Dear Editor,
Tuberculosis (TB) is an important health problem for global population and genitourinary TB is one of the most common extra-pulmonary TB.1 The clinical manifestations of renal TB tend to be low symptoms recently, which may lead to misdiagnosis and risk of renal function loss.2 How to improve the diagnosis rate of renal TB with low symptoms is an urgent issue to tackle. Therefore, in this study, 157 renal TB patients were collected to study for improving the diagnosis and treatment of renal TB especially for renal TB with low symptoms.
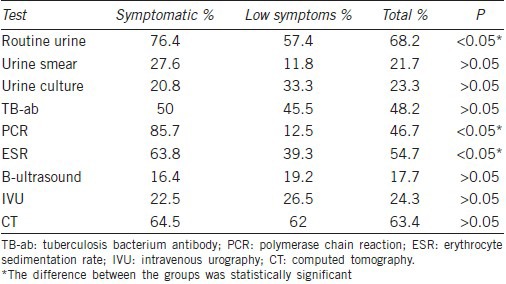
This study was approved by the Ethics Committee of Anhui Medical University. Renal TB patients (81 men and 76 women; mean age 44.13 ± 13.35 years) treated at the First Affiliated Hospital of Anhui Medical University and the Provincial Hospital in Anhui Province of China, between January 2008 and December 2013 were recruited. Diagnostic criteria for renal TB included effective empirical anti-TB drug treatment or pathological diagnosis.3 Cases were divided into two groups: 89 patients in the symptomatic group (defined as having two or more symptoms) and 68 patients in the low symptoms group (defined as having none of or only one symptom). All cases were retrospectively analyzed, including the clinical symptoms, demographic characteristics, laboratory tests, imaging studies, and treatment. The distribution of clinical symptoms is shown in Table 1. The results of laboratory and imaging examinations are summarized in Table 2. Fifty-one patients who were clinically diagnosed with renal TB underwent drug therapy with isoniazid + rifampicin + pyrazinamide/ethambutol triple therapy for 9–12 months. 49 of 68 (72.1%) patients in low symptoms group and 57 of 89 (64.0%) in the symptomatic group underwent surgery. The postoperative pathologic diagnoses were consistent with symptomatic TB. All patients that followed-up for approximately 0.5–2 years were cured.
Table 1.
Distribution of clinical symptoms
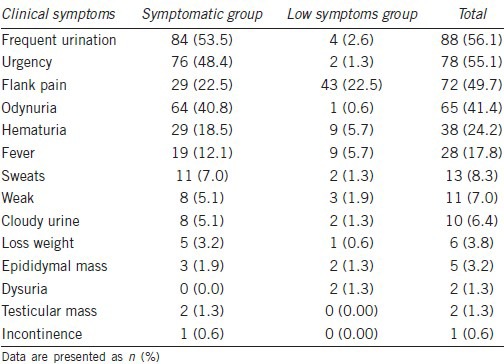
Table 2.
The positive rates of tests
Previous studies have reported a high incidence of renal TB among subjects aged 20–40 years.4 However in this study, it was found between 40 and 60 years. The reason for this may be associated with the low clinical symptoms and delayed diagnosis.
Low symptoms of renal TB mainly include flank pain. The diagnosis of renal TB with low symptoms is difficult, the following factors need to be considered: (1) renal calcification; (2) pit-shaped ureteral openings; (3) hydronephrosis of unknown causes; (4) decreased bladder capacity; (5) history of genital TB; and (6) evidence of hydronephrosis on B-ultrasonography, nonvisualized kidney on intravenous urography (IVU), or impaired renal function on radionuclide renogram. Low clinical symptoms of renal TB may be associated with several factors. First, the widespread use of broad-spectrum antibiotics particularly fluoroquinolone antibiotics5 and the irregular treatment of TB results in changes in bacterial virulence. Second, symptoms may become obscured by a nonspecific infection, stone, or tumor. Physicians may not be able to identify or suspect renal TB in patients who do not show symptoms such as urinary frequency, urgency, and odynuria and instead present with back pain, and hydronephrosis. Inexperienced young doctors often settle on a diagnosis of kidney stone or tumor, while neglecting that of renal TB.
Laboratory examinations are important means of diagnosis of renal TB. The symptomatic group showed a higher positive testing rate for abnormal routine urine examination results than the low symptoms group (P = 0.011). It is simple and cheap, and can be used as a preliminary screening of renal TB. The patients should stop anti-TB and antibacterial drugs 1-week before the urine smear for acid-fast bacilli, which should be performed 3 times in a row to improve the positive testing rate. The positive rate of urine TB-DNA-polymerase chain reaction (PCR) test was higher in the symptomatic group compared with the low symptoms group (P = 0.003). The TB-antibody test had a positive testing rate of 48.2%. Although the difference between the two groups was not significant (P > 0.05), this test is important for the early diagnosis of TB. Kamyshan6 suggested that molecular biological and immune assays may be used only for rapid diagnosis and screening, and cannot be a criterion for establishing renal TB. The positive rate of erythrocyte sedimentation rate was higher in the symptomatic group than in the low symptoms group. The ultrasonographic images provide important and reliable information for the clinical diagnosis, differential diagnosis, and treatment of renal TB.7 It is applicable for outpatient screening and follow-up, but it is rarely used to diagnose early renal TB. B-ultrasound should be used in combination with other examinations. IVU is suitable for the early diagnosis of renal TB.8 The most common findings on IVU are hydrocalycosis, hydronephrosis, or hydroureter due to stricture, whereas renal parenchymal masses and scarring, thick urinary tract walls, and extra-urinary tubercular manifestations are more common on computed tomography (CT) than on intravenous pyelogram.9 In our study, there is no significant difference between the groups (P > 0.05). CT can show some imaging changes consistent with renal TB.9 CT examination confirmed or revealed findings consistent with renal TB in 71 cases (63.4%), and had a high diagnostic value in both groups. If a radionuclide renogram shows renal failure or severely damaged renal function, doctors should perform other laboratory and imaging examinations. CT diagnosis is superior to B-ultrasound and IVU for the diagnosis of renal TB. Liu et al.10 found that the combined use of scrotal magnetic resonance imaging and PCR-based assay for mycobacterial DNA is a valuable method for rapid diagnosis of TB epididymitis.
The operation rates were 72.1% in low symptoms group and 64.0% in the symptomatic group. It shows that the concealed characteristics of renal TB with low symptoms have not attracted enough attention of patients and doctors. Therefore, the disease progresses will gradually conduce to kidney dysfunction.
The present research on the renal TB with low symptoms provides us reference for future clinical situations. A multi-center evaluation of the findings should be undertaken in the future.
AUTHOR CONTRIBUTIONS
JW, SF and CZL contributed to the concept and design of the project. JX and JW contributed to the acquisition and analysis of data. JW and SF drafted the manuscript. All authors read and approved the final manuscript.
COMPETING FINANCIAL INTERESTS
The authors declare no competing financial interests.
ACKNOWLEDGMENTS
This study was supported by grant from Construction Project of National Key Clinical Specialty.
REFERENCES
- 1.Fader T, Parks J, Khan NU, Manning R, Stokes S, et al. Extrapulmonary tuberculosis in Kabul, Afghanistan: a hospital-based retrospective review. Int J Infect Dis. 2010;14:e102–10. doi: 10.1016/j.ijid.2009.03.023. [DOI] [PubMed] [Google Scholar]
- 2.Zhukova II, Kul’chavenia EV, Kholtobin DP, Brizhatiuk EV, Khomiakov VT, et al. Urogenital tuberculosis today. Urologiia. 2013;1:13–6. [PubMed] [Google Scholar]
- 3.Fain O, Lortholary O, Lascaux VV, Amoura II, Babinet P, et al. Extrapulmonary tuberculosis in the northeastern suburbs of Paris: 141 cases. Eur J Intern Med. 2000;11:145–50. doi: 10.1016/s0953-6205(00)00076-5. [DOI] [PubMed] [Google Scholar]
- 4.Heaton ND, Hogan B, Michell M, Thompson P, Yates-Bell AJ. Tuberculous epididymo-orchitis: clinical and ultrasound observations. Br J Urol. 1989;64:305–9. doi: 10.1111/j.1464-410x.1989.tb06019.x. [DOI] [PubMed] [Google Scholar]
- 5.Webster D, Long R, Shandro C, Pettipas J, Leblanc J, et al. Fluoroquinolone resistance in renal isolates of Mycobacterium tuberculosis. Int J Tuberc Lung Dis. 2010;14:217–22. [PubMed] [Google Scholar]
- 6.Kamyshan IS. Current methods in diagnosis of the kidney tuberculosis. Urologiia. 2006;4:57–61. [PubMed] [Google Scholar]
- 7.Rui X, Li XD, Cai S, Chen G, Cai B. Ultrasonographic diagnosis and typing of renal tuberculosis. Int J Urol. 2008;15:135–9. doi: 10.1111/j.1442-2042.2007.01962.x. [DOI] [PubMed] [Google Scholar]
- 8.Valentini AL, Summaria V, Marano P. Diagnostic imaging of genitourinary tuberculosis. Rays. 1998;23:126–43. [PubMed] [Google Scholar]
- 9.Wang LJ, Wu CF, Wong YC, Chuang CK, Chu SH, et al. Imaging findings of urinary tuberculosis on excretory urography and computerized tomography. J Urol. 2003;169:524–8. doi: 10.1097/01.ju.0000040243.55265.71. [DOI] [PubMed] [Google Scholar]
- 10.Liu HY, Fu YT, Wu CJ, Sun GH. Tuberculous epididymitis: a case report and literature review. Asian J Androl. 2005;7:329–32. doi: 10.1111/j.1745-7262.2005.00038.x. [DOI] [PubMed] [Google Scholar]


