Abstract
♦ Background:
Accidental falls are common in the hemodialysis (HD) population. The high fall rate has been attributed to a combination of aging, kidney disease-related morbidity, and HD treatment-related hazards. We hypothesized that patients maintained on peritoneal dialysis (PD) would have fewer falls than those on chronic HD. The objective of this study was to compare the falls risk between cohorts of elderly patients maintained on HD and PD, using prospective data from a large academic dialysis facility.
♦ Methods:
Patients aged 65 years or over on chronic in-hospital HD and PD at the University Health Network were recruited. Patients were followed biweekly, and falls occurring within the first year recorded. Fall risk between the 2 groups was compared using both crude and adjusted Poisson lognormal random effects modeling.
♦ Results:
Out of 258 potential patients, 236 were recruited, assessed at baseline, and followed biweekly for falls. Of 74 PD patients, 40 (54%) experienced 86 falls while 76 out of 162 (47%) HD patients experienced a total of 305 falls (crude fall rate 1.25 vs 1.60 respectively, odds ratio [OR] falls in PD patients 0.78, 95% confidence interval [CI] 0.61 – 0.92, p = 0.04). After adjustment for differences in comorbidity, number of medications, and other demographic differences, PD patients were no less likely to experience accidental falls than HD patients (OR 1.63, 95% CI 0.88 – 3.04, p = 0.1).
♦ Conclusions:
We conclude that accidental falls are equally common in the PD population and the HD population. These data argue against post-HD hypotension as the sole contributor to the high fall risk in the dialysis population.
Keywords: Accidental falls, geriatric, hemodialysis, peritoneal dialysis
Canadian Organ Replacement Register data from 2012 indicate that more than half of the incident dialysis patient population in Canada are seniors, with a mean age at dialysis initiation of 65 and 62.1 years old for hemodialysis (HD) and peritoneal dialysis (PD), respectively (1). As a result, there is a growing interest in geriatric issues pertaining to nephrology and dialysis care.
Falls are a major problem in older patients. In 2004, falls were the leading cause of overall injury costs in Canada. In Canadians, seniors over the age of 65 accounted for 84% of deaths, 59% of hospitalizations, 53% of permanent partial disability, and 54% of permanent total disability from falls in 2004. This accounted for 46% of direct health care costs and 2.03 billion dollars for falls in 2004 (2,3).
There are numerous risk factors established for falls in elderly patients (4,5). Seniors on dialysis have risk factors associated with aging that are similar to community-dwelling elderly people (6–9). However, patients maintained on dialysis have additional risk factors attributable to the predisposing cause of end-stage renal disease, loss of kidney function, as well as the dialysis therapy itself (6,8–11). Predisposing causes of end-stage renal disease include diabetes, with its microvascular and macrovascular sequelae, peripheral vascular disease, and hypertension. Loss of kidney function is associated with anemia and malnutrition, depression, cognitive impairment, sleep disorders, and cardiovascular disease. Finally, HD therapy is associated with fluid and electrolyte shifts, hypotension, and arrhythmias (6,8–12). Given these additional risk factors, not surprisingly, data from the HD and PD population suggest a higher rate of falls than that typically seen amongst the general community-dwelling elderly population (1.2 – 1.8 vs 0.6 – 0.8 falls per patient-year respectively) (5,8–10,13–16).
Falls have been less frequently studied in the PD population, but data that are available suggest that the observed rate and consequences are similar to those seen in HD (12). However, patients on PD are often more independent, have lower comorbidity, and are not exposed to HD-specific fall risk factors, such as rapid fluid shifts. We therefore hypothesized that patients on PD would have fewer falls, after adjustment for comorbidity and age differences, than patients maintained on HD. The objective of this study was to compare the rate of falls between cohorts of elderly patients maintained on HD and PD therapy, using data collected prospectively from a large academic dialysis facility in Toronto, Canada.
Materials and Methods
The study protocol has previously been described in detail (8,12). Briefly, all end-stage renal disease patients 65 years and over undergoing chronic dialysis treatment during the period April 9, 2002, to April 9, 2003, at the University Health Network were approached to participate in the study. Peritoneal dialysis and HD patients were concurrently recruited and followed. Standardized comprehensive geriatric assessments were conducted by a research nurse at baseline (8,12). Medical history, medication history, dialysis history, and laboratory history were abstracted from the clinical and electronic chart records. Patients or caregivers were contacted, in person or by telephone, at biweekly intervals, and all falls were recorded prospectively using a standardized protocol. A fall was defined as an event which resulted in a person coming to rest inadvertently on the ground or other lower level (17).
Ethics approval was granted by the University Health Network Research Ethics Board.
Demographic data were summarized using mean and standard deviation or median and quartiles for continuous variables and percentages for categorical data. Data were censored at death, loss to follow up, and transplantation. Fall risk was compared between the HD and PD groups using a Poisson lognormal random effects model. As there was substantial disparity in the proportion of individuals with ≥ 12 comorbid conditions between the 2 samples, a second lognormal random effects model excluding patients with ≥ 12 comorbid conditions was used in a sensitivity analysis to limit error attributable to the effect of overdispersion.
Results
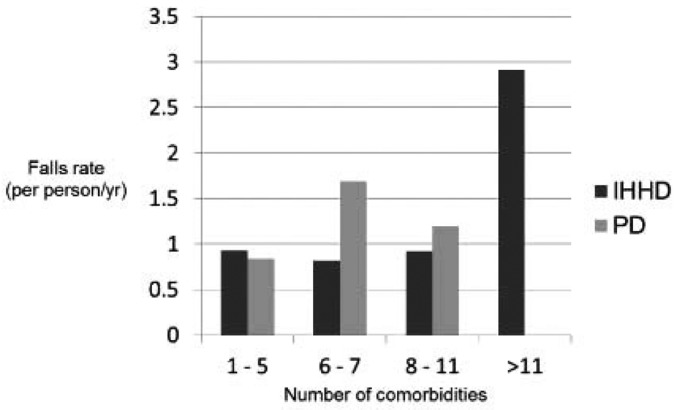
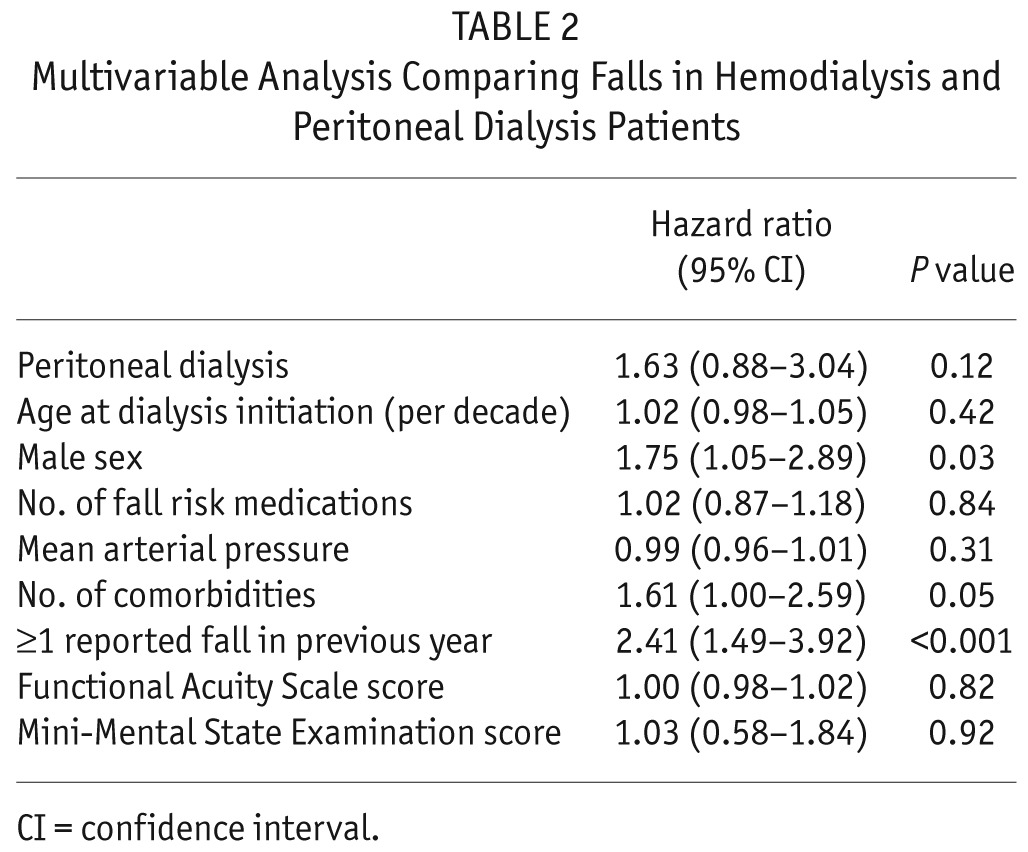
In total, 74 PD patients and 162 HD patients agreed to participate. The 2 populations were generally similar in baseline demographic characteristics and laboratory values (Table 1). The HD group were more likely to be diabetic, had a higher median number of comorbid conditions, and a slightly longer median dialysis vintage. Despite similar, or better observed measures of mobility, the PD group had a higher proportion of self-reported mobility dependence. Both groups were equally likely to have reported experiencing a fall in the previous year (42% in PD versus 47% in HD). Hemodialysis patients were followed for falls for a median of 468 days, while PD patients were followed for a median of 422 days. Over the fall observation period, a total of 87 falls occurred in 40 (54%) PD patients and 305 falls occurred in 76 (47%) HD patients (Figure 1). Factors predictive of falls, across both HD and PD modalities, included male sex and comorbidity (Table 2). In the PD group, those on continuous ambulatory PD were more likely to experience ≥ 1 fall than those on continuous cycler PD (61% versus 43%). In unadjusted analysis using a Poisson lognormal random effects model, patients on HD experienced a small non-statistically significant decrease in the risk of falls compared with patients on PD (RR 0.81, 95% confidence interval [CI] 0.48 – 1.39, p = 0.45). After adjustment for age at dialysis initiation, gender, comorbidity, medications associated with increased fall risk, mean arterial pressure, previous falls, visual acuity, and cognitive status, the HD group did not have a statistically significantly decreased risk of falls compared with the PD group (relative risk [RR] 0.61, 95% CI 0.33 – 1.13, p = 0.12) (Table 2). A sensitivity analysis, after exclusion of patients with ≥ 12 comorbid conditions (59 HD patients but no PD patients), did not significantly alter the direction or strength of the relative fall risk between the 2 groups (RR 0.57, 95% CI 0.31 – 1.06, p = 0.08).
TABLE 1.
Participant Demographics

Figure 1 —
Falls rate per person-year according to the number of comorbid conditions, for in-hospital hemodialysis (IHHD) and peritoneal dialysis (PD) patients.
TABLE 2.
Multivariable Analysis Comparing Falls in Hemodialysis and Peritoneal Dialysis Patients
Discussion
To our knowledge, this is the first study to simultaneously compare the risk of accidental falls amongst older patients on PD and HD. Our results build on our previous work showing high fall rates in patients undergoing chronic PD (12) by exploring whether this increased risk is specific to renal disease or modality-specific. In this paper we disprove our hypothesis that patients undergoing PD have lower fall rates than those maintained on HD. In contrast, we observed an equally high fall risk that suggests, if anything, that other factors are contributing to accidental falls in those maintained on PD.
We had hypothesized that PD patients may be less susceptible to falls due to the tendency for better blood pressure control and less dramatic fluid and electrolyte shifts (18–20). Therefore our finding of similar fall rates requires further study and explanation. The observation that PD patients on continuous ambulatory PD were more likely to fall than those on continuous cycler PD would seem to support the idea that those living a more active lifestyle experience an increased fall risk. However, in our study, the patients reported similar levels of functional dependence to that seen in the HD population (21). Furthermore, we have no clear explanation of the observation that patients maintained on PD reported requiring more help with ambulation than those maintained on HD, yet objectively had a better average gait speed. Current literature suggests that patients maintained on PD have lower illness intrusiveness scores (22), suggesting they may have higher expectations from their lives in terms of activity and lifestyle. If true, this may place them at higher risk of falls due to increased participation in day-to-day leisure activities inside and outside of the home. It is possible that there was a discordance between true ability and the confidence with which they walked that may impact the risk of falling; however, in our study, the fall efficacy scores between HD and PD patients were similar (data not shown). An alternate explanation is that PD therapy itself alters fall risk. To this effect, environmental factors, such as being connected to a cycler machine overnight or having tubing lying around the bed area, and mechanical factors arising from changes in the center of gravity due to large volumes of intra-abdominal fluids warrant further consideration. Patients on PD may also acquire several unfavorable characteristics that could decrease well-being and health over time and predispose them to falls. These include disordered lipid profiles and elevated glucose levels, ultrafiltration failure and the development of high transport permeability, all of which may collectively result in malnutrition, hypertension, fluid overload, and cardiovascular impairment (20,23–27).
The greatest strength of this study is the fact that data were collected simultaneously, using an identical protocol, in both PD and HD patients, allowing for optimal comparisons across the 2 populations. In addition, we chose to use biweekly patient interviews to capture falls around the time they occurred. While many studies use mail-in fall calendars on a weekly or monthly basis to reduce recall bias, we were able to reduce error from both cognitive and visual disturbances by having the study nurse interview patients in person, as well as getting additional supporting data from the nurses and health care teams. This limited underreporting and misclassification of falls attributable to recall bias. However, several limitations also exist. Patients were recruited from a single center, in a study that started several years ago, reducing the generalizability of the results. A second limitation is the relatively small sample size, resulting in poor estimation of fall-related injury rates. The data presented, however, suggest that this would result in a bias leading to an inability to identify a risk of falls associated with PD, but argue against any increased risk of falls in the HD population.
Falls in the elderly population are associated with increased hospitalization, need for long-term care, and mortality (4,8,12,16,28). Other consequences include fear of falling, resulting in physical activity restriction, functional decline, and frailty (29). Given the increased incidence of seniors in an outpatient dialysis setting and the reported fall rate in these patients, clinical nephrologists and other health care providers should consider fall risk when providing general care for these patients. Referral to multidisciplinary fall-assessment clinics may help reduce morbidity, institutionalization, and, potentially, mortality. These types of fall prevention clinics have been shown to be effective in the elderly population, and the study of these programs in the dialysis population is warranted (11,30).
Disclosures
The authors have no financial conflicts of interest to declare. SVJ has received funds to provide training in geriatric nephrology from Janssen, Canada, and speaker honoraria from Baxter and Amgen, Canada. Funding was provided by Physicians' Services Incorporated Foundation.
REFERENCES
- 1. Canadian Organ Replacement Register Annual Report, Treatment of end-stage organ failure in Canada, 2003–2012. Ottawa: CIHI; 2014. [Google Scholar]
- 2. Ontario Regional Injury Data Report. Toronto, ON: Ontario Injury Prevention Resource Centre, Parachute; 2013. [Google Scholar]
- 3. SMARTRISK InfoNotes. The economic burden of injury in Canada. Toronto, ON: Smartrisk; 2009. [Google Scholar]
- 4. Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med 1997; 337(18):1279–84. [DOI] [PubMed] [Google Scholar]
- 5. Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med 1988; 319(26):1701–7. [DOI] [PubMed] [Google Scholar]
- 6. Abdel-Rahman EM, Turgut F, Turkmen K, Balogun RA. Falls in elderly hemodialysis patients. QJM 2011; 104(10):829–38. [DOI] [PubMed] [Google Scholar]
- 7. Bannon M. Falls in older people on hemodialysis. QJM 2011; 104(10):827–8. [DOI] [PubMed] [Google Scholar]
- 8. Cook WL, Tomlinson G, Donaldson M, Markowitz SN, Naglie G, Sobolev B, et al. Falls and fall-related injuries in older dialysis patients. Clin J Am Soc Nephrol 2006; 1(6):1197–204. [DOI] [PubMed] [Google Scholar]
- 9. Rossier A, Pruijm M, Hannane D, Burnier M, Teta D. Incidence, complications and risk factors for severe falls in patients on maintenance haemodialysis. Nephrol Dial Transplant 2012; 27(1):352–7. [DOI] [PubMed] [Google Scholar]
- 10. Desmet C, Beguin C, Swine C, Jadoul M, Université Catholique de Louvain Collaborative Group Falls in hemodialysis patients: prospective study of incidence, risk factors, and complications. Am J Kidney Dis 2005; 45(1):148–53. [DOI] [PubMed] [Google Scholar]
- 11. Heung M, Adamowski T, Segal JH, Malani PN. A successful approach to fall prevention in an outpatient hemodialysis center. Clin J Am Soc Nephrol 2010; 5(10):1775–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Farragher J, Chiu E, Ulutas O, Tomlinson G, Cook WL, Jassal SV. Accidental falls and the risk of mortality amongst older adults maintained on chronic peritoneal dialysis. Clin J Am Soc Nephrol 2014; 9(7):1248–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shumway-Cook A, Ciol MA, Hoffman J, Dudgeon BJ, Yorkston K, Chan L. Falls in the Medicare population: incidence, associated factors, and impact on health care. Phys Ther 2009; 89(4):324–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Vellas BJ, Wayne SJ, Garry PJ, Baumgartner RN. A two-year longitudinal study of falls in 482 community-dwelling elderly adults. J Gerontol A Biol Sci Med Sci 1998; 53(4):M264–74. [DOI] [PubMed] [Google Scholar]
- 15. Cesari M, Landi F, Torre S, Onder G, Lattanzio F, Bernabei R. Prevalence and risk factors for falls in an older community-dwelling population. J Gerontol A Biol Sci Med Sci 2002; 57(11):M722–6. [DOI] [PubMed] [Google Scholar]
- 16. Salva A, Bolibar I, Pera G, Arias C. Incidence and consequences of falls among elderly people living in the community. Med Clin (Barc) 2004; 122(5):172–6. [DOI] [PubMed] [Google Scholar]
- 17. Buchner DM, Hornbrook MC, Kutner NG, Tinetti ME, Ory MG, Mulrow CD, et al. Development of the common data base for the FICSIT trials. J Am Geriatr Soc 1993; 41:297–308. [DOI] [PubMed] [Google Scholar]
- 18. Katzarski KS, Charra B, Luik AJ, Nisell J, Divino Filho JC, Leypoldt JK, et al. Fluid state and blood pressure control in patients treated with long and short haemodialysis. Nephrol Dial Transplant 1999; 14(2):369–75. [DOI] [PubMed] [Google Scholar]
- 19. Jang JS, Kwon SK, Kim HY. Comparison of blood pressure control and left ventricular hypertrophy in patients on continuous ambulatory peritoneal dialysis (CAPD) and automated peritoneal dialysis (APD). Electrolyte Blood Press 2011; 9(1):16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Paniagua R, Orihuela O, Ventura MD, Avila-Diaz M, Cisneros A, Vicente-Martinez M, et al. Echocardiographic, electrocardiographic and blood pressure changes induced by icodextrin solution in diabetic patients on peritoneal dialysis. Kidney Int Suppl 2008; 108:S125–30. [DOI] [PubMed] [Google Scholar]
- 21. Ulutas O, Farragher J, Chiu E, Cook WL, Jassal SV. Functional disability in older adults maintained on peritoneal dialysis therapy. Perit Dial Int 2014. doi:10.3747/pdi.2013.00293 [Epub ahead of print.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Brown EA, Johansson L, Farrington K, Gallagher H, Sensky T, Gordon F, et al. Broadening Options for Long-term Dialysis in the Elderly (BOLDE): differences in quality of life on peritoneal dialysis compared to haemodialysis for older patients. Nephrol Dial Transplant 2010; 25(11):3755–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Fortes PC, de Moraes TP, Mendes JG, Stinghen AE, Ribeiro SC, Pecoits-Filho R. Insulin resistance and glucose homeostasis in peritoneal dialysis. Perit Dial Int 2009; 29(Suppl 2):S145–8. [PubMed] [Google Scholar]
- 24. de Moraes TP, Pecoits-Filho R. Metabolic impact of peritoneal dialysis. Contrib Nephrol 2009; 163:117–23. [DOI] [PubMed] [Google Scholar]
- 25. Mehrotra R, de Boer IH, Himmelfarb J. Adverse effects of systemic glucose absorption with peritoneal dialysis: how good is the evidence? Curr Opin Nephrol Hypertens 2013; 22(6):663–8. [DOI] [PubMed] [Google Scholar]
- 26. Burkart J. Metabolic consequences of peritoneal dialysis. Semin Dial 2004; 17(6):498–504. [DOI] [PubMed] [Google Scholar]
- 27. Cheng SC, Chu TS, Huang KY, Chen YM, Chang WK, Tsai TJ, et al. Association of hypertriglyceridemia and insulin resistance in uremic patients undergoing CAPD. Perit Dial Int 2001; 21(3):282–9. [PubMed] [Google Scholar]
- 28. Speechley M, Tinetti M. Falls and injuries in frail and vigorous community elderly persons. J Am Geriatr Soc 1991; 39(1):46–52. [DOI] [PubMed] [Google Scholar]
- 29. Iglesias CP, Manca A, Torgerson DJ. The health-related quality of life and cost implications of falls in elderly women. Osteoporos Int 2009; 20(6):869–78. [DOI] [PubMed] [Google Scholar]
- 30. Cameron ID, Gillespie LD, Robertson MC, Murray GR, Hill KD, Cumming RG, et al. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev 2012; 12:CD005465. [DOI] [PubMed] [Google Scholar]