Abstract
In the present study, we evaluated the safety and efficacy of immediate surgical bipolar plasmakinetic transurethral resection of the prostate (PK-TURP) for patients with benign prostatic hyperplasia (BPH) with acute urinary retention (AUR). We conducted a retrospective analysis of clinical data of BPH patients who received PK-TURP. A total of 1126 BPH patients were divided into AUR (n = 348) and non-AUR groups (n = 778). After the urethral catheters were removed, the urine white blood cell (WBC) count in the AUR group significantly increased compared with the non-AUR group (P < 0.01). However, there was no significant difference in international prostate symptom score, painful urination, and maximal urinary flow rate. The duration of hospitalization of the AUR group was longer than that of the non-AUR group (P < 0.001). A total of 87.1% (303/348) patients in the AUR group and 84.1% (654/778) patients in the non-AUR group completed all of the postoperative follow-up visits. The incidence of urinary tract infection in the AUR group within 3 months after surgery was significantly higher than that in the non-AUR group (P < 0.01). The incidence of temporary urinary incontinence in the AUR group did not exhibit significant difference. During 3–12 months after surgery, there were no significant differences in major complications between the two groups. Multivariate regression analyses showed that age, postvoid residual, maximal urinary flow rate, diabetes, and hypertension, but not the presence of AUR, were independent predictors of IPSS post-PK-TURP. In conclusion, immediate PK-TURP surgery on patients accompanied by AUR was safe and effective.
Keywords: acute urinary retention, benign prostatic hyperplasia, lower urinary tract symptoms, plasmakinetic transurethral resection of the prostate
INTRODUCTION
Acute urinary retention (AUR) is one of the most serious and painful events during the natural progression of benign prostatic hyperplasia (BPH). Its major feature is the sudden inability to urinate, accompanied by painful urination. Thus, the disease typically requires emergency catheterization.1 AUR causes stress, anxiety, pain, and discomfort in the patients. Its influence on patient quality of life resembles that of renal colic.2 BPH is considered the most dominant cause of AUR, and AUR is considered to be part of the natural progress of BPH and an absolute surgical indicator of BPH.3 However, the desire of the patients to avoid surgery and the development of an effective drug treatment have resulted in a more conservative AUR treatment, which represents a substantial therapeutic change over the last decade.4 More and more treatments use trial without catheter (TWOC) combined with α1A blockers, which forms the basis of this change.5,6,7
TWOC includes the conventional use of α1A blockers for 2–3 days. After urethral catheters are removed, more than 60% of patients can restore urination.5 A large cross-sectional study demonstrated that the performance of TWOC after AUR occurrence was the primary treatment method worldwide. In addition, the combination of TWOC with α1A blockers could double the success rate.4 This TWOC treatment strategy might be based on a research report that unnecessary immediate surgical treatment of AUR might increase the death rate of patients within 30 days and result in increased postoperative complications.8,9 As a result, the number of transurethral resections of the prostates (TURPs) on patients with the first onset of AUR has gradually decreased in several countries in recent years.4,10 However, more patients may face the risk of AUR recurrence at any time.11,12
TURP is considered to be the gold standard with respect to the surgical treatment of BPH. However, TURP's complications, such as transurethral resection symptoms (TURS), postoperative hemorrhage, and reoperation, continue to represent a clinical challenge.13,14 Several clinical studies have demonstrated that bipolar plasmakinetic transurethral resection of the prostate (PK-TURP) is an alternative to TURP. Compared with traditional TURP, PK-TURP's surgical effects were the same. However, PK-TURP had fewer complications, a shorter hospitalization time, and lower costs.15,16,17 Therefore, this retrospective study analyzed the data of BPH patients treated with PK-TURP to compare the efficacy and safety of PK-TURP treatment in BPH patients with or without AUR.
MATERIALS AND METHODS
Patient data
Between January 2006 and June 2012, a total of 1299 patients received surgical PR-TURP in the Department of Urinary of our hospital. Of these patients, the data of 1126 BPH patients were included in this study. The inclusion criteria were (1) BPH patients older than 50 years of age with a maximal urinary flow rate (Qmax) ≤10 ml s−1 and an international prostate symptom score (IPSS) ≥18; (2) BPH patients older than 50 years of age who had undergone an ineffective drug treatment or had refused drug treatment. Patients with neurogenic bladder dysfunction, a history of prostate or urethral surgery, and prostate cancer determined by preoperative biopsy or postoperative histopathological examination were excluded from this study. Immediate surgery is defined as surgery conducted within 3–7 days of the placement of indwelling catheters during AUR. AUR patients who did not receive immediate PK-TURP were also excluded from the study.
Preoperative evaluation
All patients received an examination assessment related to systemic conditions and medical specialties before surgery. The examination of systemic conditions included liver and kidney function, a routine blood test, electrolytes, blood sugar, pulmonary X-ray, electrocardiogram, and B-mode ultrasound scanning of the liver, gallbladder, pancreas, spleen, and kidneys. Certain patients additionally received ambulatory electrocardiography, color echocardiography or digital subtraction angiography (DSA), a lung function test, brain computed tomography (CT), or magnetic resonance imaging (MRI). The specialty-related evaluation included the IPSS, a quality of life score (QoL), Qmax, serum-free prostate-specific antigen (fPSA) and total PSA (tPSA) detection, postvoid residual (PVR) detection, and transrectal ultrasound (TRUS). A secondary TRUS prostate biopsy was performed in cases of the negative initial result but with persistently elevated PSA value. Certain patients also received urodynamics, cystourethroscopy, and transrectal prostate biopsy examinations. The PVR and Qmax of patients suffering from AUR were calculated using the detected values within 6 months of the visit, whereas the PSA value was the detected value of collected blood samples without catheterization. PVR was the bladder residual urine volume detected in patients after voiding by the same doctor using a bladder scanner. Urinary tract infection (UTI) was diagnosed based on (1) positive urine culture; (2) negative urine culture but with obvious clinical symptoms and increased urine white blood cell (WBC) count. Co-morbidities were evaluated using the Charlson comorbidity index (CCI) (http://touchcalc.com/calculators/cci_js).
Preoperative treatment
The BPH patients were primarily elderly patients. They typically exhibited one or more diseases of other organs. Therefore, they required multidisciplinary assistance and treatment prior to surgery. The preoperative blood pressure of patients with hypertension was controlled under 150/90 mmHg. The fasting and postprandial blood glucose levels of patients with diabetes were controlled under 8 and 10 mmol l−1, respectively. Seven patients (0.62%) had temporary cardiac pacemakers inserted on the day of surgery. Urethral catheters were placed in AUR patients with postrenal insufficiency caused by bladder outlet obstruction (BOO) for 5–7 days, significantly improving kidney function. Surgery for patients with a history of stroke, brain hemorrhage, and myocardial infarction was performed after the diseases were stable for 6 months and discussed with appropriate specialist physicians. All of the patients received a rigorous preoperative assessment by anesthesiologists and surgeons.
Surgical treatment
The surgical method was PK-TURP. The patients were provided antibiotics before surgery and received continuous epidural anesthesia or tracheal intubation general anesthesia using the lithotomy position. The urethral catheters of the patients who had indwelling catheters because of AUR were removed. Routine disinfection was conducted, and sterile drapes were applied. The bipolar transurethral resection system (Gyrus Medical Ltd, Cardiff, UK) was used. The resection power was set at 160 W, and the coagulating power was set at 80 W. Surgeries were performed by two urologists with extensive experience in the transurethral field. The procedures of surgical resection were consistent. First, the F27 resectoscope was placed into the bladder under video monitoring to observe the condition of the urethra, external sphincter, seminal colliculus, prostate, bladder neck, double urethral opening, and inside the bladder cavity. Next, resection was conducted at the bladder neck from the 5 o’clock position to the 7 o’clock position. The depth reached the prostatic capsule, and a marker ditch was made at the seminal colliculus. The left and right lobes of the prostate were transected clockwise, and finally, the prostatic apex was trimmed. At the end of surgery, the prostate debris inside the bladder cavity was removed using an Ellik evacuator. Before the resectoscope was removed, the transection wound of the prostate was examined. If active bleeding was obvious, hemostasis was conducted. Finally, the resectoscope was removed, and the passive voiding condition was observed. An F20 three-channel balloon catheter was placed, the normal saline solution was connected to continuously irrigate the bladder, and the patient was returned to the ward. The irrigation was discontinued when the washing fluid became clear, and urethral catheters were removed when the urine was clean.
Evaluation of efficacy and follow-up
The perioperative indicators that were detected included operative time, changes in the levels of serum sodium ion and hemoglobin (Hb), TURS, duration of bladder irrigation, duration of catheter placement, and hospitalization duration. The postoperative evaluation was performed on discharge and 3, 6, and 12 months after the operation. The evaluation indicators included routine urine analysis, IPSS, QoL, Qmax, and PVR. The PSA value was measured once 12 months after the operation. All of the intraoperative and postoperative adverse events were recorded. Postoperative complications were recorded and graded using the Clavien-Dindo grading system (http://www.surgicalcomplication.info/templates_download.html).
Statistical analysis
Statistical analysis of data was performed using the SPSS 11.5 software (SPSS Inc., Chicago, IL, USA). The data were presented as x̄ ± s. The comparison of means between two samples was performed using the unpaired t-test. The comparison of two proportions was performed using the Chi-square test. Stepwise multivariate regression analyses were performed to determine which variables explained unique variance in IPSS at 3 months and 12 months post PK-TURP, respectively. The significance level of this study was set at two-sided α = 0.05.
RESULTS
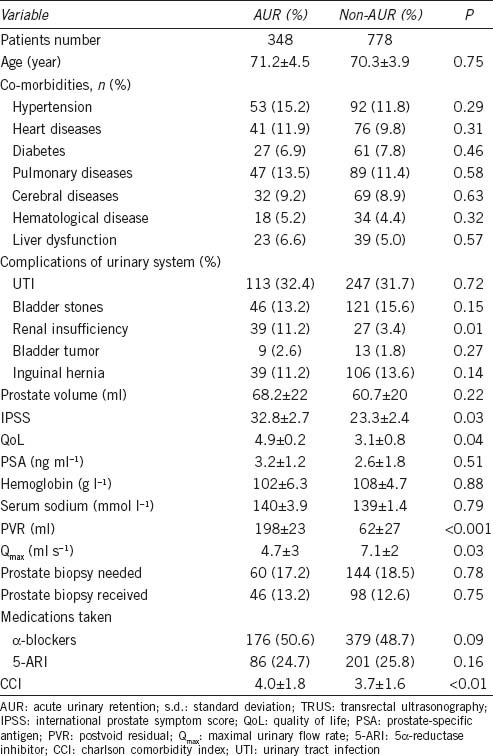
The average age of the 1126 patients was 70.3 years (51–94 years), the average duration of LUTS was 62.8 months (1–360 months), and the mean prostate volume measured by TRUS was 60.8 ± 21 ml (31.5–126.3 ml). All of the patients received PK-TURP surgery. As shown in Table 1, there were no significant differences preoperatively between the AUR (n = 348) and the non-AUR (n = 778) groups in age, prostate volume, hemoglobin, serum sodium, medications taken (α-blockers and 5α-reductase inhibitor), and distribution of co-morbidities and complications of the urinary system. The AUR group had significantly higher IPSS, PVR, and CCI score and lower Qmax than the non-AUR group preoperatively (P < 0.05). The PSA data of these two groups were not calibrated because of the use of 5α-reductase inhibitors. The combined examination results for the PSA value, digital rectal examination (DRE), and preoperative TRUS indicated that 204 (18.1%) patients required TRUS-guided prostate biopsy. However, only 144 (12.8%) patients actually received the biopsy. Nonetheless, there was no significant difference in the percentage of patients who received prostate biopsies in the two groups (P > 0.05) (Table 1).
Table 1.
Preoperative characteristics of patients with or without AUR
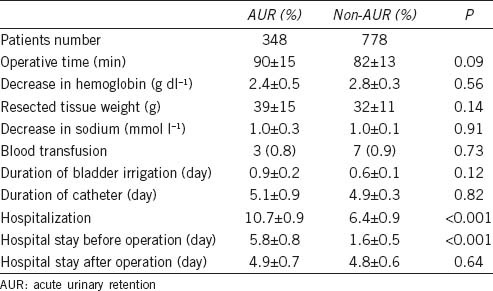
The operative time, intraoperative Hb, changes in sodium ion, resected prostate tissue weight, postoperative bladder irrigation duration, and duration of catheter placement between patients in these two groups did not have significant difference. As the AUR group had indwelling catheter for 3–7 days before surgery, while the non-AUR group received surgery 1–3 days after admission, the total hospitalization duration of the AUR group was longer than that of the non-AUR group (P < 0.001). However, the postoperative hospital stay between these two groups did not show a significant difference (P > 0.05) (Table 2). No serious perioperative adverse event occurred in either group.
Table 2.
Perioperative features of patients with or without AUR
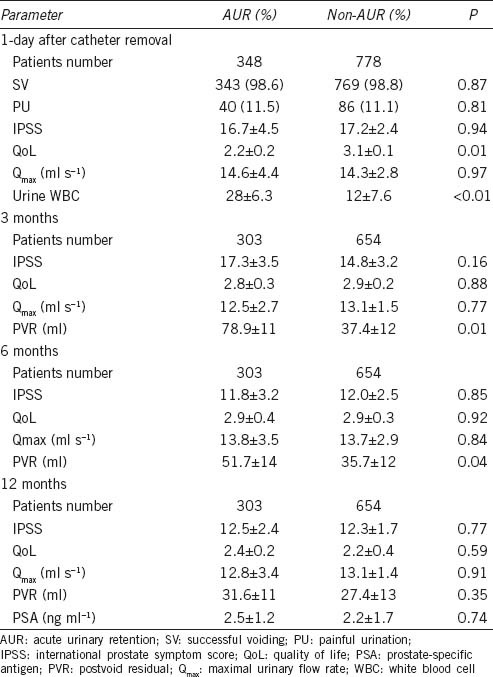
Patients in both groups could urinate on the first attempt after the urethral catheters were removed after surgery. However, there were five cases (1.4%) in the AUR group and nine cases (1.2%) in the non-AUR group in which difficulty voiding occurred at the second or third attempt after the catheters were removed. Thus, catheters were reinserted. In general, the catheters remained reinserted for 5–7 days. After the catheters were removed, the patients could naturally urinate. One day after removal of the catheter in the AUR group, the urine WBC count in the AUR group was significantly higher than that in the non-AUR group (28 ± 6.3 vs 12 ± 7.6, P < 0.01). There was no significant difference in IPSS, painful urination, Qmax, and urine RBC (red blood cell) count between the two groups. A total of 85% (957/1126) patients completed 3, 6, and 12 months of follow-up, including 87.1% (303/348) patients in the AUR group and 84.1% (654/778) patients in the non-AUR group. The number of patients who did not complete follow-up in the two groups did not have significant difference. The reasons for incomplete follow-up (n = 169, 15%) included the following: did not complete four follow-up visits (AUR: n = 21, 6.0% vs non-AUR: n = 57, 7.3%; P > 0.05), refused follow-up visits (AUR: n = 10, 2.8% vs non-AUR: n = 31, 3.9%; P > 0.05), loss of contact after discharge (AUR: n = 8, 2.3% vs non-AUR: n = 21, 2.6%: P >0.05), discovery of bladder tumor and prostate cancer (AUR: n = 3, 0.8% vs non-AUR: n = 8, 1.0%; P > 0.05), and death (AUR: n = 3, 0.8% vs non-AUR: n = 7, 0.8%; P > 0.05) (Table 3).
Table 3.
Follow-up data stratified by treatment
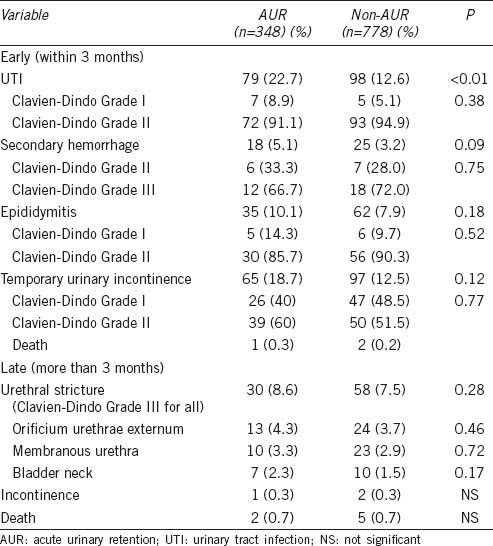
Regarding early complications (within 3 months after surgery), there were 12 cases (3.4%) of second hemorrhage in the AUR group and 25 cases (3.2%) in the non-AUR group. There was no significant difference between these two groups (P > 0.05). UTI was diagnosed based on (1) positive urine culture (in the AUR group, n = 26, 7.5%; in the non-AUR group, n = 11, 1.4%); (2) negative urine culture but with obvious clinical symptoms and increased urine WBC count (in the AUR group, n = 53, 15.2%; in the non-AUR group, n = 88, 11.3%). The incidence rate of UTI in the AUR group (n = 79, 22.7%) was significantly higher than that in the non-AUR group (n = 98, 12.6%) (P < 0.01). The incidence of temporary urinary incontinence in the AUR group (n = 65, 18.7%) was slightly higher than that in the non-AUR group (n = 97, 12.5%) but not significantly different (P = 0.09). During the subsequent 3–12 months of follow-up, there were 27 cases (8.9%) of urethral stricture in the AUR group and 68 cases (10.4%) in the non-AUR group. The most common locations were the orificium urethrae externum, membranous urethra, and bladder neck. The bladder neck stricture was usually treated with transurethral resection of the bladder neck scar, whereas the strictures in other locations were treated with urethral dilatation or direct visual internal urethrotomy. After treatment, all of the patients could void normally. Second incontinence was presented in one case in the AUR group and two cases in the non-AUR group. However, the major complications during the 3–12 months of follow-up between these two groups did not have a significant difference (Table 4). There were no significant differences between the AUR and the non-AUR groups in the grading of each of the early or late complications, as indicated by the Clavien-Dindo grades (Table 4).
Table 4.
Postoperative complications
During the 1 year of follow-up, 10 patients died. The causes were not associated with urological diseases. The major causes were cerebral hemorrhage and cardiovascular diseases. One case in the AUR group and two cases in the non-AUR group died within 3 months of surgery. There were seven cases of death during the 3–12 months of follow-up: two cases in the AUR group and five cases in the non-AUR group.
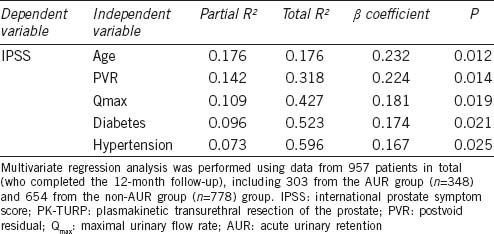
Stepwise multivariate regression analyses were performed to determine which variables explained unique variance in IPSS at 3 months and 12 months post-PK-TURP, respectively. The analysis results showed that among all variables listed in Table 1 plus the presence of AUR as an additional variable, age, PVR, Qmax, diabetes, and hypertension, but not the presence of AUR, were independent predictors of IPSS post-PK-TURP (P < 0.05), collectively explaining 0.510% and 0.596% of the variance in the IPSS at 3 months (Table 5) and 12 months (Table 6) post-PK-TURP, respectively.
Table 5.
Multivariate regression analysis of independent predictors of IPSS 3 months post-PK-TURP
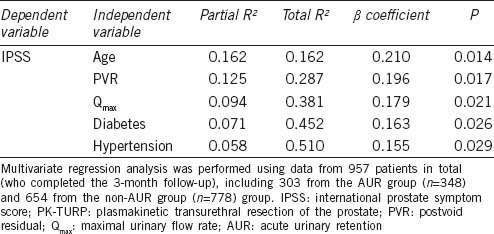
Table 6.
Multivariate regression analysis of independent predictors of IPSS 12 months post-PK-TURP
DISCUSSION
BPH is one of the most common chronic progressive diseases in aged males, and AUR is the most serious and painful complication that can occur during the natural progression of this disease. Once AUR appears, patients typical visit nearby community clinics or hospitals to receive urethral catheterization to empty the bladder and relieve the suddenly occurring pain.4,18,19,20 A consensus has not been reached regarding further treatment methods, such as how long the catheter should be placed, whether patients should be hospitalized, whether TWOC should be attempted, how patients are treated after TWOC, whether immediate surgery should be performed, and whether a1A blockers and antibiotics should be used and for how long after patients receive emergency treatment.4,18,19,21 The above considerations reflect the lack of established measures for the treatment of BPH with AUR, for which there are many underlying reasons.
After patients receive emergency catheterization, although the subsequent treatment strategies are not completely consistent, the current approach seems to rely on the combination on TWOC and a1A blockers.4,18 One study demonstrated that immediate surgery after the onset of AUR increased perioperative complications and death rates.8 Unfortunately, the success rate of TWOC after 1–3 days of AUR occurrence was lower than 40%.10,22 Although the extension of the TWOC period combined with the use of a1A blockers could increase the TWOC success rate, the extension of the TWOC period also increased a series of complications.4,10,23 Although TWOC frequently fails, many doctors continue to use TWOC.18 However, repeated TWOC not only increased hospitalization time and the economic burdens of the patients but also undoubtedly increased pain and complications. The more important issue was that although successful TWOC could smoothly eliminate the troubles caused by catheters, it remained unknown whether patients could void normally, how much LUTS was reduced, and how much QoL increased. Furthermore, patients faced the risk of AUR recurrence at any time.
In this study, 30.9% of BPH patients had AUR before receiving PK-TURP. These patients were hospitalized immediately after receiving emergency catheterization treatment and received surgical treatment within 3–7 days of catheterization. Compared with BPH patients without AUR in the same period, no death occurred in these groups during the perioperative period. In addition, the death rate within 30 days of surgery or during 12 months of follow-up between these two groups did not exhibit significant difference. Similarly, perioperative-related indicators, such as operative time, intraoperative Hb and serum electrolytes, the percentage of patients who require blood transfusion, postoperative irrigation duration, and the duration of catheterization also did not display significant difference between the two groups. However, the total hospitalization time of the AUR group was significantly longer than that of the non-AUR group, which was primarily associated with the extension of the preoperative preparation period of patients in the AUR group. In this study, after catheters were removed, the successful voiding rate of patients in the two groups reached more than 98.6%, and the percentage of patients who required a reinsertion of catheters was <1.5%. The percentage of patients in the AUR group that experienced painful urination after catheters were removed was slightly higher than that in the non-AUR group. However, the difference was not statistically significant. Previous studies demonstrated that the percentage of patients who could not urinate after TURP was between 3.0% and 12%,14,24,25,26,27 which was higher than that found in this study. The possible main explanation was that the postoperative catheterization duration in the patients studied here was longer (3–7 days). Another reason was that PK-TURP was performed in this study. Although the long postoperative catheterization time increased the hospitalization time of patients and the risk of UTI, it could reduce surgical wound inflammation and edema and was conducive to an improved recovery of postoperative detrusor functions. In fact, BOO caused by BPH could result in detrusor dysfunction.28,29 In addition, PK-TURP could obtain the same effect as TURP but had a lower incidence of complications than TURP.30,31
The incidence of postoperative hematuria, secondary hemorrhage, temporary urinary incontinence, epididymitis, and urethral stricture in the AUR group was slightly higher than that in the non-AUR group but did not exhibit statistical significance. As indicated by the Clavien-Dindo grades, there were no significant differences between the AUR and the non-AUR groups in the grading/severity of the complications. Urinary incontinence is the most disturbing postoperative symptom in BPH patients and has a substantial impact on patient QoL. It was reported that the incidence of urinary incontinence after TURP had a large variation.25,26,28,32 The incidence reported by Doll et al. reached as high as 38%.28 The incidence of postoperative urinary incontinence in patients of the two groups in this study was 14.1%. All of the cases were temporary urinary incontinence, which generally disappeared within 1 month of surgery. Only 0.3% of patients (one case in the AUR group and two cases in the non-AUR group) continued to suffer mild to moderate urinary incontinence 12 months after surgery and required urinal pads when walking. The incidence of urethral stricture has been reported to be between 2.2% and 9.8%,26 whereas the incidence of urethral stricture in the two groups in this study was 9.9%. Surgical techniques, instrument types and sizes, inflammation, and the use of lubricants were associated with the incidence of postoperative urethral stricture.26 The incidence of urethral stricture in this study was slightly higher than that reported in the literature. This was probably caused by the F27 resectoscope, which is primarily designed for the Westerners. As Chinese men normally have smaller urethral diameters than the Western men, the surgery may very likely damage the orificium urethrae externum and membranous urethra, resulting in postoperative urethral stricture. Indeed, in this study, the urethral strictures were primarily found in the orificium urethrae externum, and membranous urethra followed by the bladder neck.
The incidence of UTI after TURP was relatively high, and the variations reported in the literature were large (as high as 25%). The reasons for this high incidence might be associated with different definitions of UTI.8,9,14,28,33 This study demonstrated that UTI primarily occurred within 3 months of surgery, which was similar to what has been reported in the literature.4,8,9 The incidence of UTI in the AUR group was significantly higher than that in the non-AUR group, possibly because the indwelling catheters in the AUR group before surgery increased the chances of the occurrence of postoperative UTI.
This study's results demonstrate that PK-TURP was an effective treatment for patients with BPH-associated AUR regardless of co-morbidities, as PK-TURP led to comparable improvement on IPSS, QoL, Qmax, and PVR in both the AUR and the non-AUR groups, even though, the AUR group had a significantly higher CCI score than the non-AUR group. Interestingly, we found that the QoL score of patients in the AUR group during the short-term after surgery was significantly lower than that in the non-AUR group, possibly because of different psychological expectations. The postoperative expectations of patients in the AUR group, who only hoped to experience smooth voiding, were lower than those of patients in the non-AUR group. In fact, medium- and long-term follow-up demonstrated that the QoL scores between the two groups did not display significant difference. For most BPH patients, the primary purpose of seeking treatment is to lessen the impact of LUTS on their QoL. For patients who suffer from AUR, the more urgent purpose is to be able to urinate and relieve the pain of difficult voiding. Based on the data, such as short-term (3 months) to medium- and long-term (1-year) follow-up visits, IPSS, QoL score, and Qmax, this study demonstrated that PK-TURP could be used to treat BPH patients with or without AUR, could significantly relieve LUTS, and could enable patients to void smoothly. This was corroborated by the multivariate regression analysis results that age, PVR, Qmax, diabetes, and hypertension but not the presence of AUR, were independent predictors of IPSS post-PK-TURP.
Both the hospitalization time and the postoperative urethral catheter placement time of the patients in this study were longer than those studied in other countries or regions for many reasons, which were primarily associated with the following factors.9,18,25 First, the medical coverage and medical expense payment systems were different. In our country, the medical expenses of most patients were paid by the medical coverage system only when the patients were hospitalized. Second, the medical charge systems were different. The hospitalization expenses in our country were low (approximately 5–10 USD per day). The third factor was the psychology and the requirements of the patients. The patients in this study thought that a short hospitalization time was not conducive to the recovery of their health. Fourth, the percentage of failure voiding was high when catheters were removed 2–3 days after surgery. Catheters must be reinserted after voiding failure, which was difficult for the patients to accept and which require the hospitalization to be extended.
In summary, regardless of whether BPH patients suffered from AUR, PK-TURP was an effective method to treat BPH-associated LUTS. The effect was immediate and could be maintained for more than 1 year. On the basis of sufficient preoperative preparation, immediate surgery using PK-TURP on BPH patients who were suffering from AUR was safe. However, immediate surgery would significantly prolong the hospitalization of patients and increase the incidence of UTI. This research was a retrospective clinical study, and the follow-up time was limited to 1 year. We are currently implementing a prospective controlled study with long-term follow-up (2–5 years) to further elucidate the efficacy and safety of immediate surgery using PK-TURP to treat BPH patients suffering from AUR and to determine the best treatment for AUR.
AUTHOR CONTRIBUTIONS
LH participated in study design, collected data, carried out data analysis and drafted the manuscript. YZ, JH, LL, and YW participated in study design, carried out data analysis, and performed data check and proofreading. JT, JT, KZ, and YT participated in data collection, carried out data analysis, and performed data check and proofreading. ZL participated in study design and data analysis, drafted the manuscript, and performed data check and proofreading. All authors have read and approved the final manuscript.
COMPETING INTERESTS
The authors declare that they have no competing interests.
REFERENCES
- 1.Emberton M, Anson K. Acute urinary retention in men: an age old problem. BMJ. 1999;318:921–5. doi: 10.1136/bmj.318.7188.921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jacobsen SJ, Jacobson DJ, Girman CJ, Roberts RO, Rhodes T, et al. Natural history of prostatism: risk factors for acute urinary retention. J Urol. 1997;158:481–7. doi: 10.1016/s0022-5347(01)64508-7. [DOI] [PubMed] [Google Scholar]
- 3.Fitzpatric JM. The natural history of benign prostatic hyperplasia. BJU Int. 2006;97:3–6. doi: 10.1111/j.1464-410X.2006.06097.x. [DOI] [PubMed] [Google Scholar]
- 4.Fitzpatrick JM, Desgrandchamps F, Adjali K, Gomez Guerra L, Hong SJ, et al. Management of acute urinary retention: a worldwide survey of 6074 men with benign prostatic hyperplasia. BJU Int. 2012;109:88–95. doi: 10.1111/j.1464-410X.2011.10430.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McNeill SA, Hargreave TB. Members of the Alfaur Study Group. Alfuzosin once daily facilitates return to voiding in patients in acute urinary retention. J Urol. 2004;171:2316–20. doi: 10.1097/01.ju.0000127743.80759.7a. [DOI] [PubMed] [Google Scholar]
- 6.Tiong HY, Tibung MJ, Macalalag M, Li MK, Consigliere D. Alfuzosin 10 mg once daily increases the chances of successful trial without catheter after acute urinary retention secondary to benign prostate hyperplasia. Urol Int. 2009;83:44–8. doi: 10.1159/000224867. [DOI] [PubMed] [Google Scholar]
- 7.Zeif HJ, Subramonian K. Alpha blockers prior to removal of a catheter for acute urinary retention in adult men. Cochrane Database Syst Rev. 2009;4:CD006744. doi: 10.1002/14651858.CD006744.pub2. [DOI] [PubMed] [Google Scholar]
- 8.Pickard R, Emberton M, Neal DE. The management of men with acute urinary retention. National Prostatectomy Audit Steering Group. Br J Urol. 1998;81:712–20. doi: 10.1046/j.1464-410x.1998.00632.x. [DOI] [PubMed] [Google Scholar]
- 9.Chen JS, Chang CH, Yang WH, Kao YH. Acute urinary retention increases the risk of complications after transurethral resection of the prostate: a population-based study. BJU Int. 2012;110:E896–901. doi: 10.1111/j.1464-410X.2012.11471.x. [DOI] [PubMed] [Google Scholar]
- 10.Desgrandchamps F, De La Taille A, Doublet JD RetenFrance Study Group. The management of acute urinary retention in France: a cross-sectional survey in 2618 men with benign prostatic hyperplasia. BJU Int. 2006;97:727–33. doi: 10.1111/j.1464-410X.2006.06109.x. [DOI] [PubMed] [Google Scholar]
- 11.Lo KL, Chan MC, Wong A, Hou SM, Ng CF. Long-term outcome of patients with a successful trial without catheter, after treatment with an alpha-adrenergic receptor blocker for acute urinary retention caused by benign prostatic hyperplasia. Int Urol Nephrol. 2010;42:7–12. doi: 10.1007/s11255-009-9572-7. [DOI] [PubMed] [Google Scholar]
- 12.Cathcart P, van der Meulen J, Armitage J, Emberton M. Incidence of primary and recurrent acute urinary retention between 1998 and 2003 in England. J Urol. 2006;176:200–4. doi: 10.1016/S0022-5347(06)00509-X. [DOI] [PubMed] [Google Scholar]
- 13.Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Transurethral prostatectomy: immediate and postoperative complications. Cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol. 2002;167:5–9. doi: 10.1016/s0022-5347(05)65370-0. [DOI] [PubMed] [Google Scholar]
- 14.Reich O, Gratzke C, Bachmann A, Seitz M, Schlenker B, et al. Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 patients. J Urol. 2008;180:246–9. doi: 10.1016/j.juro.2008.03.058. [DOI] [PubMed] [Google Scholar]
- 15.Starkman JS, Santucci RA. Comparison of bipolar transurethral resection of the prostate with standard transurethral prostatectomy: shorter stay, earlier catheter removal and fewer complications. BJU Int. 2005;95:69–71. doi: 10.1111/j.1464-410X.2005.05253.x. [DOI] [PubMed] [Google Scholar]
- 16.Mamoulakis C, Ubbink DT, de la Rosette JJ. Bipolar versus monopolar transurethral resection of the prostate: a systematic review and meta-analysis of randomized controlled trials. Eur Urol. 2009;56:798–809. doi: 10.1016/j.eururo.2009.06.037. [DOI] [PubMed] [Google Scholar]
- 17.Zhu G, Xie C, Wang X, Tang X. Bipolar plasmakinetic transurethral resection of prostate in 132 consecutive patients with large gland: three-year follow-up results. Urology. 2012;79:397–402. doi: 10.1016/j.urology.2011.08.052. [DOI] [PubMed] [Google Scholar]
- 18.Cullen IM, Dowling CM, Thornhill JA, Grainger R. Emergency management of acute urinary retention: results from an all-Ireland urologist practice survey. Ir J Med Sci. 2013;182:207–11. doi: 10.1007/s11845-012-0859-9. [DOI] [PubMed] [Google Scholar]
- 19.Teoh JY, Kan CF, Tsui B, Chiu PK, Man CY, et al. Ambulatory care program for patients presenting with acute urinary retention secondary to benign prostatic hyperplasia. Int Urol Nephrol. 2012;44:1593–9. doi: 10.1007/s11255-012-0266-1. [DOI] [PubMed] [Google Scholar]
- 20.Kalejaiye O, Speakman MJ. Management of acute and chronic retention in men. Eur Urol Suppl Incorporating the EAU-EBU Update Series. 2009;8:523–9. [Google Scholar]
- 21.Manikandan R, Srirangam SJ, O’Reilly PH, Collins GN. Management of acute urinary retention secondary to benign prostatic hyperplasia in the UK: a national survey. BJU Int. 2004;93:84–8. doi: 10.1111/j.1464-410x.2004.04562.x. [DOI] [PubMed] [Google Scholar]
- 22.Taube M, Gajraj H. Trial without catheter following acute retention of urine. Br J Urol. 1989;63:180–2. doi: 10.1111/j.1464-410x.1989.tb05160.x. [DOI] [PubMed] [Google Scholar]
- 23.Kumar S, Tiwari DP, Ganesamoni R, Singh SK. Prospective randomized placebo-controlled study to assess the safety and efficacy of silodosin in the management of acute urinary retention. Urology. 2013;82:171–5. doi: 10.1016/j.urology.2013.02.020. [DOI] [PubMed] [Google Scholar]
- 24.Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Transurethral prostatectomy: immediate and postoperative complications. A cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol. 1989;141:243–7. doi: 10.1016/s0022-5347(17)40731-2. [DOI] [PubMed] [Google Scholar]
- 25.Mayer EK, Kroeze SG, Chopra S, Bottle A, Patel A. Examining the gold standard: a comparative critical analysis of three consecutive decades of monopolar transurethral resection of the prostate (TURP) outcomes. BJU Int. 2012;110:1595–601. doi: 10.1111/j.1464-410X.2012.11119.x. [DOI] [PubMed] [Google Scholar]
- 26.Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of transurethral resection of the prostate (TURP) – incidence, management, and prevention. Eur Urol. 2006;50:969–79. doi: 10.1016/j.eururo.2005.12.042. [DOI] [PubMed] [Google Scholar]
- 27.Borboroglu PG, Kane CJ, Ward JF, Roberts JL, Sands JP. Immediate and postoperative complications of transurethral prostatectomy in the 1990s. J Urol. 1999;162:1307–10. [PubMed] [Google Scholar]
- 28.Doll HA, Black NA, McPherson K, Flood AB, Williams GB, et al. Mortality, morbidity and complications following transurethral resection of the prostate for benign prostatic hypertrophy. J Urol. 1992;147:1566–73. doi: 10.1016/s0022-5347(17)37628-0. [DOI] [PubMed] [Google Scholar]
- 29.Gomes CM, Nunes RV, Araújo RM, Sacomani CR, Trigo-Rocha FE, et al. Urodynamic evaluation of patients with lower urinary tract symptoms and small prostate volume. Urol Int. 2008;81:129–34. doi: 10.1159/000144049. [DOI] [PubMed] [Google Scholar]
- 30.Fagerström T, Nyman CR, Hahn RG. Complications and clinical outcome 18 months after bipolar and monopolar transurethral resection of the prostate. J Endourol. 2011;25:1043–9. doi: 10.1089/end.2010.0714. [DOI] [PubMed] [Google Scholar]
- 31.Mamoulakis C, Trompetter M, de la Rosette J. Bipolar transurethral resection of the prostate: the ‘golden standard’ reclaims its leading position. Curr Opin Urol. 2009;19:26–32. doi: 10.1097/MOU.0b013e32831e44da. [DOI] [PubMed] [Google Scholar]
- 32.Varkarakis J, Bartsch G, Horninger W. Long-term morbidity and mortality of transurethral prostatectomy: a 10-year follow-up. Prostate. 2004;58:248–51. doi: 10.1002/pros.10339. [DOI] [PubMed] [Google Scholar]
- 33.Tasci AI, Ilbey YO, Tugcu V, Cicekler O, Cevik C, et al. Transurethral resection of the prostate with monopolar resectoscope: single-surgeon experience and long-term results of after 3589 procedures. Urology. 2011;78:1151–5. doi: 10.1016/j.urology.2011.04.072. [DOI] [PubMed] [Google Scholar]


