Abstract
Study Design.
The Bracing in Adolescent Idiopathic Scoliosis Trial (BrAIST) included skeletally immature high-risk patients with adolescent idiopathic scoliosis (AIS) with moderate curve sizes (20°– 40°). BrAIST was a multicenter, controlled trial using both randomized and preference treatment arms into either an observation group or a brace treatment group.
Objective.
The aim of this study was to analyze and compare body image and quality-of-life (QOL) in female AIS patients who were observed or treated with a brace.
Summary of Background Data.
Brace treatment is an effective means for controlling progressive scoliosis and preventing the need for surgery, but there is no consensus regarding the effect of brace treatment on body image or on QOL in adolescents with AIS.
Methods.
Data from female BrAIST patients in the randomized (n = 132) or preference (n = 187) arms and were observed (n = 120) or brace treated (n = 199) were analyzed. Patients completed the Spinal Appearance Questionnaire (SAQ) and the Pediatric Quality of Life Inventory (PedsQOL) 4.0 Generic Scales at baseline and 6 month follow-up visits up to 2 years. Items on the SAQ measured three body image constructs (self, ideal, and overall). The PedsQOL measured health, activities, feelings, social factors, and school.
Results.
. In general, there were no significant differences within or between study arms or treatments regarding body image or QOL through 2 years of follow-up. Poorer body image was significantly correlated with poorer QOL during the first 2 years of follow-up regardless of study arm or treatment. Patients who crossed-over to a different treatment and patients with largest Cobb angles ≥ 40 degrees had significantly poorer body image, in particular self-body image, compared with those that did not.
Conclusion.
This study does not support findings from previous research indicating that wearing a brace has a negative impact on or is negatively impacted by body image or QOL.
Level of Evidence: 2
Keywords: adolescent, body image, brace treatment, observation, outcome, psychological, quality-of-life, scoliosis, social, well being
Given the increased attention to body image during the adolescent development phase, it would be expected that psychosocial well-being, in particular body image and quality-of-life (QOL), would be greatly impacted in adolescents diagnosed with a possibly disfiguring condition such as adolescent idiopathic scoliosis (AIS). In addition to the possibility of and/or the degree of disfigurement that is related to the condition itself, body image and QOL might be negatively impacted by AIS treatments such as wearing a brace in front of peers and the daily physical encumbrance of wearing a brace. Despite recent evidence indicating that brace treatment is effective in preventing surgery,1 researchers have failed to conceptualize the relationships among body image, QOL, AIS-related spinal deformity, and AIS treatment.
The majority of research regarding brace treatment compares psychological well-being in adolescents with AIS undergoing brace treatment to their healthy peers. When compared with adolescents that are undergoing observation to healthy peers, some research suggests that brace treatment can negatively impact psychosocial well-being,2–7 whereas other research indicates that brace treatment does not negatively impact psychosocial well-being.1,8–12 A systematic review of the literature found that adolescents with scoliosis may experience poorer psychosocial functioning, body image, and health-related QOL when compared with their healthy peers.13
Only a few studies have compared psychological well-being in adolescents with AIS undergoing brace treatment with adolescents with AIS undergoing observation. One study found that brace treatment resulted in a reduction in body image and QOL compared with adolescents that were being observed.4 When looking at the long-term impact of brace treatment on body image, one study found that, despite similar curve size and trunk rotation, adolescents that were not braced estimated that their body appearance was significantly less distorted compared with adolescents that were braced.8
The majority of AIS studies have been retrospective studies that use different instruments to measure psychological indices and brace-wear adherence, which may have contribute to the lack of consensus regarding relationships among psychological well-being, AIS, and brace treatment.14 The Bracing in Adolescent Idiopathic Scoliosis Trial (BrAIST) was designed to overcome several of the methodological issues and limitations of previous research. BrAIST was a multicenter, randomized controlled clinical trial, using blinded outcome determination, a priori determination of the effect size and objective brace monitors for assessing brace-wear adherence.14 The BrAIST primary endpoint was to determine the effectiveness of bracing, as compared with observation, in preventing curve progression to 50 degrees or more, which is a common indication for surgery. BrAIST found that bracing significantly decreased the progression of high-risk curves to the threshold indicated for surgery.1
In addition to testing the effectiveness of bracing, the secondary aims of BrAIST were to investigate the impact of brace treatment on the psychosocial well-being of adolescents undergoing brace treatment compared with adolescents undergoing observation. When looking at whether there were any differences in QOL scores between the observation group (n = 96) and the brace treatment group (n = 146) in BrAIST patients who had reached a study endpoint (skeletal maturity or largest Cobb angle ≥ 50°), there were no significant differences at baseline or at the final follow-up assessment.1 The purpose of this study was to assess whether there were any significant differences and correlations between body image and QOL, including changes over time, in female adolescents participating in BrAIST that were based on study arm (randomized or preference) and study treatment (brace or observation).
MATERIALS AND METHODS
BrAIST enrolled 384 patients who had never undergone treatment for AIS and were deemed at highest risk for progression because of their age, skeletal immaturity, and curve size. BrAIST eligibility requirements included a confirmed diagnosis of AIS and all of the following: age ≥ 10 to < 15 years old; Risser 0, 1, and 2; female premenarchal or < 1 year postmenarchal; Cobb angle of 20°–40°; apex at or caudal to T7; and no previous treatment for AIS. Adolescents in the brace group were instructed to wear their brace for at least 18 hours/day.
Two body-image constructs in the Spinal Appearance Questionnaire (SAQ)15 coincide with body-image constructs from Cash's Cognitive-Behavioral Perspective on Body Image.16 The SAQ appearance domain (items 1–7, and 9) is similar to Cash's self-body image and is summed 8 to 40 with higher scores indicating poorer body image. The SAQ expectation domain (items 10–17) is similar to Cash's ideal-body image construct and is summed 8 to 40 with higher scores reflecting more emphasis on wanting to look “normal.” The SAQ total score is the sum of the appearance domain and the expectation domain (range 16–80), which is similar to Cash's self-ideal body-image discrepancy construct where higher scores indicate a larger discrepancy between how individuals’ think they currently look and how they want to look. Previous research indicates that the SAQ is a valid measure of body image.17,18
Adolescents also completed a QOL–Child, ages 10 to 12 years or a QOL–Teen, ages 13 to 18 years at each visit. The PedsQOL4.0 Generic Corse Scales is a valid and reliable instrument for distinguishing health-related QOL between healthy children and children with chronic illnesses.19 Scores on the PedsQOL range from 0 to 100 with higher scores indicating better QOL. The questionnaire consists of 23 items applicable for healthy and community populations, and pediatric populations with acute and chronic health conditions. The PedsQOL measures health, activities, feelings, how well one gets along with others, and school.
STATISTICAL ANALYSIS
Because of the small number of males (n = 45) in the BrAIST study, this study only assessed body image and QOL relationships in female BrAIST patients (n = 319). Figure 1 displays the enrollment of the female patients in this study. Because adolescents’ body image and QOL at the time of enrollment might have impacted whether they participated in the randomized or preference arm, the current study compares between and within study arms. Figure 2 provides a summary of the comparisons conducted between study arms (Comparison 1), within randomization arm (Comparison 2), within observation arm (Comparison 3), between study arms in braced (Comparison 4), and observation (Comparison 5) treatment groups. This study also compared brace and observation treatment groups (Comparison 6), regardless of study arm.
Figure 1.
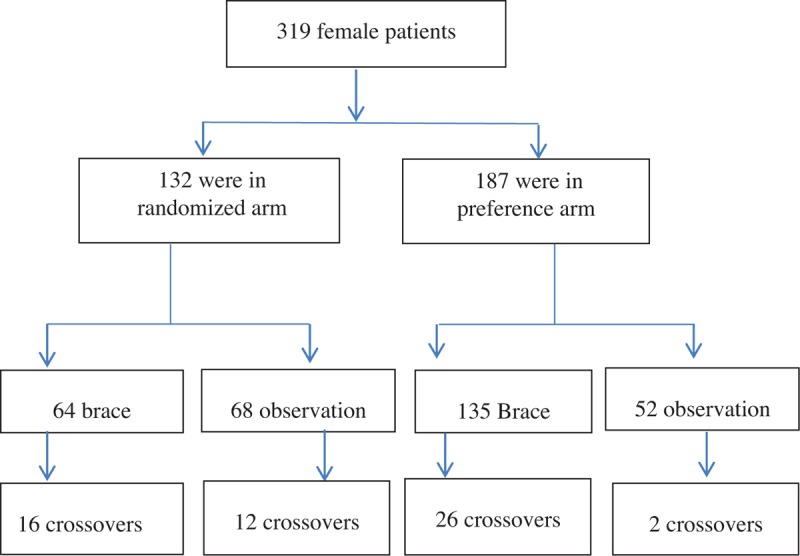
Baseline study enrollment and treatment of female adolescents.
Figure 2.
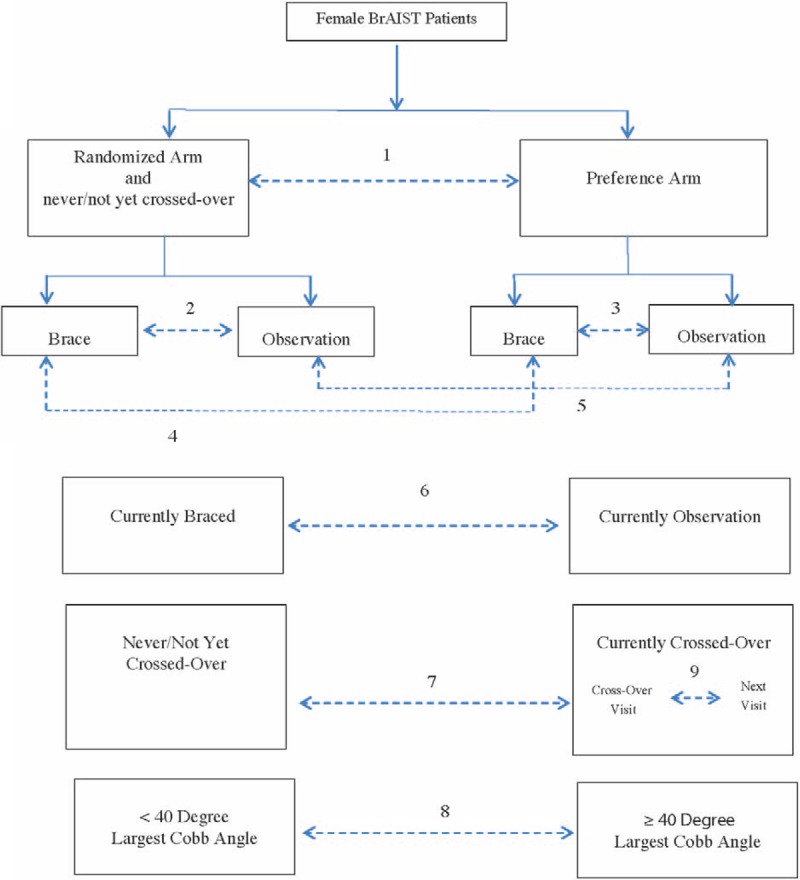
Summary of comparisons (dashed lines) at baseline, 6, 12, 18, and 24 months regarding body mass index, largest Cobb angle, body image, and quality of life.
As body image and QOL may have also played a role in a patient's decision to cross-over to the other treatment, differences were assessed between patients who had crossed-over compared with patients who had never/not yet crossed-over (Figure 2, Comparison 7). In addition, paired t tests were conducted to test for differences within the cross-over patients (Figure 2, Comparison 9), comparing body image and QOL at the visit closest with the time of cross-over to their next visit, which may have been more than 6 months later.
Spearman's rank correlation coefficient was conducted to test for associations between the three body image constructs and body mass index (BMI), largest Cobb angle, and QOL. Finally, body image and QOL were compared between patients with a ≥40 degree largest Cobb angle with those that did not (Figure 2, Comparison 8), regardless of study arm. Wilcoxon rank-sum tests were conducted to assess differences, regarding BMI, largest Cobb angle, body-image constructs, and QOL in Comparisons 1–8.
RESULTS
Table 1 and Table 2 display the comparisons among and within study arms (Table 1) and among and within treatments (Table 2). In general, there were only a few significant differences among or within study arms or among treatments regarding body-image scores and QOL during the first 2 years of follow-up.
TABLE 1.
BMI, Largest Cobb Angle, QOL, Self-Body Image, Ideal-Body Image, and Self-Ideal Body-Image Discrepancy in Randomized and Preference Study Arms
| Randomized vs. Preference | Randomized Arm (Never or Not Yet Crossed-Over) | Preference Arm | |||||
| P | Brace | Observation | P | Brace | Observation | P | |
| Baseline | (n = 64) | (n = 68) | (n = 135) | (n = 52) | |||
| BMI | 0.25 | 19.5 (3.9) | 18.9 (3.4) | 0.20 | 19.2 (3.3) | 19.7 (3.2) | 0.27 |
| Largest Cobb angle | 0.16 | 29.7 (4.7) | 29.3 (5.7) | 0.66 | 28.9 (5.8) | 27.7 (6.0) | 0.19 |
| QOL | 0.07 | 82.2 (14.6) | 83.4 (12.6) | 0.81 | 85.7 (12.6) | 85.5 (11.7) | 0.76 |
| Self-body | 0.11 | 17.6 (4.8) | 18.1 (4.2) | 0.63 | 16.9 (3.9) | 18.1 (4.7) | 0.03 |
| Ideal-body | 0.11 | 21.1 (10.4) | 19.2 (10.4) | 0.25 | 18.4 (10.2) | 17.9 (10.1) | 0.53 |
| Self-ideal | 0.07 | 38.1 (13.3) | 37.1 (12.6) | 0.64 | 35.1 (12.7) | 36.0 (13.0) | 0.68 |
| 6 months | (n = 62) | (n = 59) | (n = 125) | (n = 61) | |||
| BMI | 0.05 | 19.7 (3.6) | 19.2 (4.5) | 0.21 | 19.7 (3.4) | 20.1 (3.4) | 0.37 |
| Largest Cobb angle | 0.19 | 29.1 (8.7) | 33.7 (8.1) | 0.009 | 29.6 (8.3) | 30.8 (7.6) | 0.42 |
| QOL | 0.01 | 82.6 (15.2) | 81.8 (13.9) | 0.56 | 86.4 (11.8) | 86.7 (11.2) | 0.98 |
| Self-body | 0.07 | 17.8 (4.4) | 17.8 (4.9 | 0.79 | 16.8 (4.2) | 16.9 (4.6) | 0.82 |
| Ideal-body | 0.35 | 20.5 (10.8) | 20.5 (10.9) | 0.94 | 20.1 (10.4) | 16.8 (9.2) | 0.03 |
| Self-ideal | 0.16 | 38.3 (13.5) | 38.3 (13.5) | 0.96 | 36.9 (12.6) | 33.8 (11.7) | 0.12 |
| 12 months | (n = 57) | (n = 50) | (n = 119) | (n = 59) | |||
| BMI | 0.08 | 19.5 (2.7) | 20.0 (4.4) | 0.99 | 19.8 (3.1) | 21.1 (3.6) | 0.009 |
| Largest Cobb angle | 0.37 | 30.2 (9.6) | 37.0 (9.3) | 0.002 | 31.6 (10.4) | 34.0 (9.2) | 0.08 |
| QOL | 0.01 | 82.2 (14.0) | 83.1 (12.4) | 0.96 | 86.1 (13.6) | 85.9 (5.4) | 0.94 |
| Self-body | 0.10 | 18.9 (4.5) | 19.1 (5.8) | 0.96 | 17.7 (4.7) | 18.9 (9.6) | 0.19 |
| Ideal-body | 0.31 | 21.3 (10.7) | 19.7 (9.5) | 0.51 | 19.8 (10.8) | 18.5 (9.6) | 0.55 |
| Self-ideal | 0.18 | 40.2 (13.5) | 38.8 (13.3) | 0.56 | 37.7 (12.9) | 37.4 (13.6) | 0.89 |
| 18 months | (n = 48) | (n = 41) | (n = 93) | (n = 64) | |||
| BMI | 0.53 | 19.6 (2.4) | 20.5 (3.3) | 0.32 | 20.1 (2.9) | 20.9 (3.7) | 0.30 |
| Largest Cobb angle | 0.15 | 31.2 (9.4) | 37.8 (7.4) | 0.002 | 32.4 (10.1) | 35.2 (9.2) | 0.10 |
| QOL | 0.32 | 84.8 (10.9) | 83.0 ((15.1) | 0.63 | 86.3 (11.7) | 85.0 (13.0) | 0.56 |
| Self-body | 0.09 | 17.9 (4.5) | 20.1 (6.4) | 0.16 | 17.5 (4.2) | 18.8 (6.3) | 0.42 |
| Ideal-body | 0.60 | 18.9 (10.5) | 20.9 (10.2) | 0.34 | 19.4 (10.7) | 18.6 (10.1) | 0.81 |
| Self-ideal | 0.43 | 36.8 (13.1) | 41.0 (14.6) | 0.16 | 37.0 (12.7) | 37.4 (13.1) | 0.80 |
| 24 months | (n = 30) | (n = 37) | (n = 72) | (n = 50) | |||
| BMI | 0.87 | 20.1 (2.9) | 21.3 (3.3) | 0.11 | 20.1 (2.6) | 21.5 (4.0) | 0.06 |
| Largest Cobb angle | 0.39 | 31.9 (10.3) | 38.3 (8.3) | 0.008 | 31.9 (10.5) | 37.0 (9.8) | 0.01 |
| QOL | 0.11 | 82.3 (15.1) | 79.8 (15.4) | 0.52 | 86.4 (12.2) | 81.9 (15.5) | 0.14 |
| Self-body | 0.82 | 17.6 (5.0) | 19.7 (6.5) | 0.22 | 17.4 (4.0) | 20.5 (5.6) | 0.002 |
| Ideal-body | 0.58 | 22.1 (11.9) | 21.0 (10.8) | 0.63 | 20.0 (9.8) | 19.7 (9.8) | 0.74 |
| Self-ideal | 0.50 | 39.8 (15.0) | 40.7 (14.8) | 0.73 | 37.4 (11.4) | 40.2 (14.0) | 0.35 |
Note: Values are Means (±SD) and P values are two-sided. BMI indicates body mass index; QOL, quality of life.
TABLE 2.
BMI, Largest Cobb Angle, QOL, Self-Body Image, Ideal-Body Image, and Self-Ideal Body-Image Discrepancy in Brace and Observation Groups
| Brace Treatment Randomized vs. Preference | Observation Randomized vs. Preference | Brace vs. Observation | |
| P | P | P | |
| Baseline | |||
| BMI | 0.82 | 0.06 | 0.86 |
| Largest Cobb angle | 0.37 | 0.14 | 0.17 |
| QOL | 0.13 | 0.35 | 0.58 |
| Self-body | 0.13 | 0.81 | 0.12 |
| Ideal-body | 0.09 | 0.41 | 0.45 |
| Self-ideal | 0.09 | 0.44 | 0.79 |
| 6 months | |||
| BMI | 0.58 | 0.02 | 0.40 |
| Largest Cobb angle | 0.76 | 0.06 | 0.01 |
| QOL | 0.16 | 0.05 | 0.35 |
| Self-body | 0.13 | 0.06 | 0.55 |
| Ideal-body | 0.97 | 0.30 | 0.45 |
| Self-ideal | 0.56 | 0.06 | 0.80 |
| 12 months | |||
| BMI | 0.57 | 0.02 | 0.87 |
| Largest Cobb angle | 0.60 | 0.18 | 0.0005 |
| QOL | 0.06 | 0.12 | 0.91 |
| Self-body | 0.08 | 0.79 | 0.18 |
| Ideal-body | 0.39 | 0.45 | 0.48 |
| Self-ideal | 0.23 | 0.52 | 0.85 |
| 18 months | |||
| BMI | 0.49 | 0.78 | 0.84 |
| Largest Cobb angle | 0.78 | 0.11 | 0.002 |
| QOL | 0.31 | 0.36 | 0.17 |
| Self-body | 0.38 | 0.18 | 0.08 |
| Ideal-body | 0.86 | 0.25 | 0.79 |
| Self-ideal | 0.88 | 0.23 | 0.32 |
| 24 months | |||
| BMI | 0.74 | 0.96 | 0.16 |
| Largest Cobb angle | 0.98 | 0.53 | 0.01 |
| QOL | 0.21 | 0.50 | 0.08 |
| Self-body | 0.90 | 0.45 | 0.15 |
| Ideal-body | 0.67 | 0.81 | 0.89 |
| Self-ideal | 0.62 | 0.75 | 0.42 |
Note: P values are two-sided. BMI indicates body mass index; QOL, quality of life.
The only significant difference between the randomization and preference arms (Comparison 1) was poorer QOL in the randomization patients at 6 months (P = 0.01) and at 12 months (P = 0.01). When analyzing these results, one must consider that it is likely that some patients who were randomized and remained randomized during the first 2 years of follow-up were randomized to the treatment that they would have chosen, if making the choice, which makes them similar to the patients in the preference arm. Furthermore, it is likely that some patients were randomized into a treatment that they would not have chosen, if making the choice, so they crossed-over to a different treatment soon after randomization, which makes them part of the preference arm population at the time of the cross-over visit and through the rest of the 2 year follow-up.
When looking at treatment differences within each study arm (Comparisons 2 and 3), in both study arms, there were no significant differences between the brace and observation groups regarding BMI or QOL at any visit in the first 2 years of follow-up. Within the randomization arm (Comparison 2), despite the observation group having significantly greater largest Cobb angle at the 6, 12, 18, and 24 month follow-up visits compared with the brace group, there were no significant differences between brace and observation groups regarding any of the three body-image constructs at any visit. At baseline, within the preference arm (Comparison 3), there was a moderate significantly poorer self-body image (P = 0.03) in the observation group (n = 52) compared with the brace group (n = 135). In addition, at the 24 month visit within the preference study arm, the observation group had a significantly larger Cobb angle (P = 0.01) and significantly poorer self-body image (P = 0.002) compared with the brace group.
There were no significant differences between the randomized brace-treated and preference brace-treated patients (Comparison 4) or between the randomized observation and preference observation patients (Comparison 5) regarding largest Cobb angle, QOL, or body image at any visit during the first 2 years of follow-up. Observation preference patients had significantly higher BMI compared with the observation randomized patients at 6 months (P = 0.02) and 12 months (P = 0.02). There were no significant differences regarding BMI between the preference brace-treated patients and the observation brace-treated patients at any visit during the first 2 years of follow-up. The only significant differences in BMI, largest Cobb angle, body-image constructs, and QOL between the brace group and the observation group (Comparison 6) was in the largest Cobb angle at the 6 months through 24 month follow-up.
When comparing patients who had recently crossed-over to a different treatment to those that had not (Comparison 7), self-body image was significantly poorer in the cross-over group at 12 months (n = 25, 256, respectively; P = 0.05); 18 months (n = 35, 208, respectively; P = 0.02), and 24 months (n = 38, 146, respectively; P = 0.002). Within the patients who crossed-over (Comparison 9), there were no significant differences in body-image scores or in QOL scores between their cross-over visits compared with their next visits.
Table 3 (Randomized Arm) and Table 4 (Preference Arm) display the correlations between body-image constructs, QOL, BMI, and largest Cobb angle at baseline, 12 months, and 24 months based on study arm. In general, poorer body image was significantly correlated with poorer QOL in both arms throughout the first 2 years of follow-up, regardless of study arm or current treatment. The only time poorer body image did not significantly correlate with poorer QOL, in at least two out of the three body-image constructs, was in the randomized brace group at the 24 month visit.
TABLE 3.
Randomized Arm (Never/Not Yet Crossed-Over): Group Spearman's Rank Correlations in Self-Body Image, Ideal-Body Image, and Self-Ideal Body-Image Discrepancy and Treatment Group Characteristics Over-Time
| Brace Self-Body | Brace Ideal-Body | Brace Self-Ideal | Observation Self-Body | Observation Ideal-Body | Observation Self-Ideal | |
| BMI | ||||||
| Baseline | –0.02 P = 0.90 | 0.14 P = 0.28 | 0.11 P = 0.41 | 0.09 P = 0.47 | –0.03 P = 0.83 | 0.01 P = 0.93 |
| 12 months | 0.17 P = 27 | 0.07 P = 0.63 | 0.15 P = 0.30 | 0.003 P = 0.98 | –0.02 P = 0.87 | –0.003 P = 0.98 |
| 24 months | 0.01 P = 0.93 | –0.11 P = 0.57 | –0.06 P = 0.77 | –0.20 P = 0.25 | –0.18 P = 0.30 | –0.26 P = 0.14 |
| Largest Cobb angle | ||||||
| Baseline | 0.09 P = 0.46 | 0.24 P = 0.008 | 0.31 P = 0.01 | 0.27 P = 0.03 | –0.06 P = 0.66 | 0.02 P = 0.90 |
| 12 months | 0.45 P = 0.002 | 0.29 P = 0.05 | 0.35 P = 0.02 | 0.19 P = 0.19 | 0.24 P = 0.09 | 0.23 P = 0.11 |
| 24 months | 0.61 P = 0.0006 | 0.44 P = 0.02 | 0.57 P = 0.002 | 0.38 P = 0.02 | 0.13 P = 0.44 | 0.29 P = 0.09 |
| QOL | ||||||
| Baseline | –0.322 P = 0.01 | –0.34 P = 0.008 | –0.43 P = 0.0004 | –0.08 P = 0.55 | –0.36 P = 0.004 | –0.36 P = 0.004 |
| 12 months | –0.19 P = 0.21 | –0.60 P <0.0001 | –0.46 P = 0.001 | –0.30 P = 0.03 | –0.43 P = 0.002 | –0.46 P = 0.0007 |
| 24 months | –0.32 P = 0.09 | –0.23 P = 0.25 | –0.31 P = 0.11 | –0.42 P = 0.01 | –0.58 P = 0.0002 | –0.61 P = 0.0001 |
BMI indicates body mass index; QOL, quality of life.
TABLE 4.
Preference Arm: Spearman's Rank Correlations in Self-Body Image, Ideal-Body Image, and Self-Ideal Body-Image Discrepancy and Treatment Group Characteristics Over-Time
| Brace Self-Body | Brace Ideal-Body | Brace Self-Ideal | Observation Self-Body | Observation Ideal-Body | Observation Self-Ideal | |
| BMI | ||||||
| Baseline | 0.08 P = 0.31 | 0.11 P = 0.21 | 0.12 P = 0.16 | 0.27 P = 0.05 | 0.18 n = 0.20 | 0.25 P = 0.07 |
| 12 months | –0.06 P = 0.489 | –0.11 P = 0.21 | –0.11 P = 0.25 | 0.15 P = 0.25 | 0.17 P = 0.22 | 0.17 P = 0.22 |
| 24 months | –0.06 P = 0.65 | –0.07 P = 0.53 | –0.06 P = 0.63 | –0.05 P = 0.73 | 0.07 P = 0.65 | 0.04 P = 0.81 |
| Largest Cobb angle | ||||||
| Baseline | 0.05 P = 0.53 | –0.04 P = 0.52 | –0.01 P = 0.91 | 0.25 P = 0.08 | –0.09 P = 0.53 | 0.02 P = 0.87 |
| 12 months | 0.36 P <0.0001 | 0.08 P = 0.39 | 0.20 P = 0.25 | 0.44 P = 0.0006 | 0.12 P = 0.36 | 0.22 P = 0.09 |
| 24 months | 0.24 P = 0.04 | 0.33 P = 0.005 | 0.34 P = 0.63 | 0.44 P = 0.001 | 0.18 P = 0.22 | 0.28 P = 0.05 |
| QOL | ||||||
| Baseline | –0.26 P = 0.003 | –0.35 P <0.0001 | –0.40 P <0.0001 | –0.39 P = 0.005 | –0.34 P = 0.01 | –0.43 P = 0.002 |
| 12 months | –0.24 P = 0.008 | –0.33 P = 0.0003 | –0.32 P = 0.0004 | –0.41 P = 0.0002 | –0.43 P = 0.001 | –0.46 P = 0.0003 |
| 24 months | –0.05 P = 0.69 | –0.31 P = 0.0009 | –0.24 P = 0.04 | –0.26 P = 0.07 | –0.48 P = 0.0004 | –0.46 P = 0.0006 |
BMI indicates body mass index; QOL, quality of life.
Finally, Table 5 displays the results comparing patients who currently had ≥ 40 degree largest Cobb angle compared with those that did not (Comparison 8). In general, patients with ≥ 40 degree largest Cobb angle had significantly poorer scores in all three body-image constructs compared with the patients who did not at all follow-up visits up to 2 years.
TABLE 5.
QOL, Body-Image Constructs (Self, Ideal, and Self-Ideal Discrepancy) in Patients With Current Largest Cobb Angle of <40 Degrees Compared With ≥40 Degrees (Comparison 9)
| <40 Degree Largest Cobb Angle | ≥40 Degree Largest Cobb Angle | P | |
| 6 Months | (n = 257) | (n = 42) | |
| QOL | 85.3 (12.8) | 82.1 (14.4) | 0.20 |
| Self-body | 16.8 (4.1) | 19.9 (5.4) | 0.0002 |
| Ideal-body | 19.3 (10.4) | 21.5 (10.0) | 0.11 |
| Self-ideal | 36.2 (12.7) | 41.4 (13.0) | 0.01 |
| 12 months | (n = 221) | (n = 60) | |
| QOL | 85.9 (12.1) | 80.4 (16.6) | 0.008 |
| Self-body | 17.5 (4.5) | 21.9 (5.6) | <0.0001 |
| Ideal-body | 19.2 (10.1) | 22.4 (10.8) | 0.02 |
| Self-ideal | 36.7 (12.6) | 44.3 (13.9) | 0.0002 |
| 18 months | (n = 176) | (n = 67) | |
| QOL | 84.9 (12.9) | 85.6 (9.6) | 0.62 |
| Self-body | 17.5 (4.7) | 20.7 (6.0) | 0.0001 |
| Ideal-body | 19.2 (10.7) | 19.6 (9.6) | 0.35 |
| Self-ideal | 36.7 (13.2) | 40.2 (12.9) | 0.04 |
| 24 months | (n = 129) | (n = 56) | |
| QOL | 83.9 (14.8) | 82.0 (13.5) | 0.19 |
| Self-body | 17.3 (4.7) | 21.9 (5.3) | <0.0001 |
| Ideal-body | 19.2 (10.2) | 22.7 (10.0) | 0.01 |
| Self-ideal | 36.5 (12.7) | 44.6 (12.9) | <0.0001 |
Note: Values are means (±SD) and P values are two-sided. QOL indicates quality of life.
DISCUSSION
When looking at differences among treatment groups, findings from this study indicate that brace treatment does not negatively impact body image or QOL in female adolescents with AIS. Furthermore, the QOL scores in both treatment groups were similar to mean total scores for healthy children, which range from 83–86 depending on age.19 Results from this study do not support previous research suggesting that brace wear has a negative impact on psychosocial well-being, in particular body image and QOL.2–7 However, these findings corroborate those of previous studies, which found that brace treatment did not negatively impact body image11,12 or QOL.8,9
By comparing the randomization and preference study arms, this study found that body image is not negatively impacted by whether adolescents have played a role in their treatment decisions. For patients in the randomized arm, not having a choice in their treatment decision might have resulted in poorer QOL during the first year after AIS diagnosis compared with patients who chose their treatment. However, findings from this study suggest that, despite not having had a say in their treatment, after about a year, patients begin to adjust to their current treatment (brace or observation) and QOL improves.
When assessing body image and QOL within each arm, at baseline in the preference arm, females who chose to undergo observation had significantly poorer self-body image compared with females who chose bracing, which was not the case in the randomization arm. In addition to possibly being a motivating factor to undergo observation and not brace treatment, poorer self-body image was also related to the decision to cross-over to a different treatment. Unfortunately, self-body image did not significantly improve at the visit after the cross-over visit. Finally, regardless of study arm or treatment, poorer self-body image was also found in female patients who had ≥ 40 degree largest Cobb angle compared with those that did not, regardless of study arm or treatment.
In general, poorer QOL correlated with poorer self-body image, with placing higher importance on wanting to look “normal” (ideal-body image) and with poorer overall body image (self-ideal body image discrepancy) in both study arms and in both treatment groups. These findings are consistent with the literature regarding the importance of QOL, in particular regarding positive home environment on an adolescent's body image.20–22 Choate20 found that some familial characteristics, such as negative family attitudes and critical comments about an individual's physical shape may contribute to negative body image among daughters. Studies have found that when psychosocial distress is detected, interventions that provide psychological and social support, such as reflecting and discussing concerns about appearance and comfort when wearing a brace, can improve psychosocial well-being.5,23 Findings from this study suggest that interventions to improve psychosocial well-being should aim to improve both QOL and body image, with particular focus on addressing concerns about how the adolescent thinks she currently looks.
In summary, poorer body image, in particular self-body image, was impacted by an AIS-related outcome (degree of largest Cobb angle) and associated with other psychological characteristics (poorer QOL). Poorer QOL was found in patients who did not participate in their treatment decisions (randomized arm) but these patients seemed to adjust after the first year after diagnosis. Body image and QOL were not negatively impacted by brace treatment.
CONCLUSION
This study suggests that healthcare providers should not be concerned about the negative impact of brace treatment on body image and QOL when recommending brace treatment to their female patients. However, poorer self-body image could be a barrier to starting and continuing brace treatment. Therefore, body image should be assessed upon initial diagnosis and throughout the treatment process. As simply changing treatment does significantly improve body image, when poor body image is detected, the healthcare team should provide interventions to improve both QOL and body image, in particular concerns about current appearance. Psychosocial interventions, such as having a patient reflect on concerns about wearing the brace in front of their peers, may alleviate some of the patient's distress regarding brace treatment, amount of choice in the treatment decision, and increased spinal deformity.
Key Points.
There were no significant differences in body image or in QOL at baseline for females with AIS who chose brace treatment compared with females who chose to undergo observation.
Poorer body image, in particular concerns about current appearance, was impacted by an AIS-related outcome (larger Cobb angles) and was associated with other patient psychological factors (poorer QOL).
Initially, poorer QOL was found in patients who did not participate in their treatment decisions, regardless of whether they were undergoing brace or observation treatment, but patients seemed to adjust to their treatment and QOL improved after 1 year of being diagnosed with AIS.
Footnotes
The devices(s)/drugs(s) that is/are the subject of this article is/are exempt from FDA or corresponding national regulations. The project described was supported by Award Numbers R21AR049587 and R01AR052113 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases; the Shriners Hospitals for Children (#79125); the Canadian Institutes of Health Research (FRN-81050); the University of Rochester; the Children's Mercy Hospital and Clinics; and the Children's Miracle Network. Relevant financial activities outside the submitted work: grants and royalties.
References
- 1.Weinstein SL, Dolan LA, Wright JG, et al. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med 2013; 369:1512–1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sapountzi-Krepia DS, Valavanis J, Panteleakis GP, et al. Perception of body image, happiness, and satisfaction in adolescents wearing a Boston brace for scoliosis treatment. J AdvNurs 2001; 35:683–690. [DOI] [PubMed] [Google Scholar]
- 3.Payne WK, Ogilvie JW, Resnick MD, et al. Does scoliosis have a psychological impact and does gender make a difference? Spine 1997; 22:1380–1384. [DOI] [PubMed] [Google Scholar]
- 4.Pham VM, Houlliez A, Caprentier A, et al. Determination of the influence of the Cheneau brace on quality-of-life for adolescent with idiopathic scoliosis. Ann Readapt Med Phys 2007; 51:3–8. [DOI] [PubMed] [Google Scholar]
- 5.Matsunaga S, Hayashi K, Naruo T, et al. Psychologic management of brace therapy for patients with idiopathic scoliosis. Spine 2005; 30:547–550. [DOI] [PubMed] [Google Scholar]
- 6.Sapountzi-Krepia DS, Psychogiou M, Peterson D, et al. The experience of brace treatment in children/adolescents with scoliosis. Scoliosis 2006; 1:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Danielsson AJ, Hasserius R, Ohlin A, et al. Health-related quality of life in untreated versus brace-treated patients with adolescent idiopathic scoliosis: a long-term follow-up. Spine 2010; 35:199–205. [DOI] [PubMed] [Google Scholar]
- 8.Danielsson AJ, Hasserius R, Ohlin A, et al. Body appearance and quality of life in adult patients with adolescent idiopathic scoliosis treated with a brace or under observation alone during adolescence. Spine 2012; 37:775–862. [DOI] [PubMed] [Google Scholar]
- 9.Danielsson AJ, Wiklund I, Pehrsson K, et al. Health-related quality of life in patients with adolescent idiopathic scoliosis: a matched follow-up at least 20 years after treatment with brace or surgery. Eur Spine J 2001; 10:278–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Noonan KJ, Dolan LA, Jacobson WC, et al. Long-term psychosocial characteristics of patients treated for idiopathic scoliosis. J Pediatr Orthop 1997; 17:712–717. [PubMed] [Google Scholar]
- 11.Merenda L, Costello K, Santangelo AM, et al. Perceptions of self-image and physical appearance: conversations with typically developing youth and youth with idiopathic scoliosis. Orthop Nurs 2011; 30:383–390. [DOI] [PubMed] [Google Scholar]
- 12.Olafsson Y, Saraste H, Ahlgren R. Does bracing affect self-image? A prospective study on 54 patients with adolescent idiopathic scoliosis. Eur Spine J 1999; 8:401–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tones M, Moss N, Polly DW. A review of quality-of-life and psychosocial issues in scoliosis. Spine 2006; 31:3027–3038. [DOI] [PubMed] [Google Scholar]
- 14.Weinstein SL, Dolan LA, Wright JG, et al. Design of the Bracing in Adolescent Idiopathic Scoliosis Trial (BrAIST). Spine 2013; 38:1832–1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carreon LY, Sanders JO, Polly DW, et al. Spinal appearance questionnaire: factor analysis, scoring, reliability, and validity testing. Spine 2011; 36:1240–1244. [DOI] [PubMed] [Google Scholar]
- 16.Cash TF. Body Image: A Handbook of Science, Practice, and Prevention. 2nd ed.New York, NY: The Guilford Press; 2011. [Google Scholar]
- 17.Roy-Beaudry M, Beausejour M, Joncas J, et al. Validation and clinical relevance of a French- Canadian version of the Spinal Appearance Questionnaire in Adolescent Patients. Spine 2011; 36:746–751. [DOI] [PubMed] [Google Scholar]
- 18.Sanders JO, Harrast JJ, Kuklo TR, et al. The Spinal Appearance Questionnaire: results of reliability, validity, and responsiveness testing in patients with idiopathic scoliosis. Spine 2007; 32:2719–2722. [DOI] [PubMed] [Google Scholar]
- 19.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory Version 4.0 Generic Core Scales in healthy and patient populations. Med Care 2001; 39:800–812. [DOI] [PubMed] [Google Scholar]
- 20.Choate LH. Toward a theoretical model of women's body image resilience. J Couns Dev 2005; 83:320–330. [Google Scholar]
- 21.Larouche SS, Chin-Peuckert L. Changes in body image experienced by adolescents with cancer. J Ped Oncol Nurs 2006; 23:200–209. [DOI] [PubMed] [Google Scholar]
- 22.Lee MY, Mu PF, Tsay SF, et al. Body image of children and adolescents with cancer: a metasynthesis on qualitative research findings. Nurs Health Sci 2012; 14:381–390. [DOI] [PubMed] [Google Scholar]
- 23.Olafsson Y, Saraste H, Ahlgren R. Does bracing affect self-image? A prospective study on 54 patients with adolescent idiopathic scoliosis. Eur Spine J 1999; 8:401–405. [DOI] [PMC free article] [PubMed] [Google Scholar]


