Abstract
Objective
Psychological distress may contribute to chronic activation of acute-phase inflammation. The current study investigated how financial stressors influence psychosocial functioning and inflammation. This study examined 1) the direct relations between financial stress and inflammation, 2) whether the relationships between financial stress and inflammation are mediated in part by negative interpersonal events, psychological distress, and psychological well-being, and 3) whether social standing in one’s community moderates the relations between financial stress and psychological distress, psychological well-being, and markers of inflammation (interleukin-6 and C-reactive protein).
Methods
Stressful financial and interpersonal events over the previous year, perceived social status, indices of psychological well-being and distress, and levels of interleukin-6 and C-reactive protein were assessed in a community sample of 680 middle-aged adults (ages 40–65).
Results
Structural equation modeling analyses revealed significant relations among financial stress, interpersonal stress, and psychological distress and well-being, and complex relationships between these variables and inflammatory markers. Psychological well-being mediated the association between financial stress and IL-6 ([mediation] ab = .012, SE = .006, p = .048). Furthermore, individuals with higher perceived social standing within their communities exhibited a stronger relation between negative financial events and both interpersonal stressors (interaction B = .067, SE = .017, p < .001) and C-reactive protein (interaction B = .051, SE = .026, p = .050).
Conclusions
Financial stress demonstrates complex relations with inflammation, due partly to psychological well-being and social perceptions. Findings are discussed with regard to the social context of stress and physiological factors pertinent to stress adaptation and inflammation.
Keywords: Financial stress, positive emotions, inflammation, social status
Although a link has been established between psychological stress and illness, questions remain regarding how psychological stress gets under the skin. The impact of stress on physical factors such as inflammation is complex, as it is influenced by contextual factors in the social environment. Social relationships predict psychological distress (1) and physical health (2), and one’s social environment can modify the experience of life stress (3). Community factors, such as social status within the community and exposure to social stress, also contribute to psychological well-being (4,5). One mechanism through which the broader social environment influences psychological states is interpersonal relations, which show a reciprocal relationship with characteristics of the individual. Interactions with others may increase the distress or well-being of an individual; conversely, current psychological states may influence ongoing interpersonal relationships. The purpose of the present study was twofold. First, we examined whether the relationship between financial stress and inflammation is mediated by negative interpersonal events, psychological distress, and psychological well-being. Second, we investigated whether perceived social status moderates the relations between financial stress and interpersonal stress, psychological distress, psychological well-being, and inflammation.
Psychological stress, financial stress, and inflammation
Psychological stress appears to induce an acute-phase physiological response by activating cytokines like interleukin-6 (IL-6) (6). IL-6 is a pro-inflammatory cytokine that has been found in higher concentrations in individuals exposed to experimental stress inductions (7) and in individuals facing chronic stressors such as prolonged interpersonal difficulties (8). IL-6 is implicated in the activation of acute-phase inflammatory processes, which increases synthesis of inflammatory markers like C-reactive protein (CRP) (9). CRP is a protein found in blood plasma that has been implicated in poor cardiac health (10) and has been found in increased concentrations in individuals experiencing chronic interpersonal stressors (8) and those suffering from burnout, depression, and anxiety (9). Chronic activation of acute-phase stress responses by psychological stressors thus appears to contribute to poorer long-term health (6). As psychological stressors have notable consequences for inflammation, it is worthwhile to examine whether financial stress, a prevalent challenge in the wake of the Great Recession (11), might demonstrate similar consequences.
Financial stress predicts a myriad of psychological difficulties, including greater psychological distress (12) and increased difficulties with family members, friends, and in the workplace (13). Similarly, financial hardships uniquely contribute to poorer physical health in community samples (2). Financial hardship may also limit exposure to resources important for development throughout the lifespan, and may erode protective psychological factors such as self-esteem (13).
Mediating and moderating pathways linking financial stress and inflammation
Social factors are also important in understanding the mediational pathway from stress to physical health (14) as well as stress buffering (15). Human laboratory research suggests that negative social interactions may be an important stimulus for acute changes in inflammatory responding. For example, conflictual marital interactions are associated with increases in the concentration of circulating inflammatory markers (16). Similarly, studies have linked poor psychological functioning with higher levels of inflammation, as measured by CRP, interleukin-6, and fibrinogen (17,18). Little is known, however, about whether similar interpersonal and psychological factors account for the association between financial stress and inflammation. Financial events strain relationships among family members who must make ends meet and who face the prospect of an uncertain future. Thus, negative financial events may spill over and trigger negative interpersonal events which, in turn, influence physical processes such as inflammation.
Another social factor that may influence the consequences of financial stress for emotional and physical health is perceived social status. Perceptions of social rank within one’s community have been shown to affect social cognition, emotional functioning, and social behavior (5), as well as physical health (19). However, the evidence regarding the directionality of these effects is mixed. Although perceptions of lower socioeconomic status adversely affect physical and psychological health (20), physical health may also affect concurrent perceptions of social status (19). Thus, these factors may share a mutually influential relationship across time. In the current study we investigated whether perceptions of social status moderate the effects of financial stress. More specifically, we examined whether individuals with lower or higher perceived social standing are more vulnerable to the inimical effects of financial stressors.
Study hypotheses
We utilized biological assays and questionnaire data from a community-based sample of 688 middle-aged adults to examine the relationships between financial stress, social standing, and markers of inflammation. The goal of the parent study was to examine candidate measures of resilience and their utility in predicting physical and emotional functioning, above and beyond the effects of risk factors for disease and psychological difficulties in a representative sample of middle-aged men and women drawn from 40 census neighborhoods in the metropolitan area of Phoenix, Arizona. First, we examined the direct relations between stressful financial events over the previous year and indices of psychological distress (ratings of current anxious and depressive symptomatology and current levels of negative affect), psychological well-being (ratings of well-being, positive emotion, and vitality), and inflammation. As psychological distress and well-being have different antecedents (21,22) and consequences for health (23), independent representation of these constructs was deemed necessary for the current study. We expected that the occurrence of major financial stressors would predict greater psychological distress, lower psychological well-being, and greater inflammatory activity (characterized by elevated levels of IL-6 and CRP). Second, we hypothesized that stressors in interpersonal domains over the previous year would serve as an intervening variable between financial stressors and psychological distress, psychological well-being, and inflammation. Similarly, we predicted that both psychological distress and well-being would account for a significant proportion of the relation between negative financial events and inflammation. We tested these relations while controlling for demographic differences, health conditions, and medication use that could potentially contribute to differences in inflammation.
Third, we utilized a self-report measure of perceived social status as a moderator of the relations between financial stress and physical and psychological functioning. We assume that the adverse impact of financial stress on indices of interpersonal stress, distress, well-being and inflammation varies according to who feels most threatened by them. On one hand, perceiving oneself at a lower social position within the surrounding community could potentiate the detrimental effects of financial stressors due to a perceived inability to sustain oneself in the faces of such losses. On the other hand, individuals in higher positions might react more poorly to financial stressors, as these individuals might view themselves as having more to lose.
Methods
Participants
688 middle-aged adults between the ages of 40 and 65 years old were recruited from the Phoenix, Arizona metropolitan area between 2007 and 2012. The average age of participants in the current sample was 53.91 years (SD = 7.232). Women comprised 52.3% of the sample (360 participants), 46.9% of the sample (323 participants) was male, and 0.8% of the sample (5 participants) did not report their gender. The median household income in the current study was between $50,000 and $65,000 per year, consistent with US Census Bureau data for median household income in Arizona between 2008 and 2012 (24). Nearly half (49.1%) of the sample was married. A majority (61.8%) of the sample reported being employed, and 47.1% of the sample reported working 35 hours or more each week. With respect to ethnicity, 73.6% of the sample self-identified as Caucasian, 13.8% as Hispanic, 3.1% as African American, 1.7% as Asian, and 1.4% as Native American or American Indian. Ethnic categories were not mutually exclusive, and 12.1% of the sample reported membership in more than one ethnic group. Regarding medical conditions, 203 participants reported receiving treatment for a cardiovascular condition at the time of data collection, 81 participants reported being treated for arthritis, 74 participants reported being currently treated for diabetes, and 11 participants reported current treatment for cancer. These categories were overlapping: 71 participants reported being treated for two of these conditions, and 13 participants reported concurrent treatment for three of these conditions. 8 participants were excluded from the final analysis due to IL-6 and CRP values above cutoffs, resulting in a final sample of 680 participants.
Procedure
All procedures were approved by the Institutional Review Board at Arizona State University, and all participants provided informed consent prior to the study. Participants were required to be between the ages of 40 and 65 and to primarily reside in the Phoenix metropolitan area. They were recruited from multiple Census tracts in the Phoenix, Arizona metropolitan area. After providing consent, participants were asked to complete a series of questionnaires and a phone interview, in which they reported the incidence of stressful events related to their finances, their interactions with friends, family, significant others, and co-workers, and their current levels of physical, social, and psychological functioning. Current medication lists and markers of inflammation were obtained from blood and saliva samples drawn during a visit to participants’ homes by a research phlebotomist. Participants were asked to fast for at least 8 hours prior to blood sampling (90.3% compliance). Blood samples were drawn between 7:30 am and 8:00 pm, with the majority of samples drawn between 7:30 and 9:59 am (N=382; 59%), with remaining samples taken between 10:00 am and 11:59 am (N=185; 28.5%), 12:00 pm and 1:59 pm (N=27; 4%), 2:00 pm and 3:59 pm (N=21; 3.2%), 4 pm and 5:59 pm (N=22; 3.4%), and after 6:00 pm (N =12; 2%). Samples were transported to the laboratory on ice, and were processed within two hours of blood sampling.
Measures
Negative financial events
Major financial stressful events over the previous year were assessed using the financial stress subscale of the Psychiatric Epidemiology Research Interview (PERI) Life Events Scale (25). The frequency of endorsement for each item can be found in Table 1. 422 participants reported no negative financial events over the past year, 127 participants reported one negative financial event, 61 participants reported 2 negative financial events, 34 participants reported 3 negative financial events, 21 participants reported 4 negative financial events, 9 participants reported 5 negative financial events, one participant endorsed 6 major financial events over the previous year, and 5 participants did not complete this assessment. The internal consistency of the six-item PERI financial stress subscale was acceptable (α = .714).
Table 1.
Frequency table of major financial events
| Event | Frequency (Percent of participants who endorsed event) |
|---|---|
| Have a major worsening of financial condition | 173 (25.4%) |
| Been pressured to pay bills by stores, creditors, or bill collectors | 125 (18.4%) |
| Been unable to pay for medication or other medical necessities | 84 (12.4%) |
| Fallen behind in paying the rent or mortgage | 72 (10.6%) |
| Been unable to purchase needed food | 38 (5.6%) |
| Had a car, furniture, or some items bought on an installment plan repossessed | 20 (2.9%) |
Note: Frequency percentage based on responses from 680 participants
Negative interpersonal events
Stressful interpersonal events were measured using items from the PERI detailing stressful events with spouses (6 items), family members (6 items), co-workers (5 items), and social events (3 items). The complete list of negative interpersonal events is available as an online appendix (Supplemental Digital Content 1). As these items reflect non-overlapping domains of functioning and were compiled as a general measure of interpersonal stress, the internal consistency of this measure was low, as expected (Cronbach’s α = .558).
Perceived social status
Perceived social status was measured using the MacArthur Scale for Subjective Social Status (20). Participants rated where they felt they ranked in their communities on a scale from 1 (“Lowest standing/worst off”) to 10 (“Highest standing/best off”) relative to their community peers. The test-retest reliability of this measure has been established (26), and it has been used in previous studies assessing subjective social status and health outcomes (20, 26).
Vitality
Vitality subscale scores from the Short Form Health Survey (SF-36) (22) were computed using a mean of 4 items reflecting self-rated feelings of energy over the past 4 weeks (27). The 4-item Vitality composite score showed good internal consistency (Cronbach’s α = .844).
Mental well-being
The 5-item World Health Organization Well-Being Index (WHO-5) was used to measure current mental well-being (e.g., “I have felt cheerful and in good spirits”, “I have felt active and vigorous”) (28). WHO-5 scale items were modified to reflect functioning over the past 4 weeks. The internal consistency of this measure was good (Cronbach’s α = .864).
Positive and negative affect
Positive and negative affect scores were computed using the Positive Affect-Negative Affect Schedule (PANAS) (29). Participants were asked to rate the extent to which they experienced each of 10 positive mood adjectives and 10 negative mood adjectives over the past 7 days, on a 5-point scale from 1 “very slightly or not at all” to 5 “extremely.” Both the negative affect scale (Cronbach’s α = .881) and the positive affect scale (α = .874) showed adequate internal consistency.
Anxiety and depression
Anxiety was assessed using a composite of 3 items from the 18-item Mental Health Inventory (MHI-18) (30) measuring feelings of anxiety, nervousness, and difficulty with relaxation and one item from the original 38-item MHI (22) assessing feelings of being bothered by nervousness. This measure showed adequate model fit when these items were included in a one-factor confirmatory factor analysis and showed convergence with both neuroticism scores (r = .496, p < .001) from the Five-Factor Inventory (31) and a sum of anxiety symptoms (r = .354, p < .001) from the Structured Clinical Interview for DSM-IV disorders (32). Depression scores were computed using the 4-item depression subscale of the MHI (30). All anxiety and depression items assessed the occurrence of symptoms over the previous 4 weeks. Both the anxiety composite score (Cronbach’s α = .830) and the depression composite score (Cronbach’s α = .890) showed adequate internal consistency.
Inflammation
To quantify levels of IL-6 and CRP, 10ml of blood were collected into EDTA tubes (Becton–Dickinson, Franklin Lakes, NJ), held on ice, and centrifuged within 2 hours of collection for 15 minutes at 1500g. Plasma was then aspirated, aliquoted, and frozen at −80 °C until assay. Plasma levels of IL-6 were quantified using Quantikine High Sensitivity human IL-6 kits (R&D Systems, Inc., Minneapolis, MN), an enzyme-linked immunosorbent assay (33) with an intra-assay coefficient of variation of 4% and inter-assay coefficient of variation of 10%. The minimal detectable level of IL-6 was 0.156 pg/ml. CRP was measured using the Dade Behring N High Sensitivity CRP turbidimetric immunoassay (Dade Behring Diagnostics, Marburg, Germany) on the BN ProSpec. We excluded data from 8 participants with both IL-6 values above 10 pg/ml and CRP values above 10mg/L, in order to rule out participants who were likely to be experiencing an acute infection at the time of data collection (34). To address non-normal distribution, IL-6 and CRP variables were transformed using a natural log function.
Medications
Medication use was coded using separate binary variables representing use of at least one anti-inflammatory medication or at least one steroid medication versus those who did not use any of these medications. A full list of the anti-inflammatory and steroid medications assessed in the current study can be found in an online appendix (Supplemental Digital Content 1).
Medical conditions
Four binary variables were created that represented whether participants endorsed currently being treated for a cardiovascular illness, arthritis condition, diabetes, and cancer. A count variable was then computed that reflected the total number of current medical conditions for each participant.
Body mass index
Participant weight (in kilograms) and height scores (in meters) were used to compute body mass index (BMI) scores.
Analytic Plan
All analyses were conducted using Mplus software (35). Structural equation models were estimated to test negative financial events as a predictor of the number of negative interpersonal events over the previous year, latent psychological distress and latent well-being variables, and IL-6 and CRP. For the psychological distress latent variable, the indicators were observed scores on the PANAS negative affect and MHI Depression and Anxiety scales. For the psychological well-being latent variable, the indicators were observed scores on the PANAS positive affect scale, MHI positive emotion scale, and the SF-36 Vitality subscale. These models were constructed as a mediation model using the ab product coefficient, where the a path refers to the relation between a predictor and a mediator and the b path refers to the relation between a mediator and an outcome. Perceived social status was tested as a moderator of the relations between financial stress, interpersonal stress, and all outcome variables.
Anti-inflammatory and steroid medication use and body mass index (BMI) were entered as covariates in paths involving inflammatory markers, and all paths were tested using age, gender, education, income, employment status, and marital status as covariates. These covariates were entered as predictors in the structural model, but were not depicted in our final model for the purposes of visual clarity. As concurrent medical illnesses could meaningfully alter inflammatory processes, we examined differences in IL-6 and CRP according to the presence of cancer, arthritis, diabetes, and cardiovascular illness, which was modeled in all paths involving IL-6 and CRP. Finally, as some participants had their blood drawn at different times throughout the day, we included time of blood sampling as a covariate in all paths involving IL-6 and CRP.
As the financial events and negative interpersonal events variables were count variables (i.e., non-negative integer scores) and do not follow a normal distribution, we specified a zero-inflated Poisson distribution for paths including either negative financial events or negative interpersonal events. However, use of the Poisson distribution in structural equation models precludes the computation of traditional goodness of fit indices. To provide a rough estimate of model fit, the fully specified model was run with negative financial events and negative interpersonal events specified as continuous variables instead of count variables. These indices were meant as a general reflection of model fit and should be interpreted with the caveat that the model includes additional error due to this classification of the financial and interpersonal event variables. Adequacy of model fit was determined using the chi-square test of model fit, comparative fit index (CFI), Tucker Lewis Index (TLI), the root mean square error of approximation (RMSEA), and the standardized root-mean-square residual (SRMR). Scores of .90 or higher on the CFI and scores under .05 for RMSEA and SRMR parameters were used as benchmarks to determine good model fit (36).
Results
Descriptive statistics of all study variables can be found in Table 2, and bivariate (Pearson r) correlations between study variables can be found in Table 3.
Table 2.
Descriptive Statistics for Study Variables
| Study Variable | Mean (Standard Deviation) |
|---|---|
| Negative Financial Events | 0.72 (1.17) |
| Negative Interpersonal Events | 2.64 (2.51) |
| Perceived Social Status | 6.14 (1.81) |
| MHI-Anxiety | 2.14 (0.96) |
| MHI-Depression | 1.86 (0.93) |
| PANAS Negative Affect | 1.62 (0.60) |
| PANAS Positive Affect | 3.29 (0.72) |
| WHO Well-Being | 4.14 (1.11) |
| SF-36 Vitality | 63.39 (21.28) |
| C-Reactive Protein | 4.17 (7.33) |
| Interleukin-6 | 2.36 (3.93) |
Note: Scores based on responses from 680 participants
Table 3.
Bivariate Correlations for All Study Variables
| NFE | NIE | PSS | MHIA | MHID | NAFF | PAFF | WHO | VIT | IL-6 | CRP | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| NFE | 1 | .550** | −.330** | .314** | .344** | .313** | −.175** | −.322** | −.262** | .128 | .027 |
| NIE | 1 | −.266** | .328** | .377** | .362** | −.144** | −.313** | −.282** | .081 | .009 | |
| PSS | 1 | −.222** | −.217** | −.207** | .270** | .328** | .255** | −.077 | −.002 | ||
| MHIA | 1 | .701** | .753** | −.362** | −.562** | −.497** | .070 | −.031 | |||
| MHID | 1 | .732** | −.422** | −.598** | −.531** | .070 | −.016 | ||||
| NAFF | 1 | −.307** | −.732** | −.470** | .108** | −.010 | |||||
| PAFF | 1 | .636** | .520** | −.091* | −.094* | ||||||
| WHO | 1 | .782** | −.159** | −.092* | |||||||
| VIT | 1 | −.185** | −.091 | ||||||||
| IL-6 | 1 | .281** | |||||||||
| CRP | 1 |
NFE = Negative Financial Events, NIE = Negative Interpersonal Events, PSS = Perceived Social Status, MHIA = Mental Health Inventory – Anxiety, MHID = Mental Health Inventory – Depression, WHO = WHO Well-being Scale, VT = Vitality, PAFF = PANAS Positive Affect, NAFF = PANAS Negative Affect, IL-6 = Interleukin-6, CRP = C-Reactive Protein
Note:
p < .01,
p < .05
Non-Moderated Models
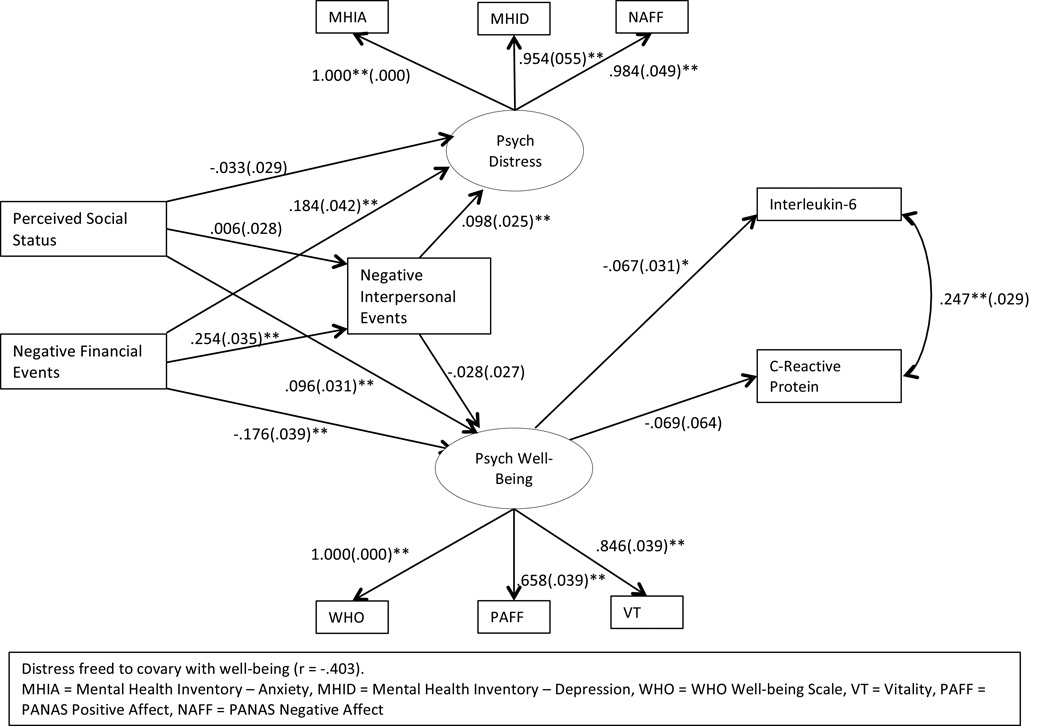
The results of the non-moderated model can be seen in Figure 1 (N=680); all path estimates are presented as unstandardized path coefficients. Individuals who experienced more negative financial events reported significantly more negative interpersonal events over the same period, greater psychological distress, and lower psychological well-being. Negative financial events did not significantly predict IL-6 levels (B = -.025, SE = .026, p = .34) or CRP levels (B = -.095, SE = .049, p = .053) in the fully specified model. Negative interpersonal events over the past year were significantly and positively related to psychological distress but were unrelated to psychological well-being. As negative interpersonal events were unrelated to levels of IL-6 (B = .010, SE = .016, p = .52) or CRP (B = .033, SE = .030, p = .28), these paths were excluded from the final model. Perceptions of higher social status were positively associated with psychological well-being, but were unrelated to negative interpersonal events, psychological distress, or IL-6 or CRP levels. The paths involving the perceived social status variable to each outcome were retained in the final model, however, as they were necessary to compute moderation effects. Greater scores on psychological well-being predicted lower levels of IL-6, but not CRP. Unexpectedly, psychological distress was unrelated to both IL-6 and CRP (p > .30 in both cases), so these paths were excluded from the final estimated model. As expected, distress and well-being showed a significant negative correlation.
Figure 1.
Measurement and path model for the relations between financial and interpersonal stress, perceived community social status, psychological distress and well-being, and inflammation.
Note: Covariates were estimated in this model, but are not depicted.
Note: Path estimates are unstandardized and presented with a path coefficient with the standard error in parentheses.
Participants with diabetes showed significantly higher values on IL-6 (t(534) = −4.720, p < .001) and CRP (t(534) = −2.401, p = .016). Similarly, participants with arthritis had significantly higher IL-6 (t(534) = 2.509, p = .012) and CRP values (t(534) = 2.932, p = .004) than those without arthritis. Individuals with a current cardiovascular condition also reported higher levels of IL-6 (t(534) = 4.087, p < .001) and CRP (t(534) = 3.331, p = .001). The time at which blood samples were collected was a significant predictor of CRP levels (B = .052, SE = .023, p = .022), but did not significantly predict IL-6 levels (B = .009, SE = .012, p = .46). The time of sample collection was unrelated to the employment status of participants (t(600) = .591, p = .55). Several differences were found for the 68 participants who demonstrated levels of IL-6 above 10 pg/ml or CRP values above 10mg/L. These participants reported a significantly higher number of financial stressors (t(77.01) = −2.216, p = .030), scored significantly lower on the well-being factor (t(77.41) = 2.946, p = .004), and also reported a lower range of family income on average (t(78.49) = 2.059, p = .043). These participants did not differ in their scores on the distress factor, age, or in their ratings of subjective social status, however.
Regarding mediation analyses, negative interpersonal events mediated the relation between negative financial events and the latent psychological distress variable (ab = .033, SE = .009, p < .001), but did not mediate the relation between negative financial events and psychological well-being (ab = −.009, SE = .009, p = .30). Psychological well-being mediated the relationship between negative financial events and IL-6 (ab = .012, SE = .006, p = .048) but not between negative financial events and CRP (ab = .013, SE = .012, p = .27). Psychological distress did not significantly mediate any of the examined relations.
Moderated Models
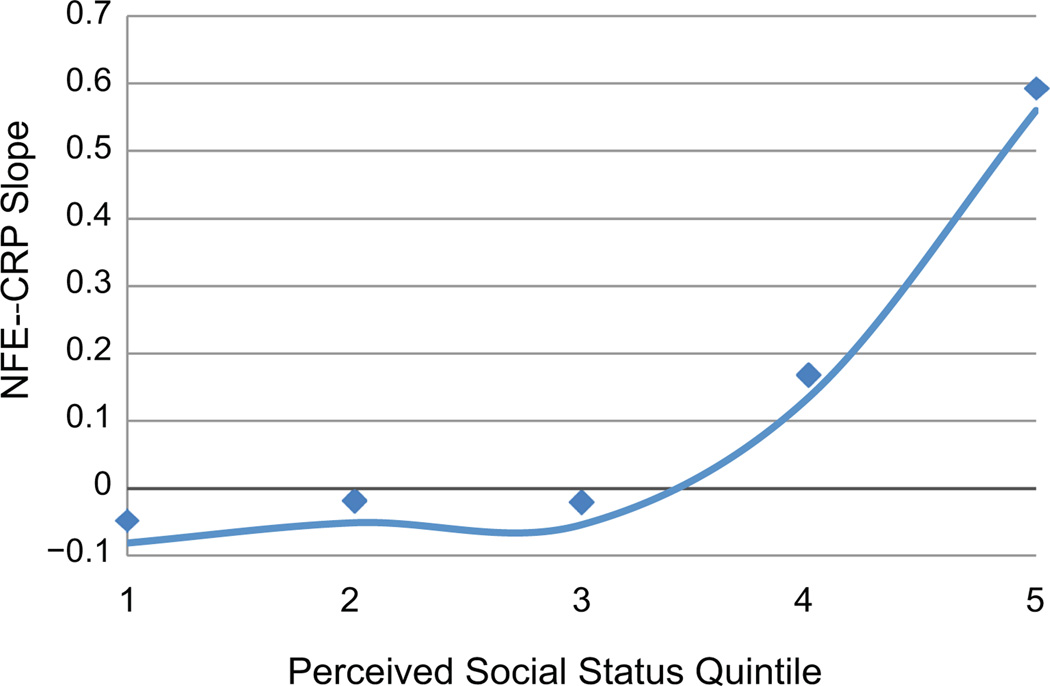
We examined whether perceived social status moderated the relations between negative financial events and (a) negative interpersonal events; (b) psychological distress; (c) psychological well-being; and (d) inflammatory markers. Interaction effects were not significant for psychological well-being, psychological distress, and IL-6 (lowest p > .39). However, perceived social status significantly moderated the effects of negative financial events on both negative interpersonal events (interaction B = .067, SE = .017, p < .001), and CRP levels (interaction B = .051, SE = .026, p = .050). These interaction effects indicated that individuals with higher levels of perceived social status showed a stronger relation between negative financial events and both negative interpersonal events and CRP levels; the interaction of these variables in predicting CRP can be seen in Figure 2.
Figure 2.
Relationship between negative financial events (NFE) and CRP, across quintiles of perceived social status ratings.
Note: NFE-CRP slope is statistically significant only in 5th quintile (N = 136).
Model Fit Indices
The model fit indices yielded from the fully-specified model suggested good fit according to the comparative fit index (CFI = .963), Tucker-Lewis Index (TLI = .937), standardized root mean square residual (SRMR = .034), and root mean square error of approximation (RMSEA = .044). The chi-square test of model fit was significant (χ2(89) = 185.80, p < .001). However, given that this index of model fit is susceptible to inflated values in large sample sizes (37), the fit of the current model was deemed to be acceptable.
Discussion
The current study examined the relations between stressors in the domains of finances and interpersonal functioning and their concomitant relations with psychological distress, psychological well-being, and markers of inflammation (IL-6 and CRP) in a sample of 680 middle-aged adults. We tested the importance of social context by examining the moderating effects of perceived social status on the relations between negative financial events and the endogenous variables. Our results revealed several interesting patterns. Individuals who reported more major financial stressors over the previous year reported more interpersonal stressors, greater psychological distress and lower levels of psychological well-being. Further, the relation of financial stressors with psychological distress was partially explained by stressors in the interpersonal domain. These findings are consistent with previous research describing the deleterious consequences of financial hardship, and support the disruptive nature of financial stress for interpersonal functioning (12,13).
Psychological well-being, but not psychological distress, showed a significant relationship with IL-6, suggesting that it is important to treat them as separate constructs. CRP levels were not found to be directly related to either psychological distress or well-being. Previous studies have highlighted the relationship between inflammation and negative emotions, as in major depression (38); however, our results suggest that positive psychological processes, such as perceived well-being and positive emotions, are more salient predictors of inflammation than depression or anxiety. Positive emotions serve a protective role against inflammation (18) and decrease cytokine production in healthy individuals (39). Although the mechanism for this effect has not been fully delineated, the relationship between positive emotion and inflammation is likely bi-directional, as inflammation may decrease positive emotions through altered patterns of activation and connectivity between brain regions (40). Our findings suggest that the experience of financial stress may influence inflammation, more so through decreased positive emotions than increased negative emotions.
We further contextualized our findings by examining perceived social status as a moderator of individual reactions to financial stress. Previous research has linked the supportive aspects of one’s social network to decreased levels of IL-6 (41). Additionally, perceptions of one’s position within the surrounding community may increase or decrease the salience of stress (42). Our results highlight the complexity of this relationship, as individuals reporting higher perceived social status reported greater psychological well-being and lower levels of psychological distress, but no direct relationship was noted with inflammatory activity. However, middle-aged adults with higher perceived social status showed stronger relationships between financial stressors and both acute inflammation (CRP) and interpersonal problems. These findings suggest that higher perceived social rank serves as a protective factor for psychological health in the absence of major financial stressors, but may predispose an individual to greater inflammation following exposure to financial stressors. The higher reactivity to financial stress observed among adults with higher perceived social status is consistent with models that incorporate identity as a moderator of the stress process (43). It may be that financial stressors are appraised as most threatening by individuals with high perceived social status because these events challenge their identity as being resource-advantaged relative to others. However, according to this model, high community social status adults may not exhibit special vulnerability following exposure to stressors in other domains such as work.
Limitations
The current study has some limitations that must be acknowledged. First, our model reflects a cross-sectional examination of stress, emotion, and inflammation. Though the PERI measures stressful events over the past year, these self-report measures were measured concurrently with inflammatory markers. We cannot definitively say that our findings reflect the true causal ordering of these variables; we cannot demonstrate that financial stressors caused a change in psychological functioning, nor can we be certain that negative interpersonal stressors over the previous year were uniquely caused by financial difficulties. Similarly, our use of items assessing psychological distress and well-being, particularly those items assessing depression and anxiety, were chosen on the basis of their representativeness of a given construct. As we chose to administer only select items from these standardized scales, our measure cannot be directly compared to published studies using the entire standardized scales.
Additionally, our measure of perceived social status does not account for changes in this status, either subjectively or objectively. Indeed, changes in perceived social status may be equally meaningful for psychological health. As the occurrence of financial stressors may affect social standing (e.g., the loss of a job leading to loss of property or moving to a new neighborhood), we acknowledge that our measurement of perceived social status may reflect an already-changed social status after the occurrence of such events. This issue highlights the need for longitudinal assessments to better characterize the interrelationships of financial stress and perceived social standing. Therefore, our results should be interpreted as a preliminary examination of the interconnected nature of stress, social perception, and inflammation.
An additional limitation concerns the large degree of variability in the timing of the blood draws in the current study. The relative inconsistency of the time of blood sampling may have contributed to additional error, which may have resulted in underestimates of the effects of predictors examined in the current model. This issue highlights a common limitation of large samples of community members, as the uniformity in sampling of smaller, more controlled studies of clinical samples may not be possible. However, this limitation is offset by the enhanced external validity attained by incorporating a greater degree of variability that is reflective of typical daily life.
It is notable that the biological variables in this paper demonstrated modest correlations with the remaining study variables. Given that our sample was a large community-based sample, it is reasonable to expect that the size of these relationships might be suppressed by factors that were not assessed nor controlled for in the current study, as is common with heterogeneous samples (44). Similarly, our modeling of multiple statistical covariates may have helped to uncover stronger relationships than might be apparent from the bivariate correlations. Further, despite the relatively small nature of the relationships between the biological variables and the remaining study variables, these effects may nevertheless have significant implications in the context of the health of the population at large.
Directions for future study
A developmental perspective may provide the best lens for understanding the complex effects of financial hardship (45). Longitudinal studies of financial stress and social factors in physical and psychological health may provide insight into the consequences of decreased exposure to resources needed for healthy development. In addition, further elucidation of the relations between positive emotional states, inflammation, and other markers of physiological reactivity may be valuable. Of particular interest is heart rate variability, a physiological index reflecting parasympathetic nervous system activity that has been connected to immune system functioning (46) and to positive emotions and adaptive stress responses (47). Incorporation of heart rate variability indices in models examining the relations between positive emotions and inflammation may provide a unique opportunity to integrate heretofore disparate models of stress adaptation.
Conclusions
The current study characterized relations between financial stressors and psychosocial functioning and inflammation in a community sample of middle-aged adults. Individuals who have experienced more major financial stressors report greater levels of psychological distress and lower levels of psychological well-being. Mediation analyses also suggested that financial stress may indirectly affect inflammatory activity through decreases in psychological well-being. Our findings also highlight the relatively greater importance of positive versus negative emotions in explaining the relationship between financial stressors and inflammation. Further, the social context of stress exposure is a key determinant of stress responses. Whereas those individuals who view themselves at a relatively higher position within their community tend to show decreased levels of inflammation and report better overall psychological health, they are also more susceptible to stressors that threaten their standing within the community. We propose that greater attention to the social and positive psychological determinants of adaptation may yield increasingly valuable information about the pathways by which stress influences health.
Supplementary Material
Acknowledgments
Sources of Funding: This work is supported by a grant from the National Institute on Aging: “Resilience and Health in Communities and Individuals” (R01 AG 026006), Alex Zautra (PI), John Hall (Co-PI).
Abbreviations
- IL-6
Interleukin-6
- CRP
C-reactive protein
- BMI
Body Mass Index
- PERI
Psychiatric Epidemiology Research Interview
- SF-36
Short Form (36) Health Survey
- WHO-5
Health Organization Well-Being Index
- PANAS
Positive Affect Negative Affect Schedule
- MHI
Mental Health Inventory
- EDTA
Ethylene-diaminetetraacetic acid
- CFA
Comparative fit index (CFI)
- TLI
Tucker Lewis Index
- RMSEA
Root mean square error of approximation
- SRMR
Standardized root-mean-square residual
Footnotes
Conflicts of Interest
The authors have no conflicts to disclose.
References
- 1.Zautra AJ, Affleck GG, Tennen H, Reich JW, Davis MC. Dynamic approaches to emotions and stress in everyday life: Bolger and Zuckerman reloaded with positive as well as negative affects. J Pers. 2005;73:1511–1538. doi: 10.1111/j.0022-3506.2005.00357.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahnquist J, Wamala SP, Lindstrom M. Social determinants of health--a question of social or economic capital? Interaction effects of socioeconomic factors on health outcomes. Soc Sci Med. 2012;74:930–939. doi: 10.1016/j.socscimed.2011.11.026. [DOI] [PubMed] [Google Scholar]
- 3.Bergeman C, Braun M, Scott S, Baird B, Montpetit M, Ong A. Effects of daily stress on negative affect: do social interactions help or hinder. Manuscript of the University of Notre Dame; 2010. [Google Scholar]
- 4.Aneshensel CS. Advances in the Conceptualization of the Stress Process. Springer; 2010. Neighborhood as a social context of the stress process; pp. 35–52. [Google Scholar]
- 5.Kraus MW, Piff PK, Keltner D. Social Class as Culture: The Convergence of Resources and Rank in the Social Realm. Curr Dir Psychol Sci. 2011;20:246–250. [Google Scholar]
- 6.Black PH, Garbutt LD. Stress, inflammation and cardiovascular disease. J Psychosom Res. 2002;52:1–23. doi: 10.1016/s0022-3999(01)00302-6. [DOI] [PubMed] [Google Scholar]
- 7.Maes M, Song C, Lin A, De Jongh R, Van Gastel A, Kenis G, Bosmans E, De Meester I, Benoy I, Neels H. The effects of psychological stress on humans: increased production of pro-inflammatory cytokines and Th1-like response in stress-induced anxiety. Cytokine. 1998;10:313–318. doi: 10.1006/cyto.1997.0290. [DOI] [PubMed] [Google Scholar]
- 8.Davis MC, Zautra AJ, Younger J, Motivala SJ, Attrep J, Irwin MR. Chronic stress and regulation of cellular markers of inflammation in rheumatoid arthritis: implications for fatigue. Brain Behav Immun. 2008;22:24–32. doi: 10.1016/j.bbi.2007.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Toker S, Shirom A, Shapira I, Berliner S, Melamed S. The association between burnout, depression, anxiety, and inflammation biomarkers: C-reactive protein and fibrinogen in men and women. J Occup Health Psychol. 2005;10:344–362. doi: 10.1037/1076-8998.10.4.344. [DOI] [PubMed] [Google Scholar]
- 10.Black PH. Stress and the inflammatory response: a review of neurogenic inflammation. Brain Behav Immun. 2002;16:622–653. doi: 10.1016/s0889-1591(02)00021-1. [DOI] [PubMed] [Google Scholar]
- 11.Ayers JW, Althouse BM, Allem JP, Childers MA, Zafar W, Latkin C, Ribisl KM, Brownstein JS. Novel surveillance of psychological distress during the great recession. J Affect Disord. 2012;142:323–330. doi: 10.1016/j.jad.2012.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Myers DG. The funds, friends, and faith of happy people. Am Psychol. 2000;55:56–67. doi: 10.1037//0003-066x.55.1.56. [DOI] [PubMed] [Google Scholar]
- 13.Kahn JR, Pearlin LI. Financial strain over the life course and health among older adults. J Health Soc Behav. 2006;47:17–31. doi: 10.1177/002214650604700102. [DOI] [PubMed] [Google Scholar]
- 14.Uchino BN. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J Behav Med. 2006;29:377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- 15.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98:310–357. [PubMed] [Google Scholar]
- 16.Kiecolt-Glaser JK, Loving TJ, Stowell JR, Malarkey WB, Lemeshow S, Dickinson SL, Glaser R. Hostile marital interactions, proinflammatory cytokine production, and wound healing. Arch Gen Psychiatry. 2005;62:1377–1384. doi: 10.1001/archpsyc.62.12.1377. [DOI] [PubMed] [Google Scholar]
- 17.Roy B, Diez-Roux AV, Seeman T, Ranjit N, Shea S, Cushman M. The association of optimism and pessimism with inflammation and hemostasis in the Multi-Ethnic Study of Atherosclerosis (MESA) Psychosom Med. 2010;72:134. doi: 10.1097/PSY.0b013e3181cb981b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Steptoe A, O'Donnell K, Badrick E, Kumari M, Marmot M. Neuroendocrine and inflammatory factors associated with positive affect in healthy men and women: the Whitehall II study. Am J Epidemiol. 2008;167:96–102. doi: 10.1093/aje/kwm252. [DOI] [PubMed] [Google Scholar]
- 19.Nobles J, Weintraub MR, Adler NE. Subjective socioeconomic status and health: relationships reconsidered. Soc Sci Med. 2013;82:58–66. doi: 10.1016/j.socscimed.2013.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Adler NE, Epel ES, Castellazzo G, Ickovics JR. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy, White women. Health Psychol. 2000;19:586. doi: 10.1037//0278-6133.19.6.586. [DOI] [PubMed] [Google Scholar]
- 21.Ruehlman LS, Wolchik SA. Personal goals and interpersonal support and hindrance as factors in psychological distress and well-being. J Pers Soc Psychol. 1988;55:293. doi: 10.1037//0022-3514.55.2.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Veit CT, Ware JE., Jr The structure of psychological distress and well-being in general populations. J Consult Clin Psychol. 1983;51:730–742. doi: 10.1037//0022-006x.51.5.730. [DOI] [PubMed] [Google Scholar]
- 23.Brief AP, Butcher AH, George JM, Link KE. Integrating bottom-up and top-down theories of subjective well-being: the case of health. J Pers Soc Psychol. 1993;64:646. doi: 10.1037//0022-3514.64.4.646. [DOI] [PubMed] [Google Scholar]
- 24.Bureau UC. [[cited 2014 November 25]];State and County QuickFacts. http://quickfacts.census.gov/qfd/states/04000.html2014.
- 25.Dohrenwend BS, Krasnoff L, Askenasy AR, Dohrenwend BP. Exemplification of a method for scaling life events: the Peri Life Events Scale. J Health Soc Behav. 1978;19:205–229. [PubMed] [Google Scholar]
- 26.Operario D, Adler NE, Williams DR. Subjective social status: Reliability and predictive utility for global health. Psychol Health. 2004;19:237–246. [Google Scholar]
- 27.McHorney CA, Ware JE, Jr, Raczek AE. The MOS36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–263. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Lowe B, Spitzer RL, Grafe K, Kroenke K, Quenter A, Zipfel S, Buchholz C, Witte S, Herzog W. Comparative validity of three screening questionnaires for DSM-IV depressive disorders and physicians’ diagnoses. J Affect Disord. 2004;78:131–140. doi: 10.1016/s0165-0327(02)00237-9. [DOI] [PubMed] [Google Scholar]
- 29.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 30.Berwick DM, Murphy JM, Goldman PA, Ware JE, Jr, Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Med Care. 1991;29:169–176. doi: 10.1097/00005650-199102000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Costa PT, McCrae RR. NEO PI-R: Revised NEO Personality Inventory and NEO Five-Factor Inventory (NEO-FFI) PAR. 1992 [Google Scholar]
- 32.First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition, January 1995 FINAL. SCID-I/P Version 2.0) New York, NY: Biometrics Research Department, New York State Psychiatric Institute; 1995. [Google Scholar]
- 33.Licastro F, Candore G, Lio D, Porcellini E, Colonna-Romano G, Franceschi C, Caruso C. Innate immunity and inflammation in ageing: a key for understanding age-related diseases. Immun Ageing. 2005;2:1–14. doi: 10.1186/1742-4933-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McCaffery JM, Marsland AL, Strohacker K, Muldoon MF, Manuck SB. Factor structure underlying components of allostatic load. PLoS One. 2012;7:e47246. doi: 10.1371/journal.pone.0047246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Muthén LK, Muthén BO. Mplus: Statistical Analysis with Latent Variables; User’s Guide;[Version 5] Muthén & Muthén; 2007. [Google Scholar]
- 36.Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- 37.Anderson JC, Gerbing DW. Structural equation modeling in practice: A review and recommended two-step approach. Psychol Bull. 1988;103:411. [Google Scholar]
- 38.Stewart JC, Rand KL, Muldoon MF, Kamarck TW. A prospective evaluation of the directionality of the depression-inflammation relationship. Brain Behav Immun. 2009;23:936–944. doi: 10.1016/j.bbi.2009.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Prather AA, Marsland AL, Muldoon MF, Manuck SB. Positive affective style covaries with stimulated IL-6 and IL-10 production in a middle-aged community sample. Brain Behav Immun. 2007;21:1033–1037. doi: 10.1016/j.bbi.2007.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Harrison NA, Brydon L, Walker C, Gray MA, Steptoe A, Critchley HD. Inflammation Causes Mood Changes Through Alterations in Subgenual Cingulate Activity and Mesolimbic Connectivity. Biol Psychiatry. 2009;66:407–414. doi: 10.1016/j.biopsych.2009.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Loucks EB, Sullivan LM, D'Agostino RB, Sr, Larson MG, Berkman LF, Benjamin EJ. Social networks and inflammatory markers in the Framingham Heart Study. J Biosoc Sci. 2006;38:835–842. doi: 10.1017/S0021932005001203. [DOI] [PubMed] [Google Scholar]
- 42.Cohen S, Janicki-Deverts D. Who's stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 20091. J Appl Soc Psychol. 2012;42:1320–1334. [Google Scholar]
- 43.Thoits PA. Handbook of the sociology of mental health. Springer; 2013. Self, identity, stress, and mental health; pp. 357–377. [Google Scholar]
- 44.McCartney K, Rosenthal R. Effect size, practical importance, and social policy for children. Child Dev. 2000:173–180. doi: 10.1111/1467-8624.00131. [DOI] [PubMed] [Google Scholar]
- 45.Elder GH., Jr . Children of the Great Depression: Social change in life experience. Westview Press; 1999. [Google Scholar]
- 46.Marsland AL, Gianaros PJ, Prather AA, Jennings JR, Neumann SA, Manuck SB. Stimulated production of proinflammatory cytokines covaries inversely with heart rate variability. Psychosom Med. 2007;69:709–716. doi: 10.1097/PSY.0b013e3181576118. [DOI] [PubMed] [Google Scholar]
- 47.Dockray S, Steptoe A. Positive affect and psychobiological processes. Neurosci Biobehav Rev. 2010;35:69–75. doi: 10.1016/j.neubiorev.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.