Abstract
Background
Atrial fibrillation (AF) and heart failure (HF) frequently coexist and together confer an adverse prognosis. The association of AF with HF subtypes has not been well-described. We sought to examine differences in the temporal association of AF and HF with preserved versus reduced ejection fraction (HFpEF vs HFrEF).
Methods and Results
We studied Framingham Heart Study participants with new-onset AF and/or HF between 1980–2012. Among 1737 individuals with new AF, (mean-age 75±12, 48% women) more than one third (37%) had HF. Conversely among 1166 individuals with new HF (mean-age 79±11, 53% women), more than half (57%) had AF. Prevalent AF was more strongly associated with incident HFpEF (multivariable-adjusted hazard ratio [HR] 2.34, 95% confidence interval [CI] 1.48–3.70, no AF as referent) vs HFrEF (HR 1.32, 95%CI 0.83–2.10), with a trend toward difference between HF subtypes (P for difference 0.06). Prevalent HF was associated with incident AF (HR 2.18, 95%CI 1.26–3.76, no HF as referent). The presence of both AF and HF portended greater mortality risk compared with those without either condition, particularly among individuals with new HFrEF and prevalent AF (HR 2.72, 95%CI 2.12–3.48) compared with new HFpEF and prevalent AF (HR 1.83, 95%CI 1.41–2.37, P for difference 0.02).
Conclusions
AF occurs in more than half of individuals with HF, and HF in more than one third of individuals with AF. AF precedes and follows both HFpEF and HFrEF, with some differences in temporal association and prognosis. Future studies focused on underlying mechanisms of these dual conditions are warranted.
Keywords: Atrial fibrillation, Heart failure, Heart failure with preserved ejection fraction, Epidemiology, Mortality
Heart failure (HF) and atrial fibrillation (AF) have emerged as two new epidemics of cardiovascular disease in the last 20 years.1 The prevalence of both conditions is expected to increase with the aging of the population. By the year 2030, there will be 12 million Americans with AF, and over 8 million with HF.2,3 Beyond sharing common predisposing risk factors such as hypertension, diabetes, ischemic heart disease, and valvular heart disease,4 it is clear that AF and HF are closely intertwined, with each disease predisposing to the other. When present in combination, AF and HF portend a worse prognosis than either condition alone.5–7
AF coexists with both HF with preserved and reduced ejection fraction (HFpEF, HFrEF).8 However, previous studies have noted differences among HF subtypes in atrial remodeling and prognosis associated with AF. For example, left atrial (LA) remodeling appears distinct between subtypes, with greater eccentric LA remodeling in HFrEF, and increased LA stiffness in HFpEF predisposing to AF.9 Additionally, cardiovascular outcomes after AF appears to be influenced by HF subtype.10 In light of these differences, we hypothesized that the temporal association between AF and HF subtypes would be distinct.
Prior studies focused on the association of AF and HF subtypes were largely conducted in hospital-based cohorts,11 where the onset of one condition compared with the other is unclear. We sought to investigate the association of AF with HFpEF and HFrEF in a large, community-based cohort, where incident AF and HF events were ascertained longitudinally, enabling accurate chronicity of HF and AF events. We sought to leverage these study characteristics to examine differences in the temporal associations between HFpEF and HFrEF events in relation to incident AF, and to characterize risk of mortality among participants with various AF and HF subtypes.
Methods
Study Participants
The study design of the Framingham Heart Study is described elsewhere.12 Briefly, participants enrolled in the original (n=5209) and offspring cohorts (n=5124) underwent periodic clinical examinations and medical history updates once every two to four years. The Framingham Heart Study was reviewed by the Boston University Medical Center Institutional Review Board and all participants signed written consent.
Participants with new-onset AF (n=1737) and/or HF (n=1166) between 1980 and 2012 were included, since echocardiography became more widely available after 1980 for determination of HF subtype. For incident AF and HF analyses, participants attending one of three baseline examinations per cohort were included: original cohort examinations 16 (1979–82), 20 (1986–90), 24 (1995–98) and offspring cohort examinations 2 (1979–83), 4 (1987–91), 6 (1995–98) (Supplemental Figure 1). From this sample, there were 14864 observations included in incident AF analyses after excluding prevalent AF (n=554), missing covariates (n=551), or no follow-up (n=28) (Supplemental Figure 2A). For incident HF analyses, observations with prevalent HF (n=217), missing covariates (n=575), or missing follow-up (n=2) were excluded, leaving 15203 observations for analysis (Supplemental Figure 2A). Follow-up was truncated at 8 years for incident AF and HF analyses.
Clinical examination
All participants underwent comprehensive clinical evaluations during the examination cycles that included blood pressure measurements, electrocardiogram (ECG), and blood tests. Diabetes was defined as a fasting glucose level ≥126 mg/dl, non-fasting glucose ≥200 mg/dl, or the use of hypoglycemic drugs or insulin. Fasting total and high density lipoprotein (HDL) cholesterol were measured. Left ventricular hypertrophy on ECG was defined using published criteria.13 Current smoking was based on self-reported use of ≥1 cigarettes/day in the year prior to the examination. Valvular heart disease was defined as any diastolic murmur or systolic murmur ≥ 3/6 grade.
Definition of clinical endpoints
All cardiovascular endpoints were adjudicated by a panel of 3 physicians using established protocols after systematic review of all available medical records. HF was defined using established Framingham criteria.4 HF subtype was determined after review of records based on left ventricular ejection fraction (LVEF) obtained by echocardiogram or radionuclide study performed at or near the HF event date (during HF admission or within 1 year of HF onset provided that no intervening myocardial infarction occurred) as previously described.4 HF events were classified as HFpEF (LVEF≥45%) or HFrEF (LVEF<45%). The presence of AF was determined after review of all available ECGs from examination cycles, outpatient and inpatient hospital records, or ambulatory ECG monitoring.
Statistical analysis
To examine the temporal association of AF and HF subtypes, we inspected the occurrence of prevalent AF, concurrent AF, and incident AF (after HF) in all individuals with new-onset HF between 1980 and 2012. Concurrent AF and HF were defined as the diagnosis of new AF and HF within 30 days of one another. Similarly, the occurrence of prevalent, concurrent, and incident HF by subtype (after AF) was examined in all individuals with new-onset AF between 1980 and 2012.
The cumulative incidence of AF, HFpEF, and HFrEF were estimated using a Kaplan-Meier-like method accounting for competing risk of death.14 Separate curves were estimated for those with and without HF (for incident AF) and those with and without AF (for incident HF). We calculated directly standardized rates (sex- and age-adjusted with 10-year age strata) using the relevant baseline sample (free of AF or HF) for incidence rates, or the sample that developed a specified condition (AF or HF) for post-event mortality rates. Multivariable Cox proportional hazards regression was used to examine the associations of prevalent and interim HF and incident AF. Analyses were first adjusted for age and sex, and then further adjusted for established risk factors of AF (height, weight, systolic and diastolic blood pressure, current smoking, use of antihypertensive medication, diabetes, and history of myocardial infarction).15 In secondary analyses, multivariable models were further adjusted for prevalent cardiovascular disease other than myocardial infarction, as well as estimated glomerular filtration rate (available in 9521 individuals in incident AF, and 9737 individuals in incident HF analyses). In order to account for participants eligible for more than one observation period, we used the sandwich estimator to generate robust standard error estimates clustered on the individual participant.16
To relate AF to incident HFpEF and HFrEF, Cox models were used and adjusted for age and sex, and then further adjusted for body mass index, systolic blood pressure, heavy alcohol use, smoking, diabetes, left ventricular hypertrophy, hypertension treatment, valvular heart disease and history of myocardial infarction. Interim events were modeled as time-varying covariates. In secondary analyses, we compared the beta coefficients of AF as a predictor of incident HFpEF and HFrEF using the Lunn McNeil method.17
Next, the association of HF and AF individually and conjointly on mortality was assessed using Cox models. The hazards of prevalent and interim AF for mortality among participants with newly diagnosed HF between 1980–2012 were assessed (Supplemental Figure 2B). The Kaplan-Meier method was used to calculate cumulative incidence plots of mortality. Similarly, the hazards of prevalent and interim HF for mortality among participants with newly diagnosed AF were assessed. Interim events were modeled as time-varying covariates, and follow-up was truncated at 10 years. Models were first adjusted for age and sex, and then further adjusted for systolic blood pressure, body mass index, anti-hypertensive treatment, smoking, diabetes, and history of myocardial infarction. Covariates were taken from the most proximal Framingham Heart Study examination attended within 8 years preceding HF or AF diagnosis. HF subtype was examined using a 4-level class variable (no HF, HFpEF, HFrEF and unclassified HF). We considered a two-sided p-value of ≤0.05 statistically significant. To check the proportional hazard assumption, we tested for interactions with variables and log-time, and we also used the 'assess' statement in PHREG. Neither approach showed violation of the proportional hazard assumption. All statistical analyses were conducted using SAS version 9.3 for Windows (SAS Institute Inc., Cary, North Carolina).
Results
Temporal association of AF and HF subtypes
Between 1980 and 2012, 1166 participants developed new-onset HF. Of these, 479 (41%) were classified as having HFpEF and 516 (44%) were classified as having HFrEF [171 (15%) could not be classified]. Of participants with HF, 38% had no AF at baseline or during follow-up, 32% had prevalent AF, 18% had AF diagnosed within 30 days of their incident HF diagnosis, and 12% developed incident AF after their incident HF diagnosis (Figure 1, Supplemental Table 1). The time distribution between prevalent, concurrent and incident AF by HF subtypes is displayed in Supplemental Table 2. Compared with HFrEF, individuals with HFpEF were more likely to have AF at any time (62% vs 55%, P=0.02). Participants with HFpEF carried a much greater burden of prevalent AF as compared to HFrEF (32% vs 23%, P=0.002).
Figure 1.
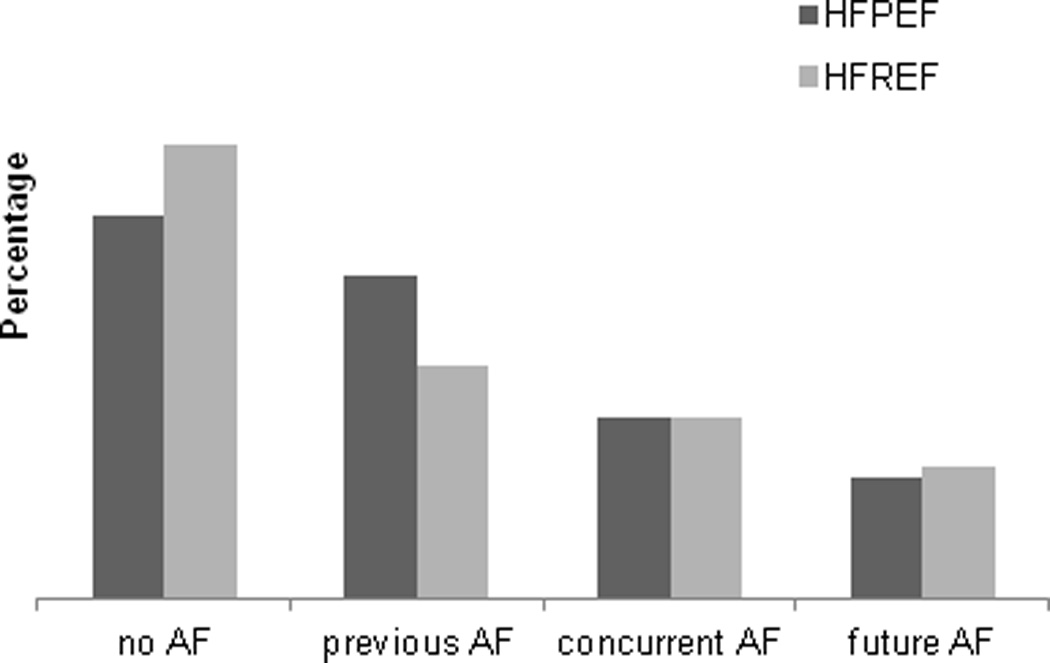
Temporal association of AF and HF subtypes. Panel A shows data for 995 participants with new HF, and whether participants had previous, concurrent, future AF, or no AF (for 479 with HFpEF: 154, 88, 56, and 181, respectively; for 516 with HFrEF: 121, 94, 67, and 234, respectively). Panel B shows data for 1737 participants with new AF, of whom 1101 had no HF (n=1101), and others had previous, concurrent, or future HF (for 284 with HFpEF: 57, 88, 139, respectively; for 272 with HFrEF: 67, 94, 111, respectively; for 80 with unclassified HF: 21, 32, and 27, respectively).
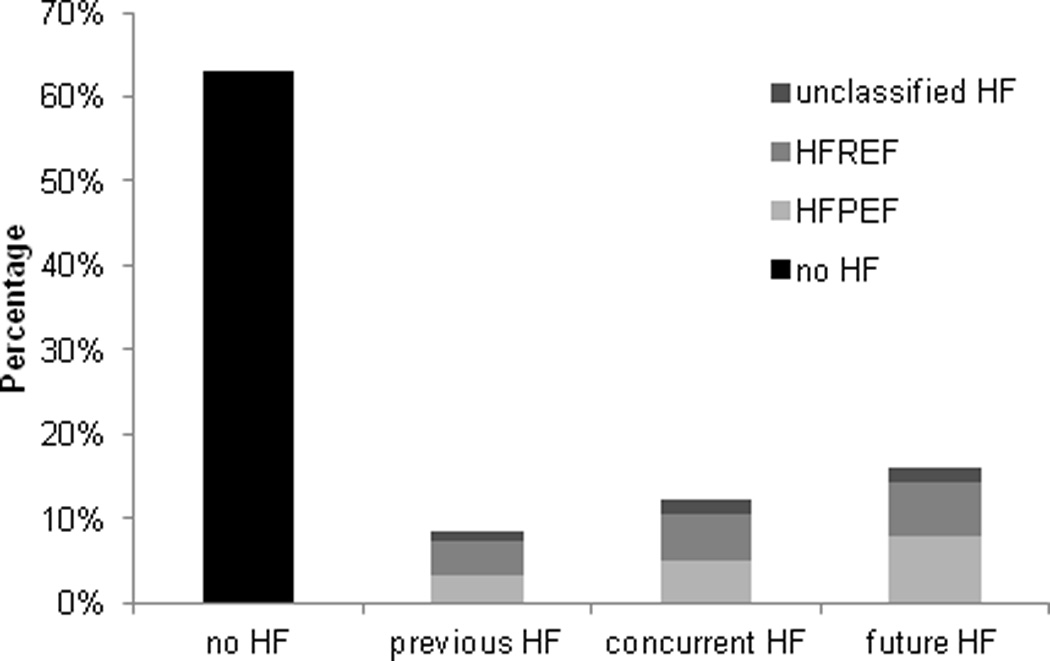
Over the same period, 1737 individuals developed new-onset AF. Of these, 1101 (63%) had no HF at any point, 145 (8%) had HF previously diagnosed at the time of their AF diagnosis, 214 (12%) had HF diagnosed concomitantly or within 30 days of their incident AF event, and 277 (16%) developed incident HF after their AF diagnosis. Among participants with HF diagnosed prior to, or concomitant with their AF diagnosis, rates of HFrEF and HFpEF did not vary significantly. Among individuals with HF diagnosed after their AF event, 50% developed HFpEF, 40% developed HFrEF, and 10% were unclassified (Figure 1, Supplemental Table 1). The time intervals between AF diagnosis and HFpEF vs HFrEF events among 644 individuals who had both AF and HF during follow-up are presented in Supplemental Figure 3.
Prevalent and interim HF predict incident AF
Among 14864 observations included in the incident AF analysis, the mean age was 58 years and 55% were women. Baseline characteristics are displayed in Table 1. A total of 90 participants had prevalent HF (28 with HFpEF, 32 with HFrEF, and 30 with unclassified HF). There were 795 AF events during a mean follow up of 7.5±1.6 years. Those with prevalent HF had higher cumulative incidence of AF compared to those free of HF, (log-rank P<0.0001, Figure 2A). The age- and sex-standardized incidence rate of AF was nearly 10-fold higher in those with prevalent HF compared to without HF (Table 2).
Table 1.
Baseline clinical characteristics for participants free of prevalent AF or HF
| Free of prevalent AF N=14864 |
Free of prevalent HF N=15203 |
|
|---|---|---|
| Age, years | 57 ± 15 | 58 ± 15 |
| Women, n (%) | 8222 (55) | 8322 (55) |
| Height, cm | 166 ± 10 | 166 ± 10 |
| Weight, kg | 74 ± 16 | 74 ± 16 |
| Body mass index, kg/m2 | 26.7 ± 4.8 | 26.7 ± 4.8 |
| Systolic blood pressure, mmHg | 130 ± 20 | 130 ± 20 |
| Diastolic blood pressure, mmHg | 77 ± 10 | 77 ± 10 |
| Hypertension treatment, n (%) | 3622 (25) | 3778 (25) |
| Prevalent myocardial infarction, n (%) | 628 (4) | 655 (4) |
| Total cholesterol, mg/dL | 211 ± 41 | 210 ± 41 |
| HDL cholesterol, mg/dL | 50 ± 15 | 50 ± 15 |
| Heavy alcohol use, n (%) | 943 (6) | 963 (6) |
| Smoking, n (%) | 3491 (23) | 3540 (23) |
| Diabetes mellitus, n (%) | 890 (6) | 927 (6) |
| Left ventricular hypertrophy, n (%) | 183 (1) | 194 (1) |
| Valvular heart disease, n (%) | 399 (3) | 418 (3) |
| Prevalent HF, n (%) | 90 (1) | - |
| Prevalent AF, n (%) | - | 403 (3) |
Values are mean ± SD unless otherwise noted.
AF, atrial fibrillation; HDL, high density lipoprotein; HF, heart failure.
Figure 2.
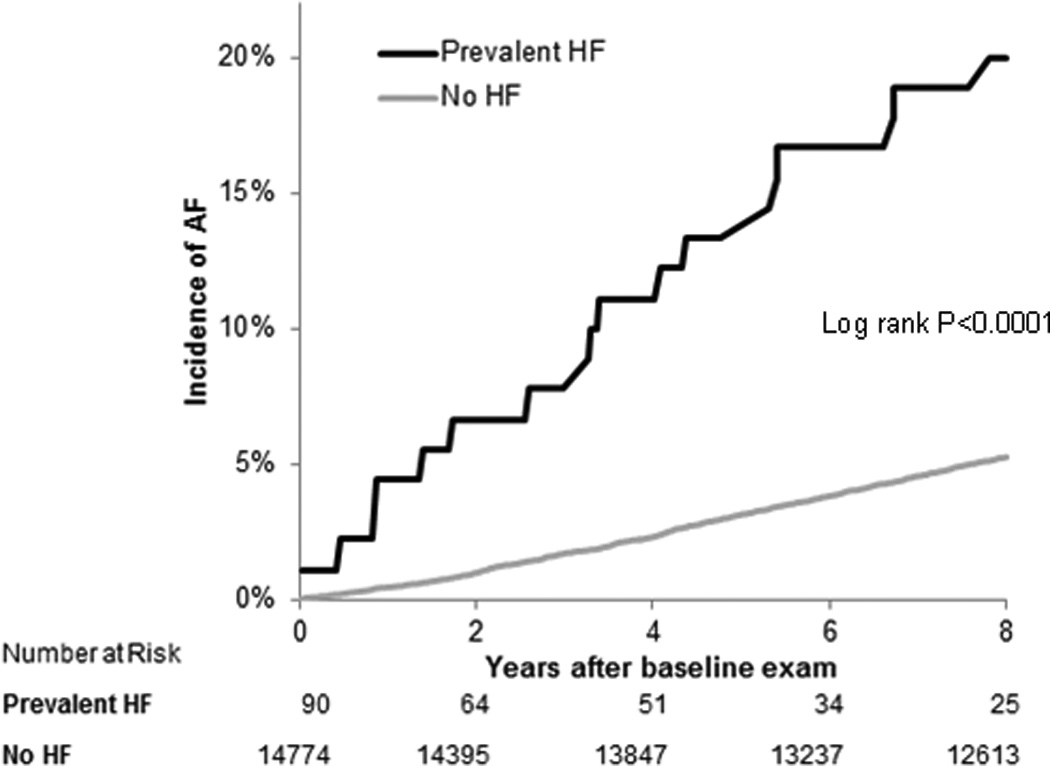
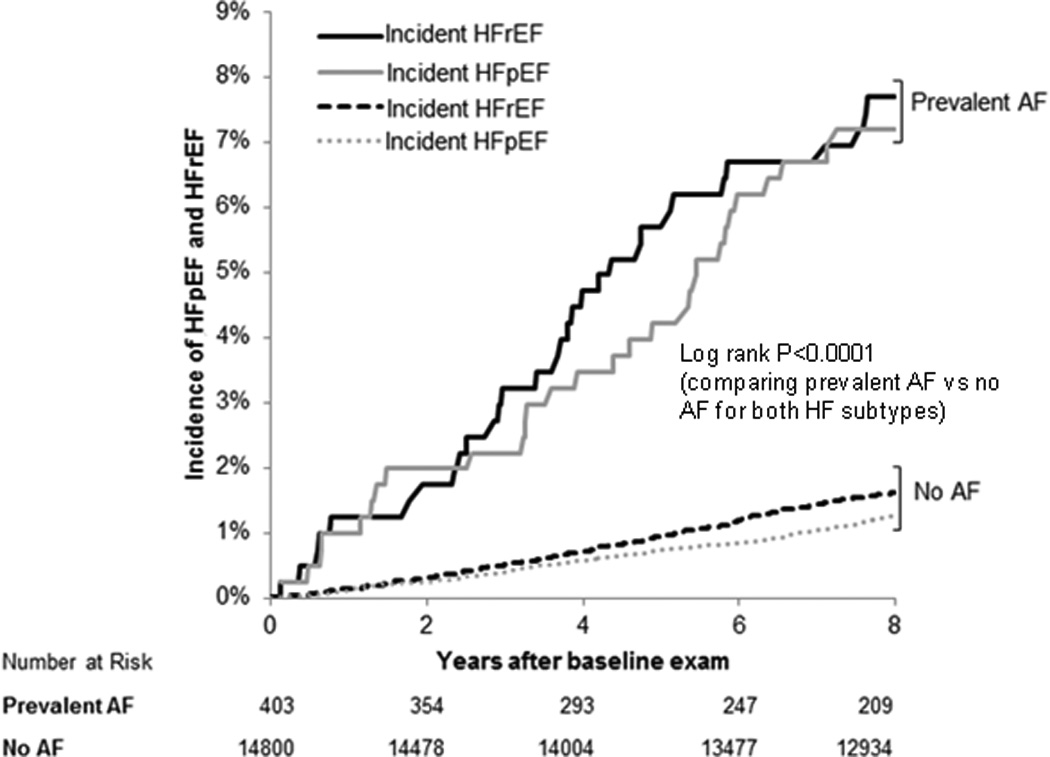
Cumulative incidence of AF and HF among those with and without the other condition. Panel A displays cumulative incidence of AF (N=795) in participants with and without prevalent HF. Panel B displays cumulative incidence of HFpEF (N=215) and HFrEF (N=272) in participants with and without prevalent AF. For 95% confidence interval estimates, please see Supplemental Table 5.
Table 2.
Incidence rates for incident disease and mortality with and without AF and HF
| Outcome | Group | Incidence rate (per 1000 PY)* |
95% CI† |
|---|---|---|---|
| Incident AF (n=795) | Prevalent HF | 47.8 | 24.1–71.6 |
| No HF | 7.9 | 7.3–8.4 | |
| Incident HF (n=549) | Prevalent AF | 31.4 | 24.0–38.8 |
| No AF | 4.8 | 4.4–5.3 | |
| Incident HFpEF (n=215) | Prevalent AF | 12.9 | 8.2–17.6 |
| No AF | 1.9 | 1.6–2.1 | |
| Incident HFrEF (n=272) | Prevalent AF | 13.2 | 8.5–18.0 |
| No AF | 2.4 | 2.1–2.7 | |
| Mortality after new HF (n=598) | Prevalent AF | 290 | 251–329 |
| No AF | 244 | 218–270 | |
| Mortality after new HFpEF (n=221) | Prevalent AF | 259 | 203–315 |
| No AF | 188 | 154–222 | |
| Mortality after new HFrEF (n=289) | Prevalent AF | 249 | 201–297 |
| No AF | 262 | 221–304 | |
| Mortality after new AF (n=683) | Prevalent HFpEF | 257 | 192–323 |
| Prevalent HFrEF | 302 | 231–373 | |
| No HF | 120 | 109–131 | |
Age (10 year interval) and sex standardized.
AF=atrial fibrillation; CI = confidence interval; HF=heart failure; HFpEF = heart failure with preserved ejection fraction; HFrEF = heart failure with reduced ejection fraction; HR = hazard ratio.
95% CI estimates assume constant incidence rate over time.
In age- and sex-adjusted Cox models, prevalent HF was significantly associated with incident AF (hazard ratio [HR] 3.42, 95% confidence interval [CI] 2.10–5.56, P<0.0001). Similarly, interim HF events predicted incident AF with a hazard of 2.41 (95% CI 1.89–3.08, P<0.0001). Prevalent and interim HF remained significantly associated with an approximately 2-fold increased hazard of incident AF after multivariable adjustment (Table 3). There were too few prevalent HF events to examine HF subtypes separately. After additional adjustment for prevalent cardiovascular disease (other than myocardial infarction) and kidney function, results remained similar, except the association of prevalent HF with incident AF, which was attenuated (P=0.11).
Table 3.
AF and HF as predictors of incident disease
| Outcome | Predictor | Age- and sex-adjusted | Multivariable-adjusted | ||
|---|---|---|---|---|---|
| HR (95% CI)‡ | P value | HR (95% CI)‡ | P value | ||
| Incident AF (n=795)* | Prevalent HF | 3.42 (2.10–5.56) | <0.0001 | 2.18 (1.26–3.76) | 0.005 |
| Interim HF | 2.41 (1.89–3.08) | <0.0001 | 1.91 (1.48–2.46) | <0.0001 | |
| Incident HFpEF (n=215)† | Prevalent AF | 3.11 (2.02–4.79) | <0.0001 | 2.34 (1.48–3.70) | 0.0003 |
| Interim AF | 1.78 (1.18–2.70) | 0.006 | 1.52 (0.99–2.31) | 0.05 | |
| Incident HFrEF (n=272)† | Prevalent AF | 2.22 (1.47–3.34) | 0.0001 | 1.32 (0.83–2.10) | 0.23 |
| Interim AF | 1.96 (1.37–2.81) | 0.0002 | 1.71 (1.19–2.45) | 0.003 | |
Adjusted for age, sex, height, weight, systolic and diastolic blood pressure, diabetes, smoking, hypertension treatment and history of myocardial infarction.
Adjusted for age, sex, body mass index, hypertension treatment, smoking, alcohol, systolic blood pressure, history of myocardial infarction, heart murmur, diabetes and left ventricular hypertrophy.
Hazard ratio referent group is 'no HF' in incident AF analyses, and 'no AF' in incident HF analyses
AF=atrial fibrillation; CI = confidence interval; HF=heart failure; HFpEF = heart failure with preserved ejection fraction; HFrEF = heart failure with reduced ejection fraction; HR = hazard ratio.
AF as a predictor of incident HF by HF subtype
A total of 15203 observations were included in the incident HF analysis, with a mean age of 58 years, 55% women, and 403 participants with prevalent AF (Table 1). Over a mean follow up of 7.5±1.5 years, there were 215 incident HFpEF and 272 incident HFrEF events. The incidence rates of both HFpEF and HFrEF were higher in those with AF compared to those without (Table 2). Those with prevalent AF had higher cumulative incidence of both HFpEF and HFrEF compared to those without prevalent AF (log-rank P<0.0001 for both Figure 2).
Prevalent AF predicted incident HFpEF (HR 2.34, 95% CI 1.48–3.70, P=0.0003) but not HFrEF (HR 1.32, 95% CI 0.83–2.10, P=0.23) in multivariable-adjusted analyses. In contrast, interim AF was significantly associated with incident HFrEF (HR 1.71, 95% CI 1.19–2.45, P=0.003) but not HFpEF in multivariable-adjusted analyses (P=0.05, Table 3). Using the Lunn McNeil method to compare beta-coefficients between the two subtypes of HF, there was a marginally significant difference in prevalent AF as a predictor of HFpEF vs HFrEF (P=0.06), whereas interim AF did not appear to have differential association with incident HFpEF or HFrEF (P=0.66). Results were not materially different after adjustment for cardiovascular disease (other than myocardial infarction) and kidney function.
Prevalent and interim AF as predictors of mortality after new HF
Of 759 participants with new-onset HF between 1980 and 2012 and available baseline examination data, 309 were classified as HFpEF, 360 as HFrEF, and 90 unclassified HF. The mean age was 79±11 years in HFpEF and 77±10 years in HFrEF, other baseline characteristics are presented in Supplemental Table 2. Over a mean follow-up of 3.6±3.4 years, there were 221 deaths among individuals with HFpEF and 289 among those with HFrEF. Cumulative incidence plots of mortality after HF are presented in Figure 3A. Incidence rates of all-cause mortality among those with HFpEF and HFrEF, with vs without prevalent AF are displayed in Table 2.
Figure 3.
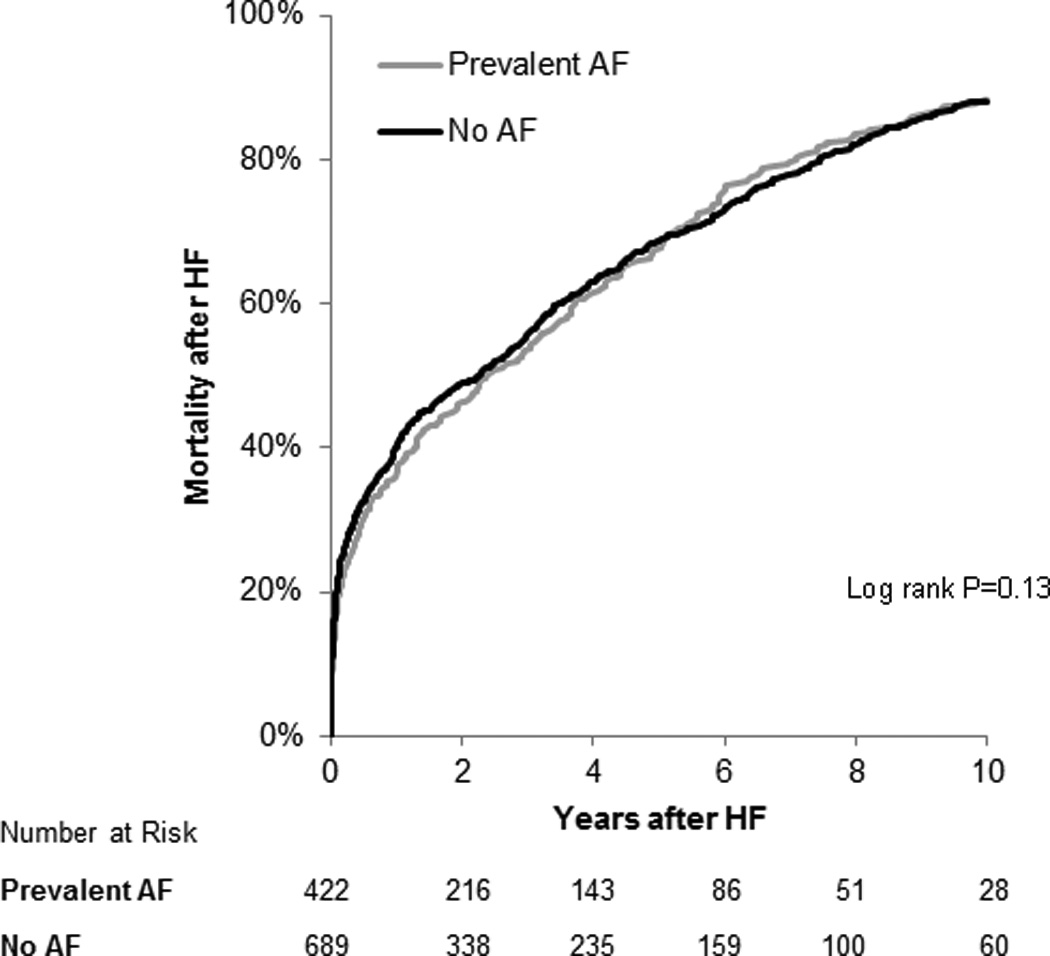
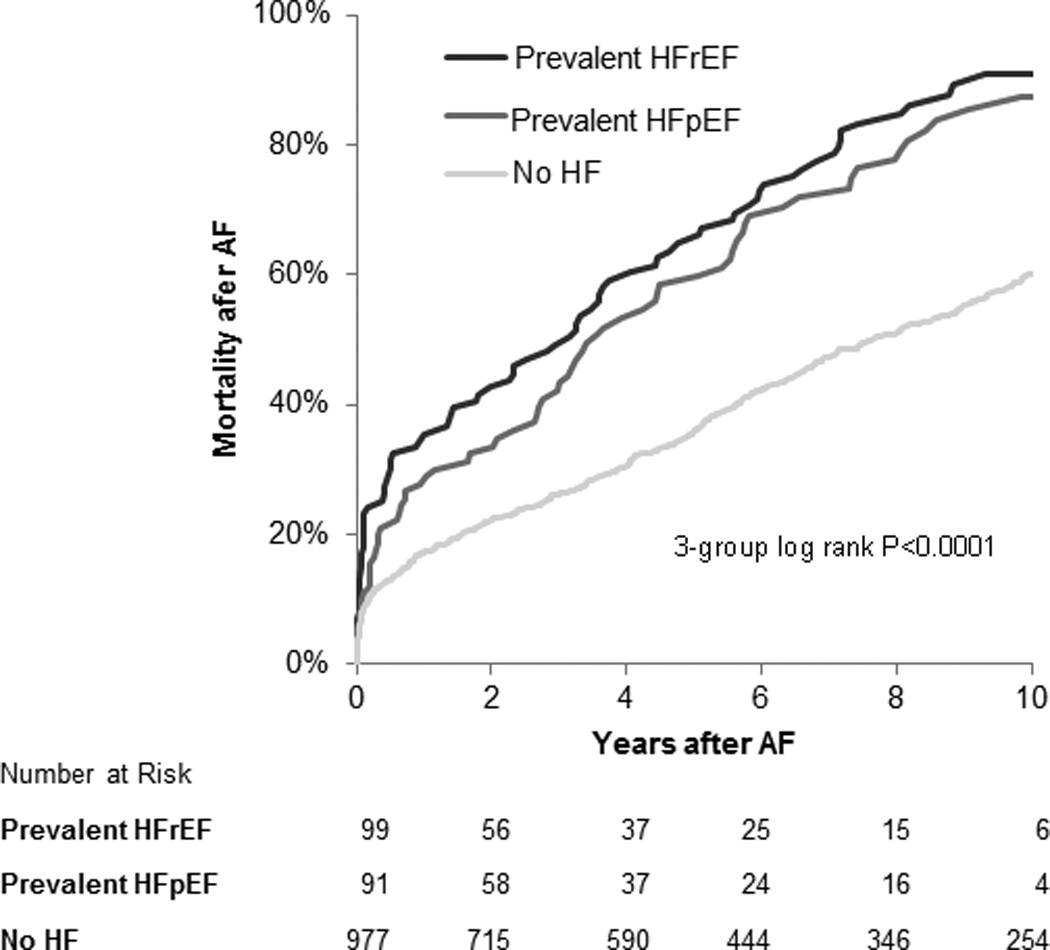
Kaplan Meier curves for all-cause death in those with HF and AF. Panel A displays cumulative incidence of all-cause mortality (N=598) after new HF by AF status. Panel B displays cumulative incidence of all-cause mortality after new AF (N=683) by HF subtype status. For 95% confidence interval estimates, please see Supplemental Table 5.
Prevalent AF was not significantly associated with mortality among individuals with new-onset HFpEF or HFrEF after multivariable analyses (Table 4, Figure 3). By contrast, interim AF (159 events) was significantly associated with mortality among individuals with both new HFpEF and HFrEF (multivariable-adjusted HR 1.58, 95% CI 1.08–2.30, P=0.02; and HR 2.02, 95% CI 1.46–2.79, P<0.0001, respectively).
Table 4.
Concomitant AF and HF as predictors of all-cause mortality
| Outcome | Predictor | Age- and sex-adjusted | Multivariable-adjusted | ||
|---|---|---|---|---|---|
| HR (95% CI)† | P value | HR (95% CI)† | P value | ||
| Mortality after new HF (n=598) | Prevalent AF | 1.18 (0.98, 1.42) | 0.09 | 1.25 (1.04, 1.51) | 0.02 |
| Interim AF | 1.88 (1.50, 2.35) | <0.0001 | 1.89 (1.51, 2.38) | <0.0001 | |
| Mortality after new HFpEF (n=221) | Prevalent AF | 1.23 (0.90, 1.68) | 0.19 | 1.33 (0.97, 1.83) | 0.08 |
| Interim AF | 1.66 (1.15, 2.39) | 0.007 | 1.58 (1.08, 2.30) | 0.02 | |
| Mortality after new HFrEF (n=289) | Prevalent AF | 1.19 (0.91, 1.56) | 0.2 | 1.18 (0.90, 1.56) | 0.23 |
| Interim AF | 2.03 (1.47, 2.80) | <0.0001 | 2.02 (1.46, 2.79) | <0.0001 | |
| Mortality after new AF (n=683) | Prevalent HFpEF | 1.85 (1.43, 2.40) | <0.0001 | 1.83 (1.41, 2.37) | <0.0001 |
| Prevalent HFrEF | 2.77 (2.18, 3.51) | <0.0001 | 2.72 (2.12, 3.48) | <0.0001 | |
| Prevalent HFpEF vs HFrEF | 0.67 (0.49, 0.92) | 0.01 | 0.67 (0.48, 0.94) | 0.02 | |
| Interim HFpEF | 2.11 (1.57, 2.83) | <0.0001 | 2.31 (1.72, 3.11) | <0.0001 | |
| Interim HFrEF | 2.43 (1.82, 3.24) | <0.0001 | 2.36 (1.76, 3.16) | <0.0001 | |
| Interim HFpEF vs HFrEF | 0.87 (0.59, 1.26) | 0.46 | 0.98 (0.67, 1.43) | 0.91 | |
Adjusted for age, sex, systolic blood pressure, anti-hypertensive treatment, body mass index, diabetes mellitus, smoking, history of myocardial infarction.
Hazard ratio referent group is 'no AF' in mortality after HF analyses, and 'no HF' in mortality analyses after AF
AF=atrial fibrillation; CI = confidence interval; HF=heart failure; HFpEF = heart failure with preserved ejection fraction; HFrEF = heart failure with reduced ejection fraction; HR = hazard ratio.
Prevalent and interim HF as predictors of mortality after new AF
Of 1191 individuals with new AF between 1980 and 2012 and available baseline covariates (Supplemental Table 2), a total of 214 (91 HFpEF, 99 HFrEF, 24 unclassified) had prevalent HF. Over a mean follow-up period of 5.1± 3.8 years, 683 (57%) participants died. Cumulative incidence plots by prevalent HF and HF subtype are shown in Figure 3B. The incidence rates of mortality in AF were highest in participants with prevalent HFrEF, followed by those with prevalent HFpEF and lowest in those without HF (Table 2). Among participants with AF, incidence rates of HF were similar in men and women (50.7 and 56.0 events per 1000 person-years, respectively), with a higher incidence of HFpEF in women (35.1 vs 21.2 events per 1000 person-years) and lower incidence of HFrEF in women (12.4 vs 27.2 events per 1000 person-years, Supplemental Table 3). In exploratory analyses, we examined the association of the CHADS2-VAsc score18 and incident HF events in those with AF, and found that each 1-point increment in the score was associated with a 1.36-fold increased hazard of HF (95% CI 1.26–1.48, P<0.0001), with modest discriminatory capability (c-statistic 0.62, 95% CI 0.59–0.66).
In multivariable analyses, both prevalent HFrEF and HFpEF were associated with adverse outcomes in individuals with new AF (Table 4). However, those with prevalent HFrEF appeared to have a worse prognosis when compared with HFpEF (HR of 2.72, 95% CI 2.12–3.48, P<0.0001 vs HR 1.83, 95% CI 1.41–2.37, P<0.0001; P for comparison 0.02). By contrast, interim HFpEF (n=105) and HFrEF (n=98) appeared to have similar adverse associations on mortality (Table 4, P=0.98 for comparison). Results were not materially different after accounting for the presence of pacemakers/implantable defibrillators at baseline (data not shown). In exploratory analyses, we examined cause-specific death in participants with AF. Age- and sex-standardized incidence rates of coronary heart disease and other cardiovascular deaths were higher compared with cerebrovascular deaths among those without heart failure (Supplemental Table 4).
Discussion
Our findings highlight the close association of AF and HF, with some distinct differences in timing between HFpEF and HFrEF. Over half of the participants with HF had AF at some point, with AF more likely to antedate than to follow HF. Specifically, AF appeared to precede incident HFpEF more frequently than it did incident HFrEF events. Similarly, over one-third of participants with AF had HF, with most developing HF onset after AF rather than beforehand. These proportions emphasize the close association between these two conditions. In fact, previous data show that incidence of HF after AF is nearly double that of stroke,19 and emphasize the need for future HF prevention strategies similar to stroke prevention strategies that are currently implemented after AF. The incidence rates of both subtypes of HF after AF in our study approach that of incident HF in individuals with mild asymptomatic LV systolic dysfunction,20 where preventive therapies exist. Furthermore, AF and HF conjointly appear to portend a poor prognosis, with a higher risk among those with HFrEF compared with HFpEF and new AF.
A previous study examined the temporal association of AF and HF in the Framingham Heart Study in cases occurring between 1948–1995.7 We now extend these findings to a more contemporary sample between 1980 and 2012, and more importantly examine the specific association with HFpEF and HFrEF. Compared with the previous analysis, a greater proportion of individuals have AF without HF, and AF more commonly precedes HF now. These differences may be due to enhanced surveillance, detection, prevalence or incidence of AF over time.21 Another recent population-based study examined the temporal relationship of AF and HFpEF in the Olmsted County cohort.22 Similar to our results, AF was found to occur in over half of individuals with HFpEF, with incident AF after HFpEF bearing a worse prognosis compared with AF prior to or concurrent with HFpEF presentation. Our study expands upon these results to directly compare HFpEF and HFrEF in relation to AF among the same study sample.
Other previous studies examining the association of AF and HFpEF5,8,10,22–24 vs HFrEF5,8,10,23,25–28 on mortality were largely focused on hospital-based cohorts with some exceptions, and showed variable results. A recent meta-analysis demonstrated a worse prognosis of AF with HFpEF when compared with HFrEF.11 Our findings show lower survival rates among participants with conjoint AF and HF, with lowest rates among participants with HFrEF and AF compared with HFpEF and AF. Our study also suggests that timing matters: prevalent AF appears to be associated with mortality less once HF has developed, likely due to a much higher mortality rate with HF regardless of prevalent AF status. Similar findings were previously described.7 It may also be that prevalent AF results in an earlier presentation of HF due to poor tolerance of this arrhythmia, making lead-time bias a potential explanation for our findings. Differences in our study compared with other prior studies may be due to limitations of studies without long-term follow-up, where timing of incident AF relative to incident HF may be unclear. Further, HF disease severity appears to influence AF,29 and prior studies focused on participants with existing HFpEF and HFrEF may have had variable disease severity or at different time points of HF progression. By contrast, our study had the unique opportunity to examine timing from the first presentation of AF relative to incident HF, and may be less heterogeneous with respect to timing along disease course.
While overall differences are modest given the strong association of AF with both HF subtypes, we show that prevalent AF precedes HFpEF in a higher proportion compared to HFrEF (32% vs 23% respectively). The mechanisms by which AF may be different among HF subtypes remain incompletely characterized. Melenovsky et al studied individuals with existing HF, and found that LA remodeling was distinct among HF subtypes. Specifically, they observed eccentric LA remodeling in HFrEF, and greater LA stiffness in HFpEF, and suggested that greater LA stiffness may contribute to greater AF burden seen in HFpEF.9 Other studies have demonstrated that diastolic dysfunction, a precursor of HFpEF, appears also to predict incident AF.30,31 This association may be due to similar underlying mechanisms driving AF and HFpEF development, including myocardial inflammation and fibrosis leading to atrial interstitial fibrosis and AF,32 as well as HFpEF.33–38 It also may be that AF is less well tolerated in individuals predisposed to HFpEF particularly with exertion, and thereby may trigger clinical recognition of HF.4,39,40 Interestingly, we found that both individuals with HFpEF and HFrEF are at similar risk of developing future AF, which may reflect elevation in atrial pressures and remodeling in both types of HF.
There are several limitations to our analyses that deserve mention. First, AF was ascertained from all available ECGs and Holter monitor readings. We may have missed clinically unrecognized AF cases secondary to our reliance on medical records plus periodic study examinations for the diagnosis of AF. Although the majority of HF cases were classified as HFpEF vs HFrEF, 15% remained unclassified due to unavailability of LV functional assessment at the time of HF, and differential misclassification could have influenced our results. Further, HF adjudication was based on Framingham criteria,4 which did not take into account biomarkers or echocardiographic data. This may have resulted in HF being under-diagnosed compared with other HF criteria. Further, once a participant was diagnosed with AF or HF, more frequent routine medical surveillance may have resulted in ascertainment bias of the other condition. Whereas we describe associations, we acknowledge that our study is observational; we cannot rule out residual confounding or prove causal relations. Specifically, we were not able to account for emerging risk factors including obstructive sleep apnea, and did not account for interim development of other risk factors. We were able to account for the use of antihypertensive medications, including beta-blockers and calcium-channel blockers, however, antiarrhythmics were not taken into account, and are known to have potential adverse effects, particularly among individuals with HF.41 The etiology of heart failure was not formally adjudicated, and specifically the contribution of tachycardia-induced cardiomyopathy to HF incidence in participants with AF in our sample remains unknown. We classified HF based on imaging at the first presentation, and subsequent transitions between HF subtypes after the first presentation were not examined. Lastly, our sample is predominantly white, limiting the generalizability of our finding, particularly in light of racial differences in both AF and HF.42,43
Our data indicate that over one-third of individuals with AF have HF at some point, with most developing HF onset after AF rather than before their AF diagnosis. The finding that HF follows rather than predates AF highlights an opportunity for future studies focused on HF prevention in AF. Clinically, the focus in patients with AF is largely directed toward stroke prevention, and less on HF prevention. The incidence rates of both subtypes of HF after AF are comparable to incident HF among individuals with asymptomatic LV dysfunction, classified as having ACC/AHA stage B heart failure. Identifying those at greatest risk of HF using established risk factors may help identify a population to target for future intervention strategies.44
In summary, we show that AF occurs in more than half of individuals with HF, and HF in more than one third of individuals with AF at some point of time. AF precedes and follows both HFpEF and HFrEF, with some differences in temporal association. Lastly, AF and HF conjointly portend a poor prognosis, with a higher risk among those with HFrEF. Future studies focused on underlying mechanisms of these dual conditions, and potential therapeutic strategies are warranted.
Supplementary Material
Clinical Perspectives.
Atrial fibrillation (AF) and heart failure (HF) frequently coexist and together confer an adverse prognosis. However, the association of atrial fibrillation with heart failure subtypes has not been well-described. We studied the temporal association of new-onset AF and HF with preserved versus reduced ejection fraction in participants of the Framingham Heart Study. We show that AF occurs in more than half of individuals with HF, and HF in more than one third of individuals with AF at some point of time. We found that AF precedes and follows both HFpEF and HFrEF, with some differences in temporal association: prevalent AF was more strongly associated with incident HF with preserved ejection fraction. Lastly, AF and HF conjointly portend a poor prognosis, with a higher risk among those with reduced ejection fraction. These findings shed light on the complex association of atrial fibrillation and heart failure, and future studies focused on underlying mechanisms of these dual conditions, and potential therapeutic strategies are warranted.
Acknowledgments
Funding Sources: This work was partially supported by the National Heart, Lung and Blood Institute's Framingham Heart Study (Contract No. N01-HC-25195 and HHSN268201500001I). This work was supported by the National Institutes of Health - K23-HL116780 (Dr. Ho). Dr. Ho is supported by a Boston University School of Medicine, Department of Medicine Career Investment award (Boston, MA). Dr. Lubitz is supported by NIH/NHLBI K23HL114724 and a Doris Duke Charitable Foundation Clinical Scientist Development Award 2014105.
Footnotes
Disclosures: None.
References
- 1.Braunwald E. Shattuck lecture--cardiovascular medicine at the turn of the millennium: triumphs, concerns, and opportunities. N Engl J Med. 1997;337:1360–1369. doi: 10.1056/NEJM199711063371906. [DOI] [PubMed] [Google Scholar]
- 2.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Després J, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh RW, Turner MB. American Heart Association Statistics Committee, Subcommittee SS. Heart disease and stroke statistics-2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 3.Colilla S, Crow A, Petkun W, Singer DE, Simon T, Liu X. Estimates of current and future incidence and prevalence of atrial fibrillation in the U.S. adult population. Am J Cardiol. 2013;112:1142–1147. doi: 10.1016/j.amjcard.2013.05.063. [DOI] [PubMed] [Google Scholar]
- 4.Ho KK, Anderson KM, Kannel WB, Grossman W, Levy D. Survival after the onset of congestive heart failure in Framingham Heart Study subjects. Circulation. 1993;88:107–115. doi: 10.1161/01.cir.88.1.107. [DOI] [PubMed] [Google Scholar]
- 5.McManus DD, Hsu G, Sung SH, Saczynski JS, Smith DH, Magid DJ, Gurwitz JH, Goldberg RJ, Go AS Study CRNP. Atrial fibrillation and outcomes in heart failure with preserved versus reduced left ventricular ejection fraction. J Am Heart Assoc. 2013;2:e005694. doi: 10.1161/JAHA.112.005694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dries DL, Exner DV, Gersh BJ, Domanski MJ, Waclawiw MA, Stevenson LW. Atrial fibrillation is associated with an increased risk for mortality and heart failure progression in patients with asymptomatic and symptomatic left ventricular systolic dysfunction: a retrospective analysis of the SOLVD trials. Studies of Left Ventricular Dysfunction. J Am Coll Cardiol. 1998;32:695–703. doi: 10.1016/s0735-1097(98)00297-6. [DOI] [PubMed] [Google Scholar]
- 7.Wang TJ, Larson MG, Levy D, Vasan RS, Leip EP, Wolf PA, D'Agostino RB, Murabito JM, Kannel WB, Benjamin EJ. Temporal relations of atrial fibrillation and congestive heart failure and their joint influence on mortality: the Framingham Heart Study. Circulation. 2003;107:2920–2925. doi: 10.1161/01.CIR.0000072767.89944.6E. [DOI] [PubMed] [Google Scholar]
- 8.Eapen ZJ, Greiner MA, Fonarow GC, Yuan Z, Mills RM, Curtis LH. Associations between atrial fibrillation and early outcomes of patients with heart failure and reduced or preserved ejection fraction. Am Heart J. 167:369–375. doi: 10.1016/j.ahj.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Melenovsky V, Hwang S, Redfield MM, Zakeri R, Lin G, Borlaug BA. Left atrial remodeling and function in advanced heart failure with preserved or reduced ejection fraction. Circ Heart Fail. 2015;8 doi: 10.1161/CIRCHEARTFAILURE.114.001667. 295-303-303. [DOI] [PubMed] [Google Scholar]
- 10.Olsson LG, Ducharme A, Granger CB, Michelson EL, McMurray JJV, Puu M, Yusuf S, Pfeffer MA, Investigators C. Atrial fibrillation and risk of clinical events in chronic heart failure with and without left ventricular systolic dysfunction: results from the Candesartan in Heart failure-Assessment of Reduction in Mortality and morbidity (CHARM) program. J Am Coll Cardiol. 2006;47:1997–2004. doi: 10.1016/j.jacc.2006.01.060. [DOI] [PubMed] [Google Scholar]
- 11.Cheng M, Lu X, Huang J, Zhang J, Zhang S, Gu D. The prognostic significance of atrial fibrillation in heart failure with a preserved and reduced left ventricular function: insights from a meta-analysis. Eur J Heart Fail. 2014;16:1317–1322. doi: 10.1002/ejhf.187. [DOI] [PubMed] [Google Scholar]
- 12.Kannel WB, Feinleib M, McNamara PM, Garrison RJ, Castelli WP. An investigation of coronary heart disease in families The Framingham offspring study. Am J Epidemiol. 1979;110:281–290. doi: 10.1093/oxfordjournals.aje.a112813. [DOI] [PubMed] [Google Scholar]
- 13.Levy D, Labib SB, Christiansen JC, Anderson KM. Determinants of sensitivity and specificity of electrocardiographic criteria for left ventricular hypertrophy. Circulation. 1990;81:815–820. doi: 10.1161/01.cir.81.3.815. [DOI] [PubMed] [Google Scholar]
- 14.Gaynor JJ, Feuer EJ, Tan CC, Wu DH, Little CR, Straus DJ, Clarkson BD, Brennan MF. On the use of cause-specific failure and conditional failure probabilities: examples from clinical oncology data. J Am Stat Assoc. 1993;88:400–409. [Google Scholar]
- 15.Alonso A, Krijthe BP, Aspelund T, Stepas KA, Pencina MJ, Moser CB, Sinner MF, Sotoodehnia N, Fontes JD, Janssens AC, Kronmal RA, Magnani JW, Witteman JC, Chamberlain AM, Lubitz SA, Schnabel RB, Agarwal SK, McManus DD, Ellinor PT, Larson MG, Burke GL, Launer LJ, Hofman A, Levy D, Gottdiener JS, Kääb S, Couper D, Harris TB, Soliman EZ, Stricker BH, Gudnason V, Heckbert SR, Benjamin EJ. Simple risk model predicts incidence of atrial fibrillation in a racially and geographically diverse population: the CHARGE-AF consortium. J Am Heart Assoc. 2013;2:e000102. doi: 10.1161/JAHA.112.000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lin DY, Wei LJ. The robust inference for the Cox proportional hazards model. J Am Stat Assoc. 1989;84:1074–1078. [Google Scholar]
- 17.Lunn M, McNeil D. Applying Cox regression to competing risks. Biometrics. 1995;51:524–532. [PubMed] [Google Scholar]
- 18.Lip GY, Halperin JL. Improving stroke risk stratification in atrial fibrillation. Am J Med. 2010;123:484–488. doi: 10.1016/j.amjmed.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 19.Piccini JP, Hammill BG, Walkey AJ, Benjamin EJ, Curtis LH, Heckbert SR. Clinical course of atrial fibrillation in older adults: the importance of cardiovascular events beyond stroke. Eur Heart J. 2014;35:250–256. doi: 10.1093/eurheartj/eht483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang TJ, Evans JC, Benjamin EJ, Levy D, LeRoy EC, Vasan RS. Natural history of asymptomatic left ventricular systolic dysfunction in the community. Circulation. 2003;108:977–982. doi: 10.1161/01.CIR.0000085166.44904.79. [DOI] [PubMed] [Google Scholar]
- 21.Schnabel RB, Yin X, Gona P, Larson MG, Beiser AS, McManus DD, Newton-Cheh C, Lubitz SA, Magnani JW, Ellinor PT, Seshadri S, Wolf PA, Vasan RS, Benjamin EJ, Levy D. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: a cohort study. Lancet. 2015:7. doi: 10.1016/S0140-6736(14)61774-8. pii: S0140-6736(14)61774-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Linssen GCM, Rienstra M, Jaarsma T, Voors AA, Van Gelder IC, Hillege HL, van Veldhuisen DJ. Clinical and prognostic effects of atrial fibrillation in heart failure patients with reduced and preserved left ventricular ejection fraction. Eur J Heart Fail. 2011;13:1111–1120. doi: 10.1093/eurjhf/hfr066. [DOI] [PubMed] [Google Scholar]
- 23.Zakeri R, Chamberlain AM, Roger VL, Redfield MM. Temporal relationship and prognostic significance of atrial fibrillation in heart failure patients with preserved ejection fraction: a community-based study. Circulation. 2013;128:1085–1093. doi: 10.1161/CIRCULATIONAHA.113.001475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rusinaru D, Leborgne L, Peltier M, Tribouilloy C. Effect of atrial fibrillation on long-term survival in patients hospitalised for heart failure with preserved ejection fraction. Eur J Heart Fail. 2008;10:566–572. doi: 10.1016/j.ejheart.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 25.Pedersen OD, Søndergaard P, Nielsen T, Nielsen SJ, Nielsen ES, Falstie-Jensen N, Nielsen I, Køber L, Burchardt H, Seibaek M, Torp-Pedersen C investigators DSG. Atrial fibrillation, ischaemic heart disease, and the risk of death in patients with heart failure. Eur Heart J. 2006;27:2866–2870. doi: 10.1093/eurheartj/ehl359. [DOI] [PubMed] [Google Scholar]
- 26.Ahmed MI, White M, Ekundayo OJ, Love TE, Aban I, Liu B, Aronow WS, Ahmed A. A history of atrial fibrillation and outcomes in chronic advanced systolic heart failure: a propensity-matched study. Eur Heart J. 2009;30:2029–2037. doi: 10.1093/eurheartj/ehp222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mahoney P, Kimmel S, DeNofrio D, Wahl P, Loh E. Prognostic significance of atrial fibrillation in patients at a tertiary medical center referred for heart transplantation because of severe heart failure. Am J Cardiol. 1999;83:1544–1547. doi: 10.1016/s0002-9149(99)00144-7. [DOI] [PubMed] [Google Scholar]
- 28.Corell P, Gustafsson F, Schou M, Markenvard J, Nielsen T, Hildebrandt P. Prevalence and prognostic significance of atrial fibrillation in outpatients with heart failure due to left ventricular systolic dysfunction. Eur J Heart Fail. 2007;9:258–265. doi: 10.1016/j.ejheart.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 29.Maisel WH, Stevenson LW. Atrial Fibrillation in Heart Failure: Epidemiology, Pathophysiology, and Rationale for Therapy. Am J Cardiol. 91:2D–8D. doi: 10.1016/s0002-9149(02)03373-8. [DOI] [PubMed] [Google Scholar]
- 30.Tsang TSM, Gersh BJ, Appleton CP, Tajik AJ, Barnes ME, Bailey KR, Oh JK, Leibson C, Montgomery SC, Seward JB. Left ventricular diastolic dysfunction as a predictor of the first diagnosed nonvalvular atrial fibrillation in 840 elderly men and women. J Am Coll Cardiol. 2002;40:1636–1644. doi: 10.1016/s0735-1097(02)02373-2. [DOI] [PubMed] [Google Scholar]
- 31.Rosenberg MA, Gottdiener JS, Heckbert SR, Mukamal KJ. Echocardiographic diastolic parameters and risk of atrial fibrillation: the Cardiovascular Health Study. Eur Heart J. 2012;33:904–912. doi: 10.1093/eurheartj/ehr378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Everett TH, Olgin JE. Atrial fibrosis and the mechanisms of atrial fibrillation. Heart Rhythm. 2007;4:S24–S27. doi: 10.1016/j.hrthm.2006.12.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pedersen OD, Bagger H, Keller N, Marchant B, Køber L, Torp-Pedersen C. Efficacy of dofetilide in the treatment of atrial fibrillation-flutter in patients with reduced left ventricular function: a Danish investigations of arrhythmia and mortality on dofetilide (diamond) substudy. Circulation. 2001;104 doi: 10.1161/01.cir.104.3.292. 292-6-296. [DOI] [PubMed] [Google Scholar]
- 34.Westermann D, Linder D, Kasner M, Zietsch C, Savvatis K, Escher F, Schlippenbach JV, Skurk C, Steendijk P, Riad A, Poller W, Schultheiss H, Tschope C. Cardiac inflammation contributes to changes in the extracellular matrix in patients with heart failure and normal ejection fraction. Circ Heart Fail. 2011:44–52. doi: 10.1161/CIRCHEARTFAILURE.109.931451. [DOI] [PubMed] [Google Scholar]
- 35.Andersen MJ, Borlaug BA. Heart failure with preserved ejection fraction: current understandings and challenges. Curr Cardiol Rep. 2014;16:501. doi: 10.1007/s11886-014-0501-8. [DOI] [PubMed] [Google Scholar]
- 36.Mohammed SF, Hussain S, Mirzoyev SA, Edwards WD, Maleszewski JJ, Redfield MM. Coronary microvascular rarefaction and myocardial fibrosis in heart failure with preserved ejection fraction. Circulation. 2015;131:550–559. doi: 10.1161/CIRCULATIONAHA.114.009625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Roy D, Talajic M, Nattel S, Wyse DG, Dorian P, Lee KL, Bourassa MG, Arnold JMO, Buxton AE, Camm AJ, Connolly SJ, Dubuc M, Ducharme A, Guerra PG, Hohnloser SH, Lambert J, Le Heuzey J, O'Hara G, Pedersen OD, Rouleau J, Singh BN, Stevenson LW, Stevenson WG, Thibault B, Waldo AL. Rhythm control versus rate control for atrial fibrillation and heart failure. N Engl J Med. 2008;358:2667–2677. doi: 10.1056/NEJMoa0708789. [DOI] [PubMed] [Google Scholar]
- 38.Paulus WJ, Tschöpe C. A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J Am Coll Cardiol. 2013;62:263–271. doi: 10.1016/j.jacc.2013.02.092. [DOI] [PubMed] [Google Scholar]
- 39.Phan TT, Abozguia K, Shivu GN, Ahmed I, Leyva F, Patel K, Fenneaux M. Increased Atrial Contribution to Left Ventricular Filling Compensates for Impaired Early Filling During Exercise in Heart Failure With Preserved Ejection Fraction. J Card Fail. 15:890–897. doi: 10.1016/j.cardfail.2009.06.440. [DOI] [PubMed] [Google Scholar]
- 40.Zakeri R, Borlaug BA, McNulty S, Mohammed SF, Lewis GD, Semigran MJ, Deswal A, LeWinter M, Hernandez AF, Braunwald E, Redfield MM. Original Article Impact of Atrial Fibrillation on Exercise Capacity in Heart Failure With Preserved Ejection Fraction A RELAX Trial Ancillary Study. Circ Heart Fail. 2014;7:123–130. doi: 10.1161/CIRCHEARTFAILURE.113.000568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bavishi C, Khan AR, Ather S. Digoxin in patients with atrial fibrillation and heart failure: A meta-analysis. Int J Cardiol. 2015;188:99–101. doi: 10.1016/j.ijcard.2015.04.031. [DOI] [PubMed] [Google Scholar]
- 42.Agarwal SK, Soliman EZ, Ambrose M, Prineas RJ, Folsom AR. Incidence of atrial fibrillation in whites and African-Americans: the Atherosclerosis Risk in Communities (ARIC) study. Am Heart J. 2009;158:111–117. doi: 10.1016/j.ahj.2009.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bibbins-Domingo K, Pletcher MJ, Lin F, Vittinghoff E, Gardin JM, Arynchyn A, Lewis CE, Williams OD, Hulley SB. Racial differences in incident heart failure among young adults. N Engl J Med. 2009;360:1179–1190. doi: 10.1056/NEJMoa0807265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schnabel RB, Rienstra M, Sullivan LM, Sun JX, Moser CB, Levy D, Pencina MH, Fontes JD, Magnani JW, McManus DD, Lubitz SA, Tadros TM, Wang TJ, Ellinor PT, Vasan RS, Benjamin EJ. Risk assessment for incident heart failure in individuals with atrial fibrillation. Eur J Heart Fail. 2013;15:843–849. doi: 10.1093/eurjhf/hft041. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


