Abstract
Grief over the loss of a family member may cause physical and mental illness, but an association between bereavement and cancer risk has not been established. Based on the Swedish National Cervical Screening Register (1969–2011) including 14,011,269 smears from 2,466,107 women, we conducted two nested case-control studies to examine the associations of bereavement (i.e., loss of a family member due to death) with abnormal cytology (390,310 first abnormal and 1,951,319 normal smears) and in situ/invasive cervical cancer (75,128 case and 375,640 control women), both individually matched on year of birth and screening adherence. Among 1,696 of the control women, we further investigated bereavement in association with HPV infection, both HPV16 and other HPV types. Bereavement was consistently associated with a 4–9% increased risk for first abnormal cytology, in situ and invasive cervical cancer (all P<0.02). The associations became stronger when multiple losses, loss of child, sibling or spouse, and loss due to unnatural cause were analyzed separately (P for trend or difference<0.0001), and for women with high screening adherence (P for difference<0.05). Among 1,696 women who had not developed cervical cancer, we further investigated the link between bereavement and HPV infection. Bereavement was associated with a 62% increased risk of HPV16 infection, high viral load, and recurrent infection, and was also more strongly associated with HPV infections designated as high-risk compared to low-risk determinants of cervical carcinogenesis. Collectively, our findings demonstrate that bereavement is associated with an increased risk of developing cervical cancer. Further, they suggest that this association may be attributed to stress-induced oncogenic HPV infections.
Keywords: bereavement, human papillomavirus, cervical dysplasia, cervical cancer, stress
INTRODUCTION
Bereavement is known to induce excess ill-health, in terms of both physical and mental illnesses (1). Whether or not bereavement is also associated with an increased risk of cancer is debated. Compared to several other cancer types, the literature on cervical cancer is, in this context, limited and conflicting. Two studies demonstrated an increased risk of invasive cervical cancer (ICC) after the loss of a close relative (2,3), whereas another three showed no association between bereavement and ICC (4–6). Similarly, some (7,8), but not all (9–12), earlier studies have suggested a link between psychological stress and cervical intraepithelial neoplasia (CIN). Although the accumulated evidence from human studies remains inconclusive, compromised immunosurveillance and overexpression of viral oncogenes resulting from stress-induced neuroendocrine dysregulation have been proposed as plausible biological mechanisms underlying the association between psychological stress and cervical carcinogenesis.
Oncogenic types of the human papillomavirus (HPV) have been established as necessary but not sufficient causes in cervical carcinogenesis (13). Most women who contract HPV develop neither persistent infection nor cervical neoplasia, and it is unclear which factors modulate the individual likelihood of malignant transformation after a primary contact (14). We hypothesized that exposure to severely stressful life events may increase host vulnerability to oncogenic HPV infections and subsequently cervical neoplasia. To this end, we used nationwide registers of cervical screening and cancer in Sweden to investigate the potential contribution of bereavement throughout the disease course of ICC, from a first cytologically abnormal smear, to cervical dysplasia and eventually to cervical cancer. We further leveraged two population-based studies with rich information on HPV infection to examine whether a causal link might be further corroborated by enhanced HPV infection following the bereavement.
METHODS
Study Base
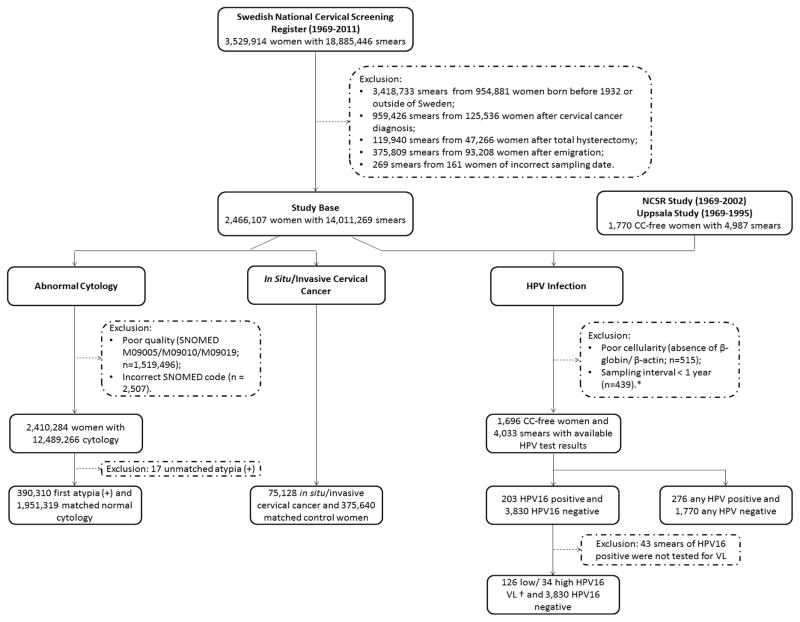
The Swedish National Cervical Screening Register (NKCx) has since 1967 collected information on all cervical Papanicolaou smears in Sweden, through both the national screening program and opportunistic screening (nationwide since 1995) (15). In the present study, we included all women born in Sweden since 1932 onward with at least one smear recorded in the NKCx during 1969–2011 (n=2,466,107) (Figure 1).
Figure 1. A Flow Chart Describing the Study Base and Three Analyses on Abnormal Cytology, Cervical Cancer and HPV Infection.
Note: CC, cervical cancer; HPV, Human papillomavirus; NCSR, National Cervical Screening Register; VL, viral load; SNOMED, the diagnostic codes used by Swedish Association for Clinical Cytology.
* Among consecutive smears with a sampling interval of less than one year, only the first smear was included, assuming that the following smears within the one-year time window were more likely diagnostic smears and not independent from the first smear.
† We classified 160 HPV16 positive smears as high or low viral load infection based on the median viral load values. Due to a batch effect observed in the NCSR Study, cut-off values were calculated both per sampling period (1969–1984/1985–1989/1990–1994/1995–2005) and per test period (2005–2007/2008–2009).
Using the individually unique national registration numbers, we followed all women through cross-linkages to the Swedish Cancer, Patient, Cause of Death and Migration Registers. The Cancer Register is available since 1958 and is essentially 100% complete. The Patient Register collects hospital discharge records in Sweden from 1964/1965, including 60% of the entire country in 1969, 85% in 1983, and 100% since 1987. All women were followed from January 1, 1969 or birth, whichever occurred later, to a first diagnosis of in situ/invasive cervical cancer (through the Cancer Register), total hysterectomy (through the Patient Register), death, emigration, or December 31, 2011, whichever came first. During follow-up (median: 43 years), we identified in total 14,011,269 smears among the participating women (Figure 1).
Organized cervical screening was first implemented in Sweden in the 1960s (16). Initially, women at 30–49 years of age (later 25–49) were invited to screening every 3–4 years; since 1998, women at 23–50 and 51–60 years of age have been invited every three and five years respectively (16). We defined degree of screening participation as the accumulated years of participation divided by the sum of years scheduled for screening, until the first recorded abnormal smear (16). Screening adherence was accordingly classified into five levels, including the quartiles of the calculated degree of participation and “unscreened” (i.e., with only opportunistic smears during the study period).
We conducted three analyses to assess separately the associations of bereavement with first abnormal cytology, in situ/invasive cervical cancer, and HPV infection (Figure 1).
Study Design
Abnormal cytology
We defined a smear as “abnormal” if any abnormal cytology was diagnosed, including atypical (i.e., atypical squamous cells of undetermined significance or atypical glandular cells), low-grade (i.e., low-grade squamous intraepithelial lesion or koilocytosis), and high-grade (i.e., high-grade squamous intraepithelial lesion or worse) abnormalities. We used the first abnormal smear during follow-up of each woman as the case smear, and accordingly the follow-up was censored at the first smear of abnormal cytology. Using incidence density sampling, we individually matched each case smear with five cytologically normal smears from other women on year of birth and screening adherence. We identified 390,310 first abnormal and 1,951,319 control smears for this analysis (Figure 1 and Supplementary Table S1).
In situ and invasive cervical cancer
During follow-up, we identified 69,674 and 5,454 cases of histopathologically confirmed in situ and invasive cervical cancer of any histological type, respectively (Figure 1 and Supplementary Table S1). In situ cancer included both carcinoma in situ (equivalent to CIN3 in the Cancer Register) and adenocarcinoma in situ. Women who developed invasive cancer from in situ cancer (N=300) were only included in the analysis of in situ cancer since the follow-up was censored at the time of the first event of cervical cancer. Using incidence density sampling, we individually matched each case woman with five women without any cervical cancer (n=375,640), on year of birth and screening adherence. All cases were classified by histological type: squamous cell, glandular cell, or other origin. ICC cases were further classified by mode of detection (i.e., screening detected cancer, interval cancer, and screening-overdue or unscreened cancer).
HPV infection
For this analysis, we used data from two earlier population-based studies, the National Cervical Screening Register (NCSR) Study (17,18) and the Uppsala Study (19), which had a primary aim of assessing the impact of HPV infection on the risk of cervical cancer. While the NCSR Study enrolled 1,360 cases (both in situ and invasive cervical cancer) and 1,360 controls from six Swedish counties during 1969–2002, the Uppsala Study enrolled 478 cases of carcinoma in situ and 608 controls from Uppsala County during 1969–1995. All available smears taken before the diagnosis of case women in each case-control pair were retrieved and tested for HPV infection (17,19). For our analysis, we only included smears from the control women, aiming to investigate the association between bereavement and HPV infection in a population at risk for cervical cancer.
Since the control women of both the NCSR Study and the Uppsala Study were randomly selected from women participating in cervical screening in these different counties during the respective study periods, these control women existed also in the NKCx. We first excluded smears not identifiable in our study base, leaving 4,987 smears from 1,770 women in the analysis (Figure 1). Smears with poor cellularity were also excluded (n=515). Among consecutive smears with a sampling interval of <1 year, only the first smear was included, assuming that the following smears within one year were likely diagnostic smears and not independent from the first smear (n=439). Finally, we included 1,696 women with 4,033 smears tested for HPV16 (including 203 HPV16 positive and 3,830 HPV16 negative smears) for the analysis of HPV16 infection. A total of 160 positive smears were also measured for HPV16 viral load (17,19) and were further classified as high or low viral load levels (20). All HPV16 positive smears were used as the case smears, whereas all HPV16 negative smears as the control smears (Supplementary Table S1).
Besides HPV16, 2,046 of 2,464 (83%) smears from the control women of the NCSR Study were tested for another 15 high-risk and six low-risk HPV types (Figure 1). Smears with a positive finding of any HPV types tested served as the case smears whereas the smears negative on all HPV types served as control smears in this analysis. We additionally analyzed bereavement in association with infection of high- and low-risk HPV types separately. Smears with a positive finding of any low-risk or high-risk HPV types tested served as the case smears for the analyses of low-risk and high-risk HPV infections respectively, whereas smears with a positive finding of both low-risk and high-risk HPV types contributed to both analyses.
Bereavement
We identified immediate family members including children, spouse, siblings and parents for all participating women from the Swedish Multi-Generation Register. This register contains largely complete familial linkages for all Swedish residents born in 1932 onward (21), which allowed us to identify mother for 97% and father for 95% of these women. We were also able to identify children for 1,850,858 (75.7%), siblings for 2,185,164 (89.3%), and spouse for 1,917,286 (78.4%) of all participating women. Spouses were defined through a registered common biological child. Bereavement, defined as the death of a family member, was ascertained through linking all family members to the Cause of Death Register during 1961–2011. We defined the exposure as bereavement before reference date, i.e., the date of diagnosis for the analysis on in situ/invasive cervical cancer and the date of smear for other analyses.
Bereavement was first categorized as loss of parent or loss of a child, spouse, or sibling, and further as due to unnatural (i.e., self-inflicted or other injuries) or natural cause of death. Time since bereavement was defined by the interval between date of loss and the reference date (≤1 year, 2–4 years, or ≥5 years).
Lifestyle factors
To evaluate the potential impact of lifestyle factors on the studied associations, we compared the distributions of smoking, sexual behavior, oral contraceptive use, parity, and abortion between women with and without bereavement. This analysis was performed among 345 of the control women in the Uppsala Study, for whom detailed questionnaire data were available (22).
Statistical Analyses
We used odds ratios (ORs) with 95% confidence intervals (CIs) estimated from conditional logistic regression to investigate the association between bereavement and first abnormal cytology. We further stratified the analyses by screening adherence (high, low, or unscreened). High adherence was defined if the degree of participation was above, whereas low adherence if below, the median value of all screened women. To assess whether the association of bereavement with abnormal cytology might be driven by prevalent but yet undiagnosed cervical cancer, in a sensitivity analysis, we excluded all abnormal smears with a subsequent diagnosis of in situ/invasive cervical cancer during the following six months.
We used conditional logistic regression to estimate the association of bereavement with in situ/invasive cervical cancer. Additional analyses were performed by cancer histology for all cases, and by mode of detection for ICC. To assess a potential modifying effect of age on the associations (2,3), we further plotted ORs by age at reference date using locally weighted scatter-plot smoothing (23).
We used logistic regression to estimate the ORs of HPV16 infection and multinomial logistic regression to estimate the relative risk ratios (RRRs) of HPV16 viral load levels. To specifically assess the role of bereavement on recurrent HPV infection, we stratified the analyses by the HPV16 status of the preceding smears for both the case and control smears. To further assess the robustness of our findings, we also stratified the analysis by study (the NCSR Study and the Uppsala Study). Finally, we used logistic regression to assess the associations of bereavement with infection of high-risk and low-risk HPV types separately. All analyses were adjusted for age at smear, and accounted for within-subject correlations using robust variance estimates. Analyses were performed using SAS 9.3 (SAS Institute) and STATA 13.1 (StataCorp LP). The study was approved by the Regional Ethical Review Board in Stockholm.
RESULTS
Abnormal Cytology
Bereavement was associated with a slightly but significantly increased risk of first abnormal cytology (P<0.0001), with a clear dose-response relationship by number of bereavements (Table 1). The association was particularly strong for loss of a child, spouse, or sibling and loss due to unnatural causes. Time since bereavement did not modify the association. A stronger association was observed among women with high screening adherence.
Table 1.
Bereavement and Abnormal Cytology, a Nested Case-Control Study in Sweden, 1969–2011
| Characteristics | Smear with Normal Cytology; N (%) | Smear with Abnormal Cytology; N (%) | OR (95% CI)* |
|---|---|---|---|
| No bereavement | 1,389,548 (71.2) | 275,830 (70.7) | 1.0 |
| Bereavement | 561,771 (28.8) | 114,480 (29.3) | 1.04 (1.03 to 1.05) |
|
| |||
| Time since bereavement | |||
| ≤1 year | 97,087 (5.0) | 19,797 (5.1) | 1.04 (1.02 to 1.05) |
| 2–4 years | 118,769 (6.1) | 24,546 (6.3) | 1.05 (1.04 to 1.07) |
| ≥5 years | 345,915 (17.7) | 70,137 (18.0) | 1.03 (1.02 to 1.04) |
| Number of bereavements | |||
| 1 | 401,738 (20.6) | 81,260 (20.8) | 1.03 (1.02 to 1.04) |
| 2 | 136,626 (7.0) | 27,844 (7.1) | 1.05 (1.04 to 1.07) |
| 3 | 20,418 (1.1) | 4,578 (1.2) | 1.17 (1.13 to 1.21) |
| ≥4 | 2,989 (0.2) | 798 (0.2) | 1.40 (1.29 to 1.52) |
| P for trend† | <0.0001 | ||
| Type of bereavement | |||
| Loss of a parent | 474,561 (24.3) | 95,323 (24.4) | 1.02 (1.01 to 1.03) |
| Loss of a child, spouse, or sibling | 87,210 (4.5) | 19,157 (4.9) | 1.12 (1.10 to 1.14) |
| P for difference‡ | <0.0001 | ||
| Cause of bereavement | |||
| Unnatural cause | 66,224 (3.4) | 14,602 (3.7) | 1.12 (1.09 to 1.14) |
| Natural cause | 495,547 (25.4) | 99,878 (25.6) | 1.02 (1.01 to 1.03) |
| P for difference‡ | <0.0001 | ||
|
| |||
|
Stratified analysis by screening adherence
| |||
| High | |||
| No bereavement | 588,071 (76.6) | 116,343 (75.8) | 1.0 |
| Bereavement | 179,499 (23.4) | 37,173 (24.2) | 1.06 (1.04 to 1.07) |
| Low | |||
| No bereavement | 428,556 (58.1) | 85,016 (57.6) | 1.0 |
| Bereavement | 309,433 (41.9) | 62,593 (42.4) | 1.03 (1.01 to 1.04) |
| Unscreened | |||
| No bereavement | 372,921 (83.7) | 74,471 (83.5) | 1.0 |
| Bereavement | 72,839 (16.3) | 14,714 (16.5) | 1.02 (0.99 to 1.04) |
| P for difference§ | 0.002 | ||
OR, odds ratio; CI, confidence interval. The matching variables, including year of birth and screening adherence (5-level), were inherently adjusted for in all models.
Cochran-Armitage test was used to examine a potential dose-response relationship by number of bereavements.
Wald test was used to compare the ORs for different bereavement characteristics.
We added an interaction term between bereavement and screening adherence in the model, and reported the P value for the interaction term as a significance test of the difference between ORs.
Consistent associations were observed for atypical, low-grade, and high-grade abnormalities (Supplementary Table S2) and after excluding abnormal smears with potentially prevalent cervical cancer (Supplementary Table S3).
Cervical Cancer
Slightly increased risks of both in situ and invasive cervical cancer were observed among women with bereavement (P<0.0001 and P=0.0168) (Table 2). The associations were not modified by time since bereavement, but were much stronger for multiple losses, loss of a child, spouse, or sibling, and loss due to unnatural causes. The associations were also more pronounced among women with high screening adherence. While loss of a child, spouse, or sibling was consistently associated with a higher risk of in situ cervical cancer through different age spans, loss of a parent was only significantly associated with a higher risk of in situ cervical cancer at younger ages (Figure 2). Similar results were suggested for ICC (Figure 2). The association did not differ by cancer histological type or mode of detection (Supplementary Table S4).
Table 2.
Bereavement and In Situ/Invasive Cervical Cancer, a Nested Case-Control Study in Sweden, 1969–2011
| Characteristics | No Cervical Cancer | Any Cervical Cancer | in Situ Cervical Cancer | Invasive Cervical Cancer | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| N (%) | N (%) | OR (95% CI)* | N (%) | OR (95% CI)* | N (%) | OR (95% CI)* | |
| No bereavement | 267,919 (71.3) | 52,797 (70.3) | 1.0 | 49,995 (71.8) | 1.0 | 2,802 (51.4) | 1.0 |
|
| |||||||
| Bereavement | 107,721 (28.7) | 22,331 (29.7) | 1.07 (1.05 to 1.09) | 19,679 (28.2) | 1.07 (1.04 to 1.09) | 2,652 (48.6) | 1.09 (1.02 to 1.17) |
| Time since bereavement | |||||||
| ≤1 year | 18,145 (4.8) | 3,728 (5.0) | 1.06 (1.02 to 1.10) | 3,310 (4.75) | 1.05 (1.01 to 1.09) | 418 (7.7) | 1.10 (0.98 to 1.24) |
| 2–4 years | 22,629 (6.0) | 4,710 (6.3) | 1.07 (1.04 to 1.11) | 4,175 (6.0) | 1.07 (1.03 to 1.11) | 535 (9.8) | 1.10 (0.99 to 1.23) |
| ≥5 years | 66,947 (17.8) | 13,893 (18.5) | 1.07 (1.05 to 1.09) | 12,194 (17.5) | 1.07 (1.04 to 1.09) | 1,699 (31.2) | 1.08 (1.00 to 1.16) |
| Number of bereavements | |||||||
| 1 | 80,052 (21.3) | 16,414 (21.9) | 1.06 (1.03 to 1.08) | 14,823 (21.3) | 1.05 (1.03 to 1.08) | 1,591 (29.2) | 1.08 (1.00 to 1.16) |
| 2 | 23,558 (6.3) | 4,868 (6.5) | 1.09 (1.05 to 1.13) | 4,073 (5.8) | 1.09 (1.05 to 1.14) | 795 (14.6) | 1.08 (0.97 to 1.19) |
| 3 | 3,439 (0.9) | 878 (1.2) | 1.37 (1.27 to 1.49) | 678 (1.0) | 1.39 (1.27 to 1.52) | 200 (3.7) | 1.34 (1.13 to 1.60) |
| ≥4 | 672 (0.2) | 171 (0.2) | 1.40 (1.18 to 1.66) | 105 (0.2) | 1.22 (0.98 to 1.51) | 66 (1.2) | 1.83 (1.36 to 2.45) |
| P for trend† | <0.0001 | <0.0001 | 0.0001 | ||||
| Type of bereavement | |||||||
| Loss of a parent | 90,068 (24.0) | 18,203 (24.2) | 1.04 (1.02 to 1.06) | 16,106 (23.1) | 1.04 (1.02 to 1.07) | 2,097 (38.5) | 1.03 (0.96 to 1.10) |
| Loss of a child, spouse, or sibling | 17,653 (4.7) | 4,128 (5.5) | 1.20 (1.16 to 1.25) | 3,573 (5.1) | 1.18 (1.13 to 1.22) | 555 (10.2) | 1.42 (1.28 to 1.59) |
| P for difference‡ | <0.0001 | <0.0001 | <0.0001 | ||||
| Cause of bereavement | |||||||
| Unnatural cause | 13,997 (3.7) | 3,254 (4.3) | 1.19 (1.14 to 1.23) | 2,948 (4.2) | 1.17 (1.12 to 1.22) | 306 (5.6) | 1.42 (1.24 to 1.63) |
| Natural cause | 93,724 (25.0) | 19,077 (25.4) | 1.05 (1.02 to 1.07) | 16,731 (24.0) | 1.05 (1.02 to 1.07) | 2,346 (43.0) | 1.04 (0.97 to 1.12) |
| P for difference‡ | <0.0001 | <0.0001 | <0.0001 | ||||
|
| |||||||
|
Stratified analysis by screening adherence
| |||||||
| High | |||||||
| No bereavement | 109,281 (77.5) | 21,425 (76.0) | 1.0 | 20,474 (76.8) | 1.0 | 951 (61.2) | 1.0 |
| Bereavement | 31,769 (22.5) | 6,785 (24.1) | 1.11 (1.07 to 1.14) | 6,181 (23.2) | 1.10 (1.06 to 1.13) | 604 (38.8) | 1.28 (1.13 to 1.45) |
| Low | |||||||
| No bereavement | 96,282 (62.1) | 19,037 (61.4) | 1.0 | 17,661 (62.9) | 1.0 | 1,376 (46.7) | 1.0 |
| Bereavement | 58,763 (37.9) | 11,972 (38.6) | 1.04 (1.01 to 1.07) | 10,404 (37.1) | 1.04 (1.01 to 1.07) | 1,568 (53.3) | 1.01 (0.92 to 1.10) |
| Unscreened | |||||||
| No bereavement | 62,356 (78.4) | 12,335 (77.5) | 1.0 | 11,860 (79.3) | 1.0 | 475 (49.7) | 1.0 |
| Bereavement | 17,189 (21.6) | 3,574 (22.5) | 1.07 (1.02 to 1.12) | 3,094 (20.7) | 1.07 (1.02 to 1.12) | 480 (50.3) | 1.06 (0.89 to 1.27) |
| P for difference§ | 0.018 | 0.107 | 0.011 | ||||
OR, odds ratio; CI, confidence interval. The matching variables, including year of birth and screening adherence (5-level), were inherently adjusted for in all models.
Cochran-Armitage test was used to examine a potential dose-response relationship by number of bereavements.
Wald test was used to compare the ORs for different bereavement characteristics.
We added an interaction term between bereavement and screening adherence in the model, and reported the P value for the interaction term as a significance test of the difference between ORs.
Figure 2. Odds Ratios of In Situ and Invasive Cervical Cancer among Women with Previous Bereavement, Compared to Women without Bereavement, Stratified by Age at Cancer Diagnosis.
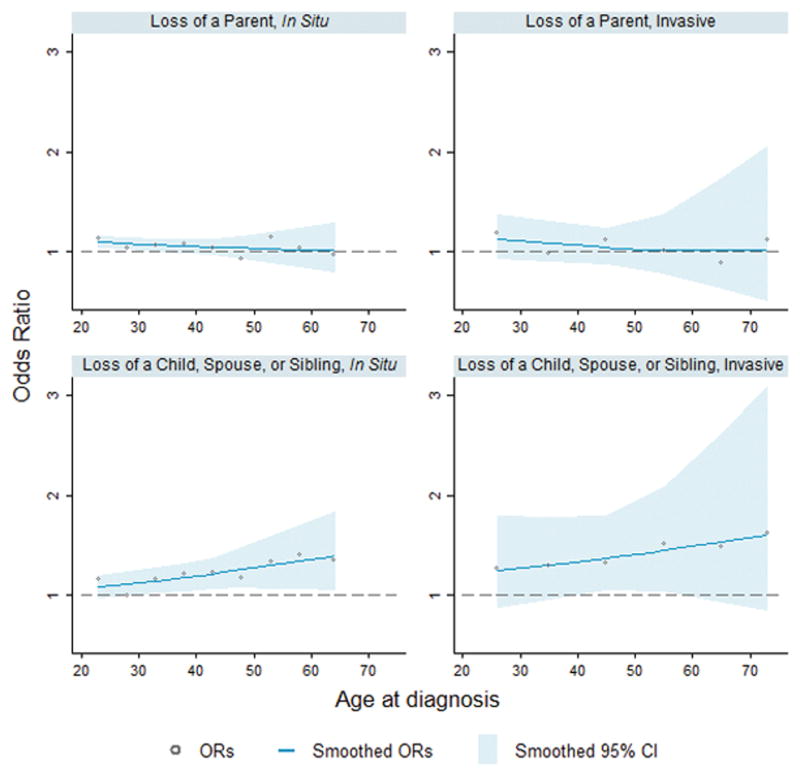
Note: Analyses on in situ cervical cancer were stratified by 5-year age groups (≤25, 26–30, 31–35, 36–40, 41–45, 46–50, 51–55, 56–60, and ≥61 years). Analyses on invasive cervical cancers were stratified by 10-year age groups (≤30, 31–40, 41–50, 51–60, 61–70, and ≥71 years). We plotted the scatters of odds ratios (ORs) at the median age of each age group. ORs and 95% confidence intervals (CIs) were fitted by locally weighted scatterplot smoothing.
HPV Infection
We observed a 62% increased risk of HPV16 infection among bereaved women (95% CI 1.05 to 2.50) (Table 3). The association was driven by high viral load infection and was stronger among women with a history of HPV16 infection. The association also appeared to be stronger among women with high screening adherence (P=0.060). Bereavement characteristics or study source did not modify the association (Supplementary Table S5).
Table 3.
Bereavement and HPV Infection, a Case-Control Study in Sweden, 1969–2002
| Analysis on HPV16 Infection | |||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Characteristics | Negative Smear | Positive Smear | Smear with Low Viral Load | Smear with High Viral Load | |||
|
|
|||||||
| N (%) | N (%) | OR (95% CI)* | N (%) | RRR (95% CI)† | N (%) | RRR (95% CI)† | |
| No bereavement | 3,038 (79.3) | 158 (77.8) | 1.0 | 102 (81.0) | 1.0 | 25 (73.5) | 1.0 |
| Bereavement | 792 (20.7) | 45 (22.2) | 1.62 (1.05 to 2.50) | 24 (19.1) | 1.34 (0.73 to 2.44) | 9 (26.5) | 2.84 (1.29 to 6.27) |
|
| |||||||
| Stratified analysis by previous HPV16 infection | |||||||
| No | |||||||
| No bereavement | 2,862 (79.7) | 139 (81.3) | 1.0 | 89 (84.0) | 1.0 | 21 (77.8) | 1.0 |
| Bereavement | 731 (20.4) | 32 (18.7) | 1.31 (0.86 to 2.00) | 17 (16.0) | 1.08 (0.62 to 1.89) | 6 (22.2) | 2.61 (1.07 to 6.33) |
| Yes | |||||||
| No bereavement | 176 (74.3) | 19 (59.4) | 1.0 | 13 (65.0) | 1.0 | 4 (57.1) | 1.0 |
| Bereavement | 61 (25.7) | 13 (40.6) | 3.94 (1.24 to 12.48) | 7 (35.0) | 3.02 (0.80 to 11.42) | 3 (42.9) | 3.46 (0.56 to 21.17) |
| P for difference‡ | <0.0001 | 0.0002 | 0.002 | ||||
|
| |||||||
| Stratified analysis by screening adherence | |||||||
| High | |||||||
| No bereavement | 2,039 (81.3) | 90 (75.0) | 1.0 | 66 (81.5) | 1.0 | 8 (53.3) | 1.0 |
| Bereavement | 468 (18.7) | 30 (25.0) | 1.95 (1.13 to 3.38) | 15 (18.5) | 1.35 (0.60 to 3.04) | 7 (46.7) | 8.00 (2.96 to 21.59) |
| Low/unscreened | |||||||
| No bereavement | 999 (75.5) | 68 (81.9) | 1.0 | 36 (80.0) | 1.0 | 17 (89.5) | 1.0 |
| Bereavement | 324 (24.5) | 15 (18.1) | 1.15 (0.58 to 2.28) | 9 (20.0) | 1.31 (0.56 to 3.05) | 2 (10.5) | 0.75 (0.18 to 3.15) |
| P for difference‡ | 0.060 | 0.919 | 0.004 | ||||
|
| |||||||
| Analysis on Any HPV Infection§ | |||||||
|
| |||||||
| Negative Smear | Positive Smear | Smear with Low-Risk HPV | Smear with High-Risk HPV | ||||
|
| |||||||
| N (%) | N (%) | OR (95% CI)* | N (%) | OR (95% CI)* | N (%) | OR (95% CI)* | |
|
| |||||||
| No bereavement | 1,426 (80.6) | 230 (83.3) | 1.0 | 55 (87.3) | 1.0 | 195 (83.3) | 1.0 |
| Bereavement | 344 (19.4) | 46 (16.7) | 1.54 (1.03 to 2.30) | 8 (12.7) | 1.13 (0.51 to 2.51) | 39 (16.7) | 1.55 (1.01 to 2.37) |
OR, odds ratio; CI, confidence interval. All models were adjusted for age at smear and within-subject variance.
RRR, relative risk ratio. All models were adjusted for age at smear and within-subject variance.
We added an interaction term between bereavement and the stratification factors (i.e., previous HPV infection and screening adherence) in the models, and reported the P values for the interaction terms as a significance test for the difference between ORs or RRRs.
Low-risk HPV includes HPV-6, HPV-7, HPV-11, HPV-42, HPV-43, and HPV-70. High-risk HPV includes HPV16, HPV-18, HPV-31, HPV-33, HPV-35, HPV-39, HPV-45, HPV-51, HPV-52, HPV-56, HPV-58, HPV-59, HPV-66, HPV-68, HPV-73, and HPV-82.
A stronger association of bereavement was noted with infections of high-risk, compared to low-risk HPV types (Table 3). When HPV16 was excluded from the high-risk HPV group, a positive association was still suggested although not statistically significant (OR 1.50, 95% CI 0.90–2.49).
Lifestyle Factors
Women with bereavement did not differ from women without bereavement, regarding self-reported smoking, oral contraceptive use, number of sexual partners, parity, or abortion (all P values > 0.05), although they were slightly older at start of smoking (P=0.013) (Supplementary Table S6).
DISCUSSION
Based on nationwide registers in Sweden, we found consistent associations of bereavement with subsequently increased risks of oncogenic HPV infection, abnormal cytology, as well as in situ and invasive cervical cancer. Although the overall associations for abnormal cytology and cervical cancer were generally weak, these associations became much stronger when multiple bereavements, loss of a child, spouse, or sibling, and bereavement due to unnatural causes were analyzed separately. Loss of a parent was the most common type of bereavement and was only associated with an increased risk of cervical cancer before 40 years of age, highlighting the potential importance of early life bereavement on cervical cancer development.
To the best of our knowledge, we are the first to comprehensively investigate the link between bereavement and cervical cancer development, through precancerous stages to invasive malignancy. We have previously reported increased risk of ICC among women with loss of a child during adulthood or loss of a parent during childhood (2,3). In the present study, we extended these findings to earlier phases of cervical carcinogenesis, including first smear with abnormal cytology and in situ cervical cancer. In addition, we examined a wider range of stressful exposures including different types of loss within the family instead of, as earlier, only one specific type (2,3,5,6) Lastly, we assessed whether the influence of different types of losses with age on the risk of cervical cancer varied with age Interestingly we were able to demonstrate that loss of a parent was associated with a higher risk of ICCs and in situ cervical cancer in early life but not thereafter, whereas loss of child, sibling, or spouse was consistently associated with a higher risk of these outcomes throughout the life span. Finally and importantly, based on a relatively smaller sample of the study participants, we were able to illustrate that the impact of bereavement on cervical carcinogenesis may be mediated through promoting oncogenic HPV infections, and is unlikely to be completely explained by differential lifestyle factors.
No clear temporal relationship was detected between time since bereavement and cancer development. This is however not surprising since neither bereavement nor cervical carcinogenesis is an instantly developed event. Severe distress in anticipation of losing a loved one might have started long before the actual loss and cervical cancer takes many years to develop (14). The lack of temporal pattern may also be conceptualized assuming that bereavement may indeed impact different phases of cervical cancer development, namely that bereavement and its resultant psychological stress might facilitate a new HPV infection among women without previous contact to HPV, promote a primary HPV contact to oncogenic HPV infection among women with a prevalent HPV infection, and expedite the progression from low-grade to high-grade precancerous lesions, as well as from precancer to cancer among women with cytological lesions.
Infections with high-risk HPV types, particularly persistent, high viral load infection with HPV16, are known determinants of cervical carcinogenesis (14,17). The stronger association observed between bereavement and high viral load infection of HPV16 may lend support to a role of bereavement in promoting overexpression and malignant transformation of HPV oncogenes (24–26); whereas the stronger association with repeated infections may suggest that bereavement may induce compromised host immunosurveillance and subsequently mediate persistence or reactivation of HPV infection (26). For example, psychological stress decreases T-cell proliferative response to HPV16 among women with cervical dysplasia (27), and stress hormone down-regulates the expression of class I human leukocyte antigens (28). Furthermore, psychological stress has also been demonstrated to induce higher titers of Epstein-Barr virus (EBV) antibodies as well as reactivation of EBV, cytomegalovirus, and herpes simplex virus (29–32). Our findings substantiate, therefore, the hypothesis that bereavement contributes to cervical carcinogenesis through promoting oncogenic HPV infections and modulating host vulnerability to such infections.
Given the unique nationwide cervical screening and cancer registers, the major strength of our study is the opportunity to study the impact of bereavement on different phases of cervical carcinogenesis. Given the strictly defined study base and time-varying nature of the bereavement exposure, we performed three case-control studies nested in the study base. Nested case-control study is computationally efficient and preserves the validity of full cohort analysis (33). By linking NKCx to other nationwide registers, we obtained essentially complete ascertainment of both the exposure and outcomes, and importantly, all such information was independently and prospectively collected, alleviating concerns regarding selection and information biases. Although the NKCx was not nationwide until 1995, analysis restricted to the period 1995–2011 rendered similar results (data not shown).
One limitation of the present study is the lack of information on lifestyle factors for all included women. Lifestyle factors might be associated with the risks of both bereavement and cervical cancer. As screening adherence is highly correlated to both socioeconomic status (34) and the risk of cervical dysplasia and cancer, we carefully matched or adjusted for degree of screening participation whenever possible and stratified all analyses by different screening adherence. In a sensitivity analysis, we additionally adjusted for socioeconomic status obtained from the Swedish Population and Household Censuses, and found that the results were virtually unchanged after this additional adjustment (data not shown). Bereavement might also entail lifestyle changes and consequently alter the risk of cervical cancer. Such lifestyle changes should, however, not be considered as confounders of the studied associations but rather mediators linking bereavement to cervical carcinogenesis. Regardless, in the present study, we showed that bereaved women did not differ significantly from other women regarding a few major established or suggested lifestyle risk factors for cervical cancer, including smoking, oral contraceptive use, sexual behavior, parity, and abortion, apart from HPV infection (35–37). Although this analysis was based on a small subset of our study participants, these women were randomly selected from the general population and had a very high response rate to the questionnaire (>90%) (22). The stronger association noted for infection of high-risk, compared to low-risk, HPV types further argued against a pure explanation by lifestyle factors, assuming that lifestyle factors alone would more likely lead to equally increased risks for both.
As we aimed to study a continuum of pathological events through the process of cervical carcinogenesis, some overlap among the study participants in the different analyses of the present study could be expected. For example, we found that 68,409 out of the total 390,310 (17.5%) abnormal cytology smears and 70,143 out of the total 1,951,319 (3.6%) normal cytology smears in the analysis of abnormal cytology belonged to women who later developed in situ/invasive cervical cancer. Similarly, we also found that 17 out of the total 203 (8.4%) HPV16 positive smears and 134 out of the total 3830 (3.5%) HPV16 negative smears in the analysis of HPV infection were cytologically abnormal. To assess the independence of different results obtained in our main analyses, we performed additional analyses by excluding overlapping participants or smears. The results from these additional analyses remained largely unchanged (OR=1.03 of first abnormal cytology and OR=1.60 of HPV16 infection for any bereavement). Furthermore, given the nationwide design of the study, we enrolled almost all women with abnormal cytology or cervical cancer in Sweden during the study period. As a result, not all cases were independent of each other. For example, 3,617 cases of the 147,366 cases enrolled in the in situ/invasive cervical cancer analysis (2.45%) were sisters. Taking into account such familial dependence using clustered analysis did however not change the results clearly (data not shown).
We might have misclassified some cervical dysplasia as normal cytology, since cervical cytology is featured by high specificity while with moderate sensitivity (14). Since the validity of the cytology test should not have been influenced by the woman’s bereavement status, such potential misclassification, if any, would only have attenuated a real association between bereavement and abnormal cytology. Finally, although we aimed to comprehensively assess the role of bereavement due to loss of a close family member, other types of stressful life events were not considered and accordingly the impact of such additional events on the studied association could not be evaluated.
In conclusion, we found a consistent association of bereavement with all defined phases of cervical carcinogenesis. Although potential influence on unmeasured and unknown confounding could not be ruled out completely, such consistency, together with the clear dose-response relationship by the number and type of bereavement as well as clear biologic rationale proposed from previous experimental studies, lends strong evidence to refute the possibility of pure confounding or chance as explanations for these findings. We propose, therefore, that the observed associations are instead attributable to loss of the control of oncogenic HPV infections after bereavement, and psychological stress may serve as one of the modulators differentiating individual likelihood in the malignant transformation of a primary HPV contact. These findings may also be applicable to other infection-related, especially virus infection-related, cancers.
Supplementary Material
Acknowledgments
Financial Support
The NCSR Study was supported by the National Cancer Institute at the National Institutes of Health (grant numbers 1R01CA093378-01A1, 5R01CA111720-03) and grant from Swedish National Cancer Society (4877-B03-01XAC). The Uppsala Study was supported by the National Institutes of Health (R01 CA61197-01A3) and grant from Swedish National Cancer Society (3436-B97-04XAA). This work was supported by Partial Financing of New Doctoral Student (KID) from the Karolinska Institutet (to Dr. Lu); by Karolinska Institutet Distinguished Professor Award (2368/10-221 to Dr. Adami) and by Swedish Society for Medical Research and Karolinska Institutet Research Associate Award (to Dr. Fang). The sponsors of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
We thank Pouran Almstedt and Ninoa Malki for database management, Alexander Ploner and Patrik Magnusson for intellectual contributions on the viral load analysis, and the staff in Joakim Dillner’s and Ulf B. Gyllensten’s laboratories for the HPV testing in the NCSR study and Uppsala study, respectively.
Footnotes
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Authors’ Contributions
Conception and design: D. Lu, K. Fall, A. Sjölander, U. Valdimarsdóttir, F. Fang
Development of methodology: D. Lu, A. Sjölander, F. Fang
Acquisition of data: K. Sundström, P. Sparén, J. Dillner, N. Ylitalo Helm
Analysis of data: D. Lu, A. Sjölander
Interpretation, writing, review, and/or revision of the manuscript: all authors
Administrative, technical, or material support: K. Sundström, P. Sparén, J. Dillner, N. Ylitalo Helm
Financial support and study supervision: P. Sparén, J. Dillner, H.-O. Adami, F. Fang
References
- 1.Stroebe M, Schut H, Stroebe W. Health outcomes of bereavement. Lancet. 2007;370:1960–73. doi: 10.1016/S0140-6736(07)61816-9. [DOI] [PubMed] [Google Scholar]
- 2.Fang F, Fall K, Sparen P, Adami HO, Valdimarsdottir HB, Lambe M, et al. Risk of infection-related cancers after the loss of a child: a follow-up study in Sweden. Cancer Res. 2011;71:116–22. doi: 10.1158/0008-5472.CAN-10-0470. [DOI] [PubMed] [Google Scholar]
- 3.Kennedy B, Valdimarsdottir U, Sundstrom K, Sparen P, Lambe M, Fall K, et al. Loss of a parent and the risk of cancer in early life: a nationwide cohort study. Cancer Causes Control. 2014;25:499–506. doi: 10.1007/s10552-014-0352-z. [DOI] [PubMed] [Google Scholar]
- 4.Graham S, Snell LM, Graham JB, Ford L. Social trauma in the epidemiology of cancer of the cervix. J Chronic Dis. 1971;24:711–25. doi: 10.1016/0021-9681(71)90096-8. [DOI] [PubMed] [Google Scholar]
- 5.Kvikstad A, Vatten LJ, Tretli S, Kvinnsland S. Widowhood and divorce related to cancer risk in middle-aged women. A nested case-control study among Norwegian women born between 1935 and 1954. Int J Cancer. 1994;58:512–6. doi: 10.1002/ijc.2910580410. [DOI] [PubMed] [Google Scholar]
- 6.Kvikstad A, Vatten LJ. Risk and prognosis of cancer in middle-aged women who have experienced the death of a child. Int J Cancer. 1996;67:165–9. doi: 10.1002/(SICI)1097-0215(19960717)67:2<165::AID-IJC2>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 7.Coker AL, Bond S, Madeleine MM, Luchok K, Pirisi L. Psychosocial stress and cervical neoplasia risk. Psychosom Med. 2003;65:644–51. doi: 10.1097/01.psy.0000041471.57895.08. [DOI] [PubMed] [Google Scholar]
- 8.Goodkin K, Antoni MH, Blaney PH. Stress and hopelessness in the promotion of cervical intraepithelial neoplasia to invasive squamous cell carcinoma of the cervix. J Psychosom Res. 1986;30:67–76. doi: 10.1016/0022-3999(86)90068-1. [DOI] [PubMed] [Google Scholar]
- 9.Tiersma ES, van der Lee ML, Peters AA, Visser AP, Jan Fleuren G, Garssen B, et al. Psychosocial factors and the grade of cervical intra-epithelial neoplasia: a semi-prospective study. Gynecol Oncol. 2004;92:603–10. doi: 10.1016/j.ygyno.2003.10.046. [DOI] [PubMed] [Google Scholar]
- 10.Tiersma ES, van der Lee ML, Garssen B, Peters AA, Visser AP, Fleuren GJ, et al. Psychosocial factors and the course of cervical intra-epithelial neoplasia: a prospective study. Gynecol Oncol. 2005;97:879–86. doi: 10.1016/j.ygyno.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 11.Antoni MH, Goodkin K. Host moderator variables in the promotion of cervical neoplasia--II. Dimensions of life stress. J Psychosom Res. 1989;33:457–67. doi: 10.1016/0022-3999(89)90007-x. [DOI] [PubMed] [Google Scholar]
- 12.De Punzio C, Salvestroni C, Guazzelli G, Papa MC, Freschi G, Ferdeghini M, et al. Stress and cervical dysplasia. Eur J Gynaecol Oncol. 1998;19:287–90. [PubMed] [Google Scholar]
- 13.Bosch FX, Lorincz A, Munoz N, Meijer CJ, Shah KV. The causal relation between human papillomavirus and cervical cancer. J Clin Pathol. 2002;55:244–65. doi: 10.1136/jcp.55.4.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schiffman M, Castle PE, Jeronimo J, Rodriguez AC, Wacholder S. Human papillomavirus and cervical cancer. Lancet. 2007;370:890–907. doi: 10.1016/S0140-6736(07)61416-0. [DOI] [PubMed] [Google Scholar]
- 15.Cervixcancerprevention NKf. Förebyggande av livmoderhalscancer i Sverige - Verksamhetsberättelse och Årsrapport 2013 med data tom 2012. 2013 < http://www.cancercentrum.se/Global/RCC%20Samverkan/Dokument/Screening/NKCx_%C3%A5rsrapport_2013.pdf>.
- 16.Azerkan F, Sparen P, Sandin S, Tillgren P, Faxelid E, Zendehdel K. Cervical screening participation and risk among Swedish-born and immigrant women in Sweden. Int J Cancer. 2012;130:937–47. doi: 10.1002/ijc.26084. [DOI] [PubMed] [Google Scholar]
- 17.Sundstrom K, Ploner A, Dahlstrom LA, Palmgren J, Dillner J, Adami HO, et al. Prospective study of HPV16 viral load and risk of in situ and invasive squamous cervical cancer. Cancer Epidemiol Biomarkers Prev. 2013;22:150–8. doi: 10.1158/1055-9965.EPI-12-0953-T. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dahlstrom LA, Ylitalo N, Sundstrom K, Palmgren J, Ploner A, Eloranta S, et al. Prospective study of human papillomavirus and risk of cervical adenocarcinoma. Int J Cancer. 2010;127:1923–30. doi: 10.1002/ijc.25408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Josefsson AM, Magnusson PK, Ylitalo N, Sorensen P, Qwarforth-Tubbin P, Andersen PK, et al. Viral load of human papilloma virus 16 as a determinant for development of cervical carcinoma in situ: a nested case-control study. Lancet. 2000;355:2189–93. doi: 10.1016/S0140-6736(00)02401-6. [DOI] [PubMed] [Google Scholar]
- 20.Kim JY, Park S, Nam BH, Roh JW, Lee CH, Kim YH, et al. Low initial human papilloma viral load implicates worse prognosis in patients with uterine cervical cancer treated with radiotherapy. J Clin Oncol. 2009;27:5088–93. doi: 10.1200/JCO.2009.22.4659. [DOI] [PubMed] [Google Scholar]
- 21.Ekbom A. The Swedish Multi-generation Register. Methods Mol Biol. 2011;675:215–20. doi: 10.1007/978-1-59745-423-0_10. [DOI] [PubMed] [Google Scholar]
- 22.Ylitalo N, Sorensen P, Josefsson A, Frisch M, Sparen P, Ponten J, et al. Smoking and oral contraceptives as risk factors for cervical carcinoma in situ. Int J Cancer. 1999;81:357–65. doi: 10.1002/(sici)1097-0215(19990505)81:3<357::aid-ijc8>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 23.Cleveland WS, Devlin SJ, Grosse E. Regression by local fitting: methods, properties, and computational algorithms. J Econom. 1988;37:87–114. [Google Scholar]
- 24.Mittal R, Pater A, Pater MM. Multiple human papillomavirus type 16 glucocorticoid response elements functional for transformation, transient expression, and DNA-protein interactions. J Virol. 1993;67:5656–9. doi: 10.1128/jvi.67.9.5656-5659.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pater MM, Hughes GA, Hyslop DE, Nakshatri H, Pater A. Glucocorticoid-dependent oncogenic transformation by type 16 but not type 11 human papilloma virus DNA. Nature. 1988;335:832–5. doi: 10.1038/335832a0. [DOI] [PubMed] [Google Scholar]
- 26.Antoni MH, Lutgendorf SK, Cole SW, Dhabhar FS, Sephton SE, McDonald PG, et al. The influence of bio-behavioural factors on tumour biology: pathways and mechanisms. Nat Rev Cancer. 2006;6:240–8. doi: 10.1038/nrc1820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fang CY, Miller SM, Bovbjerg DH, Bergman C, Edelson MI, Rosenblum NG, et al. Perceived stress is associated with impaired T-cell response to HPV16 in women with cervical dysplasia. Ann Behav Med. 2008;35:87–96. doi: 10.1007/s12160-007-9007-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bartholomew JS, Glenville S, Sarkar S, Burt DJ, Stanley MA, Ruiz-Cabello F, et al. Integration of high-risk human papillomavirus DNA is linked to the down-regulation of class I human leukocyte antigens by steroid hormones in cervical tumor cells. Cancer Res. 1997;57:937–42. [PubMed] [Google Scholar]
- 29.Esterling BA, Antoni MH, Kumar M, Schneiderman N. Emotional repression, stress disclosure responses, and Epstein-Barr viral capsid antigen titers. Psychosom Med. 1990;52:397–410. doi: 10.1097/00006842-199007000-00002. [DOI] [PubMed] [Google Scholar]
- 30.Fagundes CP, Glaser R, Malarkey WB, Kiecolt-Glaser JK. Childhood adversity and herpesvirus latency in breast cancer survivors. Health Psychol. 2013;32:337–44. doi: 10.1037/a0028595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rector JL, Dowd JB, Loerbroks A, Burns VE, Moss PA, Jarczok MN, et al. Consistent associations between measures of psychological stress and CMV antibody levels in a large occupational sample. Brain Behav Immun. 2014;38:133–41. doi: 10.1016/j.bbi.2014.01.012. [DOI] [PubMed] [Google Scholar]
- 32.Shirtcliff EA, Coe CL, Pollak SD. Early childhood stress is associated with elevated antibody levels to herpes simplex virus type 1. Proc Natl Acad Sci U S A. 2009;106:2963–7. doi: 10.1073/pnas.0806660106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ernster VL. Nested case-control studies. Prev Med. 1994;23:587–90. doi: 10.1006/pmed.1994.1093. [DOI] [PubMed] [Google Scholar]
- 34.Katz SJ, Hofer TP. Socioeconomic disparities in preventive care persist despite universal coverage. Breast and cervical cancer screening in Ontario and the United States. JAMA. 1994;272:530–4. [PubMed] [Google Scholar]
- 35.Waggoner SE. Cervical cancer. Lancet. 2003;361:2217–25. doi: 10.1016/S0140-6736(03)13778-6. [DOI] [PubMed] [Google Scholar]
- 36.International Collaboration of Epidemiological Studies of Cervical C. Appleby P, Beral V, Berrington de Gonzalez A, Colin D, Franceschi S, et al. Cervical cancer and hormonal contraceptives: collaborative reanalysis of individual data for 16,573 women with cervical cancer and 35,509 women without cervical cancer from 24 epidemiological studies. Lancet. 2007;370:1609–21. doi: 10.1016/S0140-6736(07)61684-5. [DOI] [PubMed] [Google Scholar]
- 37.International Collaboration of Epidemiological Studies of Cervical C. Cervical carcinoma and reproductive factors: collaborative reanalysis of individual data on 16,563 women with cervical carcinoma and 33,542 women without cervical carcinoma from 25 epidemiological studies. Int J Cancer. 2006;119:1108–24. doi: 10.1002/ijc.21953. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.