Abstract
Objectives
The built food environment surrounding people's homes may influence their dietary intake. This exploratory study examined how the density of different sources of food in the residential environment was associated with dietary consumption among 77 African-American adults in Houston, Texas.
Methods
The number of fast-food-type restaurants, large grocery stores, and convenience-type stores within 2- and 5-mile residential buffers were divided by the respective areas to obtain food environment density variables. Intake of fruit and vegetables [FV], fiber [FI], and percent energy from fat [PEF] was assessed using National Health Interview Survey items. Covariate-adjusted regressions were used to assess relations of interest.
Results
Greater density of fast-food-type restaurants within 2 miles was associated with greater FV, FI, and PEF (ps ≤ .012); and for FV and FI within 5 miles (ps < .004). Density of large grocery stores was unrelated to intake. Greater density of convenience-type stores within 2 miles was negatively associated with FV and FI (ps ≤ .03); results became marginal at 5 miles for FV (p = .10) but not FI (p = .03).
Conclusion
Maximizing healthy offerings in venue-rich metropolitan areas might provide direction for policies to reduce obesity.
Keywords: diet, African Americans, fast food, grocery stores, convenience stores, obesity
The built food environment around people's homes may affect their dietary intake via enhanced food access, exposure, and availability.1 For example, greater access and exposure to large grocery stores or healthy food vendors might lead to healthier diets that include more fruit and vegetable and fiber intake, whereas greater access and exposure to fast-food-type restaurants and convenience-type stores that sell primarily calorie-dense foods might result in less healthy diets comprising higher fat intake. Results of previous studies in this area, however, have been mixed. For example, some studies have reported healthier diets among residents in communities with proximal large grocery stores,2 as well as less healthy dietary intake among residents in communities with a greater presence of convenience stores.3,4 Other research, however, suggests no relationship between proximal large grocery stores and fruit and vegetable consumption.5,6 Moreover, one study reported that the opening of a large grocery store in a community area previously bereft of such access noted no subsequent change in fruits and vegetable consumption among surveyed residents.7 Similar results have been reported elsewhere.8
The associations between the built food environment and dietary intake are complex, with factors such as food prices, shopping frequency, product advertising, and perceptions of the consumer environment playing a role in shopping and consumption behaviors.9-16 The mixed results found in the built food environment literature also may be at least partially attributable to a failure to examine multiple food vendor types and multiple aspects of dietary intake within the same sample. This seems particularly important to improved understanding of these potentially complex associations, as healthy and unhealthy food sources may spatially co-occur (ie, fast food restaurants may be located around supermarkets).17 In addition, the distribution of healthy and unhealthy food sources in the built environment may vary by the racial/ethnic characteristics of the area in question,18 with potentially unfavorable results for areas with predominately African-American residents regarding both access19 and exposure to outdoor obesity-related advertising.20 However, the nature and strength of these associations also may vary based on where the study was conducted (eg, rural vs metropolitan area, southern vs northern United States),13,21,22 suggesting the need for local studies to inform local policies/interventions involving the built food environment. Also, the data source used to characterize the built food environment may contribute to contradictory findings, with accuracy problems (eg, under-counting some vendor types and over-counting others, incorrect characterization of vendors, location inaccuracies) arising when relying upon large commercial databases for the characterization of a local food environment.23-25 Because field validation via ground-truthing can be cost prohibitive, alternative local data sources such as city food inspection records may offer a more location-accurate and comprehensive view of food sources, including vendors potentially not captured in large databases (eg, dollar stores selling food items).26 Although no data source is without some weakness,27 the use of food inspection records may result in potentially greater validity for restaurants and more similar sensitivities across food vendor types relative to the use of commercial databases.25
The purpose of the current study was to explore the relationships among the density of fast-food-type restaurants, large grocery stores, and convenience-type stores and dietary intake of fruits and vegetables, fiber, and fat in a sample of African-American adults in the city of Houston, Texas. Study strengths included the use of rich food inspection records to characterize multiple aspects of the built food environment, the assessment of multiple dietary components, and a focus on an ethnic subgroup at risk of obesity-related health disparities.28,29 Better understanding of these associations within Texas is important given that it is among the states with the highest rates of obesity among non-Hispanic African-American adults (38.2% [CI: 35.4, 41.1]).29 Moreover, data characterizing the proportion of healthy versus unhealthy food vendors indicated that census tracts in metropolitan areas were among the least favorable in the state,30 suggesting the relevance of examining these associations in the city of Houston, one of the largest metropolitan areas in the state and the fifth largest in the United States.31 This study extends previous research linking the density of fast food restaurants with higher body mass among low-income African-American adults32 by examining associations among fast-food-type restaurants, as well as other aspects of the larger food environment, and the presumed underlying causal mechanism of dietary intake.
METHODS
Participants and Procedures
Participants were adults recruited from a large African-American church of over 17,000 members in Houston, Texas. This site was selected based on a successful multi-year partnership with church leadership and parishioners within which several previous studies have been conducted.32-38 Individuals who participated in our previous studies and who consented to be contacted for future studies were sent a flyer about the present data collection via email. The email announcement indicated we were engaging in limited recruitment for a new study focused broadly on stress and health behaviors among African-American adults. Study participation was not limited to the email recipients or to church attendees, and the solicitation could be forwarded to friends and colleagues per directions on the flyer.
Interested individuals called a devoted study line where they were provided more information about the study and screened for eligibility. Individuals were eligible to participate if they were: (1) ≥18 years old; (2) self-reported African-American ethnicity; (3) able to provide valid contact information; and (4) willing to comply with the study protocol, which included 2 in-person visits to the church for survey completion. Only the first of these visits was relevant to the current study.
This study was limited to 124 participants, and individuals were screened, scheduled, and enrolled into the study in the order within which they contacted the study team. Data collection occurred on site at the church and spanned December 2013 to February 2014. Participants could be compensated up to $100 in department store gift cards for the completion of all study procedures.
Measures
Participant characteristics
Participant characteristics included sociodemographic data: age, sex, partner status (single/widowed/divorced vs married/living with partner), total annual household income (asked in increments and dichotomized as closely as possible to similar research: ≤$42,000/year vs >$42,000/year),32 educational level (<Bachelor's degree vs ≥Bachelor's degree), employment status (employed full time vs part-time employed, disabled, homemaker, student, retired), and car ownership or leases (none vs ≥1 car). In addition, participant BMI (kg/m2) was calculated using staff-administered height and weight measurements and was used to describe the sample.
Dietary intake variables
Estimated intake of (fresh, frozen, canned, or dried) fruit and vegetables [FV] excluding fried potatoes, fiber [FI], and percent energy from fat [PEF] was assessed by self-report using National Health Interview Survey-2000 Diet items.39 Dietary intake data were scored using conventional procedures and variance-adjusted per recommendations in the literature.40
Participant residential locations
Participants provided their residential mailing address, which was geocoded so that food environment density variables could be calculated. Specifically, an address locator was built using the ArcGIS software version 10.2 (ESRI, Redlands, CA) with data from the 2013 Southeast Texas Addressing and Referencing Map. Overall, 121 (97.6%) participants were successfully geocoded.
Food environment locations
The names and addresses of establishments selling food products were obtained from the 2013 city of Houston food inspection data, which includes all food establishments within the >600 square miles of the city. These data were already arranged by gross categories (eg, full-service restaurant, single-service restaurant, cafeterias). Study investigators used knowledge of the local area food chains coupled with North American Industry Classification System defining classifications to refine this list further into the following categories: (1) fast-food-type restaurants (traditional fast food restaurants like McDonalds and Kentucky Fried Chicken, pizzerias, limited-service facilities like Subway and Jimmy John's, and bakeries); (2) large grocery stores; and (3) convenience-type stores (convenience stores and small, mom-and-pop grocery stores with limited selection). Resulting food environment data (N = 14,101) were integrated into a geodatabase for density calculation as described below.
Food environment density variables
Two density variables were created for each of the 3 aforementioned food environment groupings, for each participant, using the Service Area tool in ArcGIS Network Analyst. Density variables were based on road/street network distances of 2 and 5 miles around the geocoded residential address. These buffers were chosen based on consistency with previous research,41 data characteristics (high prevalence of 0 counts with smaller buffers), area characteristics (Houston is a large, sprawling urban area with little reliance on public transportation), and prevalence of car availability in the sample (over 90% of the sample owned/leased cars). Density variables for each buffer were calculated by dividing the relevant food grouping counts by each buffer area.
Statistical Analysis
Although the parent study comprised 124 participants, data for the present study were limited to 80 participants (of the 121 participants whose residential address could be geocoded) based on their residence within the city of Houston, as our food environment data were relevant only to the city of Houston. Three participants were removed from the dataset due to edge effects (residence so close to the border of the city that food environment data would not be representative of access). Consequently, the current study used 63.6% (77/121) of all geocoded participant data, and 96.3% (77/80) of all geocoded data from city of Houston residents. Of the analyzable sample of 77 persons, 2 individuals skipped survey items related to fiber intake and percent energy from fat. These missing data were maintained in analyses involving those criterion variables.
Statistical analyses were performed using SPSS, version 19 (IBM, NY). Participant and food environment characteristics were examined with descriptive statistics. Main analyses consisted of linear regressions to examine the associations between each food environment density variable and each dietary intake variable. All models controlled for participants’ age, sex, partner status, income, educational level, employment status, and census tract of residence. Covariates were determined a priori based on the literature41 and limited in number due to the sample size. Although potentially relevant, car lease/ownership was not included as a covariate based on limited variability in this sample.15 All variables were entered in a single step for each regression analysis.
RESULTS
Participant Characteristics
Participants (N = 77; 79.2% women) had a mean age of 48.3 years (±11.3) and slightly less than one-third reported being married or living with a significant other. Almost half of participants (46.8%) reported an annual household income of ≤$42,000 year. The average BMI among participants was 31.5 (±7.5), and 58.1% were obese. Self-reported and variance-adjusted daily FV servings were 4.6 (±2.2), FI grams were 15.6 (±7.3), and PEF was 34.2 (±6.1). Table 1 shows these participant characteristics. Participants resided in 42 census tracts in the city of Houston, with a range of 1 to 4 participants per tract. The distance from their homes to the recruitment site (church) ranged from less than a mile to 63 miles. Participants in this sample lived a mean distance of 6.93 (±7.50) miles from the church.
Table 1.
Participant Characteristics (N = 77)
| M (SD) / N [%] | |
|---|---|
| Age | 48.25 (11.29) |
| Sex | |
| Men | 16 [20.8] |
| Women | 61 [79.2] |
| Partner Status | |
| Not partnered | 53 [68.8] |
| Partnered | 24 [31.2] |
| Annual Household Income | |
| ≤ $42,000 | 36 [46.8] |
| > $42,000 | 41 [53.2] |
| Education | |
| < Bachelor's degree | 42 [54.5] |
| ≥Bachelor's degree | 35 [45.5] |
| Employment Status | |
| Full-time | 43 [55.8] |
| All other | 34 [44.2] |
| Car Lease/Ownership | |
| 0 cars owned/leased | 7 [9.1] |
| ≥ 1 cars owned/leased | 70 [90.9] |
| Number Participants per Census Tract | 1.83 (1.01) |
| Body Mass Indexa | 31.50 (7.51) |
| Weight Statusa | |
| Normal (18.5-24.99 kg/m2) | 16 [21.6] |
| Overweight (25-29.99 kg/m2) | 15 [20.3] |
| Obese (≥30 kg/m2) | 43 [58.1] |
| Estimated Daily Dietary Intake | |
| Fruit & vegetable servings | 4.62 (2.17) |
| Fiber intake (grams)b | 15.55 (7.25) |
| Percent energy from fatb | 34.21 (6.09) |
Note.
N = 74 due to missing data
N = 75 due to missing data
Built Food Environment Characteristics
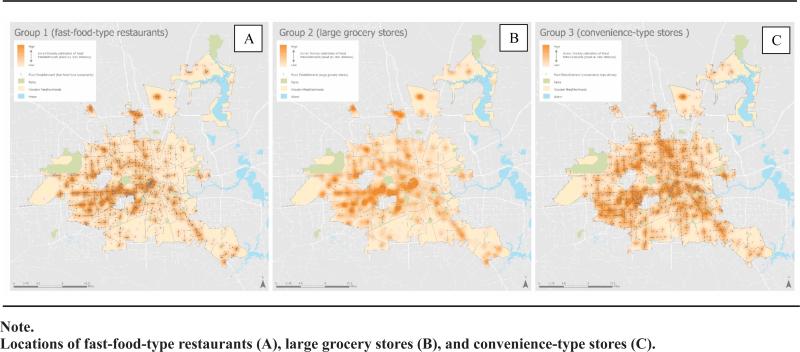
On average, there were 40.1 (±1.9) fast-food-type restaurants (range = 2 - 285), 3.7 (±2.9) large grocery stores (range = 0-10), and 7.9 (±7.2) convenience-type stores (range = 1-22) within 2 miles of participants’ homes. On average, there were 252 (±178.9) fast-food-type restaurants (range = 24-790), 20.7 (±11.9) large grocery stores (range = 2-42), and 23.6 (±12.6) convenience-type stores (range = 1 - 45) within 5 miles of participants’ homes. Figure 1 shows location data by food source grouping in the city of Houston.
Figure 1.
City of Houston and Food Environment Landscape Based on City of Houston Food Inspection Data, 2013
It is notable that food environment vendors were reduced when traditional fast food restaurants were examined separately from the fast-food-type restaurant grouping (which also included pizzerias, bakeries, etc). Specifically, there was an average of 14.2 (±11.5) traditional fast food restaurants within 2 miles and 90.8 (±52.3) traditional fast food restaurants within 5 miles of participants’ homes. These estimates are about 25% greater than the numbers of fast food restaurants reported by a previous study in Houston, Texas: 11.4 (±9.8) within 2, and 71.3 (±50.4) within 5 miles of participants’ homes.32 Elevated numbers might be expected in the present study given the use of a local and potentially more comprehensive food environment data source relative to the large commercial database used in the prior study. In contrast, average numbers of convenience stores (only) were virtually identical to estimates of convenience-type stores within both buffer zones.
Main Analyses
Greater density of fast-food-type restaurants within 2 miles was associated with greater FV, FI, and PEF (ps ≤ .012); results held for 5-mile density analyses for FV and FI only (ps ≤ .004). Density of large grocery stores was unrelated to intake outcomes. Greater density of convenience-type stores within 2 miles was negatively associated with FV and FI (ps ≤ .03); results became marginal at 5-mile buffers for FV (p = .10) but not FI (p = .03) as data in Table 2 show.
Table 2.
Adjusted Associations of the Built Food Environment and Dietary Intake
| Dietary Intake Outcomes of Interest |
|||||||
|---|---|---|---|---|---|---|---|
| Number of Stores/Restaurants | Fruit & Vegetable Intake | Fiber Intakea | Percent Energy from Fata | ||||
| M (SD) | β (SE) | p | β (SE) | p | β (SE) | p | |
| Within 2-mile Buffer | |||||||
| Fast-food-type restaurants | 40.12 (46.13) | .11 (.04) | 0.010 | .47 (.12) | <0.001 | .30 (.12) | 0.012 |
| Large grocery stores | 3.70 (2.93) | .21 (.61) | 0.726 | 1.02 (1.90) | 0.595 | 1.34 (1.69) | 0.431 |
| Convenience-type Stores | 7.86 (7.17) | −.56 (.22) | 0.014 | −1.53 (.71) | 0.034 | −.46 (.65) | 0.481 |
| Within 5-mile Buffer | |||||||
| Fast-food-type restaurants | 252.03 (178.89) | .28 (.08) | 0.001 | .76 (.25) | 0.004 | .11 (.24) | 0.658 |
| Large grocery stores | 20.66 (11.09) | 1.56 (1.25) | 0.218 | 1.54 (4.01) | 0.701 | −.18 (3.58) | 0.960 |
| Convenience-type stores | 23.55 (12.63) | −1.70 (1.01) | 0.099 | −7.11 (3.18) | 0.029 | .33 (2.95) | 0.911 |
Note:
Each aspect of the food environment within each buffer area was variance-adjusted prior to analysis and assessed in its own adjusted regression analysis. Covariates were: age, sex, income, education, employment, partner status and census tract. Results are presented without associated covariate information for conciseness.
FI and PEF have a reduced sample size due to N = 2 missing data
DISCUSSION
Results indicate that fast-food-type restaurant availability was associated with more FV consumption and FI (2- and 5-mile buffers), as well as more PEF (2-mile buffer only). It was somewhat unexpected that greater availability of fast food, pizzerias, limited-service facilities, and bakeries was associated with more desirable dietary characteristics like greater FV consumption and FI. Interestingly, a previous study in a large sample of African-American adults from central Mississippi also found this unexpected positive association between fast food restaurant availability and FI, though significant findings were limited to those younger than age 55.41 Also, in a previous study among African-American adults in Houston, the density of traditional fast food restaurants within 2, but not 5, miles was associated with higher body mass in the lower-income portion of the sample.32 Therefore, greater PEF associated with more fast-food-type restaurants within 2 miles of the home may suggest that greater FV and fiber consumption is embedded in the context of a less healthy, and potentially more fat-laden diet overall – an undesirable outcome. On the other hand, it may be that individuals are making healthier food choices at fast-food-type restaurants, which might be contributing to this positive association with FV and FI. That said, it is notable that the average FV consumption (4.6 servings) was slightly lower, and in the case of FI (15.6 grams) much lower, in this sample than prescribed by recommended daily intake guidelines (5 - 8 servings and 25 - 38 grams), whereas the proportion of calories from fat (34.2%) was at the top of the recommended guideline amount (20 - 35%).42 Consequently, despite positive relations between fast-food-type restaurants around the home and these criterion variables, consumption of desirable dietary components may not be reaching adequate levels. Results suggest the potential relevance of fast-food-type restaurants within 2 miles of the home in increased dietary fat consumption. Although more research is needed to support causality, results may have relevance for policies affecting the built food environment nutritional landscape that attempt to increase the convenience of healthy choices relative to less healthy choices via land use, taxation, and point-of-sale environmental changes.16,43,44
There were no associations between large grocery store density and dietary intake in the current study. These results appear to replicate findings of some previous studies suggesting a lack of association between large grocery stores and FV intake,5,6 and extend null findings to FI and PEF as well. Although it might be that the accessibility of a single grocery store is enough to affect dietary intake, rendering the density of large grocery stores relatively unimportant, post hoc analyses examining residential proximity to the closest store also yielded null results. In this sample, the majority of participants (83.1%) had access to at least one large grocery store within 2 miles, and all participants had 1 or more within 5 miles of their home, suggesting reasonable availability. However, the sheer number of fast-food-type restaurants and convenience-type stores relative to large grocery stores in Houston might overwhelm any potential for positive dietary influence of large grocery stores on dietary intake if mere exposure plays a role in consumption choices. Taken together with results from intervention studies suggesting that the addition of a large grocery store to a food desert does not alter the dietary intake of local residents,7,8 these results may suggest a similarly limited role for interventions involving large grocery stores in directly affecting dietary behaviors among African-American adults in Houston, Texas. However, a study in South Carolina suggested that grocery stores affected FV intake indirectly via shopping frequency and subjective perceptions of healthy food availability.12 Such indirect effects were not examined in this study, nor were customer store preferences, but provide direction for future work in this area. In addition, it is important to acknowledge that not all large grocery stores are equivalent in terms of healthful offerings or the proportion of healthy versus unhealthy products on shelves,45,46 which can affect consumer choices about purchases.47 Unfortunately, the proportion of FV to calorie-dense foods on store shelves may be lower in grocery stores located in African-American neighborhoods, relative to neighborhoods of other racial/ethnic composition.48 Consequently, future studies should consider not only the presence of large grocery stores but also individual store content, as well as pricing,15 when assessing effects on dietary intake.
In contrast to results involving fast-food-type restaurants, the density of convenience-type stores was associated with lower FV consumption (2-mile buffer) and FI (2- and 5-mile buffers). Limited-service, convenience-type stores are typically bereft of healthy foods relative to supermarkets, a discrepancy that is greater in African-American neighborhoods relative to white neighborhoods.49 The current findings supporting inverse relations between convenience-type store availability and intake of desirable dietary components may complement other studies supporting a link between convenience store availability and fast-food-type snacking behavior.3,50 In particular, an ecological momentary assessment study found that closer real-time proximity to convenience-type stores in daily travels was associated with higher snack food consumption among African-American women, an association that became stronger during times of higher stress.3 Although additional studies are needed to explicate causal pathways between convenience-type store density and dietary intake, the current results lend additional support to there being a link between this aspect of the built food environment and less desirable dietary constituents among African-American adults. Future studies that can examine the impact of limiting convenience store availability within 2 and 5 miles around residential neighborhoods on dietary intake are needed to support the potential relevance of zoning policies for obesogenic built environments. In addition, programs to incentivize convenience stores to sell healthy foods, similar to those used with larger grocery stores51,52 could be considered. However, it is important to acknowledge that the neighborhood represents only one source of exposure to the built food environment, perhaps particularly in a car-dependent city like Houston, and that exposures in the larger activity space also may affect dietary choices.53 Therefore, greater attention to a healthy food availability in urban workplaces (eg, downtown, in and around medical centers) and its effect on dietary intake is needed. Moreover, additional research on the potential positive effects of the residential built food environment on out-of-home food consumption choices is also important to inform policies.54
Limitations of the current study include its small sample size of primarily women, which inherently limits the generalizability of the findings. Future studies can use a similar strategy to replicate these results within a larger and potentially more representative sample (eg, greater proportion of men, greater socioeconomic variability). Although a high proportion of African-American adults, particularly African-American women, attend church,55 future studies should include individuals who do not attend church. Although the use of local food source data was a perceived strength of the current study, future work in this area might combine data sources for optimum accuracy.26,27 In addition, other factors affecting relations between the built food environment and dietary intake should be examined for their relative and potentially explanatory or moderating influence in future studies, including food prices, shopping frequency, and perceptions of the shopping environment.1,9-16 The self-reported estimates of dietary intake reported in this study may be over- or underinflated, although variance adjustment was employed to mitigate this issue in part. Future studies in this area might also minimize error from self-reported dietary data, as well as better understand how the environment translates into purchasing behaviors, by supplementing it with observational methods or the provision of food purchase receipts.56 In addition, the current study examined only large grocery stores as a potential source of healthy food and it is important to note that some healthy or relatively healthier vendors may have been missed (eg, food trucks) or potentially mischaracterized in the fast-food-type group (eg, Subway). Finally, like many studies in the area, the current work used a cross-sectional design and was unable to determine causality of effects, but benefited from a more comprehensive approach to characterizing the built food environment and its association with multiple aspects of dietary intake within a single sample. That said, it is important to acknowledge that this is an observational study from a convenience sample and results require replication in larger, more representative samples.
In summary, the current study indicated that the density of fast-food-type restaurants and convenience-type stores hold stronger links with dietary intake relative to large grocery stores among this sample of African-American adults living in an urban setting, and that the strongest effects were found within a 2-mile buffer of the home. Although causal study designs are needed, results may suggest that fast-food-type restaurant availability facilitate more FV and fiber consumption, whereas convenience-type stores availability may decrease it; however, FV consumption and FI were less than desirable in this sample and “eating more” FV and fiber is not necessarily “eating enough” to affect obesity,57 perhaps particularly when the percent energy from fat also was associated with fast-food-type restaurant availability. Future research in Houston and other metropolitan areas with similar built food environment characteristics might explore the extent to which healthy consumption choices can be made more convenient and easy, and unhealthy choices less desirable, so that these extant food venues better promote healthy eating by default, thereby reducing the prevalence of obesity and its associated health risks.1
Human Subjects Statement
Study procedures were approved by the Institutional Review Boards at the primary institution (University of Houston) and collaborating institution (University of Texas MD Anderson Cancer Center). Informed consent, which included the collection and use of residential address information to better understand contextual effects on health behaviors, was obtained from all participants prior to data collection. Participants were free to refuse to answer any questions and decline to participate in any procedures that they were uncomfortable with.
Acknowledgments
This project was supported by institutional funding from the University of Houston and the University of Texas MD Anderson Cancer Center (to LR Reitzel) and the National Cancer Institute at the National Institutes of Health through The University of Texas MD Anderson's Cancer Center Support Grant (CA016672). Recruitment was achieved with the assistance of Project CHURCH (Creating a Higher Understanding of cancer Research and Community Health) staff members who are supported in part by the Duncan Family Institute through the Center for Community-Engaged Translational Research. Manuscript authorship received further support from the National Institute on Drug Abuse at the National Institutes of Health through R01 DA034739 (to EM Obasi) and the University of Houston's Provost's Undergraduate Research Scholarship (to Hiroe Okamoto. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the project supporters.
The authors acknowledge the research staff members at the University of Houston who assisted with implementation of the project including Alison Shellman, Hannah LeBlanc, Sarah Childress, Hui-Ling “Michelle” Chang, Alexis Moisiuc, Daniel Kish, and Erin “Charli” Washington. We especially thank the church leadership (who approved the study and provided a devoted room for data collection) and the participants (whose contributions made this study possible). Finally, we thank Rachel Kimbro and Justin Denney of the Kinder Institute Urban Health Program at Rice University, as well as the students in attendance who provided feedback on this study via a Sociologists Talking about Population Health (STAPH) talk.
Footnotes
Conflict of Interest Statement
The authors have no competing interests pertaining to this research.
Contributor Information
Lorraine R. Reitzel, The University of Houston, Department of Psychological, Health, and Learning Sciences, Houston, TX..
Hiroe Okamoto, The University of Houston, Department of Psychological, Health, and Learning Sciences, Houston, TX..
Daphne C. Hernandez, The University of Houston, Department of Health and Human Performance, Houston, TX..
Seann D. Regan, All Points Consulting, Houston, TX..
Lorna H. McNeill, The University of Texas MD Anderson Cancer Center, Department of Health Disparities Research, Houston, TX..
Ezemenari M. Obasi, The University of Houston, Department of Psychological, Health, and Learning Sciences, Houston, TX..
References
- 1.Story M, Kaphingst KM, Robinson-O'Brien R, et al. Creating healthy food and eating environments: policy and environmental approaches. Annu Rev Public Health. 2008;29:253–272. doi: 10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- 2.Zenk SN, Lachance LL, Schulz AJ, et al. Neighborhood retail food environment and fruit and vegetable intake in a multiethnic urban population. Am J Health Promot. 2009;23(4):255–264. doi: 10.4278/ajhp.071204127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zenk SN, Horoi I, McDonald A, et al. Ecological momentary assessment of environmental and personal factors and snack food intake in African American women. Appetite. 2014;83:333–341. doi: 10.1016/j.appet.2014.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rummo PE, Meyer KA, Boone-Heinonen J, et al. Neighborhood availability of convenience stores and diet quality: findings from 20 years of follow-up in the coronary artery risk development in young adults study. Am J Public Health. 2015;105(5):e65–e73. doi: 10.2105/AJPH.2014.302435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boone-Heinonen J, Gordon-Larsen P, Kiefe CI, et al. Fast food restaurants and food stores: longitudinal associations with diet in young to middle-aged adults: the CARDIA study. Arch Intern Med. 2011;171(13):1162–1170. doi: 10.1001/archinternmed.2011.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fuller D, Cummins S, Matthews SA. Does transportation mode modify associations between distance to food store, fruit and vegetable consumption, and BMI in low-income neighborhoods? Am J Clin Nutr. 2013;97(1):167–172. doi: 10.3945/ajcn.112.036392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cummins S, Flint E, Matthews SA. New neighborhood grocery store increased awareness of food access but did not alter dietary habits or obesity. Health Aff. 2014;33(2):283–291. doi: 10.1377/hlthaff.2013.0512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Elbel B, Moran A, Dixon LB, et al. Assessment of a government-subsidized supermarket in a high-need area on household food availability and children's dietary in-takes. Public Health Nutr. 2015:1–10. doi: 10.1017/S1368980015000282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ghosh-Dastidar B, Cohen D, Hunter G, et al. Distance to store, food prices, and obesity in urban food deserts. Am J Prev Med. 2014;47(5):587–595. doi: 10.1016/j.amepre.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cannuscio CC, Hillier A, Karpyn A, et al. The social dy namics of healthy food shopping and store choice in an urban environment. Soc Sci Med. 2014;122:13–20. doi: 10.1016/j.socscimed.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 11.Dubowitz T, Zenk SN, Ghosh-Dastidar B, et al. Healthy food access for urban food desert residents: examination of the food environment, food purchasing practices, diet and BMI. Public Health Nutr. 2014:1–11. doi: 10.1017/S1368980014002742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liese AD, Bell BA, Barnes TL, et al. Environmental influences on fruit and vegetable intake: results from a path analytic model. Public Health Nutr. 2014;17(11):2595–2604. doi: 10.1017/S1368980013002930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gustafson A, Hankins S, Jilcott S. Measures of the consumer food store environment: a systematic review of the evidence 2000-2011. J Community Health. 2012;37(4):897–911. doi: 10.1007/s10900-011-9524-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blitstein JL, Snider J, Evans WD. Perceptions of the food shopping environment are associated with greater consumption of fruits and vegetables. Public Health Nutr. 2012;15(6):1124–1129. doi: 10.1017/S1368980012000523. [DOI] [PubMed] [Google Scholar]
- 15.Lear SA, Gasevic D, Schuurman N. Association of supermarket characteristics with the body mass index of their shoppers. Nutr J. 2013;12:117. doi: 10.1186/1475-2891-12-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meyer KA, Guilkey DK, Ng SW, et al. Sociodemographic differences in fast food price sensitivity. JAMA Intern Med. 2014;174(3):434–442. doi: 10.1001/jamainternmed.2013.13922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lamichhane AP, Warren J, Puett R, et al. Spatial patterning of supermarkets and fast food outlets with respect to neighborhood characteristics. Health Place. 2013;23:157–164. doi: 10.1016/j.healthplace.2013.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hilmers A, Hilmers DC, Dave J. Neighborhood disparities in access to healthy foods and their effects on environmental justice. Am J Public Health. 2012;102(9):1644–1654. doi: 10.2105/AJPH.2012.300865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.James P, Arcaya MC, Parker DM, et al. Do minority and poor neighborhoods have higher access to fast-food restaurants in the United States? Health Place. 2014;29:10–17. doi: 10.1016/j.healthplace.2014.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yancey AK, Cole BL, Brown R, et al. A cross-sectional prevalence study of ethnically targeted and general audience outdoor obesity-related advertising. Milbank Q. 2009;87(1):155–184. doi: 10.1111/j.1468-0009.2009.00551.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zenk SN, Schulz AJ, Lachance LL, et al. Multilevel correlates of satisfaction with neighborhood availability of fresh fruits and vegetables. Ann Behav Med. 2009;38(1):48–59. doi: 10.1007/s12160-009-9106-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morland K, Filomena S. The utilization of local food environments by urban seniors. Prev Med. 2008;47(3):289–293. doi: 10.1016/j.ypmed.2008.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ma X, Battersby SE, Bell BA, et al. Variation in low food access areas due to data source inaccuracies. Appl Geogr. 2013:45. doi: 10.1016/j.apgeog.2013.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liese AD, Barnes TL, Lamichhane AP, et al. Characterizing the food retail environment: impact of count, type, and geospatial error in 2 secondary data sources. J Nutr Educ Behav. 2013;45(5):435–442. doi: 10.1016/j.jneb.2013.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fleischhacker SE, Evenson KR, Sharkey J, et al. Validity of secondary retail food outlet data: a systematic review. Am J Prev Med. 2013;45(4):462–473. doi: 10.1016/j.amepre.2013.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liese AD, Colabianchi N, Lamichhane AP, et al. Validation of 3 food outlet databases: completeness and geo-spatial accuracy in rural and urban food environments. Am J Epidemiol. 2010;172(11):1324–1333. doi: 10.1093/aje/kwq292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fleischhacker SE, Rodriguez DA, Evenson KR, et al. Evidence for validity of five secondary data sources for enumerating retail food outlets in seven American Indian communities in North Carolina. Int J Behav Nutr Phys Act. 2012;9:137. doi: 10.1186/1479-5868-9-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention (CDC) [May 31, 2015];Obesity Prevalence Maps, BRFSS, 2011-2013. Available at: http://wwwcdcgov/obesity/data/prevalence-maps.html.
- 29.Centers for Disease Control and Prevention (CDC) [June 25, 2015];Early release of selected estimates based on data from the 2012 National Health Interview Survey. Available at: http://www.cdc.gov/nchs/nhis/released201306.htm.
- 30.Salinas JJ, Sexton K. A border versus non-border comparison of food environment, poverty, and ethnic composition in Texas urban settings. Front Public Health. 2015;3:63. doi: 10.3389/fpubh.2015.00063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. [June 26, 2015];ProximityOne. Metropolitan Areas: Assessing Competitive Position and Change. Available at: http://proximityone.com/metros2013.htm.
- 32.Reitzel LR, Regan SD, Nguyen N, et al. Density and proximity of fast food restaurants and body mass index among African Americans. Am J Public Health. 2014;104(1):110–116. doi: 10.2105/AJPH.2012.301140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fisher FD, Reitzel LR, Nguyen N, et al. Loneliness and self-rated health among church-attending African Americans. Am J Health Behav. 2014;38(4):481–491. doi: 10.5993/AJHB.38.4.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cuevas AG, Reitzel LR, Adams CE, et al. Discrimination, affect, and cancer risk factors among African Americans. Am J Health Behav. 2014;38(1):31–41. doi: 10.5993/AJHB.38.1.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hernandez DC, Reitzel LR, Wetter DW, et al. Social support and cardiovascular risk factors among black adults. Ethn Dis. 2014;24(4):444–450. [PMC free article] [PubMed] [Google Scholar]
- 36.Watkins KL, Reitzel LR, Wetter DW, et al. HPV awareness, knowledge and attitudes among older African-American women. Am J Health Behav. 2015;39(2):205–211. doi: 10.5993/AJHB.39.2.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Strong LL, Reitzel LR, Wetter DW, et al. Associations of perceived neighborhood physical and social environments with physical activity and television viewing in African-American men and women. Am J Health Promot. 2013;27(6):401–409. doi: 10.4278/ajhp.120306-QUAN-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Advani PS, Reitzel LR, Nguyen NT, et al. Financial strain and cancer risk behaviors among African Americans. Cancer Epidemiol Biomarkers Prev. 2014;23(6):967–975. doi: 10.1158/1055-9965.EPI-14-0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thompson FE, Subar AF, Smith AF, et al. Fruit and vegetable assessment: performance of 2 new short instruments and a food frequency questionnaire. J Am Diet Assoc. 2002;102(12):1764–1772. doi: 10.1016/s0002-8223(02)90379-2. [DOI] [PubMed] [Google Scholar]
- 40.Thompson FE, Midthune D, Subar AF, et al. Dietary in-take estimates in the National Health Interview Survey, 2000: methodology, results, and interpretation. J Am Diet Assoc. 2005;105(3):352–363. doi: 10.1016/j.jada.2004.12.032. [DOI] [PubMed] [Google Scholar]
- 41.Hickson DA, Diez Roux AV, Smith AE, et al. Associations of fast food restaurant availability with dietary intake and weight among African Americans in the Jackson Heart Study, 2000-2004. Am J Public Health. 2011;101(Suppl 1):S301–S309. doi: 10.2105/AJPH.2010.300006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Institute of Medicine (IOM). [June 2, 2015];Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. doi: 10.1016/s0002-8223(02)90346-9. Available at: https://www.iom.edu/Reports/2002/Dietary-Reference-Intakes-for-Energy-Carbohydrate-Fiber-Fat-Fatty-Acids-Cholesterol-Protein-and-Amino-Acids.aspx. [DOI] [PubMed]
- 43.Ashe M, Feldstein LM, Graff S, et al. Local venues for change: legal strategies for healthy environments. J Law Med Ethics. 2007;35(1):138–147. doi: 10.1111/j.1748-720X.2007.00118.x. [DOI] [PubMed] [Google Scholar]
- 44.Ashe M, Jernigan D, Kline R, et al. Land use planning and the control of alcohol, tobacco, firearms, and fast food restaurants. Am J Public Health. 2003;93(9):1404–1408. doi: 10.2105/ajph.93.9.1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Farley TA, Rice J, Bodor JN, et al. Measuring the food environment: shelf space of fruits, vegetables, and snack foods in stores. J Urban Health. 2009;86(5):672–682. doi: 10.1007/s11524-009-9390-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zenk SN, Powell LM, Isgor Z, et al. Prepared food availability in U.S. food stores: a national study. Am J Prev Med. 2015;49(4):553–562. doi: 10.1016/j.amepre.2015.02.025. [DOI] [PubMed] [Google Scholar]
- 47.Gustafson A, Christian JW, Lewis S, et al. Food venue choice, consumer food environment, but not food venue availability within daily travel patterns are associated with dietary intake among adults, Lexington Kentucky 2011. Nutr J. 2013;12:17. doi: 10.1186/1475-2891-12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bodor JN, Rice JC, Farley TA, et al. Disparities in food access: does aggregate availability of key foods from other stores offset the relative lack of supermarkets in African-American neighborhoods? Prev Med. 2010;51(1):63–67. doi: 10.1016/j.ypmed.2010.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zenk SN, Powell LM, Rimkus L, et al. Relative and absolute availability of healthier food and beverage alternatives across communities in the United States. Am J Public Health. 2014;104(11):2170–2178. doi: 10.2105/AJPH.2014.302113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zenk SN, Schulz AJ, Izumi BT, et al. Neighborhood food environment role in modifying psychosocial stress-diet relationships. Appetite. 2013;65:170–177. doi: 10.1016/j.appet.2013.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Giang T, Karpyn A, Laurison HB, et al. Closing the grocery gap in underserved communities: the creation of the Pennsylvania fresh food financing initiative. J Public Health Manag Pract. 2008;14(3):272–279. doi: 10.1097/01.PHH.0000316486.57512.bf. [DOI] [PubMed] [Google Scholar]
- 52.Karpyn A, Manon M, Treuhaft S, et al. Policy solutions to the ‘grocery gap'. Health Aff. 2010;29(3):473–480. doi: 10.1377/hlthaff.2009.0740. [DOI] [PubMed] [Google Scholar]
- 53.Zenk SN, Schulz AJ, Matthews SA, et al. Activity space environment and dietary and physical activity behaviors: a pilot study. Health Place. 2011;17(5):1150–1161. doi: 10.1016/j.healthplace.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Moore K, Diez Roux AV, Auchincloss A, et al. Home and work neighbourhood environments in relation to body mass index: the multi-ethnic study of atherosclerosis (MESA). J Epidemiol Community Health. 2013;67(10):846–853. doi: 10.1136/jech-2013-202682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pew Research Center [May 31, 2015];A religious portrait of African-Americans. Available at: http://www.pewforum.org/2009/01/30/a-religious-portrait-of-african-americans/.
- 56.Rahmanian E, Gasevic D, Vukmirovich I, et al. The association between the built environment and dietary intake - a systematic review. Asia Pac J Clin Nutr. 2014;23(2):183–196. doi: 10.6133/apjcn.2014.23.2.08. [DOI] [PubMed] [Google Scholar]
- 57.Liu S, Willett WC, Manson JE, et al. Relation between changes in intakes of dietary fiber and grain products and changes in weight and development of obesity among middle-aged women. Am J Clin Nutr. 2003;78(5):920–927. doi: 10.1093/ajcn/78.5.920. [DOI] [PubMed] [Google Scholar]