Since the discovery of adipose-derived adult stem (ADAS) cells in adipose tissue [1], many studies have articulated a new concept of lipofilling, which is no longer seen as adipocyte grafting, but rather as stem cell transplantation.
Tonnard et al. [2] proposed a new technique of fat grafting, known as nanofat grafting, which involves an emulsified suspension that can be injected in a more superficial plane through finer needles (27-gauge) than is possible in standard lipofilling.
Vulvar lichen sclerosus (VLS) is a chronic inflammatory disease of the anogenital area that often leads to significant impairments in sexual function and quality of life [3].
In this report, we present a case of advanced VLS treated with nanofat grafting in addition to standard lipofilling. The rationale of this approach was to take advantage of the regenerative capacities of ADAS cells to stimulate cellular growth and wound healing in lesions that do not show a tendency for spontaneous recovery.
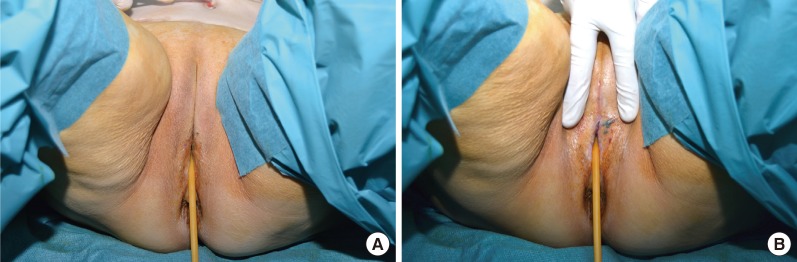
A 48-year-old woman with a history of VLS diagnosed 18 years previously complained of genital distortion making sexual intercourse completely impossible, decreased sexual desire, itching, burning, and soreness. The diagnosis of VLS was confirmed through histological examination. Topical treatments had unsatisfying results, and she suffered from ulcers and infections after every treatment with clobetasol. The patient presented with flattened labia majora, a complete agglutination of the labia minora, and a completely buried clitoris with a large sensation deficit. Additionally, she demonstrated an advanced stage of introitus sclerosis (Fig. 1). These problems led to anorgasmia and lack of sexual activity over the previous three years.
Fig. 1. Preoperative photographs showing flattened labia majora and completely agglutinated labia minora (A). The clitoris is totally buried, and the introitus is narrowed and sclerotic (B).
Under general anaesthesia, we excised the scar tissue over the clitoris and released the adhesions between the clitoris and the hood. Once the clitoris was exposed, the periclitoral skin was sutured to prevent the early recurrence of phimosis. After liposuction and fat processing, we injected 40 mL of standard lipoaspirate into the labia majora and the clitoral area in a subdermal plane to restore the volume deficit.
Following the Tonnard technique [2], we emulsified the lipoaspirate and injected 20 mL of nanofat around the introitus and the clitoris in the intradermal plane, using a 27-gauge needle.
The patient's informed consent was obtained to analyse a sample of 15 mL of nanofat in order to assess the isolation and proliferation of ADAS cells. The population of stem cells was composed of CD44+, CD90+, and CD105+ cells. When viewed under the fluorescence microscope and after staining with Sudan III, the morphology of the adipocytes was found to be normal (data not shown).
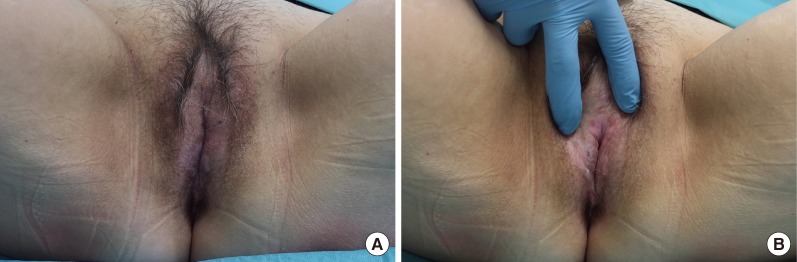
Betamethasone ointment was applied for one week after surgery. Fig. 2 shows the results 10 months after surgery, at which point the labia majora showed a much greater degree of curvature, as observed with a pinch test and photographic comparison. Although partial recurrence of clitoral phimosis was noted, the patient recovered sensation and the ability to experience an orgasm. We planned a second treatment three months after the first surgery, but the patient refused additional treatment due to the improvement in her symptoms. The patient experienced a remarkable improvement in the texture and elasticity of the skin and mucosa, as demonstrated by decreased dryness and dyspareunia. Itching and burning decreased after two months and almost completely disappeared after four months. The patient's sexual function was completely restored. We asked her to complete a questionnaire about her quality of life related to VLS symptoms and sexual activity [4] before and after the treatment, and the authors developed a scoring system for the signs of VLS as observed before surgery and at each examination after surgery [4]. Four items were included in the patient questionnaire: pruritus, burning, soreness, and dyspareunia. Each item was scored from 0 (no complaints) to 10 (an extreme level of complaints), for a maximum score of 40. Six items were included in the clinical questionnaire completed by the physicians: erosion, hyperkeratosis, fissures, agglutination, stenosis, and atrophy; each item was scored on a three-point Likert scale from 0 (normal findings) to 2 (severe changes), for a maximum score of 12. Both final scores were classified as low, medium, and high [4]. The physician administered clinical score was classified as low when it ranged from 0 to 4, medium from 5 to 8 and high from 9 to 12. The patient administered symptom score was classified as low when it reached a maximum of 13, medium between 14 and 26 and high when it was included between 27 and 40.
Fig. 2. Postoperative photographs showing the clitoris and improved labia majora trophism (A), as well as the amelioration of the skin texture in the vaginal introitus 10 months after surgery (B).
The patient's symptoms decreased simultaneously with the signs of VLS. The greatest improvement was reported in the first two months after surgery. The results then remained stable over the following eight months, with slight further amelioration in the signs between the second and fifth months.
The literature of the last century contains many reports about lipofilling and its applications, since adipose tissue is always available without invasive harvesting procedures.
Since the discovery of ADAS cells in adipose tissue [1], many studies have articulated a new conception of lipofilling, which is no longer seen as adipocyte grafting, but rather as stem cell transplantation. The sole purpose of lipofilling was once to achieve volumetric augmentation, but many surgeons are now focusing on the regenerative capacities of ADAS cells and looking forward to new applications. The use of ADAS cells seems to be very helpful in lesions that do not heal spontaneously, such as pathological scars, chronic ulcers, and VLS [5].
Tonnard et al. [2] proposed a new technique of fat grafting, known as nanofat grafting. Nanofat grafting is currently most commonly applied in aesthetic surgery to treat wrinkles and dark coloration of the eyelids.
VLS is a chronic inflammatory disease of the anogenital area with a probable autoimmune pathogenesis. It affects between 1 in 1,000 and 1 in 300 individuals in the general population, and is more common in white postmenopausal women. It typically manifests as atrophic white plaques, purpura, fissuring, sclerosis, and distortion of the anatomic structures with fusion of the labia minora, clitoral phimosis with loss of sensitivity, and progressive narrowing of the vaginal introitus. Common symptoms include pruritus, burning, soreness, and dyspareunia, leading to significantly impaired quality of life. The topical administration of corticosteroids has been shown to have poor results in treating VLS [3].
In VLS, histologic findings are typically characterised by orthokeratotic hyperkeratosis, hydropic degeneration of the basal cells, oedema of the upper dermis, and homogenization of collagen associated with a predominantly lymphocytic inflammatory infiltrate [3]. Since these pathological changes predominantly involve the superficial dermal layer, we believe that nanofat grafting is the best procedure for improving the symptoms and signs of VLS.
Nanofat grafting is a simple procedure that allows the administration of adipose stem cells and growth factors in a very superficial layer to treat several pathological conditions that do not show spontaneous healing, such as lichen sclerosus. The standard lipotransfer technique is much more suitable for treating volume deficits.
This was a preliminary study for a longer series of VLS cases showing that nanofat grafting leads to satisfying results due to the regenerative capacities of ADAS cells.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Zuk PA, Zhu M, Mizuno H, et al. Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng. 2001;7:211–228. doi: 10.1089/107632701300062859. [DOI] [PubMed] [Google Scholar]
- 2.Tonnard P, Verpaele A, Peeters G, et al. Nanofat grafting: basic research and clinical applications. Plast Reconstr Surg. 2013;132:1017–1026. doi: 10.1097/PRS.0b013e31829fe1b0. [DOI] [PubMed] [Google Scholar]
- 3.Gutiérrez-Pascual M, Vicente-Martin FJ, Lopez-Estebaranz JL. Lichen sclerosus and squamous cell carcinoma. Actas Dermosifiliogr. 2012;103:21–28. doi: 10.1016/j.adengl.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 4.Gunthert AR, Duclos K, Jahns BG, et al. Clinical scoring system for vulvar lichen sclerosus. J Sex Med. 2012;9:2342–2350. doi: 10.1111/j.1743-6109.2012.02814.x. [DOI] [PubMed] [Google Scholar]
- 5.Casabona F, Priano V, Vallerino V, et al. New surgical approach to lichen sclerosus of the vulva: the role of adipose-derived mesenchymal cells and platelet-rich plasma in tissue regeneration. Plast Reconstr Surg. 2010;126:210e–211e. doi: 10.1097/PRS.0b013e3181ea9386. [DOI] [PubMed] [Google Scholar]