Abstract
Background:
With the progress of perinatal medicine and neonatal technology, more and more extremely low birth weight (ELBW) survived all over the world. This study was designed to investigate the short-term outcomes of ELBW infants during their Neonatal Intensive Care Unit (NICU) stay in the mainland of China.
Methods:
All infants admitted to 26 NICUs with a birth weight (BW) < l000 g were included between January l, 2011 and December 31, 2011. All the data were collected retrospectively from clinical records by a prospectively designed questionnaire. The data collected from each NICU transmitted to the main institution where the results were aggregated and analyzed. Categorical variables were performed with Pearson Chi-square test. Binary Logistic regression analysis was used to detect risk factors.
Results:
A total of 258 ELBW infants were admitted to 26 NICUs, of whom the mean gestational age (GA) was 28.1 ± 2.2 weeks, and the mean BW was 868 ± 97 g. The overall survival rate at discharge was 50.0%. Despite aggressive treatment 60 infants (23.3%) died and another 69 infants (26.7%) died after medical care withdrawal. Furthermore, the survival rate was significantly higher in coastal areas than inland areas (53.6% vs. 35.3%, P = 0.019). BW < 750 g and GA < 28 weeks were the largest risk factors, and being small for gestational age was a protective factor related to mortality. Respiratory distress syndrome was the most common complication. The incidence of patent ductus arteriosus, intraventricular hemorrhage, periventricular leukomalacia, bronchopulmonary dysplasia, retinopathy of prematurity was 26.2%, 33.7%, 6.7%, 48.1%, and 41.4%, respectively. Ventilator associated pneumonia was the most common hospital acquired infection during hospitalization.
Conclusions:
Our study was the first survey that revealed the present status of ELBW infants in the mainland of China. The mortality and morbidity of ELBW infants remained high as compared to other developed countries.
Keywords: Extremely Low Birth Weight, Infant, Mortality, National Survey
INTRODUCTION
Extremely low birth weight (ELBW, birth weight [BW] < 1000 g) infants have a very special high risk of developing varied morbidities and mortality. Recent advances in perinatal care including surfactant replacement therapy, mechanical ventilation (MV), and neonatal transfer; however, have resulted in significantly increased survival rates for ELBW infants. Early in the 1990s, it has been reported that the survival rate of ELBW infants significantly increased from 49% to 68% in the United States.[1] In Finland, a nationwide survey showed that the overall survival rate of ELBW infants were 60% and 65% between 1996–1997 and 1999–2000.[2] In Japan, it was also reported that overall mortality and mortality rate of ELBW infants in 2005 during treatment in the Neonatal Intensive Care Unit (NICU) were 13.0% and 17.0%, respectively, which were lower than that in the year of 2000.[3] Similarly, a population-based study of consecutive ELBW born in the state of Victoria during 2005 showed that the survival rate was 89.7%.[4] These studies have demonstrated that improved neonatal intensive care for ELBW infants over the past decades has significantly decreased the overall mortality rate. However, most of these studies on survival and morbidity of ELBW infants were conducted in the developed countries. Very few data have been reported to show the trends in mortality and morbidity rates among ELBW infant in the developing countries such as China.
Thus, to investigate the mortality and morbidity of ELBW infants, along with the risk factors and disease burden, a multi-center survey was performed to collect a series of random data nationwide. The results of this study were compared with the outcomes from other countries and expected to provide valuable information for possible further care design to improve the overall survival rate.
METHODS
Study design
The 33 NICUs which participated in this survey are collaborative tertiary hospitals of the Group for Neonatology of the Chinese Medical Association. These NICUs locate in six Chinese regional areas, which are representatives of health facilities offering newborn intensive care in their respective areas. In order to collect data consistently, in each NICU, the same international criteria were followed to determine disease types and stages. Children's Hospital of Zhejiang University School of Medicine was agreed to coordinate this survey study, where all the data were collected, stored, and analyzed with confidence after received from other NICUs.
This study was approved by the Ethics Committees of Children's Hospital of Zhejiang University School of Medicine.
Subjects and data collection
The study population consisted of ELBW infants who were admitted to all these NICUs between January 1, 2011 and December 31, 2011. Among these NICUs, 26 of 33 NICUs (8 general hospitals, 12 children's hospitals, and 6 maternity hospitals) provided data for this ELBW infant study, whereas other 7 NICUs did not due to no ELBW infants admitted in 2011. Data collected from these NICUs were based on a prospectively designed questionnaire including neonatal demographics, major complications, therapy, prognosis, and cost of hospital stay. The cost mainly consisted of the medicine, treatment, nursing care, examination, and daily bed fee; and other subject information of this study was collected retrospectively from clinical records and neonatologist by a written survey.
Definition and classification
In order to maintain consistency of this study, the same international criteria were followed. Small for gestational age (SGA) was described as a neonate whose BW or birth crown-heel length is < l0th percentile for gestational age (GA) according to Fenton intrauterine growth curves.[5] Respiratory distress syndrome (RDS) was diagnosed in preterm infants with the onset of respiratory distress shortly after birth and a compatible chest radiograph appearance.[6] Bronchopulmonary dysplasia (BPD) and the grade of BPD were defined by the National Institutes of Health Workshop severity-based diagnostic criteria.[7] Patent ductus arteriosus (PDA) in our survey was defined as a hemodynamically significant PDA, which required pharmacological therapy or surgical ligation.[8] The criteria utilized in our survey for the diagnosis of necrotizing enterocolitis (NEC) and for grading the severity of disease were based on Bell's stage.[9] Retinopathy of prematurity (ROP) and the graded standard were defined as the international classification of ROP.[10] The diagnosis of intraventricular hemorrhage (IVH) and severity of IVH was according to cranial ultrasound. Periventricular leukomalacia (PVL) was defined as degeneration of white matter adjacent to the cerebral ventricles following cerebral hypoxia or brain ischemia and diagnosed by cranial ultrasonography or magnetic resonance imaging (MRI).[11] Hospital acquired infection included ventilator associated pneumonia (VAP), sepsis, and peripherally inserted central catheter (PICC) associated infections. VAP was defined as a new change of clinical signs and chest radiograph plus positive low airway secretion culture;[12] sepsis was defined as clinical signs and positive blood culture; and PICC associated infections was defined as positive culture of blood and tip of PICC line at the same time.[13] Hospital acquired infection included these three kinds of infections with a positive culture. Survival was defined as the infants being alive and underlying diseases cured at the stage of home discharge.
Statistical analysis
All statistical analyses were performed using SPSS version 16.0 software (SPSS Inc., Chicago, IL, USA). Continuous variables were summarized as the median and range, or the mean ± standard deviation (SD), depending on whether their distributions were or were not highly skewed. Comparisons of categorical variables were performed using the Pearson Chi-square test. A Kruskal–Wallis test or median test was applied for the comparisons of continuous variables. Binary Logistic regression analysis was applied to detect risk factors for mortality of ELBW infants. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated for statistically significant variables. P < 0.05 was considered as statistically significant in all tests if applied.
RESULTS
Demographics of extremely low birth weight infants and the medical cost
During the 1-year survey, a total of 258 ELBW infants were admitted to 26 NICUs including 149 (57.8%) males and 109 (42.3%) females. According to the BW, ELBW infants were divided into two subgroups: BW < 750 g: 30 infants; BW between 750 and 999 g: 228 infants. The infant numbers at 24–25, 26–27, 28–29, and more than 29 weeks GA were 26, 89, 81, and 62, respectively. The mean GA of all the ELBW infants was 28.1 ± 2.2 weeks, and the mean BW was 868 ± 97 g. Eighty-eight subjects (34.1%) were classified as SGA. Of all ELBW infants, 19.4% (n = 50) were born under the assisted reproduction using hyper-stimulation or in-vitro fertilization. The average cost of NICU stay for each ELBW infant was 10,244 China Yuan (CNY) for nonsurvivors and 62,206 ± 39,762 CNY for survivors. The characteristics of the ELBW infants in this study were presented in Table 1.
Table 1.
Characteristics of ELBW infants in BW categories
| Characteristics | BW (g) | Total | |
|---|---|---|---|
| <750 | 750–999 | ||
| Cases, n (%) | 30 (11.6) | 228 (88.4) | 258 (100) |
| GA (weeks), mean ± SD | 27.4 ± 2.5 | 28.1 ± 2.2 | 28.1 ± 2.2 |
| BW (g), mean ± SD | 675 ± 66 | 893 ± 67 | 868 ± 97 |
| Male, n (%) | 14 (46.7) | 135 (59.2) | 149 (57.8) |
| SGA, n (%) | 20 (66.7) | 68 (29.8) | 88 (34.1) |
| Assisted reproduction, n (%) | 11 (36.7) | 39 (17.1) | 50 (19.4) |
| Survive at discharge, n (%) | 9 (30.0) | 120 (52.6) | 129 (50.0) |
| LOHS (days), median (range) | |||
| Nonsurvivor | 1 (33) | 3 (143) | 2 (143) |
| Survivor | 82 (122) | 63 (138) | 64 (138) |
| Cost of NICU stay (CNY, ×103) | |||
| Nonsurvivor, median (range) | 9.330 (1.265–67.687) | 10.244 (0.060–342.777) | 10.244 (0.060–342.777) |
| Survivor, mean ± SD | 90.686 ± 65.718 | 60.015 ± 36.580 | 62.206 ± 39.762 |
GA: Gestational age; BW: Birth weight; LOHS: Length of hospital stay; CNY: China Yuan (6.2 CNY=1 USD); SD: Standard deviation; NICU: Neonatal intensive care unit; SGA: Small for gestational age; ELBW: Extremely low birth weight.
Mortality and survival rate
The overall survival rate at discharge was 50.0%. Sixty infants (23.3%) died despite aggressive treatment applied, and 69 infants (26.7%) died after medical care withdrawal. Of the total 129 infants who died during hospitalization, 52 cases died within 24 h of life, and another 45 cases died in the first 7 days of life. Survival rate was improved with increased GA (P < 0.001). The percentage of death and survival in relation to GA of the ELBW infants was summarized in [Figure 1].
Figure 1.
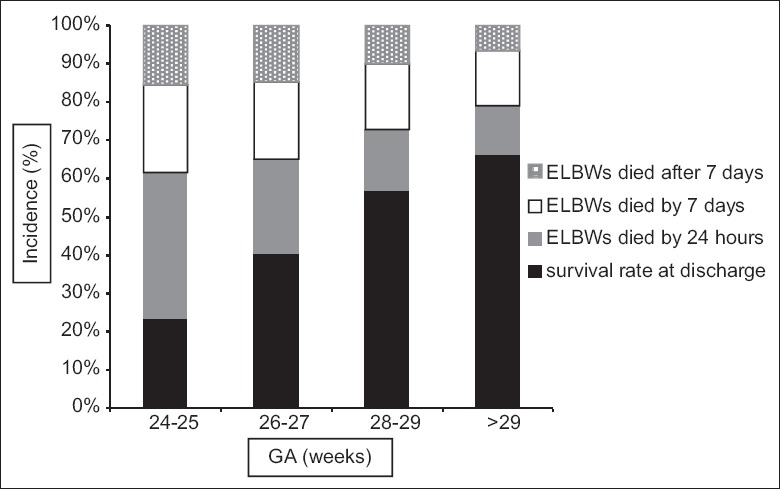
The percentages of extremely low birth weight (ELBW) infants who survived or died at different times in relation to gestational age (GA). Figure 1 shows that survival rate was improved with increased GA (P < 0.001). Moreover, the mortality of the first 7 days decreased with increased GA.
Morbidity and complications
The clinical information of total 206 ELBW infants who survived more than 24 h was analyzed. RDS was the most common complication in ELBW infants. There were 189 infants who had developed RDS, of whom 72.0% (n = 136) have received surfactant replacement therapy. Respiratory support was used for all the infants with RDS including 41.7% received nasal continuous positive airway pressure, 46.6% received conventional MV, and 18.0% received high-frequency oscillation ventilation. Hemodynamically significant PDA was detected in 26.2% (n = 54) of these 206 ELBW infants. To achieve medical closure, indomethacin was used in 7.3% (n = 15) infants, and ibuprofen was used in 18.9% (n = 39) infants. These two kinds of medicine were administrated orally. In addition, the surgical closure was conducted in 1.5% (n = 3) infants who had failed medical treatment previously.
Moreover, there were 178 infants who had at least one time head ultrasound or MRI. As a result, 33.7% (n = 60) infants were found to have IVH, and 12.9% (n = 23) were IVH grade III–IV. The incidence of PVL in all these 178 infants was about 6.7%.
In addition, a total of 133 infants survived more than 28 days and reached a corrected GA of 36 weeks. The overall incidence of BPD was 48.1% (n = 64) including 40.6% mild BPD, 3.0% moderate BPD, and 4.5% severe BPD. For all infants with BPD, 14.1% (n = 9) were treated with diuretics, 10.9% (n = 7) were treated with glucocorticoids, and 34.4% (n = 22) were treated with a combination of diuretics and glucocorticoids.
The ROP screening in China was initiated at 4–6 weeks after birth or a corrected GA of 32–34 weeks. The percentage of ROP screening completion among these ELBW infants was 90.0% during hospitalization. As a result, 140 infants met the screening criteria, with the incidence of ROP as 41.4%. Finally, 20 infants (14.3%) required laser therapy for treating ROP stage 2 or 3. Interestingly, the incidence of IVH, IVH grade III–IV, PVL, PDA, BPD, and ROP of the infants decreased steadily with increased GA [Figure 2].
Figure 2.
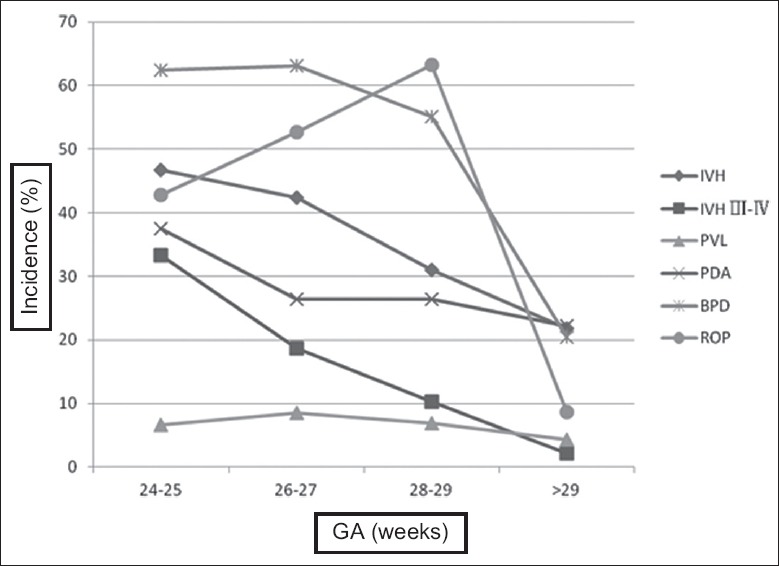
The incidence of complications at each gestational age (GA) group. Figure 2 shows that GA-specific rates of intraventricular hemorrhage (IVH), IVH grades III–IV, periventricular leukomalacia (PVL), patent ductus arteriosus (PDA), bronchopulmonary dysplasia (BPD), and retinopathy of prematurity (ROP) decreased (P < 0.05). P value means the contrast between different GA groups.
Among these 206 infants who survived more than 24 h, 45 infants (21.8%) had a total of 65 episodes of hospital acquired infection including 7.3% (n = 15) infants with more than two episodes. The hospital acquired infections included three types of infections: VAP, sepsis, and PICC associated infections. VAP was the most common infection during hospitalization, accounting for 56.9% in total, and most commonly happened in infants at 28–29 weeks. Sepsis that accounted for 40.0% was another most common infection for infants but occurred in infants at more than 29 weeks. PICC associated infections were the least common one and only accounted for 3.1% of total infections. The pathogens of the hospital acquired infection were detected, containing 72.3% (n = 47) Gram-negative pathogens, 16.9% (n = 11) Gram-positive pathogens, and 10.8% (n = 7) fungi. Only 2 (1.8%) of 110 infants inserted a line had a PICC associated infection.
The incidence of NEC was 5.8% (n = 12) for infants who survived > 24 h, of which the incidence of stage I, stage II, and stage III was 2.4%, 1.9%, and 1.5%, respectively; and four infants with NEC have been received surgery.
Hospital and regional differences
The NICUs participating in this study were divided into three groups: Pediatric hospital, maternal hospital, and general hospital. No significant differences were found regarding the mean GA or BW of ELBW infants among these three groups. However, significant differences were found in the survival rate and morbidity: The survival rate was higher in the pediatric hospitals than other two groups of hospitals, while the mortality rate on the 1st day of life was higher in the maternal hospitals than other two (P < 0. 05) such as the incidence of IVH was the highest at the maternal hospitals (P = 0.00l) [Table 2].
Table 2.
Differences between three types of hospital
| Variables | Pediatric hospital | Maternal hospital | General hospital | P |
|---|---|---|---|---|
| Cases, n (%) | 129 (50.0) | 82 (31.8) | 47 (18.2) | |
| Surviving ELBW infants, n (%) | 80 (62.0) | 29 (35.4) | 20 (42.6) | 0.000* |
| Died by 24 h, n (%) | 11 (8.5) | 35 (42.7) | 6 (12.8) | 0.000* |
| Mean BW (g) | 876 | 862 | 857 | 0.384 |
| Mean gestational week (weeks) | 28 | 27 | 28 | 0.642 |
| IVH, n (%) | 24 (23.3) | 21 (56.8) | 15 (39.5) | 0.001* |
| IVH III–IV, n (%) | 13 (12.6) | 2 (5.4) | 8 (21.1) | 0.129 |
| PVL, n (%) | 3 (2.9) | 4 (10.8) | 5 (13.2) | 0.053 |
| ROP, n (%) | 38 (44.7) | 13 (40.6) | 7 (30.4) | 0.465 |
| NEC, n (%) | 9 (7.6) | 1 (2.1) | 2 (4.9) | 0.380 |
| BPD, n (%) | 36 (42.9) | 14 (48.3) | 14 (66.7) | 0.148 |
| Hospital acquired infection, n (%) | 23 (19.5) | 15 (31.9) | 7 (17.1) | 0.156 |
*P values showed that survival rate and mortality was different between these three types of hospitals, and the incidence of IVH was higher in the maternal hospital. ELBW: Extremely low birth weight; BW: Birth weight; IVH: Intraventricular hemorrhage; PVL: Periventricular leukomalacia; ROP: Retinopathy of prematurity; NEC: Necrotizing enterocolitis; BPD: Bronchopulmonary dysplasia.
In order to compare the difference in survival rate between hospitals from coastal areas and inland areas of China, all participated NICUs were categorized as coastal hospitals and inland hospitals according to their geographic locations. As summarized, there were 17 hospitals with 207 infants from coastal areas and 9 hospitals with 51 infants from inland areas. No significant differences were observed in the mean BW (870 g vs. 856 g, P = 0. 177) and mean GA (28 weeks vs. 28 weeks, P = 0. 634); while the survival rate was significantly higher in hospitals from coastal areas than those from inland areas (53.6% vs. 35.3%, χ2 = 5.499, P = 0.019).
Risk factors associated with mortality
The risk factors analysis was performed to determine any associations between mortality and physical/disease conditions of infants. Totally, 12 variables including sex, BW < 750 g, GA < 28 weeks, SGA, hospital acquired infections, BPD, IVH, IVH grade III–IV, PDA, RDS, surfactant replacement, and NEC were selected and analyzed. As shown in Table 3, 3 of these 12 variables were determined and significantly associated with mortality rate. These three factors included BW < 750 g, GA < 28 weeks, and SGA. Interestingly, SGA was a significantly protective factor regarding mortality rate in ELBW infants [Table 3].
Table 3.
Risk factors for death in ELBW infants
| Risk factors | OR | 95% CI | P |
|---|---|---|---|
| BW <750 g | 4.305 | 1.417–13.079 | 0.042 |
| GA <28 weeks | 2.188 | 1.030–4.650 | 0.010 |
| SGA | 0.310 | 0.143–0.673 | 0.003 |
GA: Gestational age; ELBW: Extremely low BW; OR: Odds ratio; CI: Confidence interval; BW: Birth weight; SGA: Small for gestational age.
DISCUSSION
The quality of public health is closely associated with economic development in the country. Since the l980's, China has made great progress in economy, and improved people life conditions dramatically. Furthermore, the NICUs have been established and covered in almost every province. Several national surveys have showed that the neonatal subspecialty in the mainland of China have been progressing steadily, and also, the medical instruments and new techniques have been improved remarkably.[14,15] However, the preterm birth rate has steadily increased every year. One report from the World Health Organization indicated that the preterm birth rate was more than 10% worldwide, and China was one of the top 10 countries that have the highest number of preterm births.[16] The increased proportion of preterm births may be related with a high risk of infant mortality, although numerous preterm infants have been treated and rescued in China over the past decades.
This study is the first nationwide study, so far as we know, to investigate the short-term outcomes of ELBW infants in the mainland of China. The key criterion to recruit infant subjects was their BW < 1000 g when admitted to NICUs. Therefore, this study was primarily focused on the live-born infants, whereas the stillbirth in the delivery room was not enrolled. From this study, it was showed that the major proportion of our ELBW infants admitted to NICU with BW > 750 g, and the percentage of SGA was quite higher as compared to others.[17,18] Meanwhile, the survival rate of ELBW infants was lower than that in developed countries over the same period.[3,19,20] Our survey showed that the overall survival rate was about 50%, which was comparable with the data from the developed countries during 1980–1990s,[17,21] but higher than that in 2000s.[22] Our survey showed a significant portion of infants (26.7%) died after withdrawal of medical care, accounting for more than half of all the deaths. Similarly, in a recent survey of ELBW infants in one province of China, it was reported that 30.3% infants died after medical care withdrawal, even higher than our results.[23] The termination of medical care for ELBW infants may partially explain the low overall survival rate. Although it was possible that the withdraw decisions had to be made for infants due to the lethal disease progression.
There were other possible issues for parents/guardians considering to terminate intensive treatment for the ELBW infants have been discussed. First, lack of financial support could be the main reason. Though the annual incomes have been improved, the total disease cost is still high for the majority of the population. Our study showed that the mean total cost for infant survivors was 62,206 ± 39,762 CNY, which was nearly 3 times higher than the entire annual income of an urban resident in 2011 (19,118 CNY). Thus, socioeconomic status may have a substantial impact on the parents/guardians’ decisions and the outcomes of ELBW infants. Another possible reason might be the concern of possible severe complications. A large portion of parents concerned about the long-term neurodevelopment sequelae or other serious complications during infant treatment. In addition to the reason of medical care withdraw, another major reason for low survival rate may be related to differences of regions and hospital types. Our study has shown a significant difference in survival rates between hospitals in coastal and inland areas where ELBW infants admitted. The economic imbalance may play a key role in influencing the medical development and technology in different regions. For example, due to the limited medical resources in inland hospitals, many ELBW infants may not be efficiently cared and treated after birth. Even worse, for some of extremely immature infants, their parents may decide to go for no aggressive resuscitation in the delivery room at the prenatal consultation. Because infants with GA < 28 weeks, in general, might be considered as abortion in the early period of time in China. Thus, ELBW infants who were born before 28 weeks may be not resuscitated and transferred, which may partially explain the fact that more ELBW infants died at an early stage in maternal hospitals than other two hospitals.
Our current study confirmed that the survival rate was improved with the increased GAs and BWs, which was consistent with previous results from other investigators.[3,17,20] The Logistic regression analysis for risk factors of mortality has shown that BW < 750 g and GA < 28 weeks were the main prognostic indicators of ELBW infant death. However, which are the bottom lines of GA and BW of infants deemed eligible for resuscitation is still unclear. One example from Dutch centers recommended to provide life support for infants born with GA > 26 weeks but changed this policy to treat infants from GA > 24 weeks in 2011.[24] The American Academy of Pediatrics suggested that noninitiation of resuscitation shall be considered appropriate for newborns of GA < 23 weeks and/or BW < 400 g.[25] In a word, in most developed countries and medical care resources were used to rescue the preterm infants with GA > 24 weeks. However, how to balance the medical burden and long-term outcome of ELBW infants in developing country is still controversial. Based on our results, the mortality and morbidity rates of infants with BW <750 g and/or GA < 28 weeks were significantly higher, although the population size in this study may not be sufficient to represent general ELBW infant population in China. Thus, it is unclear whether GA could serve as an indicator for resuscitation.
The decreased incidence of BPD, ROP, and IVH grade III through IV was related to increased GAs, which was agreed with the previous studies. Though the frequency of ROP screening was as high as 90% in our study, a previous survey based on 16 tertiary class-one hospitals in China reported that the overall screening rate was only 59.94% during hospitalization.[26] Why was the incidence of ROP higher in the infants of 28–29 weeks than in those of 24–25 weeks? The reason may be related to the limit number of infants less than 25 weeks. In contrast, the incidence of PDA and NEC, including PDA with surgical closure and NEC with the surgical intervention was lower than the other studies.[17,20,27] Although the PDAs in our survey, defined as “Hemodynamically significant PDAs,” was different from other studies, one of possible reasons for lower incidence of PDA and NEC in our study as compared to others studies also could be less numbers of the lower GA infants, especially < 25 weeks in this study.
Urrea et al. reported that 55.5% of the neonates with a BW of < 1000 g had at least 1 nosocomial infections episodes during 6 months in a level III neonatal care unit.[28] Mireya et al. also reported that the incidence of nosocomial infection was 74.3/100 admissions and 2.7/100 patient-days.[29] In order to keep consistency of diagnosis standard among different NICUs, the hospital acquired infections in our study only included culture positive VAP, sepsis, and PICC associated infections, with exclusion of conjunctivitis, urinary tract infections, and other kinds of infections. Thus, the inconsonant inclusion criteria may contribute to the lower incidence of nosocomial infections observed in our study. VAP has been described as the most common type of hospital acquired infections in NICUs and associated with increased mortality and prolonged NICU length of stay.[30] In our study, VAP was also the most common cause of hospital acquired infection. However, it was unlikely to be an independent risk factor associated with mortality. In developed countries, Gram-positive bacteria are the most frequently isolated microorganism in hospital infection, with coagulase-negative staphylococcus being the main pathogen.[28,29] Conversely, Gram-negative bacteria were the most common pathogen seen in our report.
One of the limitations in our study is that the mortality of ELBW infants admitted to NICUs may not be representative for general ELBW infant population in China because of exclusion of infants stillborn in the delivery room. Another limitation is that our survey only included 33 large tertiary hospitals, but was not a population-based study. In addition, the classification system of neonatal units in our country has not been strictly set up yet, thus, due to the limitation of neonatal transport resources, a significant part of ELBW infants may be treated in level ΙΙ hospitals. Though the total subjects of our study were limited, our study may represent the medical care level and status for ELBW infants from different regions/hospitals of the mainland. Therefore, our study could be an additive to understand the current survival rate and morbidity of ELBW infants in China, and serve as a benchmark for future investigations and studies, for example, the long-term outcome of the infant survivors in this study would be followed up.
In conclusion, this study has discussed the current status of ELBW infants in the mainland of China. It has confirmed that even with modern technology and rapid development of neonatal intensive care, the survival rate of ELBW infants was still low in China as compared to other developed countries. The high mortality and morbidity remains a challenge issue for each pediatrician to work out.
Acknowledgments
The authors gratefully acknowledge all the institutes and investigators: Anhui Provincial Hospital (Ming-Wu Chen, Wei Shen), BaYi Children's Hospital of the General Military Hospital of Beijing People's Liberation Army (Zhi-Chun Feng), Children's Hospital of Fudan University (Chao Chen), Gansu Provincial Maternity and Children-care Hospital (Fang-Ping Zhao, Xiu-Jing Li), Guiyang Maternal and Child Health Care Hospital (Pin Hu), Women and Children Hospital of Guangdong province (Jun-Ping Wang, Yan-Li Wang), Guangxi Maternal and Child Health Hospital (Xin-Nian Pan, Yan Li), The Third Affiliated Hospital of Guangzhou Medical University (Qi-Liang Cui), Harbin Children's Hospital (Fei Lu), Children's Hospital of Hebei Province (Yao-Fang Xia), Hunan Children's Hospital (Fan Zhang), Hubei Maternity and Child Heath Hospital (Hong-Yan Liu), Togji Hospital Affiliated to Tongji Medical College, Huazhong University of Science and Technology (Li-Wen Chang, Wei Liu, Zhi-Hui Rong), The First Hospital of Jilin University (Ying Liu, Jun Han), Jiangxi Provincial Children's Hospital (Li-Ping Chen, Li-Chun Zeng), First Affiliated Hospital of Kunming Medical University (Mei Wu, Xiang-Ying He), Nanjing Children's Hospital of Nanjing Medical University (Qing Kan), Nanjing Maternity and Child Health Care Hospital Affiliated to Nanjing Medical University (Xiao-Hui Chen), Ningbo Women and Children's Hospital (Ming-Huan Wang), General Hospital of Ningxia Medical University (Wei Wu, Ying-Shan Fei), Qilu Hospital of Shandong University (Jing-Hui Zhang), Quanzhou Women's and Children's Hospital (Rui-Quan Wang), Shanxi Provincial People's Hospital (Yu-Feng Han, Qin Zhang), Shenzhen Children's Hospital (Zhen-Zhu Yu), The Second Affiliated Hospital and Yuying Children's Hospital, Wenzhou Medical University (Su Lin, Si Chen), The First Affiliated Hospital of Medical School, Xi’an Jiaotong University (Mi Xiao, Shu-Juan Fan, Jie Zhang), Women's Hospital, School of Medicine, Zhejiang Univeristy (Ming-Yuan Wu), Zhengzhou Children's Hospital (Hui-Qing Sun), Xiangya Hospital, Central South University (Xiao-He Yu), The First Affiliated Hospital, Sun Yat-sen University (Yi-Juan Li).
Financial support and sponsorship
This work was funded by the grants from National Key Technology Research and Development Program (No. 2012BAI04B04) and Zhejiang Province Ministry of Education (No. Y200908620).
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Yuan-Yuan Ji
REFERENCES
- 1.Wilson-Costello D, Friedman H, Minich N, Siner B, Taylor G, Schluchter M, et al. Improved neurodevelopmental outcomes for extremely low birth weight infants in 2000-2002. Pediatrics. 2007;119:37–45. doi: 10.1542/peds.2006-1416. [DOI] [PubMed] [Google Scholar]
- 2.Tommiska V, Heinonen K, Lehtonen L, Renlund M, Saarela T, Tammela O, et al. No improvement in outcome of nationwide extremely low birth weight infant populations between 1996-1997 and 1999-2000. Pediatrics. 2007;119:29–36. doi: 10.1542/peds.2006-1472. [DOI] [PubMed] [Google Scholar]
- 3.Itabashi K, Horiuchi T, Kusuda S, Kabe K, Itani Y, Nakamura T, et al. Mortality rates for extremely low birth weight infants born in Japan in 2005. Pediatrics. 2009;123:445–50. doi: 10.1542/peds.2008-0763. [DOI] [PubMed] [Google Scholar]
- 4.Doyle LW, Roberts G, Anderson PJ. Victorian Infant Collaborative Study Group. Changing long-term outcomes for infants 500-999 g birth weight in Victoria, 1979-2005. Arch Dis Child Fetal Neonatal Ed. 2011;96:F443–7. doi: 10.1136/adc.2010.200576. [DOI] [PubMed] [Google Scholar]
- 5.Fenton TR. A new growth chart for preterm babies: Babson and Benda's chart updated with recent data and a new format. BMC Pediatr. 2003;3:13. doi: 10.1186/1471-2431-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhakta KY. Respiratory distress syndrome. In: Cloherty JP, editor. Manual of Neonatal Care. 7th ed. Philadelphia: Little, Brown and Company; 2012. pp. 406–16. [Google Scholar]
- 7.Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9. doi: 10.1164/ajrccm.163.7.2011060. [DOI] [PubMed] [Google Scholar]
- 8.Sekar KC. Protective strategies to prevent patent ductus arteriosus. Chin Med J. 2010;123:2914–8. [PubMed] [Google Scholar]
- 9.Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978;187:1–7. doi: 10.1097/00000658-197801000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.An international classification of retinopathy of prematurity. The Committee for the Classification of Retinopathy of Prematurity. Arch Ophthalmol. 1984;102:1130–4. doi: 10.1001/archopht.1984.01040030908011. [DOI] [PubMed] [Google Scholar]
- 11.Volpe JJ. Neurobiology of periventricular leukomalacia in the premature infant. Pediatr Res. 2001;50:553–62. doi: 10.1203/00006450-200111000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Kollef MH. Ventilator-associated pneumonia. A multivariate analysis. JAMA. 1993;270:1965–70. [PubMed] [Google Scholar]
- 13.Levy I, Bendet M, Samra Z, Shalit I, Katz J. Infectious complications of peripherally inserted central venous catheters in children. Pediatr Infect Dis J. 2010;29:426–9. doi: 10.1097/INF.0b013e3181c94d9e. [DOI] [PubMed] [Google Scholar]
- 14.Coordination Group for National Survey of Development in Pediatric and Neonatal Intensive Care Units. Development of pediatric and neonatal intensive care units: Results of a national survey (2000-2009) (in Chinese) Chin J Pediatr. 2011;49:669–74. [PubMed] [Google Scholar]
- 15.Coordination Group for Present Situation of Neonatal Subspecialty in the Mainland of China. Present situation of neonatal subspecialty in the mainland of China: A survey based on 109 hospitals (in Chinese) Chin J Pediatr. 2012;50:326–30. [PubMed] [Google Scholar]
- 16.Geneva: WHO; 2012. [Last accessed on 2012 May 02]. World Health Organization. Born Too Soon: The Global Action Report on Preterm Birth. Available from: http://www.who.int/maternal_child_adolescent/documents/born_too_soon/en/ [Google Scholar]
- 17.Tommiska V, Heinonen K, Ikonen S, Kero P, Pokela ML, Renlund M, et al. A national short-term follow-up study of extremely low birth weight infants born in Finland in 1996-1997. Pediatrics. 2001;107:E2. doi: 10.1542/peds.107.1.e2. [DOI] [PubMed] [Google Scholar]
- 18.Narayan S, Aggarwal R, Upadhyay A, Deorari AK, Singh M, Paul VK. Survival and morbidity in extremely low birth weight (ELBW) infants. Indian Pediatr. 2003;40:130–5. [PubMed] [Google Scholar]
- 19.Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126:443–56. doi: 10.1542/peds.2009-2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hahn WH, Chang JY, Chang YS, Shim KS, Bae CW. Recent trends in neonatal mortality in very low birth weight Korean infants: In comparison with Japan and the USA. J Korean Med Sci. 2011;26:467–73. doi: 10.3346/jkms.2011.26.4.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roberts G, Anderson PJ, Doyle LW. Victorian Infant Collaborative Study Group. Neurosensory disabilities at school age in geographic cohorts of extremely low birth weight children born between the 1970s and the 1990s. J Pediatr. 2009;154:829–34.e1. doi: 10.1016/j.jpeds.2008.12.036. [DOI] [PubMed] [Google Scholar]
- 22.Lau C, Ambalavanan N, Chakraborty H, Wingate MS, Carlo WA. Extremely low birth weight and infant mortality rates in the United States. Pediatrics. 2013;131:855–60. doi: 10.1542/peds.2012-2471. [DOI] [PubMed] [Google Scholar]
- 23.Collaborative Study Group for Extremely Preterm and Extremely Low Birth Weight Infants. Survival and mortality rate of extremely preterm and extremely low birth weight infants admitted to neonatology departments (in Chinese) Chin J Pediatr. 2014;52:729–35. [PubMed] [Google Scholar]
- 24.Sheldon T. Dutch doctors changs policy on treating preterm babies. Br Med J. 2001;322:1383. [Google Scholar]
- 25.MacDonald H. American Academy of Pediatrics. Committee on Fetus and Newborn. Perinatal care at the threshold of viability. Pediatrics. 2002;110:1024–7. doi: 10.1542/peds.110.5.1024. [DOI] [PubMed] [Google Scholar]
- 26.Coordination Group for the Survey of Present Status of Oxygen Use in Premature Infants in NICUs and Prevention and Treatment of ROP. Present situation of oxygen therapy and retinopathy of prematurity management in premature infants in NICUs: A survey based on 16 tertiary class-one hospitals in the mainland of China (in Chinese) Chin J Pediatr. 2012;50:167–71. [PubMed] [Google Scholar]
- 27.Tsao PN, Teng RJ, Wu TJ, Tang JR, Yau KI. Early outcome of extremely low birth weight infants in Taiwan. J Formos Med Assoc. 1998;97:471–6. [PubMed] [Google Scholar]
- 28.Urrea M, Iriondo M, Thio M, Krauel X, Serra M, LaTorre C, et al. A prospective incidence study of nosocomial infections in a neonatal care unit. Am J Infect Control. 2003;31:505–7. doi: 10.1016/s0196-6553(03)00077-4. [DOI] [PubMed] [Google Scholar]
- 29.Mireya UA, Martí PO, Xavier KV, Cristina LO, Miguel MM, Magda CM. Nosocomial infections in paediatric and neonatal intensive care units. J Infect. 2007;54:212–20. doi: 10.1016/j.jinf.2006.03.023. [DOI] [PubMed] [Google Scholar]
- 30.Apisarnthanarak A, Holzmann-Pazgal G, Hamvas A, Olsen MA, Fraser VJ. Ventilator-associated pneumonia in extremely preterm neonates in a neonatal intensive care unit: Characteristics, risk factors, and outcomes. Pediatrics. 2003;112(6 Pt 1):1283–9. doi: 10.1542/peds.112.6.1283. [DOI] [PubMed] [Google Scholar]


