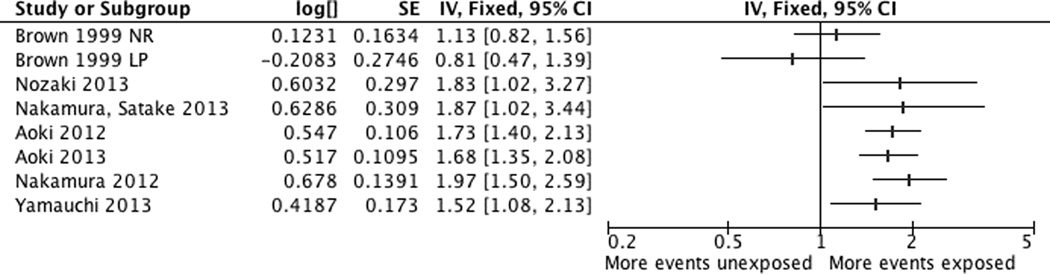
Four studies provide data on the change in acute coronary syndrome incidence in the first week following 4 different earthquakes.5, 16–18 Brown and colleagues have described the cardiac sequelae of two different events in California, the 1989 Lomo Prieta earthquake and the 1994 Northridge earthquake.16 An increase in AMI admissions on the day of the Northridge (RR 1.83; 95% CI 1.29–2.59), but not the Loma Prieta event (RR 0.96, 0.55–1.67), was identified.16 At one week after the event, there was again an increase in events in the Northridge, but not the Loma Prieta population. Following the 2004 Niigata, Japan earthquakes, a study of 8 hospitals noted an increase in cases of ACS, however, it was not statistically significant.17 Similarly, studies of ACS incidence diagnosed in the ER and by cardiologists identified only a non-significant trend toward increased ACS admissions in the week immediately following the earthquake.5, 18 The first-week trend in ACS admissions is summarized in Figure 3.
Figure 3.
Incidence rate ratio for ACS in the first week following natural disaster
One study reported the incidence of ACS during the 2-week period following two earthquakes in Christchurch.19 The September 10th earthquake, magnitude 7.1, occurred at 4:36 am, while the Feb 2011 event occurred around noon and had a lesser magnitude of 6.3. ST-elevation myocardial infarction (STEMI) increased following the September event (p=0.016), but not following the February event.
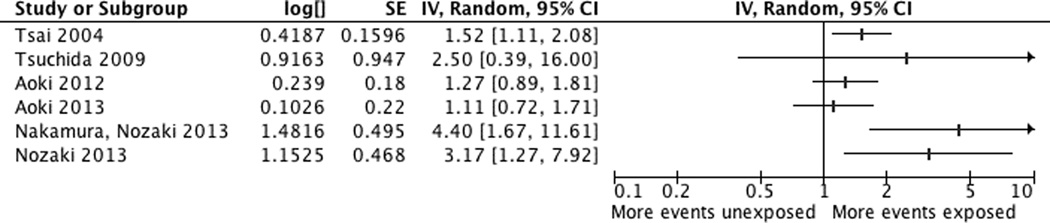
Six studies report on the incidence of acute coronary syndrome in the period 1–2 months following a natural disaster.5, 18, 20–23 In a study of 6 counties in Taiwan, there was a significant increase in AMI incidence during the 6-week period following the 1999 Ji-Ji earthquake (99 admissions vs. 65 admissions, p=0.009).20 A rural hospital-based study of ACS incidence following the 2007 Noto Peninsula earthquake also found an increase in ACS events compared with corresponding historical averages (5 vs. 2, p<0.01).21 Four studies describe the effects of the Great East Japan Earthquake. Using ER records, Nozaki noted a significant increase in the number of patients with ACS in the three-week period following the earthquake, compared with historical controls (n=19 vs. n=7 in 2009, n=5 in 2010, p=0.004).22 Hospital admission data on the same subset of patients yielded similar results (odds ratio for AMI 4.40, 1.01–18.35).23 Likewise, a study of ACS presentations to the ER5 and cardiology admissions18 found a weekly increase in the number of patients presenting to the ER with ACS in the two weeks following the event that did not persist beyond that time. A forest plot of these findings is provided in Figure 4.
Figure 4.
Incidence rate ratio for ACS 3-8 weeks following natural disaster
Two included studies describe the long-term effects of Hurricane Katrina on ACS presentations several years following the hurricane.24, 25 A single-center study found a 3-fold increased incidence in the proportion of admissions for AMI in the 2 years following Katrina (2.18% vs. 0.71%, p<0.0001), and also noted that the post-Katrina group had higher rates of unemployment, lack of insurance, medication non-compliance, smoking, and substance abuse. The expected trends in circadian variation of AMI onset were also altered in the post-Katrina period.25
Acute decompensated heart failure
Following the Northridge and Loma Prieta earthquakes, there was no difference in the daily admission rate for ADHF in the 7 days before, the day of, or 6 days following the event for either quake.16 The studies of ADHF following the great East Japan Earthquake had longer follow-up and consistently identified an increase in ADHF.5, 18, 22, 26–28 Nozaki and colleagues identified an increase in ER visits for ADHF during the 3-week period after the earthquake compared with the same periods in 2009 and 2010 (32 in 2011 vs. 16 in 2009, 19 in 2010, P=0.039).22 Aoki et. al. found an increase in ADHF admissions that persisted for 6 weeks following the event.5, 18 When compared with the pre-disaster group, patients admitted in the post-disaster period were also more likely to be older than 75 (OR 1.89, 1.12–3.19).18
A study of the tsunami-hit area following the Great East Japan Earthquake found a relative risk of ADHF admission of 1.97 (1.50–2.59) in the tsunami area, compared with a relatively unaffected control region. Admissions for ADHF peaked 3–4 weeks following the event and then gradually returned to baseline over the remainder of the 12-week period studied.27 Compared with patients admitted in the pre-disaster period, patients admitted during the first 3 weeks following the event were also less likely to have a history of admission for ADHF, more likely to have hypertension, and more likely to have atrial fibrillation.26 At Fukishima Medical University, 84 patients were admitted with ADHF in the 6 months following the event, compared with 55 in the control period.28 Patients admitted in the post-disaster period were also older (p=0.031), more hypertensive (p=0.0039), had a greater incidence of incident ADHF due to valvular disease (p=0.040), and were more likely to have interrupted their drugs prior to admission (p=0.001).28 A summary of findings is provided in Figure 5.
Figure 5.
Incidence rate ratio for Acute Decompensated Heart Failure following natural disaster (ordered by length of study period)
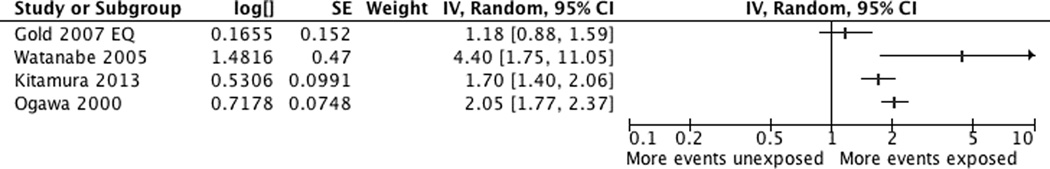
Sudden cardiac death
Four studies report on sudden cardiac death following natural disasters.15, 17, 29, 30 In the 48 hours following the 2001 Nisqually Earthquake there were 32 SCDs, compared with an average of 22 in control periods (p=0.02).15 There was no statistically significant difference at the one-week point after the event. Following the 2004 Niigata Earthquake, there was increase in the daily median of SCD in the week following the event (daily median = 3 in week following event, compared to 0.5 in 2003, 0 in 2002), but no statistically significant increase beyond that period.17 Kitamura and colleagues used Poisson modeling to examine trends in out-of-hospital cardiac arrest (OHCA) of presumed cardiac origin in the 8-week period following the Great East Japan Earthquake.29 The risk of OHCA was increased for the first 4 weeks following the earthquake [Week 1 RR 1.70 (1.40–2.07), Week 2 1.48 (1.21–1.81) Week 3 1.47 (1.20–1.82), Week 4 1.26 (1.02–1.54), Week 5 and onwards did not reach statistical significance)]. This is in keeping with a previous study that identified increased mortality attributable to AMI that persisted for 8 weeks following the 1995 Great Hanshin-Awaji Earthquake.30 The highest standardized mortality ratio for AMI death was in the first week (SMR 8.4, p<0.05); overall, there were 546 deaths attributable to AMI in the earthquake year, compared to 266 in the control period. A summary of findings is provided in Figure 6.
Figure 6.
Incidence rate ratio for death of presumed cardiac origin (Ordered by length of study period)
Risk of bias within studies
A modified version of the Newcastle-Ottawa Score for Cohort Studies was used to assess the risk of bias in individual studies.31 Three main domains were assessed: selection of the exposed and unexposed populations, ascertainment of exposure and outcome, and comparability of the groups. A summary of the risk of bias assessment for individual studies is presented in Table 2.
9 of 24 studies utilized single-center data from hospitalized inpatients; these studies may not be representative of the regional population, particularly in regions where health costs are prohibitive or if transportation patterns were restricted in the aftermath of the event.10, 12, 13, 18, 19, 21, 23, 26, 28 This is particularly apparent when considering studies of the September 11th terrorist attacks since many patients did not report to work in Manhattan in the weeks after the event, altering the daily hospitalization patterns of patients both in the city and in the surrounding areas.12–14 As almost all studies utilized historical controls from the previous year, the comparison population was generally similar to the exposed population. Comparability of the groups was not always well reported, and was particularly concerning for the three studies describing the effects of long-term conflict on the population.6, 9. 10 While the authors included only patients who resided in the affected area for the duration of the conflict, population change due to emigration and demographic change due to military recruitment remain strongly possible and could bias the results.
Risk of bias across studies
Publication bias may have contributed to the findings of this review, as studies reporting no change in the rate of cardiac events following a disaster may be less likely to be published. This is particularly true for studies of heart failure and sudden cardiac death, as these are less well-established phenomena than the change in ACS risk following a disaster. Many of these studies also report on a small subset of disaster events; of 24 studies, 8 report on the Great East Japan Earthquake alone.5, 18, 22, 23, 26–29 Several of the Japanese studies report on emergency department admissions and cardiac care unit admissions in the same population of patients in sequential papers.5, 18, 22, 23, 26 Studies reporting on AMI, ADHF, and/or SCD among the same population in separate papers may have included overlapping subsets of patients, thus these results also cannot be interpreted independently of one another.22, 23, 26, 27 Non-English studies may not have been identified by our search strategy, and may have yielded different results.
Discussion
Overall, studies of cardiac disease in conflict settings consistently find an increase in admissions for acute myocardial infarction in the period months to years following the stressor. The studies reporting on short-term effects have disparate findings, with a clear increase in AMI in the population already under wartime stress but a weaker correlation in the American population affected by the September 11th attacks. It is possible that the acute-on-chronic stressor had a different physiologic effect in the Kuwaiti population studied, however, it is also possible that the methodological limitations discussed earlier biased the results of the New York studies, since changes in hospital utilization in the immediate aftermath of the attacks may have altered the admission patterns at hospitals studied.
Altered patterns of ACS admission also varied among the studies of natural disasters. Early morbidity from ACS is likely predominantly attributable to the psychological stress of the event and corresponding physiologic derangements. Some of this derangement is due to sympathetic dysregulation, as demonstrated by altered patterns of heart rate variability and increased tachyarrhythmia in patients undergoing Holter and ICD monitoring during earthquakes.32, 33 Hypertension and hypercoagulability likely also play a role in pathogenesis.34
AMI incidence is known to correlate with time of day; findings of this review are consistent with the hypothesis that earthquakes occurring in the early morning hours are more closely correlated with increased ACS morbidity than events occurring later in the day. The Loma Prieta and Great East Japan Earthquakes both occurred in the afternoon hours and were not as clearly associated with an early increase in ACS. The increase in acute coronary syndrome events in the weeks following these earthquakes may be predominantly attributable to psychosocial factors such as missed medications, changed diet, poor living conditions, and the stress of disorder and crime following the event.35 These psychosocial factors have a significant long-term impact on population vulnerability to AMI and are further compounded by compensatory behavioral changes. For example, AMI patients in the post-Katrina phase had a higher incidence of smoking, which is potentially a coping mechanism for the chronic stress of displacement and unemployment.24
The widespread impact of the Great East Japan Earthquake was clearly associated with an increase in admission for acute decompensated heart failure, peaking several weeks after the initial event. While sympathetic activation with resulting hypertension and tachycardia may have played a role, disruptions to the healthcare system likely also contributed. Aoki describes that the medication delivery system was significantly disrupted following the earthquake, tsunami, and nuclear disaster. Further, many people consumed salted preserved foods rather than fresh foods during this period, which may have further exacerbated heart failure.5 Future morbidity from disasters may be preventable through improved disaster preparedness planning, particularly to ensure that patients have medications available in advance. Additionally, post-disaster messaging to cardiac patients to minimize sodium consumption may help to decrease the risk of ADHF during this period of vulnerability.
Our review has some limitations. We sought to identify the change in population prevalence of cardiovascular disease following emergencies, however, the studies included lacked a clear denominator in most instances, therefore population prevalence of disease could not be extrapolated. A small number of high risk populations such as those with cardiac devices may have been excluded. Most of these included studies are from Asia, which may have serious implications for the generalizability of results, given that population vulnerability and health systems resources differ considerably between regions. While generalizability may be limited, these results are still meaningful in terms of global disaster preparedness as Asia is disproportionately affected by natural disasters when compared with other regions.36 Future study of the cardiovascular effects of disasters in low- and middle-income settings is needed, particularly to assist local governments and humanitarian aid organizations in disaster preparedness and response planning in those regions.
Conclusions
Despite the identified correlations between humanitarian emergencies and cardiac morbidity, non-communicable diseases have not traditionally been considered in planning the humanitarian response.2 The findings of this review suggest that addressing chronic disease in disaster planning and response efforts may help mitigate cardiac morbidity and mortality following a disaster. Given the changing global burden of disease, planning for the monitoring and management of cardiac disease in the post-disaster period should be prioritized.
Supplementary Material
Acknowledgments
Funding
No funding was provided for this review.
Summary of abbreviations used in text and figures
- IHD
Ischemic heart disease
- ACS
Acute coronary syndrome
- ADHF
Acute decompensated heart failure
- SCD
Sudden cardiac death
- AMI
Acute myocardial infarction
- STEMI
ST-segment myocardial infarction
- NSTEMI
Non-ST segment myocardial infarction
- LP
Loma Prieta Earthquake
- NRDG
Northridge Earthquake
- ER
Emergency Room
- NR
Not reported
- ICH
Intracranial hemorrhage
- CPA
Cardiopulmonary arrest
- IE
Infectious endocarditis
- PTE
Pulmonary thromboembolism
Footnotes
Appendix 1. MEDLINE Search Strategy
Table 1a. Characteristics of included studies, conflict events
Table 1b. Characteristics of included studies, natural disaster events
Table 2. Risk of Bias Summary for Individual Studies
References
- 1.Forouzanfar MH, Moran AE, Flaxman AD, Roth G, Mensah GA, Ezzati M, et al. Assessing the global burden of ischemic heart disease, part 2: analytic methods and estimates of the global epidemiology of ischemic heart disease in 2010. Global heart. 2012;7(4):331–342. doi: 10.1016/j.gheart.2012.10.003. Epub 2013/03/19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Demaio AJJ, Horn R, de Courten M, Tellier S. Non-Communicable Diseases in Emergencies: A Call to Action. PloS Current. 2013 doi: 10.1371/currents.dis.53e08b951d59ff913ab8b9bb51c4d0de. Epub Sept 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Strike PC, Steptoe A. Behavioral and emotional triggers of acute coronary syndromes: a systematic review and critique. Psychosomatic medicine. 2005;67(2):179–186. doi: 10.1097/01.psy.0000155663.93160.d2. [DOI] [PubMed] [Google Scholar]
- 4.Carroll DES, Tilling K, Macleod J, Smith GD. Admissions for myocardial infarction and World Cup football: database survey. BMJ. 2002;325(7378):1439–1442. doi: 10.1136/bmj.325.7378.1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aoki T, Fukumoto Y, Yasuda S, Sakata Y, Ito K, Takahashi J, et al. The Great East Japan Earthquake Disaster and cardiovascular diseases. Eur Heart J. 2012;33(22):2796–2803. doi: 10.1093/eurheartj/ehs288. [DOI] [PubMed] [Google Scholar]
- 6.Bergovec M, Heim I, Vasilj I, Jembrek-Gostovic M, Bergovec M, Strnad M. Acute coronary syndrome and the 1992–1995 war in Bosnia and Herzegovina: a 10-year retrospective study. Mil Med. 2005;170(5):431–434. doi: 10.7205/milmed.170.5.431. [DOI] [PubMed] [Google Scholar]
- 7.Lo CK, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers' to authors' assessments. BMC Med Res Methodol. 2014;14:45. doi: 10.1186/1471-2288-14-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Review Manager (Rev Man) 5.2. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; 2012. [Google Scholar]
- 9.Vasilj I, Bergovec M, Kvesic A, Strnad M, Ostojic L, Ostojic Z, et al. Acute coronary syndrome frequency in western Herzegovina over the fifteen year period (1987–2001) Coll Antropol. 2006;30(4):915–919. [PubMed] [Google Scholar]
- 10.Miric D, Giunio L, Bozic I, Fabijanic D, Martinovic D, Culic V. Trends in myocardial infarction in Middle Dalmatia during the war in Croatia. Mil. Med. 2001;166(5):419–421. [PubMed] [Google Scholar]
- 11.Zubaid M, Suresh CG, Thalib L, Rashed W. Could Missile Attacks Trigger Acute Myocardial Infarction? Acta Cardiol. 2006;61(4):427–431. doi: 10.2143/AC.61.4.2017304. [DOI] [PubMed] [Google Scholar]
- 12.Chi JS, Speakman MT, Poole WK, Kandefer SC, Kloner RA. Hospital admissions for cardiac events in New York City after September 11, 2001. Am J Cardiol. 2003;92(1):61–63. doi: 10.1016/s0002-9149(03)00468-5. [DOI] [PubMed] [Google Scholar]
- 13.Feng J, Lenihan DJ, Johnson MM, Karri V, Reddy CV. Cardiac sequelae in Brooklyn after the September 11 terrorist attacks. Clin Cardiol. 2006;29(1):13–17. doi: 10.1002/clc.4960290105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Allegra JR, Mostashari F, Rothman J, Milano P, Cochrane DG. Cardiac events in New Jersey after the September 11, 2001, terrorist attack. J Urban Health. 2005;82(3):358–363. doi: 10.1093/jurban/jti087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gold LS, Kane LB, Sotoodehnia N, Rea T. Disaster events and the risk of sudden cardiac death: a Washington State investigation. Prehosp Disaster Med. 2007;22(4):313–317. doi: 10.1017/s1049023x00004921. [DOI] [PubMed] [Google Scholar]
- 16.Brown DL. Disparate effects of the 1989 Loma Prieta and 1994 Northridge earthquakes on hospital admissions for acute myocardial infarction: importance of superimposition of triggers. Am Heart J. 1999;137(5):830–836. doi: 10.1016/s0002-8703(99)70406-0. [DOI] [PubMed] [Google Scholar]
- 17.Watanabe H, Kodama M, Okura Y, Aizawa Y, chinushi M, Nakamura Y, Nagai T, Sato M, Okabe M. Impact of Earthquakes on Takotsbubo Cardiomyopathy. JAMA. 2005;294(3):305–307. doi: 10.1001/jama.294.3.305. [DOI] [PubMed] [Google Scholar]
- 18.Aoki T, Takahashi J, Fukumoto Y, Yasuda S, Ito K, Miyata S, et al. Effect of the Great East Japan Earthquake on Cardiovascular Diseases. Circ J. 2013;77(2):490–493. doi: 10.1253/circj.cj-12-1594. [DOI] [PubMed] [Google Scholar]
- 19.Chan C, Elliott J, Troughton R, Frampton C, Smyth D, Crozier I, et al. Acute myocardial infarction and stress cardiomyopathy following the Christchurch earthquakes. PloS one. 2013;8(7):e68504. doi: 10.1371/journal.pone.0068504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tsai CH, Lung FW, Wang SY. The 1999 Ji-Ji (Taiwan) earthquake as a trigger for acute myocardial infarction. Psychosomatics. 2004;45(6):477–482. doi: 10.1176/appi.psy.45.6.477. [DOI] [PubMed] [Google Scholar]
- 21.Tsuchida M, Kawashiri MA, Teramoto R, Takata M, Sakata K, Omi W, et al. Impact of severe earthquake on the occurrence of acute coronary syndrome and stroke in a rural area of Japan. Circ J. 2009;73(7):1243–1247. doi: 10.1253/circj.cj-08-0812. [DOI] [PubMed] [Google Scholar]
- 22.Nozaki E, Nakamura A, Abe A, Kagaya Y, Kohzu K, Sato K, et al. Occurrence of cardiovascular events after the 2011 Great East Japan Earthquake and tsunami disaster. Int Heart J. 2013;54(5):247–253. doi: 10.1536/ihj.54.247. [DOI] [PubMed] [Google Scholar]
- 23.Nakamura A, Nozaki E, Fukui S, Endo H, Takahashi T, Tamaki K. Increased risk of acute myocardial infarction after the Great East Japan Earthquake. Heart Vessels. 2014;29(2):206–212. doi: 10.1007/s00380-013-0353-y. [DOI] [PubMed] [Google Scholar]
- 24.Gautam S, Menachem J, Srivastav SK, Delafontaine P, Irimpen A. Effect of Hurricane Katrina on the incidence of acute coronary syndrome at a primary angioplasty center in New Orleans. Disaster Med Public Health Prep. 2009;3(3):144–150. doi: 10.1097/DMP.0b013e3181b9db91. [DOI] [PubMed] [Google Scholar]
- 25.Peters MN, Katz MJ, Moscona JC, Alkadri ME, Khazi Syed RH, Turnage TA, et al. Effect of Hurricane Katrina on chronobiology at onset of acute myocardial infarction during the subsequent three years. Am J Cardiol. 2013;111(6):800–803. doi: 10.1016/j.amjcard.2012.10.050. [DOI] [PubMed] [Google Scholar]
- 26.Nakamura A, Satake H, Abe A, Kagaya Y, Kohzu K, Sato K, et al. Characteristics of heart failure associated with the Great East Japan Earthquake. J Cardiol. 2013;62(1):25–30. doi: 10.1016/j.jjcc.2013.02.015. [DOI] [PubMed] [Google Scholar]
- 27.Nakamura M, Tanaka F, Nakajima S, Honma M, Sakai T, Kawakami M, et al. Comparison of the incidence of acute decompensated heart failure before and after the major tsunami in Northeast Japan. Am J Cardiol. 2012;110(12):1856–1860. doi: 10.1016/j.amjcard.2012.08.020. [DOI] [PubMed] [Google Scholar]
- 28.Yamauchi H, Yoshihisa A, Iwaya S, Owada T, Sato T, Suzuki S, et al. Clinical features of patients with decompensated heart failure after the Great East Japan Earthquake. Am J Cardiol. 2013;112(1):94–99. doi: 10.1016/j.amjcard.2013.02.057. [DOI] [PubMed] [Google Scholar]
- 29.Kitamura T, Kiyohara K, Iwami T. The great east Japan earthquake and out-of-hospital cardiac arrest. NEJM. 2013;369(22):165–167. doi: 10.1056/NEJMc1306058. [DOI] [PubMed] [Google Scholar]
- 30.Ogawa K, Tsuji I, Shiono K, Hisamichi S. Increased acute myocardial infarction mortality following the 1995 Great Hanshin-Awaji earthquake in Japan. Int J Epidemiol. 2000;29(3):449–455. [PubMed] [Google Scholar]
- 31.Wells GASB, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P. [Accessed April 19, 2014];Newcastle-Ottawa Quality Assessment Scale Cohort Studies. Available from http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- 32.Lin LYWC, Liu YB, Ho YL, Liau CS, Lee YT. Derangement of Heart Rate Variability During a Catastrophic Earthquake: A possible mechanism for increased heart attacks. Pacing Clin Electrophysiol. 2001;24(11):1596–1601. doi: 10.1046/j.1460-9592.2001.01596.x. [DOI] [PubMed] [Google Scholar]
- 33.Nakano M, Kondo M, Wakayama Y, Kawana A, Hasebe Y, Shafee MA, et al. Increased Incidence of Tachyarrhythmias and Heart Failure Hospitalization in Patients With Implanted Cardiac Devices After the Great East Japan Earthquake Disaster. Circ J. 2012;76(5):1283–1285. doi: 10.1253/circj.cj-12-0261. [DOI] [PubMed] [Google Scholar]
- 34.Nishizawa M, Hoshide S, Shimpo M, Kario K. Disaster Hypertension: Experience from the Great East Japan Earthquake of 2011. Current Hypertens Rep. 2012;14(5):375–381. doi: 10.1007/s11906-012-0298-z. [DOI] [PubMed] [Google Scholar]
- 35.Lavie CJ, Gerber TC, Lanier WL. Hurricane Katrina: the infarcts beyond the storm. Disaster Med Public Health Prep. 2009;3(3):131–135. doi: 10.1097/DMP.0b013e3181bab1d4. [DOI] [PubMed] [Google Scholar]
- 36. [Accessed April 18, 2014];OFDA/CRED. 2013 Disasters in Numbers Available from: http://www.emdat.be.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.