Abstract
Background
No population-based studies have directly compared the long-term health and mental health outcomes of conflict- versus non-conflict-affected communities from the same ethnic background.
Aims
To identify and compare levels of psychiatric morbidity between a traumatized and non-traumatized civilian community; to investigate the long-term impact of mass violence.
Methods
Double-stratified community surveys in Siem Reap and Surin provinces were conducted by highly qualified Cambodian interviewers using culturally validated survey instruments with known psychometric properties. These included Cambodian versions of the Hopkins Symptom Checklist-25, the Harvard Trauma Questionnaire and the Medical Outcome Study Short Form.
Results
Siem Reap and Surin respondents experienced 12,266 and 621 major trauma events, respectively; 745 (76.2%) Siem Reap respondents and six (0.6%) Surin respondents reported torture events; 499 (49.5%) Siem Reap respondents and 203 (19.7%) Surin respondents met the clinical threshold for depression (OR 4.01, 95% CI 3.29–4.88); 204 (20.6%) Siem Reap respondents and 23 (2.2%) Surin respondents met the clinical threshold for post-traumatic stress disorder (PTSD) (OR 11.39, 95% CI 7.3–17.7).The MOS physical disability was higher in Siem Reap versus Surin respondents (74 (7.5%) vs 13 (1.3%), χ2 = 47.4 df = 1, p < .001). Health status was poorest among Siem Reap respondents when compared with Surin respondents (mean score 1.59 vs 0.59, respectively; t = 19.85 df = 2018, p < .001). Path analysis reveals that recent and past extreme violence are associated with the health and mental health status of the Siem Reap community.
Conclusion
After 25 years, the Khmer civilian population that experienced the Pol Pot genocide continues to suffer psychiatric morbidity and poor health.
Keywords: Genocide, structural equation modelling, traumatic experience, Cambodian mental health
Introduction
In 1990, a team of researchers from the Harvard Program in Refugee Trauma (HPRT), with the co-sponsorship of the World Federation for Mental Health and the Ford Foundation, conducted the first large-scale mental health survey of the Cambodian refugee camp known as Site 2 (Mollica et al., 1993). This survey was conducted in a camp that housed, for over a decade, more than 150,000 Cambodian refugees who had escaped the 1975–79 Pol Pot genocide in their country of origin, and revealed a population with high levels of mass trauma and acute psychiatric morbidity. Approximately two-thirds of the Site 2 population surveyed had symptoms of major depression and one-third had symptoms of post-traumatic stress disorder (PTSD) in the clinical range. Similarly, about one-third of the Site 2 residents interviewed described their health status as poor. These refugees were eventually repatriated from Thailand to Cambodia.
At that time, a longitudinal follow-up study was neither feasible nor politically possible because of the massive UN-brokered repatriation effort. However, an important scientific question remained about whether or not these findings of high levels of psychiatric distress were unique to Cambodian refugees or generalizable to Cambodian civilians who had remained in the country. Recent studies have revealed a high prevalence of depression and PTSD in post-conflict societies (Bolton, Neugebauer & Ndongoni, 2002; Chung & Kagawa-Singer, 1996; de Jong et al., 2001; de Jong, Komproe & van Ommeren, 2003; Karam et al., 2006; Mollica et al., 2004; Pham, Weinstein & Longman, 2004; Silove et al., 2008). Community studies of Cambodian populations in Cambodia and the USA show prevalence rates of depression and PTSD significantly higher than those found in mainstream American populations (Marshall, Schell, Elliott, Berthold & Chun, 2005; Mollica et al., 1999). However, it has not been feasible to study the long-term impact of extreme violence in a civilian population both before and after an historic catastrophic event. A retrospective study by Steel, Silove, Phan and Bauman (2002) of Vietnamese refugees, more than two decades after the Vietnam War, suggested that there was a substantial reduction of symptoms over time. In contrast, the few longitudinal studies following conflict-affected and refugee populations have demonstrated that trauma-related psychiatric morbidity among refugees and other traumatized populations is chronic and unremitting in those who develop PTSD and depression (Mollica et al., 2001). At this time, the long-term mental health impact of mass violence has not been clearly demonstrated. Interpretation of the data is limited by the absence of a comparison group not affected by war and/or mass violence.
HPRT, because of its long history of clinical work in Cambodia, was in a unique position to assess the long-term mental health consequences of the Pol Pot era violence (1975–79) on Khmer citizens living in Cambodia today, and then compare these results to a non-traumatized Cambodian civilian population living in Surin, Thailand. To the best of our knowledge, this is the first community study that compares a conflict-affected and a non-conflict-affected civilian population from similar ethnic backgrounds in order to examine whether survivors of extreme violence continue to suffer from health and mental health problems decades later.
Our research goals were: (1) to examine the chronological sequencing of traumatic exposure among Cambodian civilians exposed to sequential epochs of conflict, repression and abuse; (2) to evaluate the mental health impact of the Cambodian civil war 25 years later on a Cambodian civilian population living in Cambodia; (3) to compare the mental health status of a Cambodian civilian population exposed to mass violence with a non-traumatized Cambodian civilian population; (4) to examine the extent to which age, gender and traumatic exposure mediate symptoms of PTSD and depression in Cambodian civilians; and (5) to consider the public health implications of our survey results for the health and mental health care of Cambodian survivors, as well as to discuss the ability to generalize findings to other traumatized communities.
Methods
The survey design and methodology was based upon the 1990 survey undertaken by the HPRT research team among Cambodian refugees displaced to the Site 2 refugee camp located on the Cambodia–Thailand border (Mollica et al., 1993). In accordance with the findings of that previous survey, we aimed to undertake respondent interviews with approximately 1,000 households in the province of Siem Reap, Cambodia and the province of Surin, Thailand.
Siem Reap province has a rural population of 170,000 persons according to the Cambodian Consul Ministry of Planning in 2001–02. Siem Reap is the ancestral home of Angkor Wat and is considered the cultural, historical and spiritual heart of Cambodia. Because of its spiritual importance, Siem Reap was a major stronghold of the Khmer Rouge regime from 1975 to 1979. HPRT, with the support of United States Agency for International Development (USAID) and the Cambodian Ministry of Health, founded one of the first mental health clinics in Cambodia primary health care in Siem Reap City in 1994. Due to the presence of trained Cambodian clinical staff, HPRT was in an ideal position to conduct a survey in Siem Reap province.
The communities in Surin province in Thailand are principally people of Cambodian origin and identity who live in the Muang and Prasat districts. Characteristics of the typical Thai–Khmer community include people of Khmer origin who: (1) have a traditional Khmer lifestyle; (2) live in villages traced to Cambodian origin; (3) principally speak Khmer language; and (4) live in geographical settlements surrounded by ancient Khmer monuments. The Prasat district was selected for the study because its citizens are predominantly Khmer and they were not directly affected by the civil war in neighbouring Cambodia. The Prasat district located in the southern part of Surin province is similar in size to Siem Reap province with a total population in 1998 of 152,873 residents.
Both surveys applied multi-stage cluster sampling designs to obtain representative samples of the selected provinces. In the first step a regional map of each province was obtained from local health authorities to randomly select 50 clusters, with the probability of selection proportional to the population size of the cluster, drawing on census data for the two regions. We next identified a simple random sample of 20 households within each of the selected clusters from a list of households obtained from local authorities. Trained Khmer interviewers visited each household to complete a household census of all resident adults (age 18 and older) within the household. Each adult was assigned a number between 1 and n (n being the number of adults who resided in that household), with one adult being randomly selected and requested to participate in the survey based upon age (oldest received number 1, youngest number n). In addition, all children 12 or 13 years old and adolescents 16 or 17 years old were asked to participate. The child survey is not reported in this manuscript.
In Siem Reap, the survey interviews were conducted by trained Cambodian mental health practitioners who were members of HPRT’s primary health care mental health clinic in Siem Reap City. In Surin, health practitioners working for the local Thai Ministry of Health who were fluent in both Khmer and Thai conducted the household interviews. Interviewers across both surveys were supervised by HPRT’s local and international research staff. All Surin respondents were confirmed during the interviews by self-report and staff observation of being of Khmer ethnicity. Training sessions were conducted at each site for five days by HPRT’s research staff from Cambodia and the USA. The interviewers were instructed to refrain from prompting, probing or other departures from the survey questions. Each interviewer explained to potential participants that this was a survey of their health status that was being supported by their respective local Ministries of Health. The participants were not offered any compensation at the start of the interview process. However, at the end of the completed survey cycle all participants received a bag of rice as an honorarium for their time and effort. There was no evidence that respondents exaggerated their mental health problems or their traumatic life events in order to please the HPRT interviewers, the Ministry of Health or to obtain compensation since none was initially offered.
In Surin, all surveys were also translated into Thai so that the proper meaning of terms was available to bilingual respondents. Equal numbers of male and female interviewers were used and the interviewers were randomly assigned to the selected clusters. The interviews averaged approximately 90 minutes and were conducted in the Khmer language in Siem Reap and Surin. At the end of each survey day, the supervisor reviewed every questionnaire for completeness and accuracy in reporting. Problems were immediately corrected. This quality assurance process previously cited by HPRT (Mollica et al., 1993) maximized reporting with almost a 100% survey completion rate. Informed consent was obtained from each respondent. No individual identifying information such as names or addresses was recorded. Given the sensitive nature of some questions, the services of HPRT’s clinic in Siem Reap and the local health clinic in Surin were made available. At each site, less than five people refused to be interviewed and no one sought services at the local health centre. All aspects of this current research were reviewed and approved by the Institutional Review Board (IRB) of the Harvard Medical School, the Ethics Committee of the Thai Ministry of Health, the IRB of the Massachusetts General Hospital and the Ethics Committee of the Cambodian Ministry of Health.
The Surin interviews were conducted in 1998; political instability in Cambodia did not allow the next phase of the survey in Cambodia until 2004. Once the permanent government in Cambodia was securely in place, we conducted the Siem Reap survey.
Measures
As in our previous population research among Cambodian refugees, we applied the Hopkins Symptom Checklist (HSCL-25) and the Harvard Trauma Questionnaire (HTQ) (Mollica et al., 1992; Mollica, Wyshak, Marneffe, Khuon & Lavelle, 1987). The HSCL-25 includes a 15-item scale of depressive symptoms and the HTQ contains a 16-item scale of diagnostic criteria for PTSD as defined in the DSM-IV (APA, 1994). Both instruments have been widely translated and used in general studies among diverse cultural groups (Cardozo, Vergara, Agani & Gotway, 2000; Kagee, 2005; Mollica et al., 1999; Shrestha et al., 1998), including Cambodian populations (Dubois et al., 2004; Mollica et al., 1993), and have demonstrated high internal consistency and reliability across a range of population groups (Kleijn, Hovens & Rodenburg, 2001). Palmieri, Marshall and Schnell (2007) have conducted a confirmatory factor analysis study of the HTQ administrated in Khmer to resettled Cambodian refugees in a community study that demonstrated results similar to those found for English speakers completing other measures of PTSD symptom severity. Categorical measures of probable depression and PTSD from the HSCL-25 and HTQ, respectively, have validated against clinical diagnosis (Silove et al., 2007; Smith Fawzi et al., 1997), with a recent study in Bosnia revealing a sensitivity and specificity for each instrument of greater than 90% for depression and PTSD, respectively (Oruc et al., 2008). Established cut-off scores for the HTQ and HSCL-25 among Cambodian populations were applied to determine prevalence estimates for each population. Continuous scores were also used to examine differences in symptom severity.
The HTQ trauma event section assessed lifetime exposure to 38 events of extreme violence and 19 possible torture events. The torture experiences conformed to international definitions of torture (Rasmussen, 1990). Respondents were also asked using a calendar to identify in which of the five eras (relevant to Cambodian history) these traumatic events had occurred: (1) pre-Pol Pot period (before 1975); (2) Pol Pot era (1975–79); (3) Vietnamese occupation of Cambodia (1979–90); (4) Cambodian election period (1990–97); and (5) recent events (1997–98 for Surin or 2004 for Siem Reap). In this paper these self-reported extreme trauma and trauma events are referred to as potential trauma events (PTEs). A list of recent life stresses commonly experienced in the year prior to the interview was also surveyed; this included 21 recent life events, including divorce, major illness and car accident, compiled by HPRT field staff through key informant surveys of local health care providers.
Disability was measured using the six-item physical functioning scale of the Medical Outcome Study 20-item short-form (SF-20), which has been tested for its reliability and validity in a large number of different settings, countries and languages (Stewart, Hays & Ware, 1988). For disability, the item responses were summed on the physical functioning scale of the SF-20 and then transformed linearly to a 0–100 scale, with 0 indicating the poorest physical functioning and 100 indicating no limitations in physical functioning. Using the conventions established in our earlier analysis, a dichotomous variable was created from the 100-point functioning impairment scale (Mollica et al., 2001). A cut-off of 50 was applied to define disability. The cut-off is more stringent than that used in the USA (Stewart et al., 1988) to determine physically impaired individuals who by most professional and clinical standards would unequivocally be classified as disabled. We also asked respondents if they had been diagnosed with any of 15 medical conditions that had been identified by the HPRT clinic in primary health care in Siem Reap, Cambodia and the local Ministry of Health in Surin, Thailand.
Inter-rater reliability was computed for all major survey items among 37 control interviews in both surveys conducted by the trained Khmer interviewers. There was near perfect agreement for almost all items, with the k statistic exceeded 0.90 for items in the scales.
Statistical analysis
Results from Siem Reap and Surin (n and %) are presented as unweighted observed estimates. The clustering effect for village and region was examined using MLwiN (v2.0) (Rasbash, Steele, William Browne & Prosser, 2005). The analyses revealed small intra-class correlations (ICC) for trauma exposure (the number of traumatic events) (ICC = 0.018), PTSD (ICC = 0.036) and depression (ICC = 0.05), obviating the need to adjust for clustering in the analyses that followed. Comparisons between socio-demographic, traumatic and symptomatic characteristics of the Siem Riep and Surin respondents was compared using two-sample t-test for count and continuous data and cross-tabulation and logistic regression for categorical variables. For analyses involving small cell sizes, the Fisher exact statistic was calculated. To control for multiple tests, a global measure was used to protect against type I errors; when that approach was not possible, Bonferroni adjustments were made.
We examined for symptomatic associations with PTSD and depression by country using the general linear model function within SPSS v 17.0. (SPSS, 2008) The initial models aggregated across samples and identified a substantial country and an age-by-country interaction effect. Hence we examined for the dose–effect relationship between lifetime PTEs and PTSD and depression separately for Siem Reap and Surin. For each mental health outcome, we tested for the effect of the frequncy of lifetime potential traumatic experience (PTE) on mental health. Due to the long-term nature of the traumatic experiences, the effects may be time limited and thus mathematically produce a nonlinear result.
To examine for the effect of era-specific traumatic experiences on current mental health, path analysis was applied using Mplus v 5.0 (Muthén & Muthén, 1998–2008). Examination of the impact of historical traumatic experience on current mental and functional health was limited to the Siem Reap sample due to the multiple periods of traumatic epochs that uniquely faced that community. Path analysis allows for the simultaneous examination of the impact of trauma on all key mental health indices while taking into account comorbidity in traumatic and other experiences across the outcome indices. The path analysis was developed using the following theoretical considerations. First, potential traumatic events preceded mental health outcomes, health status and functional status. The potential traumatic events were placed in historical order with prior history events being able to predict future events for two subsequent periods, based on the common finding that prior exposure to trauma increases vulnerability to being traumatized again. Theoretical considerations suggested that the mental health outcomes should precede health and functional status (Schnurr & Green, 2004). Age and gender were allowed to influence each independent and dependent variable and were removed if non-significant. In general, in keeping with the literature, it was anticipated that men would experience more PTEs and women have greater mental health problems (Olff, Langeland, Draijer & Gersons, 2007). The initial model hypothesized that mental health would fully mediate the effect of traumatic experience to functional and general health status. We commenced with a saturated model according to the aforementioned directional structure and any paths that did not display significant associations with proceeding variables were removed from the model.
A non-significant χ2 statistic was applied as the criterion of model fit (Hayduk, Cummings, Boadu, Pazderka-Robinson & Boulianne, 2007). The standardized β values represent the proportion of the standard deviation that β varies from zero, allowing direct comparison of different βs. Because the sample size was large (N = 989) and χ2 tends to be inflated with large samples sizes (> 200) we included other recommended indicators (Barrett, 2007; Kline, 2005): the Comparative Fit Index (CFI), the Tucker Lewis Index (TLI) (both should exceed 0.9) (Hair, Anderson, Tatham & Black, 1998); and the root mean square error of approximation (RMSEA) (< 0.05 supports a good fit) (Browne & Cudeck, 1993).
Results
Table 1 provides the demographic characteristics of the two communities, Siem Reap and Surin. There were no gender differences but a small age difference (the Siem Reap sample had fewer middle-aged and older respondents). There were more widowed participants from Siem Reap. Both communities had a low level of education with respondents from Surin having on average 4.9 years of education compared to 2.5 years for respondents from Siem Reap. Almost all identified as being Buddhist, with Surin respondents reporting a higher level of engagement in Buddhist practices such as meditation and knowledge about Buddhist principles.
Table 1.
Demographic and trauma characteristics of Siem Reap, Cambodia (N = 989) and Surin, Thailand (N = 1031).
| Variable | Siem Reap | Surin | Statistic | p |
|---|---|---|---|---|
| Gender n female (%) | 624 (63.1) | 668 (64.8) | χ2 = 0.63 df = 1 | ns |
| Mean age (SD) | 43.3 (13.1) | 45.0 (15.2) | F1,2108 = 7.41 | .007 |
| Age (category) | n (%) | n (%) | ||
| 18–25 yrs | 80 (7.8) | 74 (7.5) | χ2 = 15.2 df = 4 | .004 |
| 26–35 yrs | 225 (21.8) | 237 (24.0) | ||
| 36–45 yrs | 274 (26.6) | 292 (29.5) | ||
| 46–55 yrs | 190 (18.4) | 204 (20.6) | ||
| 56+ yrs | 262 (25.4) | 182 (18.4) | ||
| Education and literacy | ||||
| Mean years of schooling (SD) | 2.5 (2.9) | 4.9 (3.1) | F1,2014 = 318.3 | .001 |
| Marital status | n (%) | n (%) | ||
| Married | 733 (74.3) | 762 (74.2) | χ2 = 51.3 df = 4 | .001 |
| Separated | 2 (0.2) | 40 (3.9) | ||
| Divorced | 13 (1.3) | 18 (1.8) | ||
| Widowed | 190 (19.3) | 132 (12.9) | ||
| Never married | 48 (4.9) | 75 (7.3) | ||
| Religion | n (%) | n (%) | ||
| Buddhist | 976 (98.8) | 1027 (99.8) | χ2 = 9.14, df = 3 | .05 |
| Chants and meditates | 435 (44.4) | 777 (78.8) | χ2 = 246.2, df = 1 | .001 |
| Knows Buddhist | 1.48 (2.0) | 2.14 (2.0) | F1,2018 = 54.2 | .001 |
| principles (0–5) | ||||
| Traumatic experiences (PTE) | n (%) | n (%) | ||
| 0 | 26 (2.6) | 685 (66.4) | χ2 = 1506.7, df = 5 | .001 |
| 1 or 2 | 60 (6.1) | 280 (27.2) | ||
| 3 or 4 | 71 (7.2) | 47 (4.6) | ||
| 5 or 6 | 97 (9.8) | 13 (1.3) | ||
| 7–10 | 166 (16.8) | 6 (0.6) | ||
| 11–15 | 238 (24.1) | |||
| 16–20 | 214 (21.6) | |||
| 21–25 | 85 (8.6) | |||
| 26+ | 32 (3.2) | |||
| Torture | 754 (76.2) | 6 (0.6) | χ2 = 1230.3, df = 1 | .001 |
| Recent life stresses | ||||
| M (SD) | M (SD) | |||
| Count of 21 life stresses | 1.7 (1.5) | 1.9 (1.6) | t = 2.15, df = 2018 | .032 |
| No recent life stress (%) | 25.1 | 17.1 |
The communities displayed substantial differences in the level of self-reported exposure to PTEs, with 78% (n = 745) of Siem Reap respondents reporting torture experiences and a lifetime endorsement of exposure of 12 different (M = 12.2, SD = 7.0) types of trauma. Surin respondents reported almost no torture episodes (0.6%, n = 6) and a limited lifetime exposure to PTEs (M = 0.61, SD = 1.14). There were minor differences between the two samples with respect to recent life events, with Surin respondents endorsing more recent life events.
Respondent endorsement of self-reported trauma events by historical epoch are displayed in Table 2 for the Siem Reap respondents. The Khmer population in Siem Reap province had experienced extensive trauma across multiple epochs including the Vietnamese era where there was substantial violence second only to the Pol Pot era. Reporting for the most recent era showed that Siem Reap residents were not free of extreme trauma having experienced, as a group, 574 trauma events (PTEs), including reports of starvation (n = 274) and torture (n = 87). In comparison, in Surin there was minimal trauma across all epochs compared to Siem Reap. For the most the recent era in Surin there were 201 severe trauma events (PTEs), including reports of beatings (n = 27), extortion (n = 12), witnessing of beatings (n = 62), rape (n = 2) and torture (n = 2).
Table 2.
Summary table of traumatic events (PTEs) by historical period.
| Pre-Pol Pot era before 1975 |
Pol Pot era 1975–78 |
Vietnam era 1978–90 |
Election era 1990–97 |
Recent era 1997–2004 |
|
|---|---|---|---|---|---|
| Siem Reap | |||||
| Total number traumas | 386 | 7,466 | 2,793 | 843 | 574 |
| Mean (SD) | 0.39 (1.1) | 7.55 (5.8) | 2.82 (2.7) | 0.86 (1.7) | 0.58 (1.1) |
| Median | 0 | 8 | 2 | 0 | 0 |
| Maximum number | 15 | 26 | 21 | 16 | 9 |
| Number with no trauma (%) | 773 (78.2) | 185 (18.7) | 192 (19.4) | 650 (65.7) | 680 (68.8) |
| Surin | |||||
| Total number traumas | 83 | 71 | 122 | 144 | 201 |
| Mean (SD) | 0.08 (0.41) | 0.07 (0.30) | 0.12 (0.53) | 0.14 (0.45) | 0.19 (0.54) |
| Median | 0 | 0 | 0 | 0 | 0 |
| Maximum number | 5 | 4 | 8 | 5 | 7 |
| Number with no trauma (%) | 978 (94.9) | 970 (94.1) | 953 (92.4) | 918 (89.0) | 875 (84.9) |
Table 3 shows the mental health and other health indices as continuous measures and where relevant as probable diagnostic cases based on established cut-off scores. Four hundred and ninety (49.5%) of Siem Reap respondents and 203 (19.7%) of Surin were above the clinical threshold for depression. This represented a fourfold (OR 4.01, 95% CI 3.29–4.88) increase in the odds for depression among Siem Reap respondents. Two hundred and four (20.6%) of Siem Reap respondents and 23 (2.2%) of Surin respondents were above the clinical threshold for PTSD, representing a tenfold increase in the odds of PTSD (OR 11.39, 95% CI 7.3–17.7) in the Siem Reap population. The correlation of age and gender with depression and PTSD were considered in the in-depth dose–effect and path analyses controlling for trauma.
Table 3.
Psychiatric status of Khmer living in Seam Reap, Cambodia and Surin, Thailand.
| Continuous scores | Siem Reap (N = 989) |
Surin (N = 1,031) |
|||||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | ||||
| PTSD scorea | 1.98 | 0.62 | 1.41 | 0.41 | F1,2019 = 580.4, p < .001 | ||
| Depression score | 1.84 | 0.62 | 1.46 | 0.43 | F1,2019 = 308.8, p < .001 | ||
|
| |||||||
| Threshold scores | n | % | n | % | Odds | (95% CI) | |
|
| |||||||
| PTSDb | 2.5 | 204 | 20.6 | 23 | 2.2 | 11.39 | 7.33–17.7 |
| Depression | 1.75 | 490 | 49.5 | 203 | 19.7 | 4.01 | 3.29–4.88 |
PTSD score based on a continuous measure on the HTQ.
PTSD score based on cut-off point on the HTQ.
Table 4 shows the physical and health problems of each population. Based on SF-20 physical disability scale (i.e. six ranked items limited in vigorous activity through to limited in daily activities due to health), 74 (7.5%) from Siem Reap and 13 (1.3%) from Surin (χ2 = 47.4, df = 1, p < .001) were classified as disabled, respectively. On average, those in Siem Reap experienced 1.6 (SD = 1.4) physical illnesses, compared to 0.6 (SD = 0.9) in Surin (F1,2018 = 396.4, p < .001), with the largest difference being a greater prevalence of malaria in Siem Reap. There was a significant linear relationship between the number of physical illnesses and PTSD and depression in both surveys (Siem Reap r = 0.16 and 0.22, p < .001; Surin r = 0.18 and 0.20, p < .001). In contrast, those in Siem Reap reported less energy to participate in a range of daily functional activities.
Table 4.
Physical health problems of Khmer living in Siem Reap, Cambodia and Surin, Thailand.
| Physical illness | Surin (N = 1,031) |
Siem Riep (N = 989) |
||||
|---|---|---|---|---|---|---|
| n | % | n | % | χ 2 | df = 1 | |
| Severe functional health status | 13 | 1.3 | 74 | 7.5 | 47.4 | < .001 |
| Hypertension | 81 | 7.9 | 80 | 8.1 | 0.04 | ns |
| Heart disease | 48 | 4.7 | 133 | 13.4 | 43.65 | < .001 |
| Stroke | 2 | 0.2 | 4 | 0.4 | 0.75 | ns |
| Cancer | 2 | 0.2 | 0 | 0 | ||
| Anemia | 66 | 6.4 | 65 | 6.6 | 0.03 | ns |
| Tuberculosis | 31 | 3.0 | 84 | 8.5 | 27.74 | < .001 |
| Diabetes | 25 | 2.4 | 10 | 1.0 | 5.81 | < .05 |
| Arthritis | 68 | 6.6 | 277 | 28.1 | 135.72 | < .001 |
| Ulcer | 135 | 13.1 | 178 | 18.1 | 7.88 | < .005 |
| Asthma, chronic bronchitis or emphysema | 32 | 3.1 | 28 | 2.8 | 0.12 | ns |
| Cirrhosis or chronic liver disease | 2 | 0.2 | 11 | 1.1 | 6.63 | < .01 |
| Kidney, urinary tract or bladder disease | 46 | 4.5 | 34 | 3.4 | 1.33 | ns |
| Gynaecological disorders (women) | 33 | 5.0 | 116 | 11.6 | 49.87 | < .001 |
| Prostate (men) | 1 | 0.3 | 0 | 0 | ||
| Seizure disorders | 5 | 0.5 | 34 | 3.4 | 22.81 | < .001 |
| Malaria | 33 | 3.2 | 521 | 52.7 | 451.1 | < .001 |
| HIV/AIDS | 0 | 0 | 2 | 0.2 | ||
Frequency of number of 16 physical disorders mean (SD): Siem Reap 1.59 (1.36); Surin 0.59 (0.86) (t = 19.85, df = 2018, p < .001).
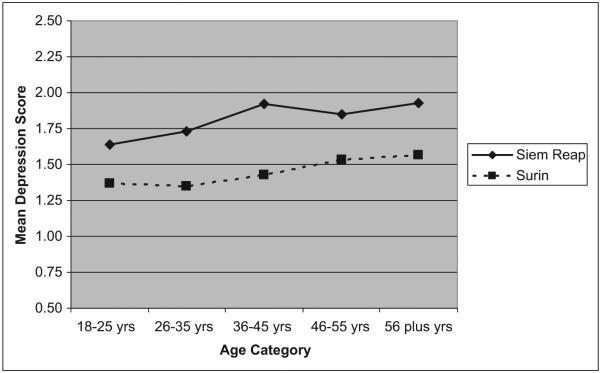
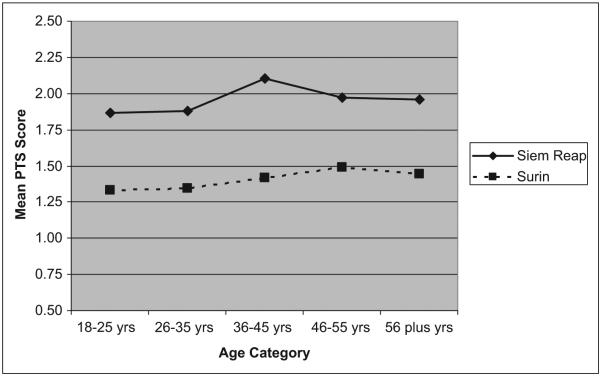
Figure 1 shows the relationship between the continuous measure of depression symptoms and age for each community, and Figure 2 shows the same for PTSD symptoms. The results from Siem Reap and Surin were first examined aggregating across the two communities. For depression, the Generalized Linear Model (GLM) suggested an overall linear trend with each age category, with a significant interaction between age and community (F4,2010 = 2.61, p = .034), and a main effect for age (F4,2010 = 13.44, p < .001) and for community (F1,2010 = 54.95, p < .001). This finding was examined using linear regression for each community separately and a linear trend was identified for Surin (β = 0.066, standardized β = 0.21, t = 6.78, p < .001) and for Siem Reap (β = 0.062, standardized β = 0.12, t = 3.84, p < .001). Based on the standardized β, the interaction term appears to be due to the differential rates of increase in depression, with age having a stronger effect in Surin. For PTSD, the GLM also revealed a significant interaction between age category and community (F4,2010 = 2.61, p = .034), and the main effect of age (F4,2010 = 13.44, p < .001) and community (F1,2010 = 54.95, p < .001). Separate linear regression models for Surin identified a linear age trend (β = 0.035, standardized β = 0.11, t = 3.51, p < .001); however, there was a non-significant linear trend for Siem Reap (β = 0.022, standardized β = 0.04, t = 1.34, p = .18).
Figure 1.
Mean depression by age and community.
Figure 2.
Mean post-traumatic stress score by age and community.
Due to the substantial difference between Siem Reap and Surin, we examined the depression and PTSD dose–effect associations with exposure to PTEs separately for each sample. Table 5 shows that female gender was associated with higher levels of PTSD and depression in both communities. In Surin there was an age relationship that indicated that for each additional year of age, the amount of PTSD and depression increased; whereas in Siem Reap, younger respondents had higher levels of PTSD and there was no relationship between age and depression. While the β coefficient for PTEs appeared lower within Siem Reap, this reflected the higher number of endorsed PTEs in this sample with the standardized parameters for PTE being stronger in Siem Reap than Surin. In examining the change in R2, it was found that age and gender played an equivalent role in determining the level of PTSD and depression in Surin. Specifically, for PTSD, R2 for age and gender was 0.06, and the model improved by 0.07 with the addition of lifetime trauma. However, in Siem Reap lifetime trauma was a much stronger predictor of PTSD and depression than age and gender: for depression, age and gender accounted for 0.05 and the addition of lifetime trauma resulted in a change in R2 of 0.16. Thus, this analysis showed a dose effect of lifetime traumatic experience in both communities for both depression and PTSD, but a stronger role for traumatic experience in Siem Reap than in Surin. A series of additional nonlinear models were also examined that tested for squared, logarithmic and exponential effects of PTE on each mental health index. The nonlinear parameters in all analyses did not result in additional fit improvement, supporting a linear relationship between traumatic experiences in both populations.
Table 5.
Dose effect of lifetime PTEs.
| Change in R2 |
Total R2 | |||||||
|---|---|---|---|---|---|---|---|---|
|
ß
a
|
St. ßb | Model 1 | Model 2 | |||||
| Gender | Age | PTE | PTE | Gender and age |
Gender, age and trauma |
|||
| PTSD | Surin | −0.44 | 0.003 | 0.10 | 0.26 | 0.06 | 0.06 | 0.12 |
| Siem Reap | −0.42 | −0.007 | 0.04 | 0.48 | 0.02 | 0.18 | 0.20 | |
| Depression | Surin | −0.45 | 0.010 | 0.10 | 0.27 | 0.10 | 0.07 | 0.17 |
| Siem Reap | −0.54 | −0.002 | 0.04 | 0.45 | 0.05 | 0.16 | 0.20 | |
raw ß coefficient;
standardized ß coefficient.
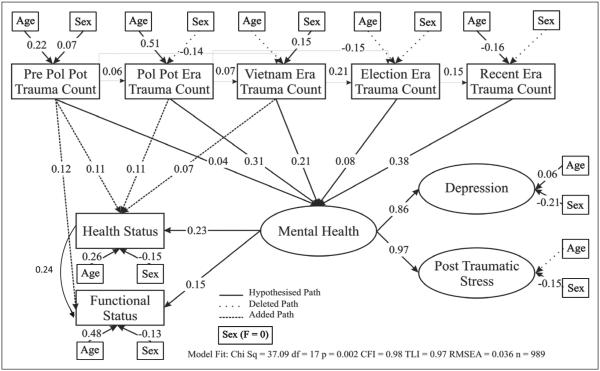
To investigate the mental health impact of sequential exposure to PTEs across multiple epochs of human rights and humanitarian abuse affecting the population of Siem Reap, we undertook a path analysis using structural equation modelling. The specified model examined the frequency of endorsed PTEs order for each of five historical epochs. Preliminary modelling supported the use of a single index of mental health distress derived from the HSCL-25 depression scale and the HTQ PTSD scale. We also looked at the impact on general health status as assessed by the six-item physical functioning scale of the SF-20 and a single four-point item global health. The model was conducted among the Siem Reap participants only because there were too few events among the Surin population by epoch. Figure 3 shows the results of the final model with non-significant age and gender influences shown as dotted lines. Table 6 presents the total effects of the path analysis based on fully standardized parameters. The final model provided a good fit to the data (χ2 = 37.09, df = 17, p = .002; CFI = 0.98, TLI = 0.97, RMSEA = 0.036), with CFI, TLI and RMSEA all indicating a satisfactory model; the significant χ2 value suggested that further improvements in the model could be made, but parsimony considerations suggested against this (Kline, 2005).
Figure 3.
Structural model for examining relationship between within-era trauma events (PTEs) and current mental health in Siem Reap, Cambodia (N = 989).
Table 6.
Total effects of the path analysis: Trauma events predicting mental health, health status and functional health.
| R2 | Gender | Age | pPP | PP | VE | EE | RE | MH | |
|---|---|---|---|---|---|---|---|---|---|
| Mental health | 0.29 | 0.04 | 0.11 | 0.03 | 0.31 | 0.24 | 0.14 | 0.38 | |
| Health status | 0.23 | −0.12 | 0.36 | 0.11 | 0.19 | 0.13 | 0.03 | 0.09 | 0.24 |
| Functional status | 0.32 | −0.12 | 0.52 | 0.12 | 0.07 | 0.02 | −0.09 | 0.07 | 0.18 |
Standardization facilitates the comparison of variables, which are measured on different scales; they have a mean of 0 and standard deviation of 1, interpreted as change in standard deviation units.
Within the total effects there exist a number of complex effects because some pathways are negative; particularly in Siem Reap, trauma counts between the eras are negative and thus the total effects are smaller than the direct effects.
pPP = pre-Pol Pot; PP = Pol Pot; VE = Vietnam era; EE = election era; RE = recent era; MH = mental health.
PTEs experienced in the Pol Pot and most recent eras were the largest contributors of mental health. Although more recent, the Vietnam era traumatic experience had a smaller impact than the Pol Pot era. For the other eras, the relationships between traumatic experience and mental health were less strong, although significant. The age and gender relationships within the path analysis made substantial ecological sense: older men experienced more pre-Pol Pot trauma; older people reported high levels of trauma during the Pol Pot era; the surviving women experienced more trauma during the Pol Pot era than the surviving men. During the Vietnam epoch, there were no age effects but men were more traumatized than women; in the recent epoch, the young experienced more trauma. Consistent with general patterns, women had more depression and PTSD symptoms. Further, women reported a poorer health status and poorer functional status. The degree of trauma in the three older epochs were directly associated with poorer health status, and the pre-Pol Pot experience was directly related to poorer functional health. Both depression and PTSD symptoms were strong indicators of current mental health, which had a strong relationship to current health status and a moderate one to current functional status. While age made the greatest contribution to health and functional status, the model identified four direct paths (Figure 3) from PTEs experienced during earlier epochs. These paths indicate that older traumatic experience were only partially mediated by mental health having a direct impact on health status.
Discussion
Over the past three decades, the mental health impact of extreme violence on refugees and civilian populations worldwide has been well documented (Bolton et al., 2002; Chung & Kagawa-Singer, 1996; de Jong et al., 2001; de Jong et al., 2003; Dubois et al., 2004; Karam et al., 2006; Mollica et al., 1993; Mollica et al., 2004; Pham et al., 2004; Silove et al., 2008). A recent five-country study in the Balkans revealed high levels of PTSD and depression among war-affected people several years after the war in former Yugoslavia had ended (Priebe et al., 2010). In Cambodia, we not only tested these findings but were also able to compare the mental health impact of extreme violence on a traumatized civilian population (i.e. Siem Reap) with an ethnically comparable non-traumatized population (i.e. Surin).
In our Siem Reap survey, the most striking findings are the high levels of experienced violence (PTEs) experienced by Siem Reap residents as compared to the Khmer living in Surin. During the five time periods reported, almost 97% of the Siem Reap group had experienced at least one event of extreme violence and 76% had been tortured. These data reaffirm the impossibility of finding non-traumatized residents in Siem Reap province and the importance of our comparative study design. In contrast, the neighbouring Surin Khmer in Thailand had not experienced the Pol Pot genocide or the Vietnamese occupation and few people had experienced extreme violence and almost no one had been tortured. What is most striking, however, is that extreme trauma events in Siem Reap, although greatly diminished after the Pol Pot period, continued to remain relatively high, affecting 30% of the Siem Reap survey population during the recent era. These events included 274 reports of starvation and 87 torture events. Our results are troubling not only in terms of possible ongoing human rights violations, but also when compared to the findings of the meta-analysis of 181 surveys in 40 countries by Steel et al. (2009). That analysis found that the high mental health impact of extreme violence was not only associated with the triggering events but also with conditions of ongoing threats and insecurity (Steel et al., 2009).
In Siem Reap, 49.5% of the respondents were above the clinical threshold for depression. This contrasts sharply with levels of depression in Surin of 19.7% and those found in non-traumatized developed countries (Kessler et al., 2005a, 2005b). Dubois et al. (2004), using similar instruments and sampling methods in Kampong Cham province, Cambodia, found the prevalence of depression to be 42.4% in their community sample, which is comparable to our Siem Reap findings of 49.5%. These two Cambodian civilian population surveys highlight the important public health significance of depression in Cambodia. Similarly, the fact that one in five Khmer civilians in Surin may be affected by depression is consistent with the economic downturn that was occurring in that country during the year of the Surin survey.
The Siem Reap rate of possible PTSD in our survey of 20.6% is also significantly higher than the 2.2% found in Surin. The Kampong Chan survey (Dubois et al., 2004) had a lower rate of PTSD of 7.3%, while a national study of Cambodia demonstrated a prevalence of PTSD of 11.2%, still much higher than baseline studies (Helzer, Robins & McEvoy, 1987; Kessler, Sonnega, Bromet, Hughes & Nelson, 1995; Sonis et al., 2009). The higher levels of PTSD that we documented in Siem Reap compared to other Cambodian mental health surveys may reflect the heightened level of historical violence in Siem Reap since it is the home of Angkor Wat and therefore was a major Khmer Rouge site of forced labour and concentration camps. After the fall of the Pol Pot regime and the invasion and occupation by the Vietnamese, many former incarcerated Khmer remained in Siem Reap.
In our dose–effect analysis, gender (i.e. being female) was associated with higher levels of PTSD in both communities (Olff et al., 2007). The extreme violence (PTEs) that has continued in Siem Reap province, although at much lower levels right up until the time of the survey, may not only explain current levels of PTSD in Siem Reap, as witnessed in the major contribution of PTEs during the recent time period as revealed by our path analysis (Figure 3), but also the potential impact of violence on young people who were not born or were under 10 years of age at the end of the Khmer Rouge Regime in 1979. In Siem Reap, younger respondents had higher rates of PTSD. They may have been affected by violence directly or through intergenerational transmission. Our data on youths of 18 years and younger, to be presented in future transcripts, will shed some light on this finding.
The significant overall differences between Siem Reap and Surin in the presence of physical illnesses and physical disability are consistent with the higher levels of psychiatric morbidity in Siem Reap. Furthermore, our dose–effect analysis has replicated the findings of our studies of Cambodian and Bosnian refugees, revealing an association between increased levels of trauma events and higher levels of psychiatric symptoms (Mollica et al., 1999; Mollica, McInnes, Poole & Tor, 1998). Our path analysis, while it cannot imply causality in a cross-sectional study, does suggest that in the Siem Reap population there is an enduring health and mental health impact of mass violence on this civilian population 25 years after the seminal historical event (Bramsen & van der Ploeg, 1999; Sonis et al., 2009). In Siem Reap, the trauma events of the Pol Pot genocide (1975–79) and to a lesser extent the Vietnam era invasion and occupation of Cambodia still appear to be exercising an adverse mental health impact on people’s lives. These mental health problems (i.e. depression and PTSD), in turn, are associated with decreased health and physical functioning of the affected population. The Dohrenwends in the 1980s described a number of models portraying the ways in which life events affect health (Dohrenwend & Dohrenwend, 1981a, 1981b, 1983). Our path analysis supports one of their hypotheses: that life events in the distant past as well as the present directly cause adverse psychiatric reactions, such as PTSD and depression. They termed this model ‘victimization’, demonstrating that trauma-related mental health problems contribute, along with personal and social factors such as age and gender, to poor health outcomes. Our results add to the current scientific literature on the contribution of adverse life events to illness and disability and the important role of extreme violence as a major risk factor (Edwards, Holden, Felitti & Anda, 2003; Felitti et al., 1998; Sareen et al., 2007; Sledjeski, Speisman & Dierker, 2008).
The high prevalence of psychiatric symptoms, especially PTSD, in highly traumatized populations affected by extreme violence, has in the past generated concerns (Kleinman, 1987; Summerfield, 1999; Weiss, Saraceno, Saxena & van Ommeren, 2003). Our results demonstrate a strong association between extreme trauma events and the symptoms and diagnoses of PTSD and depression, respectively. Most importantly, in Siem Reap, our path analysis reveals the possible link between health, mental health and extreme violence. Our results in Cambodia, supported by the research of Dubois et al. (2004) in Kampon Cham province, clearly show that depression and PTSD are not largely epiphenomena but in fact have serious health consequences (Sareen et al., 2007; Sledjeski et al., 2008).
A major concern about high levels of depression and PTSD in a civilian population is what to do with this information, especially in a resource-poor country such as Cambodia (Kessler et al., 2005b; Kroenke, 2001; van Ommeren, Sharma & de Jong, 1997). Community members suffering from mental health symptoms rely on a host of therapeutic interventions, including traditional healing, selftreatment, family consultation and spirituality (Kleinman, 1980; Lavelle, Tor, Mollica, Allden & Potts, 1996). Unfortunately, little information is available in Cambodia to identify the determinants for who uses traditional and locally available approaches from those who do not, nor the efficacy of traditional interventions. The World Health Organization (WHO, 1990, 1994) has set a priority for integrating mental health services into primary health care in low- and middle-income countries. Our team at HPRT has had extensive experience with this, including establishing one of the first mental health clinics in primary care in Siem Reap City, Siem Reap province, Cambodia in the early 1990s. Our approach has been similar to the approach used by the Dutch-based Trans-Cultural Psychosocial Organization (TPO) in Battambang province, Cambodia near the Thai–Cambodian border (Somasundaram, van de Put, Eisenbruch & de Jong, 1999). The HPRT and TPO clinics use an integrated Khmer approach to the care of mentally ill patients in a primary health care setting. This approach integrates Khmer traditional healing, traditional Khmer-style of non-intrusive compassionate counselling, Buddhist spirituality, herbal healing and western psychotropic medication (Lavelle et al., 1996). At HPRT’s clinic, community-based mental health care is integrated into a primary health care setting using only Khmer staff who utilize both Khmer folk and western DSM-IV diagnoses. The local success of these clinics run by HPRT and TPO has made them centres of expertise for the country.
Currently, only a small fraction of Cambodian citizens have access to mental health care (Belford, 2010; Kingdom of Cambodia, NRK, 2004; Prince et al., 2007; Stockwell, Whiteford, Townsend & Stewart, 2005). The high percentage of those in the survey in Siem Reap with trauma-related health problems is also of serious concern. Self-reported health status is an individual and subjective concept that is related to the strongest biological indicator, death (Jylha, 2009). Our results demonstrate that there is good reason to unite the concepts of mental health and health in post-conflict settings in clinical and public health responses even years after the most severe period of historical violence. Our findings of high levels of health and mental health problems in the Siem Reap province lead us to conclude that 25 years after the Pol Pot genocide, the community is still experiencing significant physical and emotional suffering that needs to be addressed by Cambodia’s emerging primary health care system (WHO, 1994).
Limitations
In interpreting the findings reported herein it is important to note that the cross-sectional design of the two surveys precludes the attribution of causal determinations. There are many socio-economic and cultural factors in each of the communities surveyed that were not studied and may account partially for the differences in health and mental health status. The path analysis and the general linear models should be viewed cautiously as only identifying associations between trauma, depression, PTSD, health and functional status. We felt that this exercise was valuable in our attempt to understand the ‘complex’ relationships between the two groups. Because PTSD and depression were measured with a self-report checklist rather than a diagnostic interview, the prevalence figures based on an established cut-off point measure reveal ‘probable’ PTSD and depression, respectively (Mollica, McDonald, Massagli & Silove, 2006). Yet, as part of our study design, in order to enhance data analysis we were most interested in analysing our results on a continuous scale as compared with a binary categorical diagnosis. Also, our results do not support the view that the mental health symptoms of depression and PTSD reported by the Siem Reap respondents are an artefact of being Khmer; if they were, similar findings would have been documented among Khmer surveyed in Surin, Thailand. Symptoms comprise an illness if they have an enduring presence, a relationship to health and disability, and are severe (Kroenke, 2001). These criteria for illness were well established in our study. Higher symptom/trauma levels related to age suggest the long duration of PTSD in this study sample. Since the measurement of severity relies totally upon the respondents’ self-report, we purposely used a validated PTSD scale and set the cut-off point at a level consistent with a Cambodian patient in treatment for PTSD in a specialized US clinic and in our clinic in Siem Reap, Cambodia. This cut-off of 2.5 avoids the over-inclusiveness of a DSM-IV diagnosis of PTSD (Mollica et al., 1992). Critics of PTSD, however, may be correct: that lower symptom levels of PTSD may be a well-tolerated phenomenon and should not be over-medicalized and given a western diagnosis; however, this reality still needs to be determined (Kienzler, 2008).
While our research and field experience indicate ethnic and cultural similarities between the Khmer living in Siem Reap and those who live in Surin, there may be cultural or environmental factors influencing our survey results that have not been considered in our analyses. One potential limitation is the six-year gap between the collection of survey data. The HPRT team was directly affected by the coup in Cambodia in 1997 in which it became impossible to collect the planned survey in Siem Reap province due to unsafe conditions and lack of government support. Once stability was restored, HPRT, with the support of the US Centers for Disease Control and Prevention (CDC) (Cardozo et al., 2012), was able to continue this research in Cambodia. A survey in 1998 in Cambodia might have revealed higher levels of PTSD and depression than in 2004, when political stability had returned to Cambodia. Surin’s improving economic conditions might have also widened the prevalence gap. Notwithstanding such differences, this study is the first that has been able to compare a culturally similar population with and without exposure to extreme violence.
Additionally, historical memories of events that occurred 25 years ago may not be completely accurate, although the events of extreme violence tend not to be readily forgotten (Woolcock, 2001). In fact, research is demonstrating that trauma events associated with high arousal are remembered and are integrated into one’s personality, especially in those with PTSD (Berntsen and Rubin, 2006; Bradley, Greenwald, Petry & Lang, 1992). The self-reported health problems in a resource-poor primary health care setting may be inaccurate. Certainly the latter may represent an under-reporting of diagnosable illness. Amartya Sen (2002) has warned of the possibility that very poor, uneducated communities may underestimate their self-perception of health status. The accessibility of primary health care service and traditional healing were not sufficiently studied here and will be included in the next community survey (Koch-Weser et al., 2004). In addition, data on informal work activities, including self-employment, family farming and employment, and vocational and technical training were extensively collected and will be presented in another manuscript (Woolcock, 2001).
Conclusion
The degree of suffering in Cambodia associated with past and current severe traumatic life events is enormous and is in need of a rational and effective public health approach. Our results strongly provide support for the Cambodian Ministry of Health to invest in mental health services in primary health care in Cambodia. Our survey is an important step in documenting the mental health needs of a post-conflict society. Future population-based research in Cambodia should include: (1) evaluation of the ways in which Cambodians think about their health and mental health and the factors that govern their choice of traditional and/or western treatment; (2) assessment of the impact of depression and PTSD on major health problems, such as diabetes, heart disease, malaria, and HIV/AIDS; and (3) determination of the relative cultural appropriateness and effectiveness of traditional and western treatment for mental health problems.
Acknowledgements
Dr Mollica and Dr Brooks acknowledge that they had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. The authors would also like to acknowledge the following individuals for their contributions to this paper: Laura MacDonald, PhD, who helped conduct the survey; Curtis Blanton, MS, who reviewed the manuscript; Shin Daimyo, MPH, who prepared and reviewed the manuscript and reviewed the data analysis; Zachary Steele, PhD, who assisted with the data analysis; Supang Chantavanich, PhD, who helped conduct the survey in Surin, Thailand; and the HPRT Khmer Team living and working in Siem Reap City.
Funding
This project was partially funded by the Nippon Foundation and the Centers for Disease Control and Prevention.
Footnotes
The authors of this paper declare no conflicts of interest and no financial interests.
References
- APA (American Psychological Association) Diagnostic and statistical manual of mental disorders version IV (DSM-IV) APA; Washington, DC: 1994. [Google Scholar]
- Barrett P. Structural equation modeling: Adjudging model fit. Personality and Individual Differences. 2007;42:815–824. [Google Scholar]
- Belford A. Cambodia’s mental health crisis gets little attention and money. The Cambodia Daily. 2010:14. [Google Scholar]
- Berntsen D, Rubin DC. When a trauma becomes a key to identity: Enhanced integration of trauma memories predicts posttraumatic stress disorder symptoms. Applied Cognitive Psychology. 2006;21:417–431. [Google Scholar]
- Bolton P, Neugebauer R, Ndongoni L. Prevalence of depression in rural Rwanda based on symptom and functional criteria. Journal of Nervous Mental Disorders. 2002;190:631–637. doi: 10.1097/00005053-200209000-00009. [DOI] [PubMed] [Google Scholar]
- Bradley MM, Greenwald MK, Petry MC, Lang PJ. Remembering pictures: Pleasure and arousal in memory. Journal of Experimental Psychology Learning Memory and Cognition. 1992;18:378–390. doi: 10.1037//0278-7393.18.2.379. [DOI] [PubMed] [Google Scholar]
- Bramsen I, van der Ploeg HM. Fifty years later: The long-term psychological adjustment of ageing World War II survivors. Acta Psychiatrica Scandinavica. 1999;100:350–358. doi: 10.1111/j.1600-0447.1999.tb10878.x. [DOI] [PubMed] [Google Scholar]
- Browne M, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. SAGE; Newbury Park, CA: 1993. pp. 136–162. [Google Scholar]
- Cardozo BL, Blanton C, Zalewski T, Tor S, McDonald L, Lavelle J, Mollica R. Mental health survey among landmine survivors in Siem Reap province, Cambodia. Medicine, Survival and Conflict. 2012;28:161–181. doi: 10.1080/13623699.2012.678087. [DOI] [PubMed] [Google Scholar]
- Cardozo BL, Vergara A, Agani F, Gotway CA. Mental health, social functioning, and attitudes of Kosovar Albanians following the war in Kosovo. Journal of the American Medical Association. 2000;284:569–577. doi: 10.1001/jama.284.5.569. [DOI] [PubMed] [Google Scholar]
- Chung RC, Kagawa-Singer M. Predictors of psychological distress among South-East Asian refugees. Social Science and Medicine. 1993;36:631–639. doi: 10.1016/0277-9536(93)90060-h. [DOI] [PubMed] [Google Scholar]
- de Jong JT, Komproe IH, van Ommeren M. Common mental disorders in post-conflict settings. The Lancet. 2003;361:2128–2130. doi: 10.1016/S0140-6736(03)13692-6. [DOI] [PubMed] [Google Scholar]
- de Jong JT, Komproe IH, van Ommeren M, El Masri M, Araya M, Khaled N, Somasundaram D. Lifetime events and posttraumatic stress disorder in 4 postconflict settings. Journal of the American Medical Association. 2001;286:555–562. doi: 10.1001/jama.286.5.555. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BS, Dohrenwend BP. Life stress and psychopathology. In: Regier DA, Allen G, editors. Risk factor research in the Major Mental Disorders National Institute of Mental Health. US Government Printing Office; Washington, DC: 1981a. pp. 131–141. [Google Scholar]
- Dohrenwend BS, Dohrenwend BP. Socioenvironmental factors, stress, and psychopathology – part 2: Hypotheses about stress processes linking social class to various types of psychopathology. American Journal of Community Psychology. 1981b;9:146–159. [Google Scholar]
- Dohrenwend BS, Dohrenwend BP. Life stress and illness: Formulation of the issues. In: Snell B, Dohrenwend BS, Dohrenwend BP, editors. Stressful life events and their contexts. Neal Watson Academic Publication; New York: 1983. pp. 1–27. [Google Scholar]
- Dubois V, Tonglet R, Hoyois P, Sunbaunat K, Roussaux J, Hauff E. Household survey of psychiatric morbidity in Cambodia. International Journal of Social Psychiatry. 2004;174:174–185. doi: 10.1177/0020764004043125. [DOI] [PubMed] [Google Scholar]
- Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of maltreatment and adult mental health in community respondents: Results from adverse childhood experiences study. American Journal of Psychiatry. 2003;160:1453–1460. doi: 10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Hair JR, Anderson RE, Tatham RL, Black WC. Multivariate data analysis. 5th Prentice Hall International; Upper Saddle River, NJ: 1998. [Google Scholar]
- Hayduk L, Cummings G, Boadu K, Pazderka-Robinson H, Boulianne S. Testing! Testing! One, two, three: Testing the theory in structural equation models. Personality and Individual Differences. 2007;42:841–850. [Google Scholar]
- Helzer JE, Robins LN, McEvoy L. Post-traumatic stress disorder in the general population. New England Journal of Medicine. 1987;317:1630–1634. doi: 10.1056/NEJM198712243172604. [DOI] [PubMed] [Google Scholar]
- Jylha M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Social Science and Medicine. 2009;69:307–316. doi: 10.1016/j.socscimed.2009.05.013. [DOI] [PubMed] [Google Scholar]
- Kagee A. Symptoms of distress and posttraumatic stress among South African former political detainees. Ethnicity and Health. 2005;10:169–179. doi: 10.1080/13557850500071244. [DOI] [PubMed] [Google Scholar]
- Karam EG, Mneimneh ZN, Karam AN, Fayyad JA, Nasser SC, Chatterji S, Kessler RC. Prevalence and treatment of mental disorders in Lebanon: A national epidemiological survey. The Lancet. 2006;367:1000–1006. doi: 10.1016/S0140-6736(06)68427-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DMS-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005a;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005b;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the national comorbidity survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kienzler H. Debating war-trauma and post traumatic stress disorder in an interdisciplinary arena. Social Science and Medicine. 2008;67:218–227. doi: 10.1016/j.socscimed.2008.03.030. [DOI] [PubMed] [Google Scholar]
- Kingdom of Cambodia, NRK . Ministry of Health, National Program for Mental Health. Ten Year Mental Health Development in Cambodia. Cambodian Ministry of Health; Phnom Pen: 2004. [Google Scholar]
- Kleijn WC, Hovens JE, Rodenburg JJ. Post-traumatic stress symptoms in refugees: Assessments with the Harvard Trauma Questionnaire and the Hopkins Symptom Checklist-25 in different languages. Psychological Reports. 2001;88:527–532. doi: 10.2466/pr0.2001.88.2.527. [DOI] [PubMed] [Google Scholar]
- Kleinman A. Patients and healers in the context of culture. University of California Press; Berkeley, CA: 1980. [Google Scholar]
- Kleinman A. Anthropology and psychiatry: The role of culture in cross-cultural research on illness. British Journal of Psychiatry. 1987;151:447–454. doi: 10.1192/bjp.151.4.447. [DOI] [PubMed] [Google Scholar]
- Kline R. Principles and practice of structural equation modeling. 2nd The Guilford Press; New York: 2005. [Google Scholar]
- Koch-Weser S, Grigg-Saito D, Liang S, Toof R, Kreth NN, Pot M, Giles W. Health status of Cambodians and Vietnamese: Selected communities, United States, 2001–2002. Journal of the American Medical Association. 2004;292:2208–2209. [Google Scholar]
- Kroenke K. Studying symptoms: Sampling and measurement issues. Annals of Internal Medicine. 2001;134:844–853. doi: 10.7326/0003-4819-134-9_part_2-200105011-00008. [DOI] [PubMed] [Google Scholar]
- Lavelle J, Tor S, Mollica RF, Allden K, Potts L. Harvard guide to Khmer mental health. Harvard Program in Refugee Trauma; Cambridge, MA: 1996. [Google Scholar]
- Marshall GN, Schell TL, Elliott MN, Berthold SM, Chun CA. Mental health of Cambodian refugees two decades after resettlement in the United States. Journal of the American Medical Association. 2005;294:571–579. doi: 10.1001/jama.294.5.571. [DOI] [PubMed] [Google Scholar]
- Mollica RF, Cardozo BL, Osofsky HJ, Raphael B, Ager A, Salama P. Mental health in complex emergencies. The Lancet. 2004;364:2058–2067. doi: 10.1016/S0140-6736(04)17519-3. [DOI] [PubMed] [Google Scholar]
- Mollica RF, Caridad KR, Massagli MP. Longitudinal study of posttraumatic stress disorder, depression, and changes in traumatic memories over time in Bosnian refugees. Journal of Nervous Mental Disorders. 2007;195:572–579. doi: 10.1097/NMD.0b013e318093ed2c. [DOI] [PubMed] [Google Scholar]
- Mollica RF, Caspi-Yavin Y, Bollini P, Truong T, Tor S, Lavelle J. The Harvard Trauma Questionnaire: Validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in Indochinese refugees. Journal of Nervous Mental Disorders. 1992;180:111–116. [PubMed] [Google Scholar]
- Mollica RF, Donelan K, Tor S, Lavelle J, Elias C, Frankel M, Blendon RJ. The effect of trauma and confinement on functional health and mental health status of Cambodians living in Thailand–Cambodia border camps. Journal of the American Medical Association. 1993;270:581–586. [PubMed] [Google Scholar]
- Mollica RF, McDonald LS, Massagli MP, Silove DM. Measuring trauma measuring torture. Harvard Program in Refugee Trauma; Cambridge, MA: 2006. [Google Scholar]
- Mollica RF, McInnes K, Poole C, Tor S. Dose–effect relationships of trauma to symptoms of depression and post-traumatic stress disorder among Cambodian survivors of mass violence. British Journal of Psychiatry. 1998;173:482–488. doi: 10.1192/bjp.173.6.482. [DOI] [PubMed] [Google Scholar]
- Mollica RF, McInnes K, Sarajlic N, Lavelle J, Sarajlic I, Massagli MP. Disability associated with psychiatric comorbidity and health status in Bosnian refugees living in Croatia. Journal of the American Medical Association. 1999;282:433–439. doi: 10.1001/jama.282.5.433. [DOI] [PubMed] [Google Scholar]
- Mollica RF, Sarajlic N, Chernoff M, Lavelle J, Vukovic IS, Massagli MP. Longitudinal study of psychiatric symptoms, disability, mortality, and emigration among Bosnian refugees. Journal of the American Medical Association. 2001;286:546–554. doi: 10.1001/jama.286.5.546. [DOI] [PubMed] [Google Scholar]
- Mollica RF, Wyshak G, de Marneffe D, Khuon F, Lavelle J. Indochinese versions of the Hopkins Symptom Checklist-25: A screening instrument for the psychiatric care of refugees. American Journal of Psychiatry. 1987;144:497–500. doi: 10.1176/ajp.144.4.497. [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO. Mplus user’s guide. 6th Muthén & Muthén; Los Angeles, CA: 1998–2008. [Google Scholar]
- Olff M, Langeland W, Draijer V, Gersons BPR. Gender differences in posttraumatic stress disorder. Psychological Bulletin. 2007;133:183–204. doi: 10.1037/0033-2909.133.2.183. [DOI] [PubMed] [Google Scholar]
- Oruc L, Kapetanovic A, Pojskic N, Miley K, Forstbauer S, Mollica RF, Henderson DC. Screening for PTSD and depression in Bosnia and Herzegovina: Validating the Harvard Trauma Questionnaire and the Hopkins Symptom Checklist. International Journal of Culture and Mental Health. 2008;1:105–116. [Google Scholar]
- Palmieri P, Marshall GN, Schnell TL. Confirmatory factor analysis of posttraumatic stress symptoms in Cambodian refugees. Journal of Traumatic Stress. 2007;20:207–216. doi: 10.1002/jts.20196. [DOI] [PubMed] [Google Scholar]
- Pham PN, Weinstein HM, Longman T. Trauma and PTSD symptoms in Rwanda: Implications for attitudes toward justice and reconciliation. Journal of the American Medical Association. 2004;292:602–612. doi: 10.1001/jama.292.5.602. [DOI] [PubMed] [Google Scholar]
- Priebe S, Bogic M, Ajdukovic D, Franciskovic T, Galeazzi GM, Kucukalic A, Schützwohl M. Mental disorders following war in the Balkans: A study in 5 countries. Archives of General Psychiatry. 2010;67:518–528. doi: 10.1001/archgenpsychiatry.2010.37. [DOI] [PubMed] [Google Scholar]
- Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, Rahman A. No health without mental health. The Lancet. 2007;370:859–877. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- Rasbash J, Steele F, William Browne W, Prosser B. A user’s guide to MLwiN version 2.0. University of Bristol, Centre for Multilevel Modelling; Bristol: 2005. [Google Scholar]
- Rasmussen OV. Medical aspects of torture. Danish Medical Bulletin. 1990;37(Suppl 1):1–88. [PubMed] [Google Scholar]
- Sareen J, Cox B, Stein M, Afifi T, Fleet C, Asmundson G. Physical and mental comorbidity, disability, and suicidal behavior associated with posttraumatic stress disorder in a large community sample. Psychosomatic Medicine. 2007;69:242–248. doi: 10.1097/PSY.0b013e31803146d8. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Green BL, editors. Trauma and health physical health consequences of exposure to extreme stress. Washington, DC: 2004. [Google Scholar]
- Sen A. Health: Perception vs observation. British Medical Journal. 2002;324:860–861. doi: 10.1136/bmj.324.7342.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrestha NM, Sharma B, van Ommeren M, Regmi S, Makaju R, Komproe I, de Jong JT. Impact of torture on refugees displaced within the developing world: Symptomatology among Bhutanese refugees in Nepal. Journal of the American Medical Assocation. 1998;280:443–448. doi: 10.1001/jama.280.5.443. [DOI] [PubMed] [Google Scholar]
- Silove D, Bateman CR, Brooks RT, Fonseca CZ, Steel Z, Rodger J, Buman A. Estimating clinically relevant mental disorders in a rural and an urban setting in postconflict Timor-Leste. Archives of General Psychiatry. 2008;65:1205–1212. doi: 10.1001/archpsyc.65.10.1205. [DOI] [PubMed] [Google Scholar]
- Silove D, Manicavasagar V, Mollica R, Thai M, Khiek D, Lavelle J, Tor S. Screening for depression and PTSD in a Cambodian population unaffected by war: Comparing the Hopkins Symptom Checklist and Harvard Trauma Questionnaire with the structured clinical interview. Journal of Nervous Mental Disorders. 2007;195:152–157. doi: 10.1097/01.nmd.0000254747.03333.70. [DOI] [PubMed] [Google Scholar]
- Sledjeski EM, Speisman B, Dierker L. Does number of lifetime traumas explain the relationship between PTSD and chronic medical conditions? Answers from the National Comorbidity Survey-Replication (NCS-R) Journal of Behavioral Medicine. 2008;31:341–349. doi: 10.1007/s10865-008-9158-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith Fawzi MC, Murphy E, Pham T, Lin L, Poole C, Mollica RF. The validity of screening for post-traumatic stress disorder and major depression among Vietnamese former political prisoners. Acta Psychiatrica Scandinavica. 1997;95:87–93. doi: 10.1111/j.1600-0447.1997.tb00379.x. [DOI] [PubMed] [Google Scholar]
- Somasundaram D, van de Put W, Eisenbruch M, de Jong J. Starting mental health services in Cambodia. Social Science and Medicine. 1999;48:1029–1046. doi: 10.1016/s0277-9536(98)00415-8. [DOI] [PubMed] [Google Scholar]
- Sonis J, Gibson J, de Jong J, Field N, Hean S, Komproe I. Probable posttraumatic stress disorder and disability in Cambodia: Associations with perceived justice, desire for revenge, and attitudes towards the Khymer Rouge trials. Journal of the American Medical Association. 2009;302:527–536. doi: 10.1001/jama.2009.1085. [DOI] [PubMed] [Google Scholar]
- SPSS . SPSS for windows, rel. 17.0. SPSS; Chicago, IL: 2008. [Google Scholar]
- Steel Z, Chey T, Silove D, Marnane C, Bryant RA, van Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: A systematic review and meta-analysis. Journal of the American Medical Association. 2009;302:537–549. doi: 10.1001/jama.2009.1132. [DOI] [PubMed] [Google Scholar]
- Steel Z, Silove D, Phan T, Bauman A. Long-term effect of psychological trauma on the mental health of Vietnamese refugees resettled in Australia: A population-based study. The Lancet. 2002;360:1056–1062. doi: 10.1016/S0140-6736(02)11142-1. [DOI] [PubMed] [Google Scholar]
- Stewart AL, Hays RD, Ware JE., Jr. The MOS short-form general health survey: Reliability and validity in a patient population. Medical Care. 1988;26:724–735. doi: 10.1097/00005650-198807000-00007. [DOI] [PubMed] [Google Scholar]
- Stockwell A, Whiteford H, Townsend C, Stewart D. Mental health policy development: Case study of Cambodia. Australasian Psychiatry. 2005;13:190–194. doi: 10.1080/j.1440-1665.2005.02187.x. [DOI] [PubMed] [Google Scholar]
- Summerfield D. A critique of seven assumptions behind psychological trauma programmes in war-affected areas. Social Science & Medicine. 1999;48:1449–1462. doi: 10.1016/s0277-9536(98)00450-x. [DOI] [PubMed] [Google Scholar]
- van Ommeren M, Sharma B, de Jong J. Culture, trauma, and psychotrauma programmes. The Lancet. 1997;350:595. doi: 10.1016/S0140-6736(05)63188-1. [DOI] [PubMed] [Google Scholar]
- Weiss MG, Saraceno B, Saxena S, van Ommeren M. Mental health in the aftermath of disasters: Consensus and controversy. Journal of Nervous and Mental Disease. 2003;191:611–615. doi: 10.1097/01.nmd.0000087188.96516.a3. [DOI] [PubMed] [Google Scholar]
- WHO (World Health Organization) The introduction of a mental health component into primary health care. WHO; Geneva: 1990. [Google Scholar]
- WHO (World Health Organization) Primary health care concepts and challenges in a changing world: Alma Ata revisited. SHS paper no. 7. WHO; Geneva: 1994. [Google Scholar]
- Woolcock M. Microenterprise and social capital: A framework for theory, research, and policy. The Journal of Socio-Economics. 2001;30:193–198. [Google Scholar]