Abstract
Objective
Hip shape by statistical shape modeling (SSM) is associated with hip radiographic OA (rOA); we examined associations between hip shape and knee rOA given the biomechanical inter-relationships between these joints.
Methods
Bilateral baseline hip shape assessments (for those with at least 1 hip with Kellgren-Lawrence grade [KLG] 0 or 1) from the Johnston County Osteoarthritis Project were available. Proximal femur shape was defined on baseline pelvis radiographs and evaluated by SSM, producing mean shape and continuous variables representing independent modes of variation (14 modes=95% of shape variance). Outcomes included prevalent (baseline KLG >=2 or total knee replacement [TKR]), incident (baseline KLG 0/1 with follow-up >=2), and progressive (KLG increase of >=1 or TKR) knee rOA. Limb-based logistic regression models for ipsilateral and contralateral comparisons were adjusted for age, sex, race, body mass index (BMI), and hip rOA, accounting for intra-person correlations.
Results
We evaluated 681 hips and 682 knees from 342 individuals (61% women, 82% white, mean age 62 years, BMI 29 kg/m2). Ninety-nine knees (15%) had prevalent rOA (4 knees with TKR). Lower mode 2 and 3 scores were associated with ipsilateral prevalent knee rOA; only lower mode 3 scores were associated with contralateral prevalent knee rOA. No statistically significant associations were seen for incident or progressive knee rOA.
Conclusions
Variations in hip shape were associated with prevalent, but not incident or progressive, knee rOA in this cohort, and may reflect biomechanical differences between limbs, genetic influences, or common factors related to both hip shape and knee rOA.
Keywords: Hip joint, knee osteoarthritis, radiography
Background
Statistical shape modeling (SSM) methods have been used by several groups, including ours, to describe the variability in hip shape in populations. Hip shape by SSM has been found to be a radiographic biomarker for development of osteoarthritis (OA) at the hip, defined as structural disease (radiographic OA [rOA]), clinical/symptomatic OA (rOA with OA symptoms), and/or total hip replacement (1-6). Specifically, our group has found associations between variations in modes 2 (reflecting changes in the width of the femoral neck and size of the trochanters) and 3 (variations in femoral neck length and the width of the greater trochanter) and incident symptomatic hip OA (6).
The hip and knee are biomechanically interconnected as part of the kinetic chain, and OA at one of these large joint sites increases risk at the other sites in a non-random fashion. As shown by Shakoor et al (7), in patients requiring a knee replacement after an initial hip replacement, this procedure was much more likely to be done at the contralateral knee and, similarly, for those undergoing initial knee replacement, a subsequent hip replacement was more likely on the contralateral side. Individuals with OA in one of these 4 large joints (right or left, hip or knee) have 40-80% greater odds of having OA in another joint, although the greatest odds were for OA in the contralateral cognate joint (e.g. if the right knee was affected, the odds of left knee OA were dramatically increased)(8). In addition, individuals with developmental dysplasia of the hip are more likely to undergo not only hip but also knee replacement compared with controls (9). Patients with moderate to severe knee OA, compared with controls, also demonstrate differences in biomechanical assessments, not only at the knee, but also at the hip and ankle, including decreased adduction and extension moments at the hip and dorsiflexion moments at the ankle (10). Although the specific biomechanical consequences of variations in joint shape are not yet known, given the above evidence for the inter-relationship between the hip and knee joints, in the current study we sought to assess potential structural associations between hip shape, described quantitatively using modes of variation, and prevalent, incident, and progressive knee rOA in the Johnston County OA Project (JoCo OA).
Methods
Study sample
Data were from the JoCo OA baseline and first follow-up visit (mean follow-up time 6 years [range 4-11 years]); details of the parent project have been described elsewhere (11). The JoCo OA has been continuously approved by the Institutional Review Boards of the University of North Carolina at Chapel Hill and the Centers for Disease Control and Prevention, and all participants completed informed consent. The baseline time point hip shapes used in this analysis were obtained as part of a prior analysis of hip shape and incident symptomatic and radiographic hip OA (6). In brief, of the 1726 individuals with paired radiographic data (anteroposterior [AP] supine pelvis films with the feet in 15 degrees of internal rotation, read blinded to clinical status and chronological order) from both baseline and follow-up time points, 193 hips developed incident rOA, defined as a Kellgren Lawrence grade (KLG) of 0 or 1 at baseline and 2 or more at follow-up. All of these were selected, along with randomly selected control hips (KLG 0 or 1 at both time points) in approximately equal numbers from 4 race-by-gender strata (men, women, African American, and white) for a total of 342 individuals.
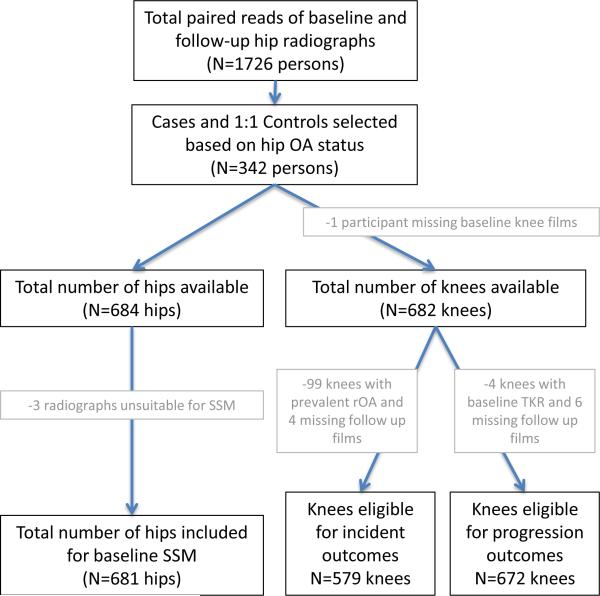
Unlike the previous analysis, which focused on case/control status at the hip (6), for the current analysis baseline hip shape from all hips from all participants (both cases and controls) with suitable radiographs (n=681 hips, Figure 1) were included, such that a small number (77 hips, or 11% of the hips) had evidence of prevalent radiographic hip OA (KLG ≥ 2) at baseline (these hips were excluded from the prior study).
Figure 1.
Flowchart of included participants and joints.
Hip Shape Assessment
A 60-point model of proximal femur shape (2, 6) was defined on the baseline AP pelvis radiographs and evaluated by SSM. Principal components analysis was performed on these 60 points; the first fourteen principal components were retained, explaining 95% of the shape variance. These in turn correspond to 14 independent modes of shape variation, which are treated as 14 continuous variables in this analysis. Further details on the derivation of these modes have been published previously (6).
Knee OA Assessment
Bilateral weight-bearing posteroanterior fixed-flexion knee radiographs were obtained for all participants and were read for rOA by a single examiner (JBR; from prior study, weighted kappa for interrater reliability 0.9; kappa for intrarater reliability 0.9, (12)). Knee rOA outcomes were defined as follows: 1) Prevalent knee rOA was defined as a KLG ≥ 2 or total knee replacement (TKR) for OA at baseline; 2) Incident knee rOA was defined as a KLG ≥ 2 at follow-up in a knee having KLG=0 or 1 at baseline; 3) Progressive knee rOA was defined as an increase of at least one KLG or progression to TKR between baseline and follow-up, regardless of baseline KLG (to avoid conditioning on an intermediate (13)), and excluding knees with baseline TKR as they could not progress further by definition.
Statistical Analysis
The 14 baseline hip shape mode scores were simultaneously included in 4 separate limb-based logistic regression models for ipsilateral and contralateral comparisons of knee outcomes (1: right hip/right knee, 2: left hip/left knee, 3: right hip/left knee, and 4: left hip/right knee), adjusted for age, sex, race, body mass index (BMI), and hip rOA (ipsilateral to the mode score in the model), accounting for intra-person correlations (using the cluster option in Stata (14)).
Results
We evaluated 681 hips and 682 knees from 342 individuals (Figure 1); characteristics are shown in Table 1. A total of 77 hips (11%) had prevalent radiographic OA at baseline, and prevalent knee rOA was present in 99 knees (15%) at baseline, of which 53 and 46 were right and left knees, respectively.
Table 1.
Sample characteristics (n=342)
| Characteristic | n(%) or mean (SD) |
|---|---|
| Female sex | 210 (61.4%) |
| White | 282 (82.5%) |
| Age (years) | 61.7 (8.9) |
| BMI (kg/m2) | 29.2 (5.9) |
| Knees at baseline (n=682) | |
| KLG=0 | 396 (58.1%) |
| KLG=1 | 187 (27.4%) |
| KLG=2 | 61 (8.9%) |
| KLG=3 | 27 (4.0%) |
| KLG=4 | 7 (1.0%) |
| TKR | 4 (0.6%) |
| Hips at baseline (n=681) | |
| KLG=0 | 121 (17.8%) |
| KLG=1 | 483 (70.9%) |
| KLG=2 | 74 (10.9%) |
| KLG=3 | 2 (0.3%) |
| KLG=4 | 1 (0.2%) |
| THR | 0 (0.0%) |
Prevalent knee rOA: Ipsilateral Associations
The odds of having prevalent rOA in the right knee were increased by 74% for every 1-SD reduction in mode 2 at the right hip in analyses adjusted for age, sex, race, BMI, and right hip rOA (Table 2). The associations between left hip mode 2 score and prevalent left knee rOA were not statistically significant. In adjusted analyses, for every 1-SD lower score for mode 3 at the right hip, the odds of right knee rOA were increased by 46%; for every 1-SD reduction in mode 3 score at the left hip, the odds of left knee rOA were increased by 50%. As shown in Table 2, there were also statistically significant associations for a 1-SD lower score for modes 8 and 14 at the left hip and prevalent left knee OA, although these modes account for only 2.3% and 0.6% of total shape variance, respectively.
Table 2.
Association between a 1-SD decrease in baseline hip shape modes and prevalent radiographic knee OA.
| Mode | % variance in hip shape explained | Ipsilateral | Contralateral | ||
|---|---|---|---|---|---|
| Right hip/Right knee aOR* (95% CI) | Left hip/Left knee aOR* (95% CI) | Right hip/Left knee aOR* (95% CI) | Left hip/Right knee aOR* (95% CI) | ||
| 1 | 37.4 | 0.87 (0.57, 1.32) | 1.17 (0.75, 1.84) | 0.78 (0.50, 1.21) | 1.31 (0.83, 2.08) |
| 2 | 16.0 | 1.74 (1.18, 2.57) | 1.06 (0.77, 1.47) | 1.22 (0.86, 1.72) | 1.35 (0.96, 1.91) |
| 3 | 12.5 | 1.46 (1.03, 2.05) | 1.50 (1.07, 2.10) | 1.19 (0.83, 1.70) | 1.78 (1.23, 2.56) |
| 4 | 9.9 | 1.00 (0.65, 1.53) | 1.08 (0.71, 1.65) | 1.05 (0.70, 1.59) | 0.99 (0.63, 1.54) |
| 5 | 5.1 | 0.96 (0.66, 1.41) | 0.97 (0.65, 1.46) | 0.99 (0.70, 1.40) | 0.77 (0.52, 1.14) |
| 6 | 3.4 | 1.03 (0.68, 1.57) | 1.40 (0.92, 2.13) | 0.92 (0.64, 1.33) | 1.17 (0.80, 1.73) |
| 7 | 2.6 | 0.85 (0.61, 1.18) | 0.76 (0.53, 1.08) | 0.89 (0.65, 1.21) | 0.76 (0.53, 1.09) |
| 8 | 2.3 | 0.97 (0.69, 1.35) | 0.65 (0.44, 0.96) | 0.97 (0.70, 1.34) | 0.71 (0.50, 1.02) |
| 9 | 1.7 | 1.31 (0.96, 1.81) | 0.80 (0.55, 1.17) | 1.21 (0.86, 1.70) | 1.04 (0.74, 1.46) |
| 10 | 1.3 | 1.02 (0.73, 1.42) | 0.70 (0.46, 1.07) | 1.04 (0.75, 1.45) | 0.73 (0.47, 1.14) |
| 11 | 1.1 | 1.06 (0.67, 1.66) | 1.15 (0.81, 1.62) | 1.01 (0.62, 1.63) | 1.27 (0.87, 1.86) |
| 12 | 0.9 | 0.86 (0.58, 1.27) | 0.74 (0.48, 1.13) | 0.97 (0.67, 1.41) | 0.83 (0.56, 1.24) |
| 13 | 0.7 | 1.03 (0.74, 1.45) | 0.83 (0.58, 1.20) | 1.01 (0.69, 1.48) | 0.96 (0.67, 1.39) |
| 14 | 0.6 | 1.08 (0.79, 1.48) | 0.65 (0.45, 0.94) | 0.95 (0.70, 1.28) | 0.87 (0.61, 1.24) |
Adjusted Odds Ratio, adjusted for age, sex, race, BMI, and hip OA ipsilateral to hip mode score
Prevalent knee rOA: Contralateral Associations
For mode 2, none of the contralateral associations between hip shape modes and prevalent knee rOA were statistically significant. However, a 35% increase in the odds of right knee rOA for every 1-SD reduction in mode 2 score at the left hip was noteworthy and approached statistical significance (aOR 1.35, 95% CI [0.96, 1.91], Table 2). For every 1-SD reduction in mode 3 score at the left hip, there was a statistically significant 78% increase in the odds of prevalent right knee rOA in adjusted analyses. Associations between mode 3 at the right hip and left knee rOA were not statistically significant.
Incident knee rOA
Of 579 eligible knees (99 had prevalent rOA, 4 lacked follow-up films), 94 (16%) developed incident rOA at follow-up, of which 50 and 44 were right and left knees, respectively. There were no statistically significant associations between modes and incident knee rOA (Table 3). Of potential interest, although not statistically significant, were suggestive associations between right hip shape and incident right knee rOA (34% higher odds for every 1-SD lower score on mode 9), and between right hip shape and incident left knee rOA (38% higher odds for every 1-SD reduction in mode 7 score, and 39% higher odds per 1-SD higher score for mode 8, Table 3).
Table 3.
Association between a 1-SD decrease in baseline hip shape modes and incident radiographic knee OA.
| Mode | % variance in hip shape explained | Ipsilateral | Contralateral | ||
|---|---|---|---|---|---|
| Right hip/Right knee aOR* (95% CI) | Left hip/Left knee aOR* (95% CI) | Right hip/Left knee aOR* (95% CI) | Left hip/Right knee aOR* (95% CI) | ||
| 1 | 37.4 | 1.24 (0.84, 1.84) | 0.85 (0.56, 1.30) | 0.94 (0.63, 1.38) | 0.98 (0.67, 1.42) |
| 2 | 16.0 | 0.97 (0.68, 1.39) | 1.17 (0.81, 1.69) | 1.24 (0.84, 1.83) | 0.98 (0.70, 1.38) |
| 3 | 12.5 | 1.05 (0.76, 1.45) | 1.08 (0.78, 1.48) | 1.04 (0.74, 1.48) | 1.12 (0.83, 1.51) |
| 4 | 9.9 | 0.95 (0.68, 1.32) | 0.99 (0.67, 1.47) | 1.03 (0.71, 1.52) | 0.93 (0.67, 1.31) |
| 5 | 5.1 | 1.27 (0.86, 1.88) | 0.98 (0.66, 1.46) | 0.97 (0.66, 1.44) | 0.91 (0.63, 1.31) |
| 6 | 3.4 | 0.95 (0.68, 1.33) | 1.26 (0.86, 1.84) | 1.13 (0.83, 1.52) | 0.90 (0.62, 1.32) |
| 7 | 2.6 | 1.05 (0.76, 1.45) | 0.96 (0.64, 1.45) | 1.38 (0.97, 1.97) | 0.95 (0.68, 1.34) |
| 8 | 2.3 | 0.99 (0.72, 1.36) | 1.07 (0.71, 1.61) | 1.39 (0.96, 2.01) | 0.96 (0.67, 1.37) |
| 9 | 1.7 | 1.34 (0.97, 1.87) | 1.25 (0.80, 1.94) | 1.00 (0.66, 1.51) | 1.30 (0.90, 1.86) |
| 10 | 1.3 | 1.27 (0.91, 1.78) | 0.82 (0.55, 1.22) | 1.01 (0.72, 1.41) | 1.05 (0.71, 1.56) |
| 11 | 1.1 | 0.82 (0.58, 1.16) | 0.86 (0.60, 1.22) | 0.74 (0.51, 1.07) | 0.88 (0.61, 1.27) |
| 12 | 0.9 | 0.81 (0.59, 1.10) | 0.88 (0.61, 1.29) | 0.81 (0.60, 1.08) | 0.83 (0.60, 1.15) |
| 13 | 0.7 | 0.97 (0.70, 1.33) | 0.91 (0.62, 1.32) | 1.26 (0.89, 1.79) | 1.02 (0.71, 1.45) |
| 14 | 0.6 | 1.10 (0.83, 1.46) | 1.23 (0.88, 1.71) | 1.24 (0.89, 1.73) | 1.06 (0.78, 1.44) |
Adjusted Odds Ratio, adjusted for age, sex, race, BMI, and hip OA ipsilateral to hip mode score
Progressive knee rOA
Of 672 eligible knees (4 had baseline TKR, 6 lacked follow-up films), 219 (33%) met the definition of progressive knee rOA, of which 118 and 101 were right and left knees, respectively. There were no significant associations between modes and progressive knee rOA (Table 4). Associations approaching statistically significance, though not formally so, were seen in adjusted analyses between right hip shape and progressive right knee rOA (28% higher odds for every 1-SD reduction in mode 9 score) and between right hip shape and progressive left knee rOA (23% lower odds for every 1-SD lower mode 11 score, Table 4).
Table 4.
Association between a 1-SD decrease in baseline hip shape modes and progressive radiographic knee OA.
| Mode | % variance in hip shape explained | Ipsilateral | Contralateral | ||
|---|---|---|---|---|---|
| Right hip/Right knee aOR* (95% CI) | Left hip/Left knee aOR* (95% CI) | Right hip/Left knee aOR* (95% CI) | Left hip/Right knee aOR* (95% CI) | ||
| 1 | 37.4 | 1.16 (0.88, 1.54) | 0.98 (0.74, 1.29) | 1.06 (0.80, 1.41) | 1.07 (0.81, 1.42) |
| 2 | 16.0 | 0.98 (0.76, 1.26) | 1.06 (0.81, 1.39) | 1.07 (0.82, 1.39) | 0.99 (0.76, 1.28) |
| 3 | 12.5 | 0.96 (0.75, 1.23) | 0.92 (0.72, 1.19) | 0.97 (0.76, 1.24) | 0.88 (0.68, 1.13) |
| 4 | 9.9 | 1.11 (0.83, 1.48) | 1.03 (0.79, 1.35) | 0.95 (0.70, 1.29) | 1.02 (0.78, 1.33) |
| 5 | 5.1 | 1.16 (0.89, 1.51) | 0.93 (0.71, 1.22) | 1.02 (0.79, 1.33) | 1.13 (0.88, 1.45) |
| 6 | 3.4 | 0.98 (0.76, 1.26) | 0.95 (0.73, 1.25) | 0.91 (0.71, 1.17) | 1.00 (0.77, 1.30) |
| 7 | 2.6 | 0.96 (0.75, 1.23) | 1.07 (0.82, 1.41) | 1.03 (0.80, 1.33) | 1.08 (0.83, 1.40) |
| 8 | 2.3 | 0.86 (0.68, 1.09) | 0.88 (0.68, 1.15) | 0.91 (0.71, 1.16) | 0.94 (0.73, 1.20) |
| 9 | 1.7 | 1.28 (0.98, 1.67) | 1.01 (0.77, 1.34) | 1.06 (0.80, 1.40) | 1.07 (0.81, 1.42) |
| 10 | 1.3 | 0.93 (0.74, 1.19) | 1.01 (0.77, 1.32) | 1.02 (0.80, 1.32) | 0.94 (0.73, 1.23) |
| 11 | 1.1 | 0.80 (0.61, 1.05) | 1.01 (0.78, 1.30) | 0.77 (0.59, 1.02) | 0.87 (0.68, 1.12) |
| 12 | 0.9 | 0.86 (0.67, 1.09) | 0.90 (0.69, 1.16) | 0.86 (0.67, 1.10) | 0.96 (0.75, 1.22) |
| 13 | 0.7 | 0.89 (0.71, 1.12) | 0.85 (0.64, 1.13) | 1.00 (0.79, 1.26) | 0.98 (0.75, 1.27) |
| 14 | 0.6 | 1.18 (0.93, 1.49) | 0.96 (0.75, 1.23) | 1.14 (0.90, 1.45) | 1.15 (0.90, 1.47) |
Adjusted Odds Ratio, adjusted for age, sex, race, BMI, and hip OA ipsilateral to hip mode score
Discussion
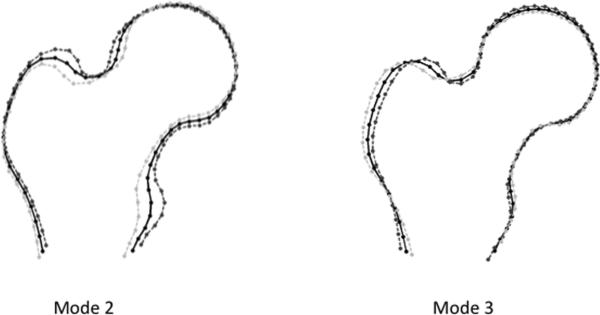
Variations in the shape of the hip (particularly modes 2 and 3) were related to the baseline prevalence of knee rOA in this cohort, although the relationships varied among ipsilateral and contralateral joint pairings. Our findings for the ipsilateral hip shape-knee rOA association are supported by a study of the Osteoarthritis Initiative cohort that reported an association between prevalent knee OA (lateral and medial compartments) with ipsilateral proximal femur shapes (15). In our study, Mode 2 reflects differences in the width of the femoral neck and size of the trochanters, while mode 3 is suggestive of variation in the width of the greater trochanter and femoral neck length (6). Our prior work shows associations between modes 2 and 3 (explaining 16% and 13% of total shape variance respectively, shown in Figure 2 as mean shape ± 2SD for illustrative purposes) with incident symptomatic hip OA. There was a likely, yet not statistically significant, relationship between mode 9 at the right hip and both incident and progressive right knee rOA that was not seen with other joint combinations. Associations with modes 7, 8, and 11 were inconsistent, and these modes explained little of the total shape variance. Therefore, this analysis suggests that radiographic hip shape by SSM represents a modest, independent risk factor for prevalent knee rOA.
Figure 2.
Hip shape modes associated with prevalent radiographic knee OA (mean: black solid lines; +2SD: dark dashed lines; −2SD: light dashed lines). Figure based on the same data as figure 2 in reference (6); a lower mode score (similar to −2SD line) was associated with incident symptomatic hip OA in reference (6).
This study is unique in that it considers the impact of hip shape on OA at joints other than the hip in a community-based cohort of African American and White men and women. The question then is, how to explain this association? Arguably the most obvious mechanism is biomechanical; the shape of the hip, whether assessed using SSM or geometric measures, may influence loading and forces generated at the knee and in the rest of the lower extremity kinetic chain (i.e. lumbar spine, ankle, foot), although a mechanism has yet to be elucidated given the complexity of the needed analyses. Alternatively, there may be common factors underlying both the shape of the hip and the development of knee OA, such as genetics or lifestyle factors, that may explain their relationship. A necessary part of future research will be to examine biomechanics, genetics, and other potentially shared risk factors for these conditions.
The associations between hip shape and knee rOA varied between ipsilateral and contralateral relationships. Consistent with prior research (16-18), we found a higher frequency of knee rOA on the right versus the left side. Kopec et al reported moderate associations between prevalent hip and knee rOA but these did not vary by side (18). Shakoor et al, in addition to demonstrating nonrandom distribution of joint replacement (7), also found higher joint loads in contralateral knees of patients undergoing unilateral hip replacement, even after surgery (19). Overall, in the current analysis, ipsilateral associations between hip shape and knee rOA were stronger than contralateral ones; that the strongest associations identified were those between right hip shape variation and right sided prevalent knee rOA may be consistent with greater right leg dominance in the participants. These findings may reflect biomechanical differences between limbs, but the present study lacked comprehensive biomechanical assessments to test this hypothesis.
Unlike prevalent knee rOA, we did not see any associations reach statistical significance between hip shape and incident and progressive knee rOA. This may be in part due to the older age of our cohort, since variation in hip shape is likely primarily genetically determined, and is present throughout life in the absence of pathologic changes (such as those that occur with OA). Therefore, variation in hip shape may primarily be a risk factor for early onset or rapidly progressive knee rOA, and may not be associated with later incident or progressive disease in this population, though it would still be associated with prevalent disease. Alternatively, 6 years of follow-up may be insufficient to allow incident and progressive knee outcomes to develop. Additionally, although our study design was longitudinal, we were not able to conclusively evaluate the causal relationship; it is conceivable that hip joint shape may lead to altered knee joint mechanics and therefore to a greater risk of knee OA, or equally reasonably, that knee OA could result in remodeling at the hip altering its shape, or potentially even a combination of these. A next step in this research is to examine the clinically relevant association of hip shape with symptomatic knee OA.
This study has several strengths, including the assessment of multiple joints on participants in this well-characterized cohort, the ability to conduct longitudinal analyses, and the standardized radiographs read with high reliability for KLG and for hip shape. The limitations of this work include the relatively small sample size precluding sub-group analyses (such as stratification by sex or race), the use of a single cohort which may limit generalizability, and the lack of long-limb radiographs for assessment of alignment.
Conclusions
Radiographic hip shape is a modest risk factor for prevalent knee rOA independent of age, sex, race, body mass index, and baseline hip rOA. Future studies should examine the role of biomechanical factors in this relationship, as well as assessment of multiple lower-body joint OA over a longer follow-up time.
Acknowledgments
We would like to thank our funding sources, as well as the staff and participants in the Johnston County Osteoarthritis Project, without whom this work would not be possible.
Role of funding source
Funding was provided in part by: NIAMS K23 AR061406 (Nelson); NIH/NIAMS P60AR30701 (Jordan/Renner/Schwartz); CDC/ASPH S043 and S3486 (Jordan/Renner); K24-AR04884, P50-AR063043, and P50-AR060752 (Lane); NIH/NCATS KL2TR001109 (Golightly)
List of Abbreviations
- BMI
body mass index
- JoCo OA
Johnston County Osteoarthritis Project
- KLG
Kellgren-Lawrence grade
- OA
osteoarthritis
- rOA
radiographic osteoarthritis
- SSM
Statistical shape modeling
- TKR
total knee replacement
Footnotes
Competing interests
The authors report no competing interests in relation to this work.
References
- 1.Gregory JS, Waarsing JH, Day J, Pols HA, Reijman M, Weinans H, et al. Early identification of radiographic osteoarthritis of the hip using an active shape model to quantify changes in bone morphometric features: can hip shape tell us anything about the progression of osteoarthritis? Arthritis Rheum. 2007;56:3634–43. doi: 10.1002/art.22982. [DOI] [PubMed] [Google Scholar]
- 2.Lynch JA, Parimi N, Chaganti RK, Nevitt MC, Lane NE. The association of proximal femoral shape and incident radiographic hip OA in elderly women. Osteoarthritis Cartilage. 2009;17:1313–8. doi: 10.1016/j.joca.2009.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agricola R, Reijman M, Bierma-Zeinstra SM, Verhaar JA, Weinans H, Waarsing JH. Total hip replacement but not clinical osteoarthritis can be predicted by the shape of the hip: a prospective cohort study (CHECK). Osteoarthritis Cartilage. 2013;21:559–64. doi: 10.1016/j.joca.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 4.Barr RJ, Gregory JS, Reid DM, Aspden RM, Yoshida K, Hosie G, et al. Predicting OA progression to total hip replacement: can we do better than risk factors alone using active shape modelling as an imaging biomarker? Rheumatology (Oxford) 2012;51:562–70. doi: 10.1093/rheumatology/ker382. [DOI] [PubMed] [Google Scholar]
- 5.Waarsing JH, Rozendaal RM, Verhaar JA, Bierma-Zeinstra SM, Weinans H. A statistical model of shape and density of the proximal femur in relation to radiological and clinical OA of the hip. Osteoarthritis Cartilage. 2010;18:787–94. doi: 10.1016/j.joca.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 6.Nelson AE, Liu F, Lynch JA, Renner JB, Schwartz TA, Lane NE, et al. Association of incident symptomatic hip osteoarthritis with differences in hip shape by active shape modeling: the Johnston County Osteoarthritis Project. Arthritis Care Res (Hoboken) 2014;66:74–81. doi: 10.1002/acr.22094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shakoor N, Block JA, Shott S, Case JP. Nonrandom evolution of end-stage osteoarthritis of the lower limbs. Arthritis Rheum. 2002;46:3185–9. doi: 10.1002/art.10649. [DOI] [PubMed] [Google Scholar]
- 8.Sayre EC, Jordan JM, Cibere J, Murphy L, Schwartz TA, Helmick CG, et al. Quantifying the association of radiographic osteoarthritis in knee or hip joints with other knees or hips: the Johnston County Osteoarthritis Project. J Rheumatol. 2010;37:1260–5. doi: 10.3899/jrheum.091154. [DOI] [PubMed] [Google Scholar]
- 9.Schiffern AN, Stevenson DA, Carroll KL, Pimentel R, Mineau G, Viskochil DH, et al. Total hip arthroplasty, hip osteoarthritis, total knee arthroplasty, and knee osteoarthritis in patients with developmental dysplasia of the hip and their family members: a kinship analysis report. J Pediatr Orthop. 2012;32:609–12. doi: 10.1097/BPO.0b013e31825fa7f2. [DOI] [PubMed] [Google Scholar]
- 10.Astephen JL, Deluzio KJ, Caldwell GE, Dunbar MJ. Biomechanical changes at the hip, knee, and ankle joints during gait are associated with knee osteoarthritis severity. J Orthop Res. 2008;26:332–41. doi: 10.1002/jor.20496. [DOI] [PubMed] [Google Scholar]
- 11.Jordan JM, Helmick CG, Renner JB, Luta G, Dragomir AD, Woodard J, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2007;34:172–80. [PubMed] [Google Scholar]
- 12.Jordan JM, Linder GF, Renner JB, Fryer JG. The impact of arthritis in rural populations. Arthritis Care Res. 1995;8:242–50. doi: 10.1002/art.1790080407. [DOI] [PubMed] [Google Scholar]
- 13.Zhang Y, Niu J, Felson DT, Choi HK, Nevitt M, Neogi T. Methodologic challenges in studying risk factors for progression of knee osteoarthritis. Arthritis Care Res (Hoboken) 2010;62:1527–32. doi: 10.1002/acr.20287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rogers WH. Regression standard errors in clustered samples. Stata Technical Bulletin. 1993;13:19–23. [Google Scholar]
- 15.Wise BL, Kritikos L, Lynch JA, Liu F, Parimi N, Tileston KL, et al. Proximal femur shape differs between subjects with lateral and medial knee osteoarthritis and controls: the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2014;22:2067–73. doi: 10.1016/j.joca.2014.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Neame R, Zhang W, Deighton C, Doherty M, Doherty S, Lanyon P, et al. Distribution of radiographic osteoarthritis between the right and left hands, hips, and knees. Arthritis Rheum. 2004;50:1487–94. doi: 10.1002/art.20162. [DOI] [PubMed] [Google Scholar]
- 17.Chitnavis J, Sinsheimer JS, Suchard MA, Clipsham K, Carr AJ. End-stage coxarthrosis and gonarthrosis. Aetiology, clinical patterns and radiological features of idiopathic osteoarthritis. Rheumatology (Oxford) 2000;39:612–9. doi: 10.1093/rheumatology/39.6.612. [DOI] [PubMed] [Google Scholar]
- 18.Kopec JA, Sayre EC, Schwartz TA, Renner JB, Helmick CG, Badley EM, et al. Occurrence of radiographic osteoarthritis of the knee and hip among african americans and whites: a population-based prospective cohort study. Arthritis Care Res (Hoboken) 2013;65:928. doi: 10.1002/acr.21924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shakoor N, Hurwitz DE, Block JA, Shott S, Case JP. Asymmetric knee loading in advanced unilateral hip osteoarthritis. Arthritis Rheum. 2003;48:1556–61. doi: 10.1002/art.11034. [DOI] [PubMed] [Google Scholar]