Key Clinical Message
A 77‐year‐old man was referred to our hospital due to enlarging mediastinal/hilar lymphadenopathy with calcification. Endobronchial ultrasound‐guided transbronchial needle aspiration (EBUS‐TBNA) and bone marrow aspiration were performed. Subsequently, monoclonal gammopathy of undetermined significance (MGUS) associated with mediastinal amyloidosis was diagnosed. We hereby report a case in which EBUS‐TBNA led to a successful diagnosis of amyloidosis.
Keywords: endobronchial ultrasound‐guided transbronchial needle aspiration, mediastinal/hilar amyloidosis
Synopsis
A 77‐year‐old man complained of slight shortness of breath, and was referred to our hospital due to enlarging mediastinal/hilar lymphadenopathy with calcification and right pleural effusion on computed tomography (CT) (Fig. 1A,B).
Figure 1.
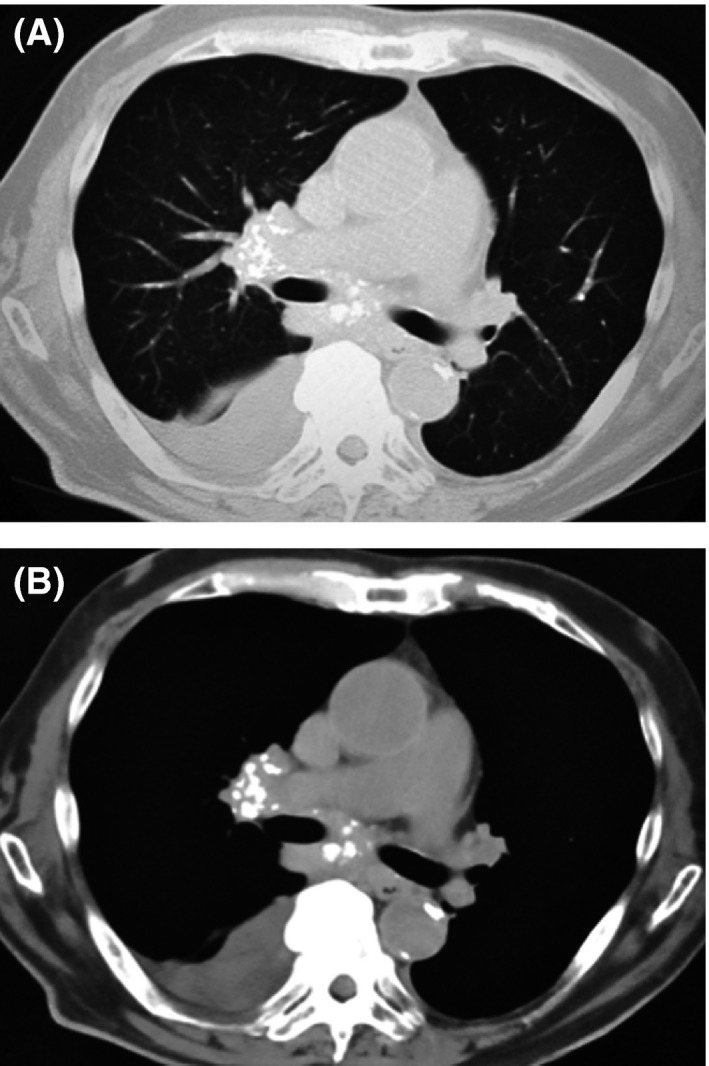
Chest CT on parenchymal (A) and mediastinal (B) window settings showed right pleural effusion and mediastinal/hilar lymphadenopathy with calcification.
Question
What is the appropriate procedure to approach this lesion, and what is the differential diagnosis?
Diagnosis
Monoclonal gammopathy of undetermined significance (MGUS) associated with mediastinal/hilar amyloidosis
Explanation
Initially, malignant neoplasm was suspected. Endobronchial diagnosis at Nagoya Medical Center was requested and endobronchial ultrasound‐guided transbronchial needle aspiration (EBUS‐TBNA) of lymph node station 7 was performed.
Pathological examination revealed amorphous eosinophilic tissue with few cellular components (Figs. 2 and 3A,B). Results of direct fast scarlet (DFS) staining were positive (Fig. 3B). There were serumal findings of high IgG and suppression of IgA and IgM. Additionally, there was IgG‐λ‐type M protein on immunoelectrophoresis. We subsequently performed bone marrow aspiration, and the plasma cell rate was 4.5%. (If the plasma cell rate is more than 10%, myeloma can be diagnosed.) As a result, monoclonal gammopathy of undetermined significance (MGUS) associated with mediastinal amyloidosis was diagnosed. And then, thoracentesis was performed. Cytology of the pleural fluid was negative. Echocardiography showed an ejection fraction of 45%, and there was brightness in part of the interventricular septum. In addition, he had myocardial dysfunction due to amyloidosis.
Figure 2.
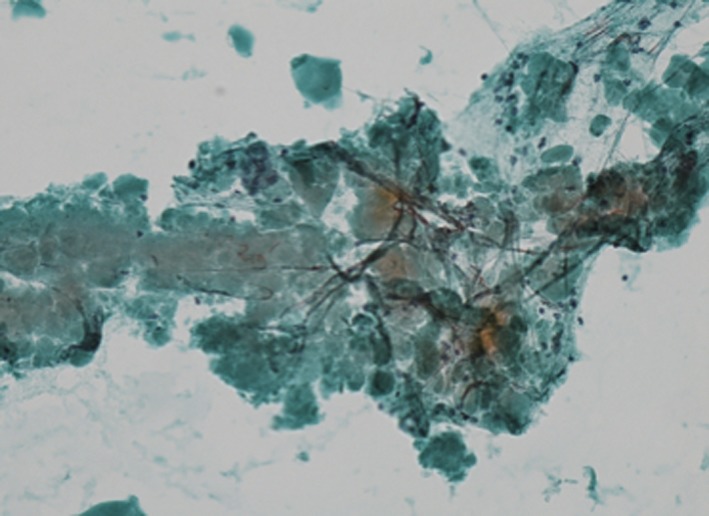
Cytology of the lymph node. A lump of amorphous light green material (Papaniclaou staining, ×200).
Figure 3.
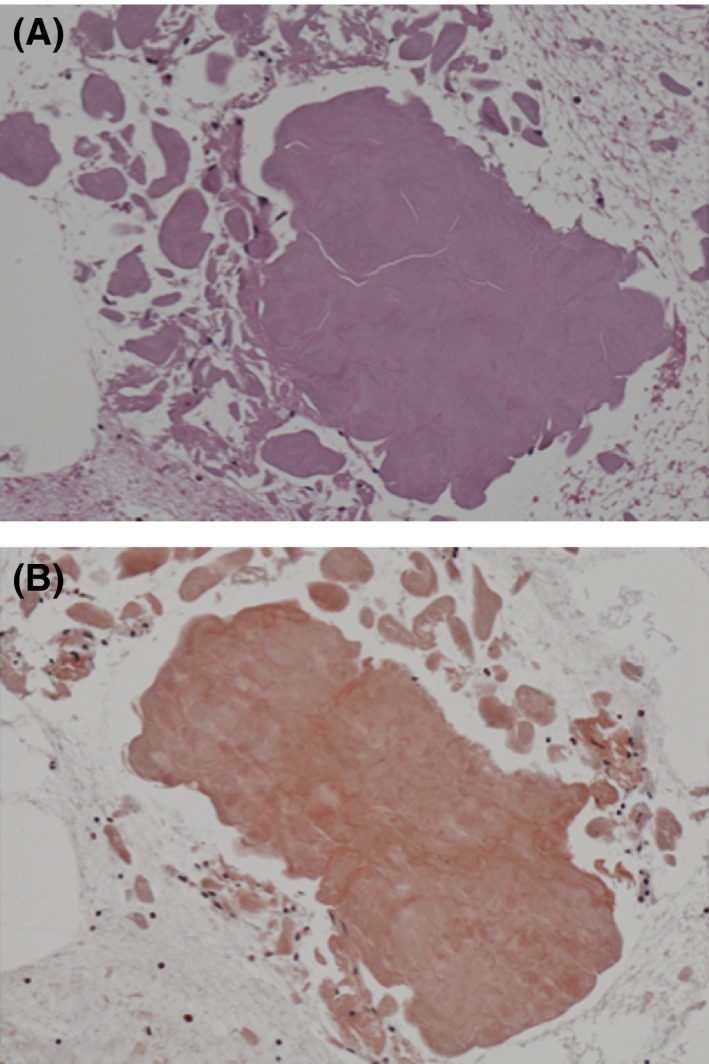
Histology of the lymph node. (A) Section showing amorphous eosinophilic materials with hematoxylin–eosin staining (H&E, ×200). (B) These materials stained positive for direct first scarlet staining (DFS, ×200), indicating amyloid deposits.
We are currently administering combination therapy of bortezomib, melphalan, and prednisolone to this patient. As a result, the serum IgG has decreased and there is no systemic aggravation; however, his cardiac function has not improved with this treatment.
As Jenkins et al. stated, amyloidosis should be considered in the differential diagnosis of a large mediastinal mass, especially if calcification and/or plasma cell neoplasm is present 1. EBUS‐TBNA for enlarging mediastinal lymphadenopathy with calcification led to a successful diagnosis of amyloidosis.
Conflict of interest
The authors declare that they have no competing interests.
Clinical Case Reports 2016; 4(2): 212–213
Reference
- 1. Jenkins, N. C. F. , and Potter M.. 1991. Calcified pseudotumoral mediastinal amyloidosis. Thorax 46:686–687. [DOI] [PMC free article] [PubMed] [Google Scholar]


