Abstract
BACKGROUND
Anabolic steroids have been widely used in recent years. It could adversely affect the cardiovascular system. Non-traditional risk factors for coronary heart diseases (CHDs) have raised great concern.
CASE REPORT
A young bodybuilder was presented with crushing retrosternal chest pain, excessive diaphoresis, and vomiting. The symptoms began during wrestling. The patient did not have a history of traditional cardiovascular risk factors. He was using large quantities of nutritional and bodybuilding supplements with multiple intramuscular injections of dexamethasone during past 6 months. The electrocardiography (ECG) revealed ST-segment elevation in the precordial, I and aVL leads consistent with acute extensive myocardial infarction (MI). Lipid profile, cardiac troponin, and creatine phosphokinase-MB (CPK-MB) was abnormal. Transthoracic echocardiography (TTE) revealed mild left ventricular (LV) enlargement and reduced global systolic dysfunction with regional wall akinesia. The patient received thrombolytic therapy which was resulted in symptomatic relief and resolution in ST-T changes. Significant smoke was seen in LV cavity without clot formation on the discharge day. About 1 week later, large fresh clots were seen in the apex. He was admitted again, and the burden of clots was reduced significantly after initiation of oral warfarin. Other laboratory tests were as follows: High-sensitivity C-reactive protein (CRP): 25.9 mg/dl, homocysteine: 26.2 µmol/l. The patient was discharged with specific medication. Clots were disappeared after 6 weeks of warfarin therapy. Later, the patient was evaluated again, and there was not any symptom and LV clots.
CONCLUSION
Hyperhomocysteinemia could be induced by steroid abuse and may cause atherosclerotic and thrombotic effects in healthy athletes. We suggest clinicians to take a careful history of young athletes presented with MI or thrombotic events and also pay special attention to their homocysteine levels in their follow-ups.
Keywords: Hyperhomocysteinemia, Anabolic Agents, Thrombosis
Introduction
Although the importance of conventional risk factors is well established, it is commonly suggested that more than 50% of patients with coronary heart disease (CHD) lack any of the conventional risk factors. This claim implies that other factors play a significant role in CHD and have led to considerable interest in non-traditional risk factors and genetic causes of CHD.1
Hyperhomocysteinemia has been proposed as a risk factor for increased tendency of vessel thrombosis and cardiac ischemia.2,3 Elevated levels of homocysteine can also affect coagulation cascade or even cause multivessel coronary artery disease.3,4 On the other hand, anabolic androgenic steroids can directly affect cardiovascular system by inducing left ventricular (LV) hypertrophy and dysfunction or even indirectly causing hyperhomocysteinemia.5 Here, we discuss a 23-year-old male wrestler with a 6 months history of excessive anabolic steroid use presenting with crushing retrosternal chest pain.
Case Report
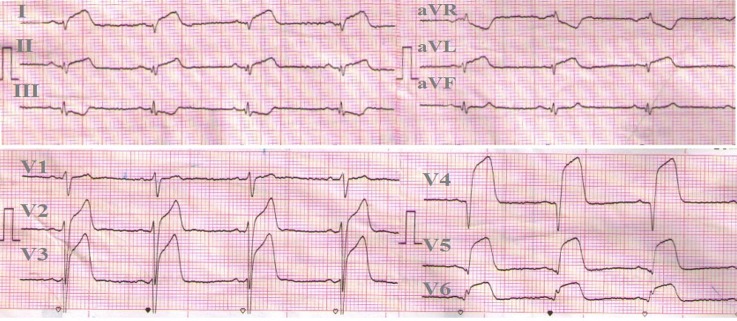
The 23-year-old man was referred to the emergency department with a 4 hours history of crushing retrosternal chest pain, excessive diaphoresis, and vomiting. The symptoms began during wrestling. The patient had a previous history of retrosternal chest discomfort ascribed to gastric upset which always relieved spontaneously. He did not have traditional cardiovascular risk factors (cigarette smoking, diabetes, and hypertension). The patient was a bodybuilder and wrestler, who was continually using large quantities of nutritional and bodybuilding supplements with multiple intramuscular injections of dexamethasone during past 6 months. The vital signs were as follows on admission: Blood pressure: 140/90 mmHg, pulse rate of 72/minutes, respiratory rate: 14/minutes. The third and fourth heart sounds were prominent. The electrocardiography (ECG) which was recorded in emergency room revealed ST-segment elevation in the precordial, I and aVL leads consistent with acute extensive myocardial infarction (MI) (Figure 1).
Figure 1.
Twelve-leads electrocardiogram revealed significant ST elevation in precordial (tombstone sign), I and aVL leads (compatible with acute extensive anterior myocardial infraction)
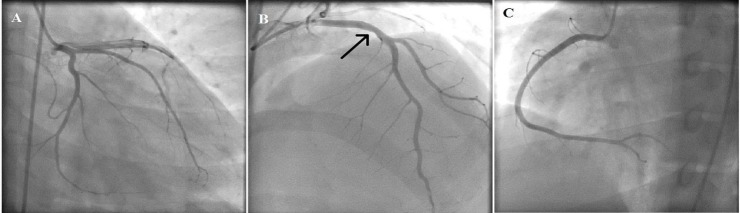
Increased serum level of cardiac troponin was detected. Lipid profile was abnormal [high-density lipoprotein (HDL): 20 mg/dl, low-density lipoprotein (LDL): 101 mg/dl, triglycerides (TG): 305 mg/dl, cholesterol: 317 mg/dl]. Transthoracic echocardiography (TTE) revealed mild LV enlargement and reduced global systolic function (ejection fraction: 35-40%) with akinesia of all apical segments and mid-anterior and anteroseptal regions. The door to needle-door to balloon time was estimated to be long lasting. Hence, thrombolytic (streptokinase) was prescribed which was resulted in symptomatic relief and resolution in ST-T changes. About 4 days later, coronary angiography was done, showing non-significant stenosis in mid portion of left anterior descending artery (Figure 2). In the last day of admission, significant smoke was seen in LV cavity without clot formation.
Figure 2.
(A, B and C) Coronary angiography showing just a non-significant lesion in mid portion of left anterior descending (arrow in B), Left circumflex and right coronary artery were normal
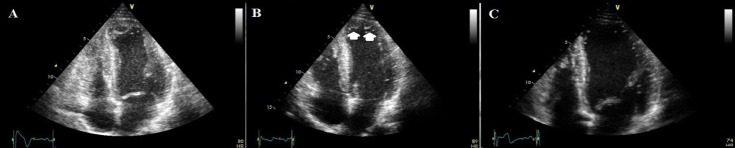
The patient was reassessed 1 week after discharge and TTE was done. LV ejection fraction was 40%, and large fresh clots were seen in the apex (Figure 3-A). He was admitted again for better cardiac monitoring and initiation of anticoagulation. The size of the clots was reduced significantly after initiation of oral warfarin (Figure 3-B). Other laboratory tests were as follow: High-sensitivity C-reactive protein (CRP): 25.9 mg/dl, homocysteine: 26.2 µmol/l. The patient was discharged on warfarin, folic acid, vitamin B12 in addition to carvedilol, atorvastatin, losartan, and low dose furosemide. In the follow-up visits, the patient underwent echocardiography. The clots were disappeared after 6 weeks of warfarin therapy (Figure 3-C).
Figure 3.
Echocardiographic images in apical four chamber views, (A) Large fresh clots in the apex (1 week later), (B) arrows denting the residual but small clots and (C) no residual clots
Six months later, the patient was evaluated again and there was not any symptom and the LV clots were disappeared. Serum level of homocysteine was within the normal limits. Vitamin B12 and folic acid drugs were discontinued. During 3 years follow-up, there was not any clot formation in LV cavity in TTE and the patient had occasionally non-angina chest pain, exertional dyspnea (New York Heart Association I/II) without worsening of global LV function or any thromboembolic events. Lipid profile was normal in repeated assessment. The patient is now taking carvedilol, captopril, aspirin, atorvastatin, spironolactone, and warfarin and involved regularly in cardiac rehabilitation programs.
Discussion
In this report, we presented a case of acute chest pain in a young wrestler who uses bodybuilding supplements and intramuscular dexamethasone. ECG, echocardiographic and laboratory data were considered to be a more compatible with MI. However, not every chest pain and rises in cardiac biomarkers are due to acute coronary syndromes. Chest pain with associated increase in cardiac biomarker could be found in acute pulmonary embolism. ECG and echocardiographic findings were not compatible with such diagnosis in this patient. Myocarditis should also be considered as a possible diagnosis in young patients with acute coronary syndrome presentation especially in the absence of atherosclerosis risk factors or with normal coronary angiogram. In one series of patients with chest pain and ECG abnormalities, 32% of the cases have myocarditis on myocardial biopsy.6 Wall motion abnormalities could also be seen in echocardiography in myocarditis, but it is more global rather than segmental. ECG abnormalities or segmental distribution of wall motion abnormalities extend beyond a single coronary artery territory in the typical cases.7 This was in contrary to the presented case in which the ECG changes and regional wall motion abnormalities were comparable and suggesting the involvement of anterior coronary circulation.
Anabolic steroids have various effects on cardiovascular system. Atherosclerosis, systemic hypertension, impaired diastolic, and systolic ventricular function and disturbances in lipid metabolisms have all been reported with anabolic steroid abuse.8 Increased platelet activity is also observed in such patients, and might be responsible for MI or even stroke.8
There are many cases of androgenic anabolic steroid abuse in young athletes showing cardiovascular problems such as MI or thrombosis of different vessels such as renal artery.5
LV dysfunction is the other effect of long-term androgenic anabolic steroid abuse and could increase the risk of sudden death in these patients.9 Pathologic studies in such patients revealed small arteriole wall thickening and intimal hyperplasia, which could be responsible for causing ischemic myocardial damage and subsequent ventricular dysfunction.10
Use of anabolic steroid can induce acute hyper homocysteinemia and associated thrombotic events.2 A higher level of homocysteine could be seen with lower HDL concentration, higher plasma LDL, and triglycerides.5
Homocysteine is a sulfhydryl amino acid, absent in human natural dietary sources.11 It can be toxic to endothelial cells leading to the smooth muscle proliferation in vessel wall and affecting the coagulation cascade.3 Multivessel coronary artery disease and acute MI have been reported in the setting of the high level of homocysteine.4 Anabolic steroids can affect the absorption of B6 and B12 vitamins and cause an elevation in homocysteine levels.12 This effect might be responsible for the elevation of homocysteine levels in our patient; causing potential stenosis and thrombosis.
While administration of folate supplement is somehow controversial, normalizing plasma homocysteine levels with healthy diet containing vegetables and fresh fruits accompanied by moderate exercise is more favorable.11 Administration of high dose of vitamin B6 with folic acid after acute MI does not reduce the risk of death or recurrence of cardiovascular disease.13 On the other hands, it can adversely affect myocardial repair and increase morbidity and mortality among patients with cardiovascular disease.13
Use of anabolic steroid in young athletes is an important issue for clinicians. These substances have various effects on the cardiovascular system as well as other organs. Hyperhomocysteinemia could be induced by steroid abuse and may have atherosclerotic and thrombotic effects in healthy athletes. However, if a patient has the previous hyperhomocysteinemia, the risk of catastrophic cardiovascular events might be higher. We suggest clinicians to take history of young athletes presented with MI or thrombotic events carefully and also pay special attention to the homocysteine levels in their follow-up visits.
Acknowledgments
None.
Footnotes
Conflicts of Interest
Authors have no conflict of interests.
REFERENCES
- 1.Amoozgar H, Soltani M, Besharati A, Cheriki S. Undiagnosed anemia in pediatric patients with congenital heart diseases. Int Cardiovasc Res J. 2011;5(2):70–1. [Google Scholar]
- 2.Ebenbichler CF, Kaser S, Bodner J, Gander R, Lechleitner M, Herold M, et al. Hyperhomocysteinemia in bodybuilders taking anabolic steroids. Eur J Intern Med. 2001;12(1):43–7. doi: 10.1016/s0953-6205(00)00131-x. [DOI] [PubMed] [Google Scholar]
- 3.Perna A, Ingrosso D, de Santo NG. Homocysteine and oxidative stress. Amino Acids. 2003;25(3):409–17. doi: 10.1007/s00726-003-0026-8. [DOI] [PubMed] [Google Scholar]
- 4.Eftychiou C, Antoniades L, Makri L, Koumas L, Costeas PA, Kyriakou E, et al. Homocysteine levels and MTHFR polymorphisms in young patients with acute myocardial infarction: a case control study. Hellenic J Cardiol. 2012;53(3):189–94. [PubMed] [Google Scholar]
- 5.Nockels K. Invalid citation [Online]. 2012. Available from: URL: http://community.thomsonreuters.com/t5/EndNote-General/INVALID-CITATION/td-p/33811.
- 6.Dec GW, Waldman H, Southern J, Fallon JT, Hutter AM, Palacios I. Viral myocarditis mimicking acute myocardial infarction. J Am Coll Cardiol. 1992;20(1):85–9. doi: 10.1016/0735-1097(92)90141-9. [DOI] [PubMed] [Google Scholar]
- 7.Magnani JW, Dec GW. Myocarditis: current trends in diagnosis and treatment. Circulation. 2006;113(6):876–90. doi: 10.1161/CIRCULATIONAHA.105.584532. [DOI] [PubMed] [Google Scholar]
- 8.Vanberg P, Atar D. Androgenic anabolic steroid abuse and the cardiovascular system. Handb Exp Pharmacol. 2010;(195):411–57. doi: 10.1007/978-3-540-79088-4_18. [DOI] [PubMed] [Google Scholar]
- 9.Baggis AL, Weiner RB, Kanayama G, Hudson JI, Picard MH, Hutter AM, et al. Long term anabolic-androgenic steroid use is associated with left ventricular dysfunction. Circ Heart Fail. 2010;3:472–6. doi: 10.1161/CIRCHEARTFAILURE.109.931063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.di Paolo M, Agozzino M, Toni C, Luciani AB, Molendini L, Scaglione M, et al. Sudden anabolic steroid abuse-related death in athletes. Int J Cardiol. 2007;114(1):114–7. doi: 10.1016/j.ijcard.2005.11.033. [DOI] [PubMed] [Google Scholar]
- 11.Eldibany MM, Caprini JA. Hyperhomocysteinemia and thrombosis: an overview. Arch Pathol Lab Med. 2007;131(6):872–84. doi: 10.5858/2007-131-872-HATAO. [DOI] [PubMed] [Google Scholar]
- 12.Hartgens F, Kuipers H. Effects of androgenic-anabolic steroids in athletes. Sports Med. 2004;34(8):513–54. doi: 10.2165/00007256-200434080-00003. [DOI] [PubMed] [Google Scholar]
- 13.Bonaa KH, Njolstad I, Ueland PM, Schirmer H, Tverdal A, Steigen T, et al. Homocysteine lowering and cardiovascular events after acute myocardial infarction. N Engl J Med. 2006;354(15):1578–88. doi: 10.1056/NEJMoa055227. [DOI] [PubMed] [Google Scholar]