Abstract
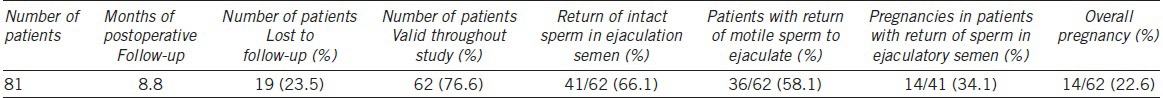
Vasoepididymostomy (VE), as the most challenging procedure in microsurgeries, is often carried out with a double-armed two-suture technique. In this study, we evaluated the efficacy and safety of the single-armed two-suture VEs on humans and studied the factors that could possibly affect the patency rates. From July 2012 to July 2013, we reviewed 81 patients with consecutive primary epididymal obstruction who underwent single-armed two-suture longitudinal intussusception microsurgical VEs by a single surgeon, Kai Hong (KH). At the same time, we analyzed seven factors that possibly related to the patency rates. With the single-armed technique, a total of 81 men underwent the microsurgical VEs. Data on 62 patients were completely recorded. 19 patients were lost to follow-up. Mean age was 31 years old. Mean follow-up time was 8.8 (2-17) months. The patency rate was 66.1% (41/62). Natural pregnancy rate was 34.1% (14/41). Overall pregnancy rate was 22.6% (14/62). No severe surgical complications were noted. With logistic regression test analysis, there were two factors related to a higher patency rate: anastomosis sites (P = 0.035) and motile sperm found in the epididymal fluid (P = 0.006). Motile sperm found in the epididymal fluid were associated with a higher patency rate (OR = 11.80, 95% CI = 1.79, 77.65). The single-armed two-suture longitudinal VE technique is feasible for microsurgical practice. The patency and pregnancy rates are comparable to the doubled-armed technique. Anastomosis sites and motile sperm found in the epididymal fluid were the most two important factors related to higher patency.
Keywords: male infertility, microsurgery, obstructive azoospermia, vasoepididymostomy
INTRODUCTION
Approximately 10% to 15% of infertile men suffer from azoospermia. Obstructive azoospermia is mostly associated with bilateral obstruction of the vas deferens and epididymis. With recent advancement and rapid developments in reproductive medicine, especially in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) combined with male infertility microsurgeries and sperm extractions from testis or epididymis, many previously untreatable azoospermia patients can father their own children. However, it is important to evaluate the male infertility comprehensively prior to IVF/ICSI. Otherwise, IVF/ICSI may result in more serious male infertility or urological issues, and increase medical costs for patients. Moreover, it could involve additional risks for the female partner during the whole process of medical preparation and IVF/ICSI.
Microsurgical vasoepididymostomy (VE) is technically the most challenging procedure of all microsurgeries. Recent innovations in VE reduced the critical demands on performing an anastomosis from the vas deferens to an epididymal tubule but showed excellent results as well with much better patency and paternity rates.1 Chan and his colleagues from Cornell first reported the double-armed two-suture technique of longitudinal intussusception microsurgical VE, which has become a “gold standard”.2,3 Nevertheless, suitable and cost-effective high-quality double-armed micro-sutures with a length of <2.5 cm (to 3 cm) for male infertility microsurgeries are not easy to obtain outside the United States, and these sutures are a critical factor for the outcomes of the VEs. For the above reason, Monoski et al. also from Cornell described a novel single-armed technique in rats and achieved similar results to the standard double-armed technique for VEs.4 Zhao et al. from China clinically confirmed the advantages of using the single-armed suture technique in humans with 17 epididymal obstructive azoospermia patients in 2013.5 Besides Zhao, there has been one more report by Binsaleh of 22 cases with the single-armed suture technique in 2014.6 Average patency rates in their articles were 58% and 59%, respectively. However, data from their studies were limited to a relatively small number of patients.
In this study, we researched our operative data and outcomes of the single-armed two-suture VEs from July 2012 to July 2013, and extensively investigated possible factors that could affect the patency rate of the single-armed VE technique.
MATERIALS AND METHODS
Patients
From July 2012 to July 2013, we retrospectively gathered the data from 81 consecutive primary epididymal obstruction patients (none of the patients’ epididymal obstruction was secondary to a vasectomy), who underwent the single-armed two-suture microsurgical vasoepididymostomies by a single surgeon in one medical center (Kai Hong, Peking University Third Hospital, Beijing, China).
Presurgical preparations
Documented data included technique descriptions, medical history (in particular any history of urinary or genital infection such as epididymitis), time of follow-ups, semen analyses (WHO 1999 criteria), and outcomes of patency and pregnancy. Azoospermia was confirmed by at least two semen analyses before the surgery. In all patients’ semen samples, the volume, pH value, and the seminal plasma fructose were within normal ranges. There were no specific abnormal physical and pathological conditions in any patient's physical exams. The range of testicular volume was from 12 to 25 ml. Serum testosterone (T), follicle-stimulating hormone (FSH), luteinizing hormone (LH), and prolactin (PRL) were all within normal ranges. There were no abnormal findings of the prostate, seminal vesicles, or ejaculatory ducts in any patient's trans-rectal ultrasound exams. All patients’ female partners were <39 years old.
Macrosurgical preparations
The patients were laid in the supine position applied with general anesthesia. The macrosurgical procedures were done through bilateral vertical scrotal incisions. Biopsy or vasogram before microsurgeries was performed irregularly.
Microsurgical preparations and procedures
The microsurgical procedures were performed with an operating microscope (Carl Zeiss, S88, Germany) with the maximum magnification power of ×20. The standard microsurgical instruments, including micro-bipolar electrocautery, were used during the operation.
As the microsurgical procedure started, testes, epididymis, vas deferens, and the location of epididymal obstruction were examined, then the proper site and the level of the epididymis for anastomosis were identified. Most of the time, we could see the epididymal tubules of different sizes either beyond or beneath the obstructive site. The epididymal tubules beyond the obstructive site with sperm inside often looked full and pale.
Under the ×20-power magnification, the vas deferens (also called the vas) was hemitransected until the lumen was seen. Vassal fluid from the lumen of the vas was examined microscopically. If there was no sperm, vasography should be performed. The end of the vas toward the seminal vesicles was then cannulated with a 24-gauge angiocatheter. At this point, diluted methylene blue was injected to confirm patency of the proximal vas deferens. At the same time, the blue color from the above could be seen in the indwelling urinary catheter.
The epididymal tunic was opened with an incision that was identical in size to the vas deferens. In order to decrease the tension of anastomosis, the vas deferens was transected and well-prepared before it was brought closer to the epididymis. A single full epididymal tubule was microsurgically dissected and prepared for the anastomosis. Four microdots were marked with a fine-tip micro-marking pen (Skin marker, fine tip, MedPlus Inc.) at the 1, 5, 7, and 11 o’clock positions on muscular layer of the vas deferens (Figures 1a and 1b, 2a). To reduce the tension for next anastomosis, the vas deferens was sutured to the edge of the epididymal tunic with one 8-0 prolene (W2777, length 6.5 mm, diameter 6 mil, 3/8C, Ethicon) stitch at the 6 o’clock position of the vas. Two single-armed 10-0 (W2790, length 3.8 mm, diameter 3 mil, 3/8C, Ethicon) or 9-0 (W2780, length 4.7 mm, diameter 6 mil, 3/8C, Ethicon) prolene sutures were used to perform longitudinal intussusception. Due to difficulties in accessing appropriate microsurgical sutures, we initially used 9-0 prolene sutures for VEs before 10-0 prolene sutures became commercially available in our hospital, which were listed with case numbers in Table 2. While this single-armed microsurgical VE technique was first reported by Monoski,4 we made a minor modification (Figure 1a and 1b) in our operating procedure. The first suture was placed with an outside-in approach through the mucosal layer of the vas deferens at microdot a1 (Figure 1a), and the second suture was placed at microdot b1. Both needles passed through the epididymal tubule longitudinally but were not completely drawn out. The epididymal tubule lumen was then gently cut longitudinally between the two needles, and the fluid was taken for sperm examination. (Ideally, the sperm should be cryopreserved. Unfortunately, we were not able to cryopreserve the sperm yet at our hospital due to lack of facilities at the time. There are current efforts to establish a sperm bank in our hospital). When sperm were identified microscopically, two needles were carefully pulled out and placed through the mucosal layer of the vas deferens with an inside-out approach at microdot a2 and b2, respectively (Figure 1b) (Figure 2a–2d). Before the two sutures were tied together, an 8-0 prolene was sutured to the vas at the 12 o’clock position and to the epididymal tunic in order to release the tension. After the two 10-0 prolene sutures were tied down, the epididymal tubules were intussuscepted into the lumen of the vas deferens. The anastomosis was then supported by an outer layer of 14 stitches with 8-0 prolene sutures as a standard procedure.
Figure 1.
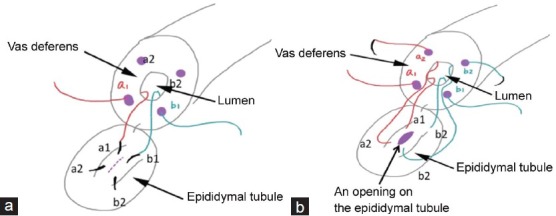
Placement of sutures in our single-armed two-suture technique for microsurgical vasoepididymostomy.
Figure 2.
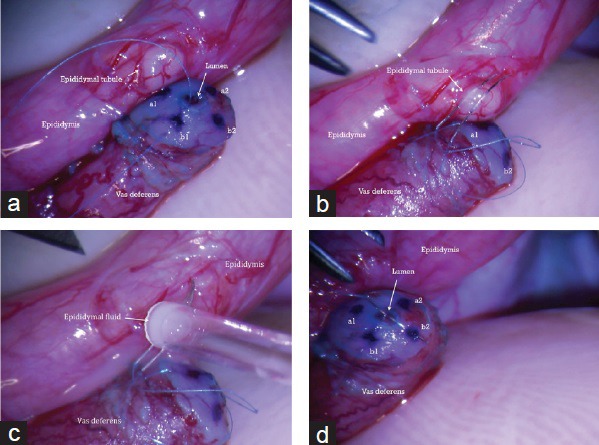
Single-armed two-suture technique. a. epididymal tube showed clearly. b. placement of two sutures in epididymal tube. c. epididymal fluid was taken for sperm examinination. d. When sperm were identified, two needles were carefully pulled out and placed though the mucosal layer of the vas deferens with an inside-out approach at microdot a2 and b2, respectively.
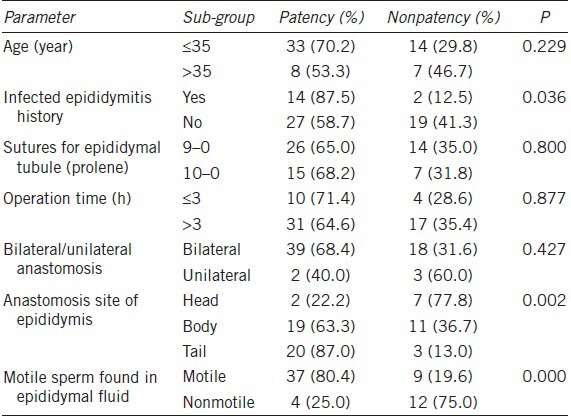
Table 2.
Comparative data of patients
Postoperative care
Postoperative patients were required to wear tight underwear as scrotal support. Antibiotics were administered once on the day of the surgery, and no more medication was needed. The patients were discharged in 3–5 days postoperatively. Within the first month, they were instructed not to engage in any strong physical activities. Ejaculation and sexual intercourse were not recommended within 30 days after the surgery. From the second month, the patients were encouraged to have sexual intercourse at least twice a week. We asked patients to undergo postsurgery semen analyses in our center in 1 month and 3 months. If the patents could not return in the first month, they must have come back once in 3 months to undergo at least one postoperative semen analysis for inclusion in this study. Return of sperm in ejaculation was defined as intact whole sperm found in a semen analysis after surgery. If sperm was not found after 3 months, the patient was recommended to continue a monthly semen analysis until the sixth month. If the sperm was still not found after 6 months, we recommended the patients to do a semen analysis every 3 months till the twelfth month, because the return of sperm in ejaculate following VEs normally takes longer than a routine vasovasostomy. For some reasons related to the Chinese culture, a majority of infertile patients would not wait for a long time postoperatively before they approached other infertility treating options. Normally, we recommended IVF to the couples who meet the following criteria: no sperm was found in semen analyses in more than 12 months after the surgery along with issues associated with the female partners’ age (>34 years).
Methods of follow-ups
Multiple follow-up methods were used, like telephone calls, text messages, etc., 23.5% (19/81) of patients were lost to follow-up and were not included in further analyses. Patients who did not respond to our phone calls or text messages were classified into the group lost to follow-up. Follow-ups were very difficult in this population because the patients were from different places all over China. It is worthwhile to note that the patients who failed VE surgeries were most likely to come back for IVF/ICSI. Because of the Chinese culture, many patients did not want anyone to know that they were undergoing male infertility related surgeries. Some patients even changed their mobile phone numbers. Considering that some patients refused to participate in the follow-ups, the actual patency and pregnancy rates would have been slightly higher if all patients’ follow-up data had been included.
Statistical analysis
SPSS 20.0 (IBM) was used to analyze the data. We analyzed age (younger or older than 35 years), previous history of epididymitis, sutures used for epididymal tubules (9-0 or 10-0 prolene), operation time (shorter or longer than 3 h), bilateral or unilateral anastomosis, anastomosis sites (the head, body or the tail of the epididymis), and epididymal fluid (motile sperm or not). Chi-square test was used for single factor analysis and logistic regression for multiple factor analysis. P < 0.05 was considered statistically significant.
RESULTS
From July 2012 to July 2013, totally 81 consecutive epididymal obstruction azoospermia patients, who underwent microsurgical vasoepididymostomy with single-armed two-suture technique, were enrolled in the study. 19 patients were lost to follow-up (23.5%, 19/81). 62 patients’ data were collected into the final statistical analysis. The mean age of patients was 31 (23~45) years old. The mean follow-up time was 8.8 (2–17) months. One patient informed us about his wife's natural pregnancy 2 months after the surgery. The patency rate was 66.1% (41/62). There were 36 patients (36/62, 58.1%) with return of motile sperm to ejaculate. Among these 36 patients, the mean concentration of sperm was 17.1 million ml−1 (ranging from several to 51.8 million ml−1), with a forward motility rate of 24% (ranging from 0% to 52%) and a normal morphology of 2% (ranging from 0% to 8%). The pregnancy rate of patients with the return of sperm seen in the ejaculated semen was 34.1% (14/41). The overall pregnancy rate was 22.6% (14/62). Five patients’ partners delivered babies during this study. Seven patients’ partners were pregnant after further IVF treatment using sperm extracted from their husband's semen samples. All seven of these patients and their partners stopped waiting for a natural pregnancy between the sixth month and the twelfth month. The reason why these patients stopped waiting was related to social factors and the pressure from their surrounding environment. If there were no sperm found in the ejaculatory semen in 12 months after the surgery, we recommended IVF to the patient as the next step. No severe surgical complications were noted. One case of mild hematoma occurred, but the problem was resolved with conservative treatment. One patient suffered epididymitis in 6 weeks postoperatively, along with failure in patency, then he was treated with antibiotics and recovered afterward. We recommended this patient to undergo IVF (Table 1).
Table 1.
Data of patients
With the single-factor analysis, there were three factors related to a higher patency rate: the history of epididymitis, the anastomosis site, and the motile sperm found in the epididymal fluid (P = 0.036, 0.002, and 0, respectively). With the analysis of logistic regression test, there were two factors related to a higher patency rate: the anastomosis site (P = 0.035) and the motile sperm found in the epididymal fluid (P = 0.006). During the surgical procedures, motile sperm found in the epididymal fluid was related to a higher patency rate (OR = 11.80, 95% CI = 1.79, 77.65) (Table 2).
DISCUSSION
Although IVF/ICSI can help many infertile men including azoospermia patients to father their own children, treating male infertility with microsurgical approaches including vasoepididymostomy still should be considered as one important option available for epididymal obstruction azoospermia patients. The disadvantages of bypassing any evaluation of the microsurgeries to treat male infertility and directly undergoing IVF/ICSI include an increased unnatural pregnancy rate, higher medical costs, and more risks for the female partners.
Microsurgical reconstruction of the male reproductive tract with vasovasostomy and vasoepididymostomy has been demonstrated by various studies to be a more cost-effective treating option with good outcomes comparable to the upfront assisted reproductive technologies with IVF/ICSI. The average patency rate of VEs varies from 50% to 90%. It is known that technically VE is a challenging microsurgery, however, the advantages of the microsurgical VE are obvious if the surgeon has extensive microsurgical training on male infertility. To performing a good VE, extreme precision and exquisite microsurgical skills are required for the surgeon to anastomose the delicate epididymal tubule to the vassal lumen. The outcomes highly depend on the surgeon's skills, experience, and previous microsurgical training.7,8
Many surgeons have adapted the double-armed two-suture longitudinal intussusception vasoepididymostomy as the “gold standard” especially in the United States. It is easier for a surgeon to avoid suturing the back wall of the vassal lumen with the inside-out fashion. However, the specialized double-armed sutures (10-0, 2.5 to 3 cm or less in length) with good needle quality are hard to obtain and extremely expensive outside the United States. Monoski and her Cornell colleagues reported the use of the single-armed suture technique for VEs in a well-controlled animal study, and they found there was no significant difference compared to the double-armed technique, but it could reduce the cost of sutures significantly.4 The first single-armed suture technique for VEs in humans was reported by Zhao et al. in 20135 and he obtained good outcomes with a 58.8% patency rate. Binsaleh6 reported similar results, showing a 59% patency rate and 36% pregnancy rate.
It seems that the patency rates with the single-armed suture technique for VEs in both reports5,6 were unexpectedly lower than the double-armed technique. This could be associated with multiple factors such as number of cases, different etiological causes of epididymal obstruction, and different microsurgical modifications or microsurgical materials.
To avoid any possible bias, to gather more accurate surgical outcomes, and to reduce any technical difference, all VE procedures in this study were performed by a single surgeon (KH). Our results showed the patency rate was 66.1% (14/62) while the overall pregnancy rate was 22.6% (14/62). Our patency rate for the single-armed suture technique was close to the double-armed technique,9 and was slightly higher than the previous reports of the single-armed VEs.5,6 As Chan reported, patency with the double-armed sutures was 73% in 1 to 1.5 months, and the totally patency rate was 92% with an average follow-up time of 16.3 months.3 In this study, 8.8 (2–17) months of the mean follow-up time was shorter than many reports. Hypothetically, we could predict that the patency rate would increase with a longer period of follow-ups. We believe that the single-armed technique is a highly acceptable and cost-effective technique with similar patency rates to the standard double-armed technique.
Although the microsurgical technique and skills of the surgeon are the most critical factors for the success of a microsurgical VE, some other factors may also influence the result of patency. In our study, in order to investigate the factors that influenced the patency rate, we chose seven parameters to evaluate their relationships with the prognosis of the single-armed technique for VEs, including patients’ age, history of epididymitis, operating time, types of sutures used, whether the VE surgery was bilateral or unilateral, anastomosis sites of the epididymis, and motile sperm in the epididymal fluid during the surgery.
It has been well-documented that the quality of semen decreases along with the patients’ age and the time length of vassal obstruction. In this study, the patency rate in the age group of 23 to 35 years old was 70.2% (33/47); and was 53.3% (8/15) for the age group ranging from 35 to 45 years old, although there was no statistical difference between the two groups. The decreased quality of semen along with aging, however, did not show relationships between age and patency rates. That is to say, when we prepare to undergo VEs for future epididymal obstruction patients, we should pay more attention to the age of their female partners than to the male patients’ age.
The etiology of epididymal obstruction is significantly different between patients in the United States and China. Vasectomy is the most commonly performed urological procedure in the United States. Therefore, in the United States, most epididymal obstruction patients were secondary of vasectomy. In China, there are more patients whose epididymal obstruction was idiopathic or due to infected epididymitis.10 It is not easy to compare the VE patency rates between the two countries because of the huge difference in etiology of epididymal obstruction and the history of epididymitis. Since the bacterial infection related epididymal obstruction can result in multiple blockage sites along the epididymis, some interesting topics have arisen regarding how to manage potential epididymal infection before and after VEs in China. In our study, the patency rate with a history of epididymitis seemed higher than the patients without epididymitis (87.5%, 14/16 and 58.7%, 27/46, P = 0.036), which made the interpretation rather challenging. We assumed that the reason for this result might be that the history of epididymitis only caused a singular obstruction while the idiopathic epididymal obstruction was related to multiple pathologic changes.
In this study, the operating time was similar among patients and there was no significant statistical difference in the patency rates between two sub-groups (OP time ≤3 h: 71.4%, 10/14; OP time >3 h: 64.6%, 31/48; P = 0.877). It suggested that the operating time might not be a key for VEs regardless of the use of single-armed or double-armed sutures. When undergoing VEs, the surgeons should focus on the procedures but not the speed of the procedures.
Single-armed 9-0 and 10-0 prolene sutures were used in the operating steps of the epididymal tubules, which had been slightly modified from the procedures in Monoski's report.4 Due to some difficulties to access appropriate microsurgical sutures, we initially used the 9-0 prolene sutures for VEs before the 10-0 prolene sutures became commercially available in our hospital. After gradually switching to the 10-0 prolene sutures, we currently use these in all VE operations. Although there was no significant difference in the patency rates between the two sub-groups (9-0 prolene suture: 65.0%, 26/40; 10-0 prolene suture: 68.2%, 15/22; P = 0.8), we still prefer to use the single-armed 10-0 prolene. Compared to the 9-0 prolene sutures, the 10-0 needle is much easier to pierce and penetrate into the epididymal tubules. The finer needle we used left more suture placement space to create an opening on a selected epididymal tubule between the two needles and also made a smaller needle hole that may reduce the chance of sperm leakage.
Unlike the prolene suture material, nylon sutures may have less tissue reactions or be more cost-effective. Sheynkin reported that nylon suture had a better patency rate and less tissue reactions compared to the prolene suture.11 Unfortunately, nylon microsurgical 10-0 sutures for male infertility microsurgeries are currently unavailable in China. We believe that prolene is still a good choice for VEs if suitable nylon sutures are unavailable.
In this study, only five patients underwent unilateral VEs and showed a patency rate of 40.0% (2/5), which was much lower than the bilateral group 68.4% (39/62).
The recorded diameter of the epididymal tubule was different due to various operating sites on the head, the body, or the tail of the epididymis. The tubule size at the tail was larger and also easier to perform microsurgical VE procedures. In this study, we showed the different patency rates with various surgical sites on the head, the body, and the tail, respectively (head: 22.2%, body: 63.3%, tail: 87.0%). Overall, our results were similar to the double-armed VE technique reported by Peng.11,12
Examination of the epididymal fluid intraoperatively was critical, after an opening was created by a pair of sharp tipped iris scissors or a sharp tipped micro-knife on the epididymal tubule. Pal found that more motile sperm indicated better results.13 In our study, the patency rate was significantly different if motile sperm was found (80.4% vs 25.0%). We also noticed more motile sperm in the epididymal fluid intraoperatively a better and higher VE patency rate could be predicted.
CONCLUSION
This is the first single surgeon report of multi-factor analytic clinical research on outcomes of single-armed two-suture longitudinal microsurgical vasoepididymostomies on humans. We believe that the single-armed suture technique for VEs is a cost-effective option, and its patency and pregnancy rates are comparable to the doubled-armed vasoepididymostomy technique.
COMPETING FINANCIAL INTERESTS DECLARATION
There was not any competing financial interest with this article.
REFERENCES
- 1.Goldstein M, Kim HH. Scrotal orchiopexy for adult retractile testis. In: Goldstein M, Schlegel PN, editors. Surgical and Medical Management of Male Infertility. New York: Cambridge University Press; 2013. pp. 157–60. [Google Scholar]
- 2.Chan PT, Brandell RA, Goldstein M. Prospective analysis of outcomes after microsurgical intussusception vasoepididymostomy. BJU Int. 2005;96:598–601. doi: 10.1111/j.1464-410X.2005.05691.x. [DOI] [PubMed] [Google Scholar]
- 3.Chan PT. The evolution and refinement of vasoepididymostomy techniques. Asian J Androl. 2013;15:49–55. doi: 10.1038/aja.2012.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Monoski MA, Schiff J, Li PS, Chan PT, Goldstein M. Innovative single-armed suture technique for microsurgical vasoepididymostomy. Urology. 2007;69:800–4. doi: 10.1016/j.urology.2007.01.091. [DOI] [PubMed] [Google Scholar]
- 5.Zhao L, Deng CH, Sun XZ, Chen Y, Wang WW, et al. A modified single-armed technique for microsurgical vasoepididymostomy. Asian J Androl. 2013;15:79–82. doi: 10.1038/aja.2012.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Binsaleh S. Two-suture single-armed longitudinal intussusception vasoepididymostomy for obstructive azoospermia: report of patients characteristics and outcome. Int Urol Nephrol. 2014;46:2271–7. doi: 10.1007/s11255-014-0835-6. [DOI] [PubMed] [Google Scholar]
- 7.Li PS, Kim H, Goldstein M. Microsurgical research and training for the male infertility. In: Goldstein M, Schlegel PN, editors. Surgery of Male Infertility. 2nd ed. New York: Cambridge University; 2013. ISBN-10: 0521881099, ISBN-13: 978-0521881098. [Google Scholar]
- 8.Mehta A, Li PS. Male infertility microsurgical training. Asian J Androl. 2013;15:61–6. doi: 10.1038/aja.2012.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schiff J, Chan P, Li PS, Finkelberg S, Goldstein M. Outcome and late failures compared in 4 techniques of microsurgical vasoepididymostomy in 153 consecutive men. J Urol. 2005;174:651–5. doi: 10.1097/01.ju.0000165573.53109.92. [DOI] [PubMed] [Google Scholar]
- 10.Peng J, Yuan Y, Cui W, Zhang Z, Gao B, et al. Causes of suspected epididymal obstruction in Chinese men. Urology. 2012;80:1258–61. doi: 10.1016/j.urology.2012.08.057. [DOI] [PubMed] [Google Scholar]
- 11.Sheynkin YR, Li PS, Magid ML, Carlson D, Chen EC, et al. Comparison of absorbable and nonabsorbable sutures for microsurgical vasovasostomy in rats. Urology. 1999;53:1235–8. doi: 10.1016/s0090-4295(99)00022-9. [DOI] [PubMed] [Google Scholar]
- 12.Peng J, Yuan Y, Zhang Z, Gao B, Song W, et al. Patency rates of microsurgical vasoepididymostomy for patients with idiopathic obstructive azoospermia: a prospective analysis of factors associated with patency – single-center experience. Urology. 2012;79:119–22. doi: 10.1016/j.urology.2011.09.034. [DOI] [PubMed] [Google Scholar]
- 13.Pal PC, Manocha M, Kapur MM, Rao DN, Sharma RS, et al. Obstructive infertility: changes in the histology of different regions of the epididymis and morphology of spermatozoa. Andrologia. 2006;38:128–36. doi: 10.1111/j.1439-0272.2006.00726.x. [DOI] [PubMed] [Google Scholar]


