Abstract
Introduction
Prevalence of planned pregnancies varies between countries but is often measured in a dichotomous manner. The aim of this study was to investigate to what level pregnant women had planned their pregnancies and whether pregnancy planning was associated with background characteristics and pregnancy‐planning behavior.
Material and methods
A cross‐sectional study that utilized the baseline measurements from the Swedish Pregnancy Planning study. Pregnant women (n = 3390) recruited at antenatal clinics answered a questionnaire. Data were analyzed with multinomial logistic regression, Kruskal–Wallis H and chi‐squared tests.
Results
Three of four pregnancies were very or fairly planned and 12% fairly or very unplanned. Of women with very unplanned pregnancies, 32% had considered an induced abortion. Women with planned pregnancies were more likely to have a higher level of education, higher household income, to be currently working (≥50%) and to have longer relationships than women with unplanned pregnancies. The level of pregnancy planning was associated with planning behavior, such as information‐seeking and intake of folic acid, but without a reduction in alcohol consumption. One‐third of all women took folic acid 1 month prior to conception, 17% used tobacco daily and 11% used alcohol weekly 3 months before conception.
Conclusions
A majority rated their pregnancy as very or fairly planned, with socio‐economic factors as explanatory variables. The level of pregnancy planning should be queried routinely to enable individualized counseling, especially for women with unplanned pregnancies. Preconception recommendations need to be established and communicated to the public to increase health promoting planning behavior.
Keywords: Planned pregnancy, unplanned pregnancy, preconception care, folic acid, health behavior
Key Message.
Women in Sweden are quite structured when it comes to planning a pregnancy. Three things can be improved prior to conception: intake of folic acid, smoking cessation and reducing alcohol consumption.
Introduction
Health and lifestyle are of great importance when women intend to get pregnant, as well as during pregnancy, as their health and lifestyles affect pregnancy outcome. Women who intend to get pregnant are advised to use folic acid supplementation prior to conception and in the first 12 gestational weeks to reduce the risk of development of neural tube defects and possibly cleft lip and cleft palate in the fetus 1, 2, 3. Women are also advised to quit using tobacco and alcohol during the pregnancy 1, 4. In Sweden, as in many other high‐income countries, many women postpone childbearing until higher ages because of investment in education and employment, and also in response to social norms 5, 6, 7, 8, 9, 10. The negative consequences of this might be that some women will have problems conceiving. Age also affects pregnancy outcome adversely 11.
From a global perspective, unplanned pregnancies are common. In the USA the proportion of planned/intended pregnancies among live births has been estimated to be around 60% 12, 13, between 57 and 66% in the UK 14, 15 and 83% in France 16. Unplanned pregnancies have been linked to increased medical costs 17 and have also been associated with low birthweight, prematurity and with socially and developmentally disadvantaged children 15, 18, 19. Unplanned pregnancies are also associated with late initiation and inadequate use of antenatal care services 20.
Measuring pregnancy planning is not an easy task 21, 22. Terms related to pregnancy planning are used and understood inconsistently by researchers, health professionals and women in general. Unplanned pregnancies are pregnancies reported to have been either unwanted (i.e. they occurred when no children or no more children were desired) or mistimed (i.e. they occurred earlier than desired). Pregnancy planning is often measured as a dichotomous variable, such as were you planning to get pregnant or was it a surprise 15? This does not take into account that a pregnancy may be more or less planned. Studies measuring pregnancy planning among women attending antenatal clinics in Sweden and Denmark showed that three of four pregnancies were very or rather well‐planned 23, 24. However, if and how pregnancies are planned is not routinely captured in the antenatal records in Sweden, apart from questions on assisted reproduction. Consequently, there is a lack of knowledge on the proportion of planned/unplanned pregnancies among live births in Sweden.
A well‐planned pregnancy may be associated with a healthy lifestyle, as maternal health affects the offspring. To understand behavior related to pregnancy planning and to design effective family planning programs there is a need for better knowledge of how women plan their childbearing. The aim of this study was to investigate to what level women entering antenatal care had planned their pregnancies and whether pregnancy planning was associated with background characteristics and pregnancy‐planning behavior. Our hypothesis was that a high level of pregnancy planning would be associated with the following: older age, higher socio‐economic status, Swedish background, longer relationships, having at least one child, self‐reported somatic or psychiatric medical histories and pregnancy‐planning behavior.
Material and methods
This cross‐sectional study utilized the baseline measurements performed in the longitudinal Swedish Pregnancy Planning study. The Regional Ethical Review Board in Uppsala, Sweden, approved the study (reference number 2010/085). All antenatal clinics in nine Swedish counties (n = 196) were invited to participate by recruiting pregnant women at the time of their registration (usually around pregnancy week 10). Of the invited clinics, 144 (73%) clinics chose to participate, ranging from small to large, in the countryside and in the cities. To increase the coverage of non‐Swedish‐speaking women, 19 clinics in the capital region with a high proportion of foreign‐born women were also invited, of which nine clinics (47%) chose to participate. Recruitment took place during the period September 2012 through July 2013.
Women were recruited in consecutive order at registration in the antenatal clinic, after receiving written and oral information from the midwives. During the study period the midwife listed all registrations, the number of women approached, and their responses (accepted/declined).
Swedish‐speaking women who agreed to participate received a questionnaire to fill out at the clinic or at home and return by post in a prepaid envelope. The midwife registered a telephone number or an email address for participating women and a reminder was sent by text message or email to those who had not returned the questionnaire within 2 weeks. Return of the completed questionnaire was regarded as informed consent. Non‐Swedish‐speaking women were asked to provide written consent along with their full contact details and were asked to choose between receiving a translated questionnaire by post (in English or Arabic) or to be interviewed on the telephone (all other languages). Professional interpreters interviewed the women using a structured interview guide containing a selection of the 29 most relevant questions from the complete questionnaire. To those who had not returned the translated questionnaire, one reminder and a new copy of the questionnaire were sent by post. Several attempts were made to reach women who had chosen to participate through telephone interviews.
Of all women approached, 61% completed the study: 98% used the Swedish questionnaire, 1% used the translated questionnaires and 1% were interviewed. A flow chart of the study procedure is presented in Figure 1.
Figure 1.
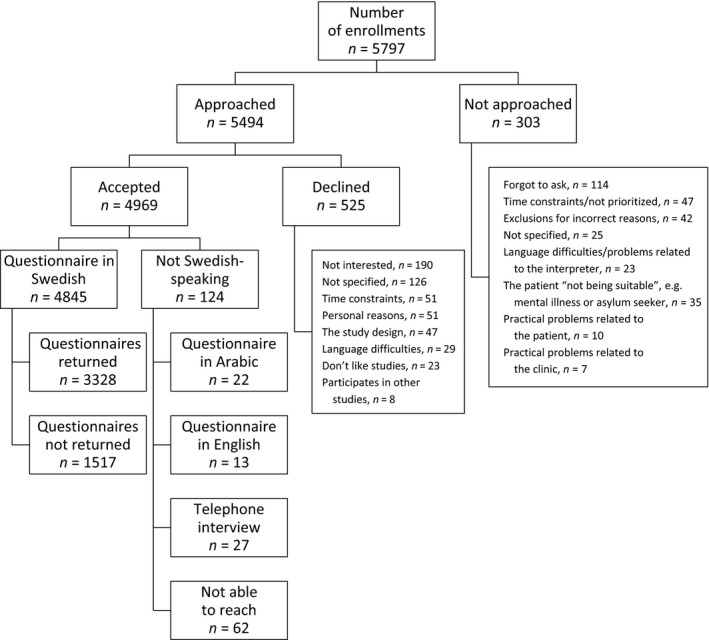
Flowchart of the study procedure.
The questionnaire consisted of 148 items, most of which were multiple‐choice questions. Researchers, clinicians and laypeople reviewed the questionnaire and a pilot study was conducted after which items were adjusted. The questionnaire covered the following themes: background characteristics, pregnancy planning in connection with the current pregnancy, physical and mental health, sexual and reproductive health, lifestyle and partner (if any). The overall non‐response for the individual items was 0.6–6%. In the following, we present items relevant to the aim of this study.
Questions about background characteristics covered the woman's age, partner's age, current relationship, length of current relationship, country of birth, parents' country of birth, level of education, occupation, gestational duration, and household income. Questions about medical history before pregnancy covered selected self‐reported somatic diagnose/disorders, such as: diabetes, epilepsy, hypertension, heart disease, polycystic ovary syndrome or endometriosis and any selected self‐reported psychiatric diagnosis/disorders, such as: attention deficit hyperactivity disorder, bipolar disorder, depression, anxiety and eating disorders. Questions about reproductive history covered previous pregnancies. No specific information regarding blood diseases was collected.
The level of pregnancy planning was measured using a single item, “How planned was your current pregnancy?” and a five‐step Likert scale with the response alternatives: very planned; fairly planned; neither planned nor unplanned; fairly unplanned; and very unplanned. This way of measuring the level of pregnancy planning has been used previously in Sweden and Denmark 23, 24. Questions also covered who took the initiative for the pregnancy, time frame of becoming pregnant and consideration of induced abortion.
Questions regarding pregnancy‐planning behavior included: intake of folic acid and/or multivitamin supplement 1 month prior to conception, weekly alcohol consumption and/or daily tobacco use during the 3 months prior to conception, average weekly frequency of vaginal intercourse during the 3 months prior to conception. Questions also included: information seeking, use of ovulation tests, and use of assisted reproductive technology treatment prior to pregnancy.
Statistical analysis
Data regarding household income, duration of gestation, length of relationship and frequency of vaginal intercourse were collected on an ordinal scale and are presented as median. However, as household income and length of relationship included as many as nine discrete or continuous categories, they were analyzed as continuous variables. A multinomial logistic regression was used to analyze the effect of background variables (independent variables) on the level of pregnancy planning (dependent variable). To increase the legibility and utility of the results, the level of pregnancy planning was categorized as planned (very or fairly planned), neither planned nor unplanned, or unplanned (fairly or very unplanned). Background characteristics for the three categories of pregnancy planning were compared at univariate and multivariate level using unplanned pregnancies as the reference category. The variable relationship status was excluded from the analysis, as the group of single women was too small. Results are reported as odds ratios (OR) with 95% confidence intervals (CI). Cox and Snell pseudo‐R 2 and Nagelkerke pseudo‐R 2 are presented as measures of the proportion of variation of outcomes explained by the model.
Differences between the five levels of pregnancy planning regarding pregnancy‐planning behavior in connection with the current pregnancy were analyzed using Kruskal–Wallis H tests for ordinal variables and Pearson's chi‐squared test for categorical variables. For all statistical analyses, a two‐sided p‐value <0.05 was considered significant. Data were entered and analyzed using IBM SPSS Statistics version 20 (IBM Corp., Armonk, NY, USA).
Results
Background characteristics of the women and the level of pregnancy planning are presented in Table 1. A very or fairly planned pregnancy was reported by 74% of the women, a pregnancy that was neither planned nor unplanned by 14%, and a fairly or very unplanned pregnancy by 12%.
Table 1.
Background characteristics of 3390 women included in the study
| Characteristic | Frequency (%) | Mean (SD) |
|---|---|---|
| Age (years) | 29.5 (5.1) | |
| Partner's age (years) | 32.6 (6.1) | |
| In a current relationship | 3308 (98) | |
| Length of current relationship (years) | 6a | |
| Pregnancy planning | ||
| Very planned | 1557 (47) | |
| Fairly planned | 914 (27) | |
| Neither planned nor unplanned | 468 (14) | |
| Fairly unplanned | 146 (4) | |
| Very unplanned | 258 (8) | |
| Born outside Sweden | 446 (13) | |
| Parent (one or both) born outside Sweden | 761 (22) | |
| Level of education | ||
| High | 1570 (46) | |
| Middle | 1532 (45) | |
| Low | 229 (7) | |
| Occupation (currently working ≥50%) | 2425 (72) | |
| Gestational age (completed weeks) | 11a | |
| Previous pregnancy | 2328 (69) | |
| Previous childbirth | 1845 (54) | |
| Previous induced abortion | 749 (22) | |
| Previous miscarriage | 843 (25) | |
| Any somatic diagnosis | 158 (5) | |
| Any psychiatric diagnosis | 315 (9) | |
| Household income/month, ≥80 000 SEK | 121 (4) | |
| Household income/month, 40 000–79 999 SEK | 1610 (47) | |
| Household income/month, <39 999 SEK | 1524 (45) | |
SD, standard deviation; SEK, Swedish Krona.
Missing values (range 0.6–6%) are not presented.
Median.
Among women with very or fairly planned pregnancies, 80.4% (n = 1986) stated that she and her partner took the initiative to become pregnant together, 13.9% (n = 343) stated that she initiated the decision, and 2.4% (n = 60) stated that the partner initiated it (3.3% missing data). One of three (n = 739) women had set a time frame to get pregnant within 1 year, while 1.5% (n = 39) had a time frame longer than 1 year.
Furthermore, 5% of all participating women had considered having an induced abortion. This proportion differed across the levels of pregnancy planning (p < 0.001). Among women with very well‐planned pregnancies, less than 1% had thought about having an induced abortion compared with 32% of women with very unplanned pregnancies.
Associations between pregnancy planning and background characteristics
In univariate multinomial regression analyses, the woman's age, length of current relationship, country of birth, parents' country of birth, level of education, current working status, psychiatric diagnosis and household income were positively associated with the level of pregnancy planning when women with planned and unplanned pregnancies were compared (Table 2). Level of education and current working status showed the highest OR: 4.1 (95% CI 2.9–5.9) and 2.3 (95% CI 1.8–2.8), respectively. When women with neither planned nor unplanned pregnancies were compared with women with unplanned pregnancies, level of education and current working status showed positive associations with pregnancy planning, whereas a younger partner was associated with less planning.
Table 2.
Results for univariate and multivariate multinomial logistic regression models with pregnancy planning (in three categories) as the outcome, given as odds ratios (ORs) with 95% confidence intervals (CIs)
| Pregnancy planning category | Variables | Univariate regression | Multivariate regressionb | ||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | ||
| Very or fairly planneda | Age (years) | 1.027 | 1.006–1.048 | 0.013 | 0.985 | 0.956–1.015 | 0.350 |
| Partner's age (years) | 0.999 | 0.981–1.017 | 0.892 | 0.978 | 0.955–1.000 | 0.055 | |
| Length of relationship (years) | 1.156 | 1.111–1.203 | <0.001 | 1.123 | 1.072–1.176 | <0.001 | |
| Born in Sweden | 1.525 | 1.154–2.014 | 0.003 | 1.130 | 0.706–1.808 | 0.610 | |
| Both parents born in Sweden | 1.337 | 1.055–1.693 | 0.016 | 1.098 | 0.757–1.593 | 0.621 | |
| Level of education | |||||||
| High | 4.139 | 2.904–5.899 | <0.001 | 2.059 | 1.294–3.274 | 0.002 | |
| Middle | 2.139 | 1.522–3.006 | <0.001 | 1.430 | 0.943–2.169 | 0.092 | |
| Low | Ref. | Ref. | |||||
| Currently working ≥50% | 2.291 | 1.855–2.830 | <0.001 | 1.600 | 1.230–2.081 | <0.001 | |
| Previous childbirth | 1.212 | 0.984–1.489 | 0.066 | Not in model | |||
| No somatic diagnoses | 0.997 | 0.613–1.621 | 0.990 | Not in model | |||
| No psychiatric diagnoses | 1.914 | 1.407–2.603 | <0.001 | 1.367 | 0.955–1.957 | 0.088 | |
| Household income (SEK) | 1.315 | 1.241–1.394 | <0.001 | 1.134 | 1.055–1.220 | 0.001 | |
| Neither planned nor unplanneda | Age (years) | 0.990 | 0.965–1.017 | 0.475 | 0.983 | 0.947–1.020 | 0.367 |
| Partner's age (years) | 0.976 | 0.954–0.999 | 0.037 | 0.980 | 0.952–1.009 | 0.169 | |
| Length of relationship (years) | 1.030 | 0.980–1.083 | 0.251 | 1.051 | 0.993–1.114 | 0.087 | |
| Born in Sweden | 1.180 | 0.826–1.686 | 0.364 | 0.948 | 0.533–1.688 | 0.857 | |
| Parents born in Sweden | 1.076 | 0.797–1.453 | 0.632 | 1.017 | 0.643–1.609 | 0.941 | |
| Level of education | |||||||
| High | 1.852 | 1.163–2.950 | 0.009 | 1.598 | 0.886–2.883 | 0.119 | |
| Middle | 1.760 | 1.127–2.747 | 0.013 | 1.549 | 0.915–2.624 | 0.103 | |
| Low | Ref. | Ref. | |||||
| Currently working ≥50% | 1.518 | 1.158–1.990 | 0.002 | 1.519 | 1.094–2.109 | 0.013 | |
| Previous childbirth | 0.910 | 0.701–1.183 | 0.482 | Not in model | |||
| No somatic diagnoses | 0.942 | 0.509–1.740 | 0.847 | Not in model | |||
| No psychiatric diagnoses | 1.264 | 0.854–1.871 | 0.242 | 1.108 | 0.713–1.720 | 0.649 | |
| Household income (SEK) | 1.066 | 0.992–1.146 | 0.083 | 0.994 | 0.908–1.089 | 0.905 | |
SEK, Swedish Krona.
Reference category: fairly or very unplanned.
n = 3390, pseudo‐R 2 = 0.059 (Cox and Snell), 0.076 (Nagelkerke). Model χ2(20) = 184.209, p < 0.001.
In multivariate multinomial regression analysis, with all factors except previous childbirth and somatic diagnosis included, length of the current relationship, level of education, current working status and household income showed positive independent associations with pregnancy planning when women with planned and unplanned pregnancies were compared (Table 2). The chance of having a planned pregnancy increased by 10% (95% CI 1.1–1.2) for each additional year the current relationship had lasted. The highest level of education, currently working and highest household income level showed an OR of 2.0 (95% CI 1.3–3.3), 1.6 (95% CI 1.2–2.1) and 1.1 (95% CI 1.0–1.2), respectively. When women with neither planned nor unplanned pregnancies were compared with women with unplanned pregnancies, in the multivariate regression model, currently working was the only factor that was significantly positively or negatively associated with having neither a planned nor an unplanned pregnancy: OR 1.5 (95% CI 1.1–2.1). The Cox & Snell pseudo‐R 2 of the full model was 0.06.
Pregnancy‐planning behavior prior to the current pregnancy
Among all women, 64% sought some kind of information, and the most frequent sources of information were Internet forums (for example familjeliv.se; n = 1304), the Swedish national online health‐care portal (1177.se; n = 900) and antenatal clinics (n = 845). As shown in Table 3, 29% took folic acid, 17% smoked daily and 11% drank alcohol weekly. The pregnancy‐planning behavior increased with increasing levels of pregnancy planning, except for alcohol use and frequencies of vaginal intercourse.
Table 3.
Pregnancy planning behaviour according to level of pregnancy planning, given as frequencies and proportions, n (%), or median
| Planning behavior prior to pregnancy | Level of pregnancy planning | All women n = 3390 | |||||
|---|---|---|---|---|---|---|---|
| Very planned n = 1557 | Fairly planned n = 914 | Neither planned nor unplanned n = 468 | Fairly unplanned n = 146 | Very unplanned n = 258 | p‐valuea | ||
| Information‐seeking | 1068 (69) | 533 (58) | 255 (54) | 74 (51) | 143 (50) | <0.001 | 2170 (64) |
| Folic acid supplement intake ≥5 times/week | 670 (43) | 223 (24) | 67 (14) | 12 (8) | 19 (7) | <0.001 | 997 (29) |
| Use of ovulation testing | 551 (35) | 158 (17) | 37 (8) | 7 (5) | 3 (1) | <0.001 | 761 (22) |
| Received assisted reproductive technology | 155 (10) | 8 (<1) | 3 (<1) | 0 (0) | 1 (<1) | <0.001 | 168 (5) |
| Daily tobacco use | 165 (11) | 151 (17) | 119 (25) | 41 (28) | 97 (34) | <0.001 | 576 (17) |
| Weekly alcohol consumption | 173 (11) | 88 (10) | 40 (9) | 19 (13) | 40 (14) | n.s. | 363 (11) |
| Frequency of vaginal intercourse per weekb | 2 | 2 | 2 | 2 | 2 | n.s. | 2 |
n.s., not significant.
Differences across levels of pregnancy planning analyzed with chi‐squared test or Kruskal–Wallis H test.
Median.
Discussion
Our main finding was that as many as three of four women considered their pregnancy to be very well or fairly well‐planned, with the decision to become pregnant being initiated jointly by four of five couples. Not surprisingly, these women represented the highest proportion of those undertaking pregnancy‐planning behavior prior to conception, including the highest proportion of folic acid intake. Women with planned pregnancies were more likely to have higher socio‐economic status than women with unplanned pregnancies, although the statistical explanation of the total variation was weak. Also, when the pregnancy was very unplanned, 32% of the women had considered an abortion compared with 1% when the pregnancy was very planned. Ambivalence in the beginning of pregnancy could result in difficulties in adapting to the situation with consequences, for example the use of alcohol and tobacco. If this is known, more support could be offered by the staff.
This was the first large‐scale Swedish study to focus on the level of pregnancy planning among women attending antenatal care. The study population was recruited from both rural and urban antenatal clinics, and group characteristics suggest that the study population was representative of pregnant Swedish women. This is also illustrated by the proportion of women having received assisted reproductive technology being similar to that reported in the national data and similar to the proportion of women known to be daily smokers prior to pregnancy 25. However, there was one exception concerning women born outside Sweden. A great effort was made to enhance recruiting immigrant women, but only 13% of the study population was of non‐Swedish origin compared with the 24% of all women giving birth in Sweden 25.
This study used a retrospective measure of pregnancy planning. It is possible that the participating women might have estimated their pregnancy planning differently, had they been asked before the current pregnancy. Furthermore, in Sweden only around 6% of the induced abortions are performed after the 12th week 26 and thus women who terminate their pregnancy are seldom enrolled at antenatal clinics. It could have been possible that a few of the participating women chose to terminate the present pregnancy for some reason, but we lack information on this.
The high proportion of planned pregnancies is consistent with two previous studies from Sweden and Denmark, where 72–75% of the pregnancies were reported as being highly or quite planned 23, 24. Our results contrast to previous studies in the USA 12, 13 and UK 14, 15. Comparisons should, however, take into account that different measures of pregnancy planning were used and also that differences exist in the availability and social acceptability of induced abortions. In Sweden, bad timing has been found to be one of the most cited reasons contributing to the decision to have an abortion 27, 28. Sweden has the highest number of abortions in the Nordic countries; 20.9 of 1000 women in fertile age (15–49 years), about 38 000 annual induced abortions compared with 110 000 births 25, 26, which can partly explain the high number of well‐planned pregnancies among women attending antenatal care.
Our finding that planned pregnancies were associated with higher socio‐economic status is consistent with findings from Scandinavia, Spain and the USA 24, 29, 30. That immigrant background had an effect on the level of pregnancy planning in the univariate, but not the multivariate, models might be explained by low socio‐economic status among these women 31.
The results of the present study suggest that pregnancy planning should be investigated routinely to improve individualized care to women. This is supported by the fact that almost one‐third of women with unplanned pregnancies had considered an induced abortion and might benefit from extra support. The five‐graded Likert scale, to measure the level of pregnancy planning used in this study, is easy to implement both in patient records and national registries to obtain reliable data. This would enable further studies on health outcomes for the mother and the child according to pregnancy planning status. As many women, even those with planned pregnancies, frequently used both tobacco and alcohol and did not take folic acid prior to pregnancy, we believe that information regarding the effect of lifestyle on fertility and pregnancy needs to be improved. Health professionals have a key role in promoting preconception health and establishing national preconception recommendations would facilitate health‐promoting behavior for women who plan to become pregnant.
Conclusions
A majority of the participating women rated their pregnancy as very or fairly planned, with socio‐economic factors as explanatory variables. The level of pregnancy planning should be questioned routinely at registration in antenatal clinics to enable individualized counseling and support for those women in need of extra care. National preconception recommendations need to be established and the education of the public reinforced to increase folic acid intake, quit smoking and stop alcohol consumption during the pregnancy‐planning period.
Funding
The study was funded by grants received from the Family Planning Fund of Uppsala, the Uppsala County Council, the Faculty of Medicine, Uppsala University and the Uppsala‐Örebro Regional Research Council, Sweden.
Stern J, Salih Joelsson L, Tydén T, Berglund A, Ekstrand M, Hegaard H, et al. Is pregnancy planning associated with background characteristics and pregnancy‐planning behavior?. Acta Obstet Gynecol Scand 2016; 95:182–189.
Conflict of interest
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
References
- 1. National Food Agency, Sweden . Råd om folsyra för kvinnor [Advice about folic acid for women] (in Swedish). Available online at: www.livsmedelsverket.se/matvanor-halsa-miljo/kostrad-och-matvanor/folsyra-for-kvinnor: Livsmedelsverket; 2015 (accessed 6 April, 2015).
- 2. Prevention of neural tube defects: results of the Medical Research Council Vitamin Study. MRC Vitamin Study Research Group. Lancet. 1991;338:131–7. [PubMed] [Google Scholar]
- 3. Bezerra JF, Oliveira GH, Soares CD, Cardoso ML, Ururahy MA, Neto FP, et al. Genetic and non‐genetic factors that increase the risk of non‐syndromic cleft lip and/or palate development. Oral Dis. 2015;21:393–9. [DOI] [PubMed] [Google Scholar]
- 4. Healthcare Guide 1177 . Tobak och graviditet [Tobacco and pregnancy] (in Swedish). Available online at: www.1177.se/Uppsala-lan/Tema/Gravid/Graviditeten/Halsa-under-graviditeten/Tobak-och-graviditet/1177. Vårdguiden, 2015 (accessed August 26, 2015).
- 5. Skoog Svanberg A, Lampic C, Karlstrom PO, Tyden T. Attitudes toward parenthood and awareness of fertility among postgraduate students in Sweden. Gend Med. 2006;3:187–95. [DOI] [PubMed] [Google Scholar]
- 6. Tyden T, Svanberg AS, Karlstrom PO, Lihoff L, Lampic C. Female university students' attitudes to future motherhood and their understanding about fertility. Eur J Contracept Reprod Health Care. 2006;11:181–9. [DOI] [PubMed] [Google Scholar]
- 7. Cooke A, Mills TA, Lavender T. Advanced maternal age: delayed childbearing is rarely a conscious choice; a qualitative study of women's views and experiences. Int J Nurs Stud. 2012;49:30–9. [DOI] [PubMed] [Google Scholar]
- 8. Virtala A, Vilska S, Huttunen T, Kunttu K. Childbearing, the desire to have children, and awareness about the impact of age on female fertility among Finnish university students. Eur J Contracept Reprod Health Care. 2011;16:108–15. [DOI] [PubMed] [Google Scholar]
- 9. Eriksson C, Larsson M, Skoog Svanberg A, Tyden T. Reflections on fertility and postponed parenthood‐interviews with highly educated women and men without children in Sweden. Ups J Med Sci. 2013;118:122–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bewley S, Davies M, Braude P. Which career first? BMJ. 2005;331:588–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Waldenström U, Aasheim V, Nilsen AB, Rasmussen S, Pettersson HJ, Schytt E. Adverse pregnancy outcomes related to advanced maternal age compared with smoking and being overweight. Obstet Gynecol. 2014;123:104–12. [DOI] [PubMed] [Google Scholar]
- 12. Guzman L, Wildsmith E, Manlove J, Franzetta K. Unintended births: patterns by race and ethnicity and relationship type. Perspect Sex Reprod Health. 2010;42:176–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mosher WD, Jones J, Abma JC. Intended and Unintended Births in the United States: 1982–2010. National Health Statistics Report, 2012; 55; 24 July 2012. [PubMed]
- 14. Wellings K, Jones KG, Mercer CH, Tanton C, Clifton S, Datta J, et al. The prevalence of unplanned pregnancy and associated factors in Britain: findings from the third National Survey of Sexual Attitudes and Lifestyles (Natsal‐3). Lancet. 2013;382:1807–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Flower A, Shawe J, Stephenson J, Doyle P. Pregnancy planning, smoking behavior during pregnancy, and neonatal outcome: UK Millennium Cohort Study. BMC Pregnancy Childbirth. 2013;13:238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Régnier‐Loilier A, Leridon H. Four decades of legalized contraception in France: an unfinished revolution? Popul Soc. 2007;439:1–4. [Google Scholar]
- 17. Trussell J. The cost of unintended pregnancy in the United States. Contraception. 2007;75:168–70. [DOI] [PubMed] [Google Scholar]
- 18. Baydar N. Consequences for children of their birth planning status. Fam Plann Perspect. 1995;27:228–34, 45. [PubMed] [Google Scholar]
- 19. Carson C, Redshaw M, Sacker A, Kelly Y, Kurinczuk JJ, Quigley MA. Effects of pregnancy planning, fertility, and assisted reproductive treatment on child behavioral problems at 5 and 7 years: evidence from the Millennium Cohort Study. Fertil Steril. 2013;99:456–63. [DOI] [PubMed] [Google Scholar]
- 20. Dibaba Y, Fantahun M, Hindin MJ. The effects of pregnancy intention on the use of antenatal care services: systematic review and meta‐analysis. Reprod Health. 2013;10:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Peterson R, Moos M. Defining and measuring unintended pregnancy: issues and concerns. Womens Health Issues. 1997;7:234–40. [DOI] [PubMed] [Google Scholar]
- 22. Morin P, Payette H, Moos MK, St‐Cyr‐Tribble D, Niyonsenga T, De Wals P. Measuring the intensity of pregnancy planning effort. Paediatr Perinat Epidemiol. 2003;17:97–105. [DOI] [PubMed] [Google Scholar]
- 23. Tyden T, Stern J, Nydahl M, Berglund A, Larsson M, Rosenblad A, et al. Pregnancy planning in Sweden – a pilot study among 270 women attending antenatal clinics. Acta Obstet Gynecol Scand. 2011;90:408–12. [DOI] [PubMed] [Google Scholar]
- 24. Backhausen MG, Ekstrand M, Tyden T, Magnussen BK, Shawe J, Stern J, et al. Pregnancy planning and lifestyle prior to conception and during early pregnancy among Danish women. Eur J Contracept Reprod Health Care. 2014;19:57–65. [DOI] [PubMed] [Google Scholar]
- 25. Gottvall K, Lundqvist E, Källén K. Pregnancies, deliveries and newborn infants. The Swedish Medical Birth Register 1973–2013, Assisted Reproduction treatment 1991–2012. The National Board of Health and Welfare, 2014. pp. 1–159. Available online at: www.socialstyrelsen.se. (accessed September 3, 2015). [Google Scholar]
- 26. Gottvall K, Lundqvist E, Källén K. Induced abortions 2011. Available online at: www.socialstyrelsen.se. The National Board of Health and Welfare, 2012. pp. 1‐56. Available online at: www.socialstyrelsen.se. (accessed September 3, 2015). [Google Scholar]
- 27. Larsson M, Aneblom G, Odlind V, Tyden T. Reasons for pregnancy termination, contraceptive habits and contraceptive failure among Swedish women requesting an early pregnancy termination. Acta Obstet Gynecol Scand. 2002;81:64–71. [DOI] [PubMed] [Google Scholar]
- 28. Makenzius M, Tyden T, Darj E, Larsson M. Repeat induced abortion – a matter of individual behavior or societal factors? A cross‐sectional study among Swedish women. Eur J Contracept Reprod Health Care. 2011;16:369–77. [DOI] [PubMed] [Google Scholar]
- 29. Font‐Ribera L, Perez G, Salvador J, Borrell C. Socioeconomic inequalities in unintended pregnancy and abortion decision. J Urban Health. 2008;85:125–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Finer LB, Zolna MR. Shifts in intended and unintended pregnancies in the United States, 2001–2008. Am J Public Health. 2014;104(Suppl. 1):S43–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hjern A. Migration and public health: health in Sweden. The National Public Health Report 2012. Chapter 13. Scand J Public Health. 2012;40(9 Suppl.):255–67. [DOI] [PubMed] [Google Scholar]


