Abstract
Background
Struck by injuries experienced by females were observed to be higher compared to males in an urban fire department. The disparity was investigated while gaining a grounded understanding of EMS responder experiences from patient‐initiated violence.
Methods
A convergent parallel mixed methods design was employed. Using a linked injury dataset, patient‐initiated violence estimates were calculated comparing genders. Semi‐structured interviews and a focus group were conducted with injured EMS responders.
Results
Paramedics had significantly higher odds for patient‐initiated violence injuries than firefighters (OR 14.4, 95%CI: 9.2–22.2, P < 0.001). Females reported increased odds of patient‐initiated violence injuries compared to males (OR = 6.25, 95%CI 3.8–10.2), but this relationship was entirely mediated through occupation (AOR = 1.64, 95%CI 0.94–2.85). Qualitative data illuminated the impact of patient‐initiated violence and highlighted important organizational opportunities for intervention.
Conclusions
Mixed methods greatly enhanced the assessment of EMS responder patient‐initiated violence prevention. Am. J. Ind. Med. 59:150–163, 2016. © 2016 The Authors. American Journal of Industrial Medicine Published by Wiley Periodicals, Inc.
Keywords: prehospital violence, assaults, paramedics, firefighter, emergency medical services
INTRODUCTION
Each year an estimated 1.7 million American workers report an injury as a result of workplace violence [Gates et al., 2011]. In 2009, data from the Consumer Product Safety Commissions’ National Electronic Injury Surveillance System (NEISS) estimated more than 137,000 workers were treated in emergency departments for nonfatal violence [Center for Disease Control and Prevention, Occupational Violence, 2014]. Health care workers have the highest rate of workplace violence compared to all other industries, with the majority of violent injuries committed by their patients [Bureau of Labor Statistics, 2007]. Reports show that health care workers have an injury rate of 20.4 per 10,000, which is significantly larger than the general sector rate of 2.1 per 10,000 [Gates et al., 2011].
There are an estimated 900,000 full‐time, part‐time, and volunteer Emergency Medical Services (EMS) workers in the United States who treat 22 million patients a year [Maguire and Smith, 2013]. EMS workers have a variety of responsibilities that include responding to emergency calls, providing clinical care in the field, and transporting patients to hospitals and health care facilities [Center for Disease Control and Prevention, Emergency Medical Services Workers, 2014]. In 2012, an estimated 2,400 EMS workers visited U.S. hospital emergency departments to treat an injury resulting from work‐related violence [Center for Disease Control and Prevention, EMS Workers Injury and Illness Data, 2014]. Maguire estimated that patient‐initiated violence to paramedics and EMTs occur in 1–2% of all nonfatal injuries in Australia and the United States, respectively [Maguire and Smith, 2013; Maguire et al., 2014]. A survey of paramedics from two Canadian provinces found 75% of respondents experienced violence in the last year, with verbal assaults more common than physical [Bigham et al., 2014].
In a previous research study, we confirmed this violence problem among EMS responders by examining data from the National Fire Fighter Near Miss Reporting System, an international voluntary reporting system created by the International Association of Fire Chiefs (www.nationalnearmiss.org). We reviewed emergency medical call reports and analyzed their narrative text fields. Of 185 reports, violence was the most commonly identified mechanism of near‐miss or injury (n = 48). We found that emergency medical responders were threatened or assaulted by patients as well as family members and bystanders. Common underlying factors included: violent patients, patients with a mental health issue, and patients with particular health conditions (e.g., seizure, hypoglycemia) [Taylor et al., 2015].
METHODS
We analyzed data from the Firefighter Injury Research and Safety Trends (FIRST) project to investigate the patient‐initiated violence issue more deeply in an urban, inner city department. FIRST was funded by the Federal Emergency Management Agency (FEMA) to research and develop a U.S. non‐fatal firefighter injury surveillance system. The career fire department we selected protects a population of over 1 million people. According to the National Fire Protection Association, there are approximately 45,000 fire departments in the United States that serve populations of this size [National Fire Protection Association, 2014].
We employed a convergent parallel mixed methods design [Creswell and Plano Clark, 2011]. Data are collected in a fairly simultaneous fashion, analyzed separately, and then results are combined into an overall interpretation. The point of such design is to use the strengths of one method to compensate for the weaknesses of the other and vice versa. Both results are combined to increase understanding of the phenomenon under study. This protocol received approval from the Drexel University Institutional Review Board and the Department of Homeland Security's Regulatory Compliance Office.
Quantitative
The study population included uniformed fire department paramedics and firefighters who were on the roster as active employees from 2005 through 2013. In order to maximize the detection of all injuries for the study period, we linked data from workers' compensation, the fire department's safety office first report of injury, and the city's accident injury and illness report. Injuries were linked by payroll identification number and then de‐duplicated across all databases. Proportions of injuries were examined by cause and gender. For patient‐initiated violence‐related injuries, chi‐square tests for independence and odds ratios were calculated for gender, patient‐initiated violence, and occupation.
Assessment of the causal mechanism of gender and occupation on patient‐initiated violence to paramedics was done in two ways. First, heterogeneity of effects was used to assess the modifying effect of occupation on the associations observed between gender and patient‐initiated violence. The effect of gender on patient‐initiated violence was calculated across strata of occupation and effect estimates compared.
Second, the Sobel method was used to assess the mediating effect of occupation on the association between gender and occupation [Sobel, 1982]. In short, we wanted to explore the direct effect of gender on patient‐initiated violence as well as the indirect effect of gender on patient‐initiated violence that is mediated through the effect of occupation.
Qualitative
To gain deeper insight regarding the experiences of paramedics and EMTs who experienced a patient‐initiated violent injury, we conducted grounded theory qualitative research that utilized interviews and one focus group.
Participants were selected for this study via purposeful sampling, in order to select participants who shared the same characteristic of a patient‐initiated violent experience. The fire department human resources division provided contact information for paramedics and EMTs currently employed by the fire department who reported a patient‐initiated violent injury in the past five years. Paramedics and EMTs were invited by phone and followed‐up by email to participate in the study. We also used a “snowball sampling” approach, in which participants were asked to help us identify other potential colleagues who had been injured for study participation.
A total of ten paramedics and EMTs from the fire department participated in the qualitative phase of the study. Five 1‐hr individual interviews and a 2‐hr focus group with five participants were conducted. The focus group was intentionally composed of female paramedics to explore experiences and opinions about the observed increased risk to women from patient‐initiated violence. After collecting and reviewing the qualitative data collected, we achieved thematic saturation after speaking with ten participants across five interviews and one focus group.
The interviews and focus group took place at a location of the subject's choosing (e.g., at the participants home, fire station, researcher office, etc.). Only participants and researchers were present for all interviews and the focus group. Prior to meeting for this research, the researchers knew none of the participants. Each participant signed an informed consent and were made aware of the minimal risks involved in participating in this research. The interviews and focus group were conducted by JAT and BB, both of whom are female public health researchers with training in qualitative data collection. The interviews and focus group were audio recorded in a private room to ensure confidentiality and privacy. Instruments used to collect data included a demographic form and a semi‐structured interview guide seen in (Table I). Field notes with preliminary reflections and reactions from the focus group were recorded by BB.
Table I.
Semi‐Structured Interview Guide
| WARM UP QUESTIONS: |
| Tell me what it is like to work as an EMT in [city name]. |
| INCIDENT SPECIFIC QUESTIONS: |
| Tell me about the assault you experienced while on a medical run? |
| Tell me about the factors that led up to your injury? |
| Patient contributions to the event? |
| Your contributions to the event? |
| Fire Department contributions/resources you need from the department? |
| PSYCHOLOGICAL QUESTIONS: |
| Tell me about the emotions you experienced during the incident. |
| How comfortable did you feel reporting your experience after being assaulted? |
| Can you tell me about the process/system in place to report incidents such as the one you experienced? Was there a follow up to ensure medical treatment or counseling had been provided after the incident? |
| After experiencing this episode of violence, please describe how it has impacted you: personally (relationships with others)? Professionally (at work)? |
| GENERAL ASSAULT QUESTIONS: |
| How do you feel about the idea of being assaulted as “a part of the job”? |
| Have you ever witnessed another colleague being assaulted on a medical run or heard them discuss being assaulted while working? |
| POLICY QUESTIONS: |
| Are you aware of a written workplace violence policies or procedures? |
| If yes, as best as you can, please explain what the policy entails? |
| If no, what type of policy would you recommend to have a safer work environment? |
| What are your thoughts about the Employee Assistance Programs (EAP)? |
| Offered by the City? |
| Offered by the Union? |
| LEADERSHIP QUESTIONS: |
| How do you feel about the quality of the job leadership is doing to address this issue? |
| Can you tell me about the kind of training you received regarding assaults and/or how to protect yourself during a high risk encounter? |
| How comfortable do you feel making suggestions to management about corrective actions that should be taken once an assault has occurred? |
| PREVENTION QUESTIONS: |
| What are your ideas about how assaults can be prevented? |
| What are your thoughts about the following prevention suggestions? |
| Would having known violent calls flagged in the system be helpful? |
| Would physical barrier (i.e. barricade tape?) assist in keeping EMTs safe? |
| Would simulation training or other training classes increase skills to keep EMTs safer? |
| How do you feel about male–female partners on medical runs as a prevention strategy? |
| CLOSING QUESTION: |
| Those are all of the questions we have for you today, is there anything else you would like to add before we end? |
The audio files from the interviews and focus groups were transcribed for data analysis by a professional transcription service. Transcripts were shared with all research participants. One participant provided feedback to researchers after reviewing their transcript. The transcripts were de‐identified and verified by a research team member for accuracy. All quotations presented within this manuscript have been assigned pseudonyms to further ensure speaker anonymity. A coding structure was developed by the research team (Table II) to allow researchers (BB & JW) to code the data using NVivo qualitative data analysis software (QSR International Pty Ltd. Version 10, 2012). As the transcripts were coded and analyzed, the researchers looked for patterns in attitudes and beliefs across emergent themes, as well as contrasting viewpoints.
Table II.
Qualitative Coding Structure
| Qualitative coding categories |
|---|
| Perceptions of paramedic and EMT work |
| Job risk |
| Community expectations and misuse of services |
| Family members/bystanders |
| Relationship with police |
| Assault experienced |
| Risk factors |
| Substance abuse |
| Mental health |
| Medical condition |
| History of violent behavior |
| Abuse |
| Injury sustained |
| Time or money loss |
| Legal process and outcomes |
| Psychological effects |
| Coping strategies |
| Organization |
| Policies, procedures and practices |
| Leadership |
| Fear of being transferred/punished |
| Fatalism of the system |
| Individual perceptions |
| Communication |
| Interdepartmental |
| Reporting incidents |
| Dispatch |
| Gender |
| Race |
| Employee Assistance Program (EAP) |
| Prevention interventions |
RESULTS
Quantitative
The Workers' Compensation Insurance Organization (WCIO) Cause of Injury rubric (https://www.wcio.org/Document%20Library/InjuryDescriptionTablePage.aspx) defines struck by injuries as “cases in which the injury was produced by the impact created by the source of injury, rather than by the injured person,” (e.g., struck by patient, struck by motor vehicle). This is in contrast to striking against or stepping on injuries that are “cases in which the injury was produced by the impact created by the person, rather than by the source” (e.g., striking against a moving part of machine, stepping on sharp object). Data from 2005 to 2013 injury reports showed that most causes of injury were of relatively equivalent proportions between males and females. However, 21% percent of female injuries had “struck or injured by” as their cause of injury compared to 13% of male injuries, a significant difference (Z‐Score 3.8466, P‐value <0.00012) (Table III).
Table III.
Main Causes of Firefighter Injury, 2005–2013
| Cause category | Total | Female | Male |
|---|---|---|---|
| Strain or injury by | 638 (26.91%) | 86 (30.82%) | 552 (26.39%) |
| Fall, slip, or trip injury | 409 (17.25%) | 50 (17.92%) | 359 (17.16%) |
| Burn or scald‐heat or cold exposure | 384 (16.20%) | 9 (3.23%) | 375 (17.93%) |
| Struck or injured by | 325 (13.71%) | 59 (21.15%) | 266 (12.72%) |
| Miscellaneous causes | 281 (11.85%) | 35 (12.54%) | 246 (11.76%) |
| Cut, puncture, scrape injured by | 104 (4.39%) | 5 (1.79%) | 99 (4.73%) |
| Motor vehicle | 101 (4.26%) | 16 (5.73%) | 85 (4.06%) |
| Caught in, under, or between | 71 (2.99%) | 12 (4.30%) | 59 (2.82%) |
| Striking against or stepping on | 58 (2.45%) | 7 (2.51%) | 51 (2.44%) |
| Total | 2,371 (100.00%) | 279 (100.00%) | 2,092 (100.00%) |
There were no additional quantitative data to explain the differences, so we reviewed female “Struck or injured by” narratives from the Safety Office's first report of injury. Excerpts from these narratives are shown in Table IV.
Table IV.
Sample Narratives When the Injured Employee Is Female and the Case of “Struck or Injured By” Was Reported
| Laceration/eye and head employees struck by patient on head resulting in laceration above eye |
| Contusion/lower arm, jaw/shin and both breast Employee was hit on the arm during the struggle with patient |
| Contusion/laceration, eye employee was punched in the face by a drunkard |
| Contusion/chest Employee was tackled by a large man in chest area |
| Contusion/pointer finger, shoulder, way assaulted by a combative patient |
| Contusion/knee employee was struck by a patient in the knee |
| Contusion eye while escorting patient to triage employee was punched in eye |
| Struck by patient multiple contusions |
| Contusion/mouth performing EMS duties patient head butted employee on the jaw |
| Sprain/forearm, wrist in transport patient became combative and pushed employee down |
Emphasis added (bold).
We postulated that the difference in proportion of “struck or injured by” events by gender were due to patient‐initiated violence. From our linked master dataset, we tabulated all patient‐initiated injuries including struck by, cut by, pushed by, etc. We calculated odds ratios and observed that women were six times as likely as men to report a patient‐initiated violent injury (OR = 6.25, 95%CI 3.8–10.2). We shared these findings with our stakeholders (e.g., fire department, the local chapter of the union, and the city's risk management department). Our stakeholders suggested that women were more likely to be paramedics than firefighters, so we conducted tests of association among the variables gender, occupation, and patient‐initiated violence. In order to do this, we had to acquire new data from the human resources department in the form of a roster to identify the ranks of the individuals and remove anyone who had retired or separated from service. As this took time and modifications to the IRB, we initiated the qualitative portion of the study described in the next section.
Once we had the quantitative data from human resources, we were able to calculate numerators and denominators for patient‐initiated violence by gender and occupation (Table V).
Table V.
Odds Ratios Comparing Gender, Occupation, and Patient‐Initiated Violence (Assault)
| Gender versus assault | Assault | No Assault | Total | ||
| Female | 24 | 167 | 191 | Odds Ratio | 6.25 |
| Male | 67 | 2,916 | 2,983 | Confidence Interval | (3.83, 10.23) |
| Total | 91 | 3,083 | 3,174 | P‐value (yates) | <0.001 |
| Occupation versus female | Female | Male | Total | ||
| Paramedic | 112 | 253 | 365 | Odds Ratio | 15.3 |
| Firefighter | 79 | 2,730 | 2,809 | Confidence Interval | (11.16, 20.97) |
| Total | 191 | 2,983 | 3,174 | P‐value (yates) | <0.001 |
| Occupation versus assault | Assault | No assault | Total | ||
| Paramedic | 56 | 309 | 365 | Odds Ratio | 14.36 |
| Firefighter | 35 | 2,774 | 2,809 | Confidence Interval | (9.27, 22.27) |
| Total | 91 | 3,083 | 3,174 | P‐value (yates) | <0.001 |
| Males only: occupation versus assault | Assault | No assault | Total | ||
| Paramedic | 34 | 219 | 253 | Odds Ratio | 12.69 |
| Firefighter | 33 | 2,697 | 2,730 | Confidence Interval | (7.70, 20.89) |
| Total | 67 | 2,916 | 2,983 | P‐value (yates) | <0.001 |
| Females only: occupation versus assault | Assault | No assault | Total | ||
| Paramedic | 22 | 91 | 113 | Odds Ratio | 9.31 |
| Firefighter | 2 | 77 | 79 | Confidence Interval | (2.12, 40.85) |
| Total | 24 | 168 | 192 | P‐value (yates) | 0.001 |
We found that women were more likely than men to experience a patient‐initiated violent injury (OR 6.25, 95%CI: 3.8–10.2). Confirming the perceptions of our firefighter advisory board, we observed that women were more likely to be paramedics then firefighters (OR 15.3, 95%CI: 11.2–21). We also found that paramedics were more likely than firefighters to experience a patient‐initiated violent injury (OR 14.4, 95%CI: 9.2–22.2). Because our chi‐squared estimates posited that gender could be a confounder, we stratified the test of association between patient‐initiated violent injury and occupation by gender. Male paramedics were at increased odds of patient‐initiated violent injury compared to male firefighters (OR 12.7, 95%CI: 7.7–21), and female paramedics were at increased odds of patient‐initiated violent injury compared to female firefighters (OR 9.3, 95%CI: 2.1–41). As the stratification did not equalize the effect estimates, we suspected effect modification by gender; however, the test for heterogeneity effects was not statistically significant (P = 0.708).
We then analyzed the potential mediating effect of occupation on the association between gender and patient‐initiated violent injury (Fig. 1). The crude association of gender and of 6.26 (95%CI 3.83–10.23) became non‐significant after controlling for the effect of occupation (OR 1.64; 95%CI 0.94–2.85). The Sobel test for mediation showed a significant result (z = 8.34, P < 0.001). It was concluded that occupation mediates the association between gender and patient‐initiated violent injury completely.
Figure 1.
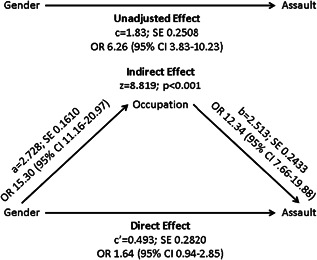
Assessing mediation effects of occupation.
Qualitative
A total of ten paramedics and EMTs who had been violently injured by patients in the line of duty from the fire department participated in the qualitative phase of the study (Table VI). One hour individual interviews (n = 5) and one 2‐hr focus group (n = 5) were conducted.
Table VI.
Participant Demographics
| Sex (n) | |
| Female | 7 |
| Male | 3 |
| Age (years) | |
| Range | 27–57 |
| Mean | 39 |
| Years as EMT/Paramedic | |
| Range | 3–18 |
| Mean | 13 |
| Years with department | |
| Range | 3–18 |
| Mean | 10 |
| Education level | |
| Some college | 3 |
| Technical school | 4 |
| 2 year college/Associate degree | 1 |
| 4 year college | 1 |
| Graduate school | 1 |
| Ethnicity (n) | |
| White/Caucasian | 5 |
| Black/African American | 4 |
| Hispanic/Latino | 1 |
From the NVivo coding of narratives, eight themes emerged relating to the paramedic's experience of their patient‐initiated violent injury. The most salient qualitative themes were: factors relating to underreporting, dispatch, community expectations, psychological impact, leadership/policy, the legal process, training, and the work environment. Some emergent themes (e.g., dispatch and the psychological impact) were unanticipated.
EMS responders work in confined spaces in very close proximity to patients. The nature of their work requires them to be face to face with their patients as they intubate, insert IVs, or stabilize wounds. The following quotes exemplify how quickly a patient‐initiated violent injury can unfold during these interactions and how unaware a medic may be of its possibility:
I have been kicked, punched, bitten, spit on, verbally abused. You name it, I've had it all. (Elizabeth, Paramedic)
And I put my hand on his back and, you know, was rubbing his back… and he just jumped up and punched me right in the face… (Nicole, Paramedic)
He's sitting on the stretcher, and I'm standing up. He puts his one arm on the stretcher to transfer, and just comes up and punches me in my mouth with everything he had. (John, Firefighter‐EMT)
Factors Relating to Underreporting
In response to our initial quantitative finding that females had a sixfold higher odds of reporting patient‐initiated violent injuries compared to males, we showed participants the data and asked them to share their thoughts. Participants indicated that the gender differences were attributed to reporting issues. The gender predilection was credited to male paramedics and EMTs not wanting to appear “weak” by reporting violent incidents, particularly by female patients.
I believe that men, they suck up more than we do. They have a rep to keep. Their thing is – what [would] I look like telling them somebody bit me, what [would] I look like saying the chick punched me in my head… (Kelly, Paramedic)
Participants also explained that the gender difference could be due to females feeling more motivated to report an incident to ensure the protection of their jobs (i.e., an employee who reports their job‐related injury to workers' compensation retains their tenure and benefits in the fire department):
I think because men view it as a weakness if you report an injury. Like I seen guys get really injured badly and they won't report it, but …I know as a female….I'm going to report it, because I know I have to prove that I got injured on the job. But most guys will shake it off. (Mary, Firefighter‐EMT)
We also heard from the participants that females can be viewed as “easy‐targets” and as “de‐escalators,” depending on the situation. Participants explained that male patients are more willing to intimidate a female and are less reluctant to be aggressive if being treated by a male paramedic or EMT. A female paramedic from the focus group agrees with this concept explaining: “We present ourselves as professionals. And we are also females. Females in general, people tend to believe are passive weaklings. Men are perceived to be stronger” (Nicole, Paramedic). In contrast, we also heard that females have the ability to diminish the likelihood of a violent encounter by verbally deescalating situations. “They're very – very good with the words. That's what I've noticed about [working] with a female partner is they try talking someone down a lot” (James, Firefighter‐EMT).
Several participants discussed normalization of risk, and how as tenure within the profession goes up, experiencing a patient‐initiated violent injury becomes an expected part of the job. Participants rationalized their risk as typical, especially when the patient is elderly, ill, or has a certain medical condition (e.g., hypoglycemia, seizures, mental health issue, etc.). Many participants appeared sympathetic to these types of combative patients and made individual judgments about whether the incident warranted reporting. For example, a female paramedic rationalized her decision not to report a violent incident with an older, combative female patient stating:
…she swung, but she caught my glasses. So [she] just brazed me. But like we said, we suck up so much. I didn't even call nobody. I didn't even tell – I didn't even report it because okay, she's old, she's upset. I understand she's upset (Kelly, Paramedic).
Additionally, the interpretation of what constitutes the definition of a patient‐initiated violent injury can influence a responder's decision to report. For example, a male paramedic explained that “wrestling with people” does not warrant reporting and “comes with the job” (James, Firefighter‐EMT). We learned that males are less likely to see certain interactions such as pushing or a tap on the chest as patient‐initiated violence.
Dispatch Information
The dispatch/911 center is the first point of contact for the community when reporting medical emergencies. The way in which the dispatch center handles a medical call can determine how the remaining healthcare experience will unfold, for both the paramedic and the patient. Participants stated that they often feel a disconnect with the dispatchers:
We're dispatched in way too many incidents that we have no idea what we're walking into. And when we ask dispatch what it is, they're very vague – 'oh, I don't know'…That's what we walk into everyday. (James, Firefighter‐EMT)
Participants felt that dispatchers are oftentimes not collecting enough background information on calls. This has been a concern with which many medics and EMTs expressed frustration. They believe the dispatchers do not listen to the needs of the medics, which places them in dangerous situations:
…because again, our dispatch system doesn't have our backs and doesn't listen to what we ask for. And I can say I know a lot of members on the street don't feel comfortable if – ever something serious would have happened with the way our dispatch system works because they don't listen to us. (James, Firefighter‐EMT)
Another sentiment that was expressed from the participants is the feeling that dispatchers do not realize that they are working with the EMS providers and not above them:
A lot of times we feel very disconnected from the dispatch center. They send us in situations that we don't feel safe with and when we ask more questions, we're therefore yelled at by them. They feel they're our supervisors, which is not the case at all. They have no repercussions for any actions that they take.” (James, Firefighter‐EMT)
The issue of feeling unsafe and unprotected oftentimes stemmed from the actions of the dispatchers. Participants revealed that they often felt disconnected when they asked for assistance or backup. Many paramedics and EMTs shared occurrences where there were lapses in time before the dispatchers would send a police assist, leaving medics vulnerable to a possible patient‐initiated violent injury. This was emphasized by participants who stated:
I don't even wait, because if you press the button, dispatch will say are you declaring an emergency? And then if you don't answer, [dispatch says] “Medic, Medic, are you declaring an emergency”? They say it like three times before they say okay, it must be an emergency. So when I press my button, I need help now. (Nicole, Paramedic)
But as far as I know, the department has no standard on if we need a backup…what we're supposed to do. I understand that…when we request an assist, a protocol for semi‐assist, which is a ladder, an engine, and a chief, but at the same time, if we don't get that when we request it, there's no backup protocols at all. I mean the example I used a few minutes ago with the person requesting an assist and he never got it, he was put in a very dangerous situation. (James, Firefighter‐EMT)
Community Expectations
Participants discussed what they think the community expects from their services, and how they are expected to act while meeting those expectations. This was a predominant theme that appeared in every interview and the focus group. One viewpoint expressed by participants was the idea that community members are calling 911 and EMS services for non‐emergent needs resulting in the paramedics feeling like little more than a ride to the hospital:
…people think that we're there to be their taxi service and they talk to us the way they want to and we're not allowed to raise an eyebrow to them. That is the way people see us.” (James, Firefighter‐EMT)
Along with feeling frustrated at being seen as merely a taxi service, this participant is also bringing up the idea of professionalism while out in the field. Multiple participants explained that they felt community members have a shared understanding that EMTs and paramedics must remain professional at all times, and that knowledge can sometimes influence the way medical providers are treated in the field:
…and your hands are tied with that. Not like I'm out to physically assault anybody, but a lot of the things that you hear and a lot of the ways that you're expected to act because the patient knows that your hands are tied, that kind of gives you a different level of treatment towards them, and it's hard. (John, Firefighter‐EMT)
All participants described how they believe that the community has learned how to work the 911 system to their advantage, often calling 911 for non‐emergent medical issues, or entirely non‐medical issues.
We get calls for…the remote…I mean, they were bedridden or whatever. You know what I mean? Or I mean, there's calls where people said I needed my remote over here. (John, Firefighter‐EMT)
Participants talked in tones of fatalism regarding their job risk:
But the problem is, is I guess when we're assaulted they're not arrested because they're intoxicated or because they have a mental emotional problem, and so they tend to do it over and over again. There is no repercussion for their actions. I mean that's my personal opinion. Then there is a lot of drug use and there is a lot of alcoholism and just no respect period for life. (Mary, Firefighter‐EMT)
I don't know if you can ever fix it. You can educate people but people are going to call. Their emergency is their emergency. We – I can say it's not an emergency but they think it's the worst thing that ever happened to them today. We could put in deterrents, but I mean right now the [City name] does not charge for an ambulance to come to your house. There needs to be a way to make these people pay. If it's – if you're going to call the ambulance, this is how much it costs. That would definitely be a deterrent and of course, education. I think we could definitely do a better job with education. (Robert, Firefighter‐EMT)
Participants reflected on how this sense of entitlement puts them in danger every time they need to respond to a non‐emergent call because they drive with the same lights, sirens, and speed they would for a true medical emergency. A female paramedic explains:
People don't realize that it's not just about your loved one that you call for. You're jeopardizing also the people who you call to respond to your house. You've gotta think – they don't think about us. It's always just them, them, them. (Anna, Paramedic)
Psychological Impact
Although we asked participants about the physical injury they sustained after a patient‐initiated violent injury, we were surprised by their interest in discussing the event's psychological impact. Participants spoke about feeling defensive, anxious, and detached after facing a violent encounter. A female paramedic shared how her interactions with patients changed after experiencing a violent encounter:
I'm more like ready…I don't get that close to a patient that I feel…can become combative to me…there's a look about a lot of them. You just know that they're not happy when you pull up, and they're not happy for a reason. They're gonna take it out on somebody. I don't get close to them. I sit behind them. I put my monitor sideways with my blood pressure cuff and pulse on them. They're strapped in, seat belted. I'm not, so I can run out the side door if I need to. But I'm not getting too close. (Jane, Paramedic)
This change in approach can have implications for the quality of care that a paramedic or EMT provides in that care may be compromised after experiencing a violent attack:
…it's always….on your mind going forward. You know what I mean? You can only live by what happened to you in the past. And now your perception, the way I'm doing my job now, the way you're looking at stuff now is different. (John, Firefighter‐EMT)
The subsequent vulnerability and negative psychological impact plays a significant role in whether an EMS responder chooses to report an incident and proceed with pressing charges against their attacker. It can also impact whether or not they are able to do their job properly.
Leadership Support
Participants described the role that leadership plays when dealing with line of duty patient‐initiated violent injury. The majority of the paramedics and EMTs felt unsupported by fire department leadership when an injury occurred:
…they're not saying 'oh, I hope you get better. I'm sorry this happened to you.' It is more like watch yourself, and that's the way I take it. I feel like they're not concerned about my wellbeing. They're concerned about the patient and that I did a report, not my wellbeing. (Mary, Firefighter‐EMT)
Paramedics and EMTs described a very different organizational response to a firefighter being injured versus an EMT being injured. Participants felt that firefighters were more strongly supported by the department when they needed medical attention, whereas EMTs and paramedics were often unsupported and rushed back into service due to staffing and resourcing needs.
So when you work in a department that's the majority of firefighters. And the minority is paramedics. It makes everything difficult for us to get our needs because the larger has the bigger voice, and we don't. (Jane, Paramedic)
Paramedics and EMTs commented that leadership might say they are supportive, but their actions do not always follow their words:
…the only thing that I could say is that if you want to be a role model to someone and you want people to be treated a certain way, then to do that, you need to start doing it and showing. I don't see that in this department at all. We have a big communication problem here, a big lack of communication. (Jane, Paramedic)
Participants expressed concern of being held liable by the fire department if they leave a scene out of regard for their safety without providing care. A male firefighter‐EMT shares his apprehension with deserting a volatile patient in the back of an ambulance:
I can see myself getting in trouble for doing that, for abandoning the patient and [abandoning all my equipment]. If I get out of that medic unit and then all my drugs are stolen because he runs out the back of the door, I'm going to be held liable. And I feel like we're held liable more than we should be. (James, Firefighter‐EMT)
Fear of punishment via transfer or retribution by leadership also appears to be related to the issue of underreporting. A male EMT explains, “I do feel that there are other members out there that, if they were injured, they feel that it could negatively impact, whether it's a promotion or a transfer that they're going for” (James, Firefighter‐EMT). Another EMT agrees with this fear of reporting incidents because of the fear that it could negatively impact their career in the future: “You try to avoid having your name go down there [Headquarters] at all. And that's why a lot of guys don't – they don't report anything” (Mary, Firefighter‐EMT). Across all focus groups and interviews, participants described the important role that leadership can play and the value that a supportive organization can provide to a workforce that feels under‐resourced and unsupported on the issue of patient‐initiated violence.
Legal Process
Assaulting a first responder is a felony in the state in which the study took place. Paramedics and EMTs reported multiple issues with the legal process and its varying outcomes after a patient‐initiated violent injury occurred. Participants indicated that they felt re‐victimized by the judicial process. The combination of having to face their assailants, having to retell their stories, and having no support from the fire department had a negative effect. One female paramedic shares her story:
…so you're in this room first of all feeling uncomfortable…I know no one here…[The man that] sexually assaulted me and physically assaulted me…I didn't know he was sitting right behind me the whole time. No one told me…And then he got up on the stand, and then they wanted me on the stand repeating in front of all these people I don't know what he had said to me word for word. That's embarrassing and humiliating. I just want to be out of here. I could care less now. (Jane, Paramedic)
Participants indicated not having support or protection from leadership in the department during court proceedings.
I know we have a law here that if you assault a paramedic, firefighter, police…you're supposed to be charged with a felony. That rarely ever happens. You know, most of the time, you go in there alone…Our medics go alone…You sit there alone…And [the assailant] will explain how sorry they are and what they did to you. And the judge says, 'okay'…And that's all you get. (Jane, Paramedic)
The constant feeling of having no confidence in the judicial system is one that echoed continuously. Paramedics and EMTs expressed dissatisfaction with the lack of repercussions attackers faced, which contributes to the problem of underreporting and a culture of silence. Participants felt that reporting incidents and pressing charges was ultimately pointless because they believed the cases would not be fully prosecuted in the courts. Their reasons included charges being diminished or dropped due to the perpetrators characteristics (such as mental illnesses, medical problems, etc.). A male EMT shares his perception:
They [police officers] were totally disheartened. And they came to me outside the courtroom and they were like, “See?” They said this is why we let people go, because…we're putting our self in jeopardy and the court just lets them go…There's no confidence [in the system] because these people get off…You shouldn't be able to do that to someone who's trying to help you. Felony assault should stick. (John, Firefighter‐EMT)
Training
Participants in this study reported that there was no part of their EMS training that made them knowledgeable about the risks from combative patients or familiar with protocols for self‐protection during patient care.
No, basically in a nutshell, no matter how much the training was, in a nutshell comes down to suck it up. No matter what someone gives you, suck it up. Smile. Wave. They could be spitting on you. Just take it, because you can in no way retaliate, because this person, they have the upper hand on you no matter what, and they called you and they're the ones expecting you to do everything that they want you to do…(John, Firefighter‐EMT)
It wasn't really training on an assault. It was more like you get to see people at their worst. They might lash out. You have to deal with a lot of drama, but they never really said you might get assaulted or whatever like that, but so we didn't really go over that. We went more over driving safety, the safety of the patient, but then they always say, you know wear your gloves. Try to be careful, you know somebody is violent you back away, but they don't really pound it in your head. (Mary, Firefighter‐EMT)
In conversations with the larger EMS community in the United States, there is no standardized training program on patient‐initiated violent injury to EMS responders.
Prevention Versus Protection
As public health scientists, we asked participants for primary prevention suggestions to prevent or mitigate a patient‐initiated violent injury from occurring in the first place (such as de‐escalation techniques, cultural competency, and curbside first aid). We were surprised when our questions were met with self‐preservation responses such as guns, tasers, mace and bulletproof vests.
Female Speaker 1: I want a taser.
Female Speaker 2: Taser. I agree.
Female Speaker 1: I want a taser and I want some mace.
Female Speaker 2: Or mace. Exactly.
Female Speaker 1: But the first choice would be a taser, because I'm taking you.
Female Speaker 2: I agree with that. I mean, and you gotta remember, them tasers are recorded. So it's not like we can run around having taser fights, you know, tasering each other.
Female Speaker 1: I'm tasing first, and asking questions later.
Female Speaker 3: They're legally recorded. Every time you discharge that taser, it's recorded. It's not like they're – even the cops are recorded. So as many times as they push that damn button, there's a recording for that. So if they're going around being abuses of it, people know. It's not something that is not controlled. It's very controlled.
Female Speaker 1: You know, so I mean, like I said, if they want to give us something, you know, I mean, the taser would be my first choice. My real first choice would be a gun, but I know they're not gonna do that. I know in some cities –
Female Speaker 2: Some cities I know carry the guns.
When we did get to talk about primary prevention strategies, the participants expressed the belief that department leadership would not take such training seriously or support it with the required resources:
Nicole: But I really think that a lot of us, even the men need a way to defend themselves, you know, need that. If you've got this great big old bag on your back, the bag weighs maybe 30 pounds or more. That is a weapon. Well, that O2 bottle is a weapon, too. I mean, we all know that because I think we've all had to use an O2 bottle once or twice.
Elizabeth: It's called oxygen therapy.
Nicole: Exactly. So there are a lot of tools that are not tools, fighting tools, that we can incorporate into a protective something, you know, if taught how to use it.
Kelly: I deal with the mental emotional aspect of it, because most of the time when you're dealing with these situations, they're either intoxicated, on drugs, they're having a mental emotional breakdown, whether it's they're angry, whatever. It's a mental emotional thing. And my supervisor there was saying the same thing. He was like – he has asked about incorporating that into some of our training. I don't know if it's because the fire department feels as though they're the fire department, and if they don't ask for it, then they don't want it, or I don't know. I don't know what their reasoning is.
Along with the lack of communication from leadership, participants also commented on the lack of training being offered on the issue of patient‐initiated violence. Participants expressed frustration, feeling as though they were not properly trained or resourced to deal with the patient‐initiated violence they were facing in the field.
But I think they need to become more open to different trainings…I think they just need to be more open and stop being more conscious of them being the fire department and making their – I mean, I can't say that, because I don't know what happens at the top. But I think they really need to take into consideration us and these different types of trainings and stop shunning them to the side if it ain't something that they came up with or whatever. I think they just need to be more open to it, especially if it's gonna help in the long run, because no matter how much we talk about it, if they're not open to it, it's what's the point.” (Kelly, Paramedic)
Work Environment
All participants described their job as a paramedic or EMT as stressful. A female paramedic describes her perception of the EMS division:
…our department is overworked and overstressed. We have a lot of calls. When we don't have the ambulances to respond to the calls because we don't have the resources, but we do the best that we can. (Jane, Paramedic)
I believe that we're good people. I believe that we're just as good as the firefighters and police, and that we're treated differently. For what reason, I don't know why. I don't think it's fair… when you've got these people who are dedicated who come in all the time and are willing to risk their lives for other people and you treat them like crap, how do you expect that they're gonna treat other people? The same way. Abuse is done by abuse. And I don't mean to get upset, but it's frustrating. It really, really is frustrating. (Jane, Paramedic)
Participants expressed feeling overworked and burnt out, which can have a major impact on how long a person will continue to work in a particular field or position.
…I don't think I should be that worried about being assaulted for a person that I'm supposed to be helping. I mean, I really don't think it's fair. But it's the only option that I have because I have a department that doesn't back us. And also the judicial system doesn't either so, you know, I have to take care of myself and my family. We all do different things. Some people will pick up an oxygen bottle, and they will. Some people will fight them back. Some people will not tell anyone. Some people will tell everyone. And then, you know, you go home, you take it all in, and you go back the next day and [you're] expected to be the same person. You're not. Every time someone does something to you, you're different than you were the day before… (Jane, Paramedic)
DISCUSSION
By utilizing both quantitative and qualitative data, we were able to best express the impact of patient‐initiated violence on paramedics in a large urban fire department (Fig. 2). We identified that women were more likely to be paramedics than firefighters (OR 15.3, 95%CI: 11.1–20.9), and paramedics were more likely to be assaulted by patients than firefighters (OR 14.4, 95%CI: 9.2–22.3). The association of gender and patient‐initiated violence was totally mediated through occupation: the crude association of 6.26 (95%CI 3.83–10.23) became non‐significant after controlling for the effect of occupation (AOR 1.64; 95%CI 0.94–2.85). The Sobel test for mediation showed a significant result (z = 8.34, P < 0.001) (Fig. 1). This mediation analysis reflected what was reported in the qualitative phase: that gender was not a meaningful predictor of patient‐initiated violence. From the interviews and focus group eight themes emerged: factors relating to underreporting, dispatch, community expectations, psychological impact, leadership/policy, the legal process, training, and the work environment. We learned that there is a disconnect between paramedics and EMTs in the field and the dispatchers who collect information about the medical emergency. This apparent gap in communication leaves the paramedics and EMTs vulnerable in precarious environments. Improvements in the specificity of information would allow for the provision of optimal patient care, while prioritizing the safety of the EMS providers. We believe the department's computer‐aided dispatch (CAD) system should utilize a flag that dispatchers could use to alert medics that a destination is the location of a previous patient‐initiated violent injury. Conversations with leadership in the department have suggested that this flag capability exists, but whether it is widely and properly utilized is undetermined. In conversations with the Assistant Chief of EMS for the Dallas Fire Department, this technique is in use in their city system (Norman Seals, personal communication). In Pennsylvania, the Montgomery County Department of Public Safety's Division of Emergency Medical Services uses a similar flag in its county‐wide dispatch system (Tom Garrity, personal communication).
Figure 2.
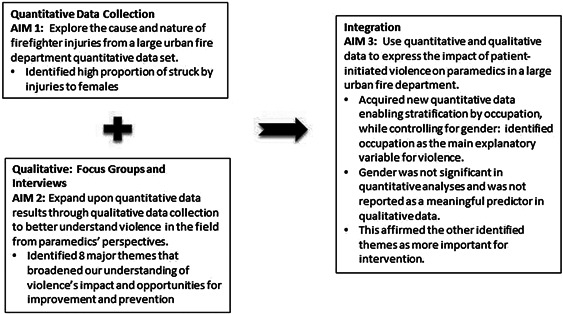
Convergent parallel mixed methods design.
We found there is a lack of knowledge and skills on how to prevent these violent attacks from occurring, which could be addressed partly through training opportunities. There is a free online training and education course available on the Center for Disease Control and Prevention website [Center for Disease Control and Prevention, 2013] that is used to train healthcare workers on how to handle violent patients. The EMS community has also developed an industry‐specific training that emphasizes de‐escalation over self‐defense or weapons [Defensive Tactics for Escaping, Mitigating, Surviving, 2015].
EMS responders have constant interaction with community members as they provide pre‐hospital care. In this study, we heard from medics that community members are experiencing stress due to multiple factors including poverty, violence, and lack of healthcare access. Participants felt that the community was seeing them as outlets for this stress.
One of the participants recommended posting signage that states, “It is a felony to assault a first responder” in the back of ambulances to deter patients from assaulting EMS workers. Such signage is currently in use in the city's public transportation system and is widely used in Canada and the United Kingdom. In addition to informing the public, such a sign would show fire department support for the paramedics—an overture strongly needed based on the stress load participants were observed to be carrying.
The observations paramedics had about the stress their communities are currently undergoing, coupled with their own reflections on their stressful work environment is reflective of recent events in Ferguson, Missouri. A stressed workforce responding to a stressed community during a stressful event can have unwanted consequences. The “taser” dialog about wanting self‐defense training and defensive equipment is indicative of the stressful working conditions participants described. This way of thinking demonstrates that our participants believe assaults are inevitable and the only way to remain safe is to be armed with weapons against these combative patients. The paramedics in this fire department responded to about 750 calls a day. First responders who are overworked and do not have sufficient time to recover from the intensity of their job demands, have little to give to the communities to which they respond. From the fire department's perspective, it can reduce the stress levels of its medics by evaluating opportunities to add more paramedics to the roster, ensuring medics have food and rest breaks during their shifts to encourage recovery from work, and addressing medics' need for support during legal proceedings after an assault occurs. Resolving the community's stress may be better served by comprehensive risk reduction techniques among all city agencies. Our study was limited by its scope in that we spoke only with medics and not with the community. Future work intends to elicit the perceptions and experiences community members have had with the department.
There were multiple strengths associated with the study. Conducting interviews with EMS responders who experienced a violence‐related injury from a patient provided an in‐depth understanding of the multiple factors that increase a paramedic or EMT's susceptibility to violence. Conducting in‐person interviews allowed us to establish a rapport, ask in‐depth questions, and ask for clarification of information. With the knowledge gained from the interviews and focus groups, we can begin to make recommendations to the fire department to produce a safer work environment for EMS workers who provide care for patients in urban settings. This manuscript was shared with fire department leadership prior to its submission for publication.
Several limitations are also present in our research. Our study participants originated from one fire department; therefore, our results are not generalizable to all fire‐based EMS work in the United States. The qualitative arm of the study interacted with a small percentage of the EMS workforce in this department. Although data saturation was achieved during the interviews and focus group, the results of our study may not represent all viewpoints of EMS providers within the department. Additional research should elicit perspectives from leadership within the fire department, as well as community members, in order to ascertain a more comprehensive picture of the violence issue. Additionally, objective assessments of department‐wide stress levels, job satisfaction, and work control should be assessed using currently available validated instruments.
CONCLUSION
This study investigated a large urban fire department's injuries to paramedics and EMTs from patient‐initiated violence. We found that women had sixfold higher odds than men of experiencing a patient‐initiated violent injury. However, the association of gender and patient‐initiated violent injury was totally mediated through occupation. Women were 15‐fold more likely to be paramedics then firefighters, and paramedics were more 12‐fold more likely than firefighters to experience a patient‐initiated violent injury.
Factors relating to underreporting of injury, non‐specific information from dispatchers, community expectations, psychological impact of the injury, leadership support, lack of procedural justice from the legal process, training needs, and the work environment were raised by our focus group and interview participants. These findings provide multiple opportunities for intervention development to improve EMS responder safety and satisfaction with their work environment.
The addition of qualitative data to quantitative findings greatly enriched our understanding of risk factors and opportunities for prevention of patient‐initiated violent injury to EMS responders.
DISCLOSURE BY AJIM EDITOR OF RECORD
Paul Landsbergis declares that he has no conflict of interest in the review and publication decision regarding this article.
ACKNOWLEDGMENTS
This research was supported by the Federal Emergency Management Agency (FEMA) Assistance to Firefighters Grant Program, Fire Prevention and Safety Grants (Research & Development)‐grants numbers EMW‐2009‐FP‐00427 and EMW‐2012‐FP‐00205, and the National Institutes of Health, Opening Doors Training Program: 1R25MD006792‐01. The fire department in this city preferred to remain anonymous. We wish to thank them, the local union, the city's risk management department for their support and assistance with the design and implementation of this study. Jasmine Yolanda Wright, MPH was violently taken from us in July 2015. We dedicate this study to her, and to the study participants who have responded to situations like hers too many times.
Current address of Brittany Barnes is Center to Advance Palliative Care, New York, NY.
REFERENCES
- Bigham BL, Jensen JL, Tavares W, Drennan IR, Saleem H, Dainty KN, Munro G. 2014. Paramedic self‐reported exposure to violence in the emergency medical services (EMS) workplace: A mixed‐methods cross‐sectional survey. Prehosp Emerg Care 18(4):489–494. [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics [BLS]. 2007. Nonfatal occupational injuries and illnesses requiring days away from work. [Internet] Press release. [cited 2015 September 3]. Available from: http://www.bls.gov/news.release/osh2.nr0.htm
- Center for Disease Control and Prevention [CDC]. 2013. Workplace Safety & Health Topics: Occupational Violence [Internet] Atlanta (GA): National Institute for Occupational Safety and Health; [cited 2015 September 3]. Available from: www.cdc.gov/niosh/topics/violence/training_nurses.html
- Center for Disease Control and Prevention [CDC]. 2014. Emergency Medical Services Workers: Overview [Internet] Atlanta (GA): National Institute for Occupational Safety and Health; [cited 2015 September 3]. Available from: http://www.cdc.gov/niosh/topics/ems/
- Center for Disease Control and Prevention [CDC]. 2014. Emergency Medical Services Workers: Injury and Illness Data‐2012 Data [Internet] Atlanta (GA): National Institute for Occupational Safety and Health; [cited 2015 September 3]. Available from: www.cdc.gov/niosh/topics/ems/data2012.html
- Center for Disease Control and Prevention [CDC]. 2014. NIOSH Workplace Safety and Health Topics. Occupational Violence. [Internet] Atlanta (GA): National Institute for Occupational Safety and Health; [cited 2015 September 3]. Available from: http://www.cdc.gov/niosh/topics/violence/
- Creswell JW, Plano Clark VL. 2011. Designing and conducting mixed methods research. Los Angeles: Sage; pp. 77–81. [Google Scholar]
- Defensive Tactics for Escaping, Mitigating, Surviving: DT4EMS' Escaping Violent Encounters (EVE) . 2015. [Internet]; [cited 2015 September 4].
- Gates DM, Gillespie GL, Succop P. 2011. Violence against nurses and its impact on stress and productivity. Nurs Econ 59(2):66. [PubMed] [Google Scholar]
- Maguire BJ, O'Meara PF, Brightwell RF, O'Neill BJ, Fitzgerald GJ. 2014. Occupational injury risk among Australian paramedics: An analysis of national data. Med J Aust 200(8):477–480. [DOI] [PubMed] [Google Scholar]
- Maguire BJ, Smith S. 2013. Injuries and fatalities among emergency medical technicians and paramedics in the united states. Prehosp Disaster Med 28(4):376–382. [DOI] [PubMed] [Google Scholar]
- National Fire Protection Association. 2014. US Fire Department Profile 2013 [Internet] Quincy, MA [cited 2015 September 3]. Available from: www.nfpa.org/research/reports‐and‐statistics/the‐fire‐service/administration/us‐fire‐department‐profile.
- Sobel ME. 1982. Asymptotic confidence intervals for indirect effects in structural equation models. Sociolog Methodol 13:290–312. [Google Scholar]
- Taylor JA, Davis AL, Barnes B, Lacovara AV, Patel R. 2015. Injury risks of EMS responders: Evidence from the national fire fighter near‐miss reporting system. BMJ Open 5(6):e007562, 2014–007562. [DOI] [PMC free article] [PubMed] [Google Scholar]


