Abstract
The popularity of electronic (e-) cigarettes has greatly increased recently, particularly in adolescents. However, the extent of psychiatric comorbidity with adolescent e-cigarette use and dual use of conventional (combustible) and e-cigarettes is unknown. This study characterized psychiatric comorbidity in adolescent conventional and e-cigarette use. Ninth grade students attending high schools in Los Angeles, CA (M age=14) completed self-report measures of conventional/e-cigarette use, emotional disorders, substance use/problems, and transdiagnostic psychiatric phenotypes consistent with the NIMH-Research Domain Criteria Initiative. Outcomes were compared by lifetime use of: (1) neither conventional nor e-cigarettes (non-use; N=2557, 77.3%); (2) e-cigarettes only (N=412, 12.4%); (3) conventional cigarettes only (N=152, 4.6%); and (4) conventional and e-cigarettes (dual use; N=189, 5.6%). In comparison to adolescents who used conventional cigarettes only, e-cigarette only users reported lower levels of internalizing syndromes (depression, generalized anxiety, panic, social phobia, and obsessive-compulsive disorder) and transdiagnostic phenotypes (i.e., distress intolerance, anxiety sensitivity, rash action during negative affect). Depression, panic disorder, and anhedonia were higher in e-cigarette only vs. non-users. For several externalizing outcomes (mania, rash action during positive affect, alcohol drug use/abuse) and anhedonia, an ordered pattern was observed, whereby comorbidity was lowest in non-users, moderate in single product users (conventional or e-cigarette), and highest in dual users. These findings: (1) raise question of whether emotionally-healthier (‘lower-risk’) adolescents who are not interested in conventional cigarettes are being attracted to e-cigarettes; (2) indicate that research, intervention, and policy dedicated to adolescent tobacco-psychiatric comorbidity should distinguish conventional cigarette, e-cigarette, and dual use.
Keywords: adolescents, electronic cigarettes, smoking, mental health, comorbidity
Graphical Abstract
INTRODUCTION
Mid-adolescence is a vulnerable developmental period for cigarette smoking uptake, the onset of mental health conditions, and the emergence of comorbid tobacco use and mental health problems (Upadhyaya, Deas, Brady, & Kruesi, 2002). The over-representation of smoking among adolescents with mental health problems generalizes across various conditions (e.g., depressive, mania, anxiety, alcohol/drug use disorders), remains robust after controlling for confounders, and is mediated by theoretically-relevant factors suggesting a causal relation (e.g., beliefs that smoking has mood-modulating effects) (Audrain-McGovern et al., 2012; Upadhyaya et al., 2002). The rapid emergence and appeal of novel tobacco and nicotine products such as electronic (e-) cigarettes raises the question as to whether the same adolescent subgroup with mental health problems is at risk for using these products (Cummins, Zhu, Tedeschi, Gamst, & Myers, 2014). This is important to address because this population may be particularly vulnerable to nicotine addiction, given that neural plasticity during adolescence and neuropathology in psychiatric conditions can enhance the brain’s sensitivity to nicotine (Balfour & Ridley, 2000; Counotte, Smit, Pattij, & Spijker, 2011; Sinha, 2008).
E-cigarettes—electronic devices that deliver inhaled nicotine emulate the sensorimotor properties of conventional (combustible) cigarettes—are gaining popularity among adolescents. According to 2014 estimates, past 30 day use of e-cigarettes is more common than conventional cigarettes among U.S. 8th- (9% vs. 4%) and 10th- (16% vs. 7%) graders, and many adolescent e-cigarette users have never tried conventional cigarettes (Johnston, O’Malley, Miech, Bachman, & Schulenberg, 2015). E-cigarettes may be an attractive alternative to conventional cigarettes among youth because of beliefs that they are less harmful, addictive, malodorous, and costly than conventional cigarettes (Peters, Meshack, Lin, Hill, & Abughosh, 2013). Furthermore, e-cigarettes come in flavors appealing to youth and may be easier to obtain than conventional cigarettes because of inconsistent enforcement of restrictions against sales to minors (Collaco, Drummond, & McGrath-Morrow, 2015). Such factors may facilitate e-cigarette initiation in adolescents who would not otherwise smoke conventional cigarettes and may perhaps have fewer risk factors for smoking (Wills, Knight, Williams, Pagano, & Sargent, 2015)—including mental health problems.
Dual use of conventional and e-cigarettes is also common in adolescents (Johnston et al., 2015; Wills et al., 2015), raising the possibility that some adolescents may use e-cigarettes to substitute for conventional cigarettes in situations where smoking is restricted. Indeed, school bathrooms and staircases are among the most common places adolescents report using e-cigarettes (Peters et al., 2013). Given that adolescents with (vs. without) mental health symptoms are more prone to nicotine dependence (Upadhyaya et al., 2002), these populations could be more likely to initiate use of e-cigarettes to bridge situations when they are not able to smoke, which ultimately could perpetuate the over-representation of smoking among individuals with mental health problems.
While research has yet to characterize the psychiatric comorbidity with patterns of conventional and e-cigarette use in adolescents, a recent study of Hawaiian adolescents found that alcohol/marijuana use and other psychosocial risk factors (e.g., sensation seeking, rebelliousness, emotional/behavioral dysregulation) were highest in dual users, moderate in e-cigarette only users, and lowest in non-users (Wills et al., 2015). Most pairwise comparisons involving conventional cigarette only users were not significant in that study, perhaps limited by reduced statistical power due to the smaller size of this group (N=53) (Wills et al., 2015). Given these findings, stratification of psychiatric comorbidity across dual use, single-product use, and non-use in adolescents is plausible.
The current study characterized the mental health of adolescents who reported ever using e-cigarettes, conventional cigarettes, both, or neither. To provide a wide-ranging picture of psychiatric comorbidity, traditional syndrome-based indices of various depressive, manic, anxiety, and substance use disorders were administered. Consistent with NIMH’s Research Domain Criteria Initiative (Insel et al., 2010), we also assessed several transdiagnostic phenotypes implicated in multiple internalizing and externalizing psychopathologies and conventional cigarette use (e.g., impulsivity, anhedonia, distress tolerance) (Leventhal & Zvolensky, 2015b). Up to this point, data on the psychiatric comorbidity associated with e-cigarette and dual use is virtually absent, leaving unclear as to how the mental health of these two groups compare to conventional cigarette users and non-users. Given that conventional cigarettes and e-cigarettes have both similarities (e.g., the experience of inhaling aerosol/smoke, nicotine intake) and differences (e.g., e-cigarettes are perceived as less harmful than conventional cigarettes; (Ambrose et al., 2014)), whether the patterns of psychiatric comorbidity are similar or different between e-cigarette only users and conventional cigarette users is unclear. As the first study to comprehensively characterize psychiatric comorbidity in adolescent e-cigarette and dual use, this study may yield data that is important to tobacco policy by identifying adolescent populations that are psychiatrically vulnerable and potentially at risk for use of traditional and emerging tobacco products. Such data could highlight the need to protect psychiatrically vulnerable adolescents from tobacco product use take via targeted tobacco product regulation and behavioral health prevention programming for this populations.
METHODS
Participants and Procedure
This report is based on a cross-sectional survey of substance use and mental health among 9th grade students enrolled in ten public high schools surrounding Los Angeles, CA, USA. The schools were recruited based on their adequate representation of diverse demographic characteristics. The percentage of students eligible for free lunch within each school (i.e., student’s parental income ≤ 185% of the national poverty level) on average across the ten schools was 31.1% (SD=19.7, range: 8.0% – 62.4%). Students not in special education (e.g., severe learning disabilities) or English as a Second Language programs were eligible (N=4100). Of the students who assented to participate (N=3,874; 94.5%), 3,383 (82.5%) provided active parental consent and enrolled in the study. In-classroom paper-and-pencil surveys were administered across two 60-minute data collections during the fall of 2013, conducted less than two weeks apart. Some students did not complete all questionnaires within the time allotted or were absent for data collections (n=73), leaving a final sample of 3310. The University of Southern California Institutional Review Board approved the protocol.
Measures
Each study measure described below has shown good psychometric properties in previous adolescent samples (Audrain-McGovern et al., 2004; Bastiani et al., 2013; Eaton et al., 2010; Johnston et al., 2015; Leventhal et al., 2015 in press; Martino, Grilo, & Fehon, 2000; Muris & Meesters, 2008; Pang, Farrahi, Glazier, Sussman, & Leventhal, 2015 in press; Wagner et al., 2006; White & Labouvie, 1989). Unless otherwise specified, a mean score per item composite was calculated and composites were scored such that higher scores reflect higher psychopathology.
Electronic Cigarettes, Conventional Cigarettes, and other Substance Use
Using items derived from the Youth Behavior Risk Surveillance (Eaton et al., 2010) and Monitoring the Future (Johnston et al., 2015) Surveys, lifetime use of e-cigarettes (described as “electronic cigarettes, personal vaporizers; prevalence in this sample = 18.2%) and conventional cigarettes (10.3%) was measured, as well as these additional substances: marijuana (15.1%), one full drink of alcohol (26.5%), inhalants (6.0%), cocaine (1.0%), methamphetamines (0.71%), ecstasy (1.5%), LSD/mushrooms/psychedelics (1.7%), salvia (1.0%), heroin (0.5%), prescription pain killers (2.3%), tranquilizers or sedatives (3.3%), diet pills (1.7%), prescription stimulant pills (0.82%), and other drugs (1.2%). Only substances with lifetime prevalence greater than 5% were analyzed as individual outcomes.
Clinical Syndromes
Revised Children’s Anxiety and Depression Scale (RCADS) (Chorpita, Yim, Moffitt, Umemoto, & Francis, 2000)
The RCADS instructs respondents to report the frequency of 40 different DSM-IV symptoms from 1=never to 4=always. Subscales yield scores for major depression, generalized anxiety disorder, obsessive-compulsive disorder, panic disorder, and social phobia.
Mood Disorder Questionnaire (MDQ) (Hirschfeld et al., 2000)
The MDQ instructs respondents to indicate whether they experienced 13 DSM-IV mania symptoms in the past year (yes=1, no=0). A symptom count sum score was utilized for analyses, per prior work (Boschloo et al., 2014). (Supplemental analyses utilizing the cutoff for probable DSM-IV hypomanic/manic episode yielded the same findings with the continuous score.)
Transdiagnostic Phenotypes
Each of the transdiagnostic phenotype measures described below has been consistently associated with multiple psychopathologies (Audrain-McGovern et al., 2009; Audrain-McGovern et al., 2004; Cyders et al., 2007; Ellis & Rothbart, 2001; Isolan, Salum, Menezes Flores, de Carvalho, & Gus Manfro, 2012; Leventhal et al., 2015 in press; Leyro, Zvolensky, & Bernstein, 2010; Muris et al., 2008; Muris, Schmidt, Merckelbach, & Schouten, 2001; Pang et al., 2015 in press; Smith et al., 2007).
Distress Tolerance Scale (DTS) (Simons & Gaher, 2005)
The 14-item DTS measures capacity to tolerate affective distress (e.g., “I’ll do anything to avoid feeling distressed or upset”) using 5-point ratings (1=strongly disagree, 5=strongly agree).
Childhood Anxiety Sensitivity Index (CASI) (Silverman, Fleisig, Rabian, & Peterson, 1991)
The 18-item CASI measures fear of and concerns about anxiety-related sensations and consequences (e.g., “It scares me when my heart beats fast”; none=0, some=1, a lot=2).
Snaith-Hamilton Pleasure Scale (SHAPS) (Snaith et al., 1995)
The SHAPS assesses anhedonia using 14 self-statements regarding pleasure response to common pleasant experiences (e.g., “I would enjoy seeing others’ smiling faces”; 1=strongly agree, 4=strongly disagree).
Temperament and Character Inventory (TCI)-Impulsivity Scale (Cloninger, Przybeck, Syrakic, & Wetzel, 1994)
The 5-item TCI Impulsivity subscale assesses tendency towards acting on instinct without conscious deliberation (e.g., “I often do things based on how I feel at the moment”). It uses a sum across items (True=1, False=0; range: 0–5).
UPPS-P Impulsive Behavior Scale-Positive and Negative Urgency Subscales (Whiteside & Lynam, 2001)
The UPPS-P Impulsive Behavior Scale(Whiteside et al., 2001) has subscales tapping the tendency towards rash action during states of negative affect (negative urgency; 12 items, e.g., “When I’m upset I often act without thinking”) and positive affect (positive urgency; 14 items, e.g., “I tend to lose control when I am in a great mood”). Items are rated from 1=disagree strongly to 4=agree strongly.
The Early Adolescent Temperament Questionnaire – Revised (EATQ-R)-Inhibitory Control Scale (Ellis et al., 2001)
The 5-item EATQ-R Inhibitory Control scale assesses ability to inhibit reflexive responses (e.g., “When someone tells me to stop doing something, it is easy for me to stop”; 1=almost always true to 5=almost always untrue).
Substance Abuse and Problems
Drug Abuse Screening Test-Adolescent Version (DAST) (Martino et al., 2000)
The 10-item DAST assesses problems associated with use and abuse of drugs other than alcohol (e.g., blackouts, family problems, withdrawal symptoms, legal problems; yes/no). A total sum score (0 – 10) is calculated.
Cannabis Abuse Screening Test (CAST) (LEGLEYE, KARILA, BECK, & REYNAUD, 2007)
The 6-item CAST measures problems experienced from cannabis use (e.g., failed attempts to stop use, social or academic consequences). Participants rate frequency from never (=0) to often (=4) and a sum score is calculated.
Rutgers Alcohol Problem Index (RAPI) (White et al., 1989)
The 23-item RAPI measures the frequency of negative consequences associated with drinking within the last 12 months. Responses to items (0=never to 4=10 or more times) are summed.
Data Analysis
Based on patterns of lifetime use, the sample was divided into: (1) use of neither electronic nor conventional cigarettes (non-use; N=2557); (2) use of conventional cigarettes only (N=152); (3) use of electronic cigarettes only (N=412); (4) use of electronic and conventional cigarettes (dual use; N=189). Primary analyses used generalized linear mixed models (GLMMs) that accounted for clustering of data within school, in which the 4-level cigarette use group variable was a categorical regressor variable and a mental health indicator was the outcome variable, with separate models for each outcome. GLMM specified binary and continuous distributions for the lifetime substance use status and mental health quantitative outcomes, respectively. Because of skewed distributions on the three substance use problems measures, Poisson distributions were specified for these outcomes. For outcomes with omnibus groups differences, we conducted follow up pairwise contrasts using an adjusted p-value, correcting for study-wise false discovery rate of 0.05. GLMMs were adjusted for gender, age, ethnicity, and highest parental education; missing data on covariates were accounted for by dummy coding a ‘missingness’ variable to allow inclusion in analyses. Results are reported as standardized effect size estimates (rs).
RESULTS
Use of e-cigarettes only (12.4%) was more common than conventional cigarettes only (4.6%) and dual (5.7%) use, ps < .0001. Dual use was more common than conventional cigarette use only, p = .04. Demographic characteristics by group are reported in Table 1. Cronbach αs for continuous outcomes are reported in Table 2. The correlations between all of the continuous mental health measures can be found in Supplementary Table 1, which showed a wide range correlations across each pair of constructs (M[SD] r-statistic between two measures = 0.27 [0.20], range: −0.25, 0.77).
Table 1.
Demographic Characteristics by Lifetime Electronic and Conventional Cigarette Use Status
| Lifetime Conventional and Electronic Cigarette Use Status: Descriptive Statistics | Omnibus Test | ||||||
|---|---|---|---|---|---|---|---|
| Outcome | Non-Use (N=2557) | Electronic Cigarettes Only (N=412) | Conventional Cigarettes Only (N=152) | Dual Use (N=189) | Entire Sample | r | p |
| Female, % | 54.4%a | 44.6%b | 59.2%a | 53.2%ab | 53.4% | .07 | .001 |
| Age, M(SD) | 14.07 (0.42)a | 14.10 (0.38)a | 14.18 (0.48)b | 14.17 (0.43)b | 14.08 (0.42) | .08 | .0003 |
| Race/Ethnicity, % | - | - | - | - | - | .03 | .52 |
| American Indian/Alaska Native | 0.9% | 0.5% | 2.0% | 1.6% | 0.9% | ||
| Asian | 17.6% | 14.6% | 9.3% | 5.5% | 16.2% | ||
| Black/African American | 4.5% | 5.0% | 6.0% | 2.7% | 4.9% | ||
| Hispanic/Latino | 45.0% | 50.5% | 54.7% | 59.0% | 46.9% | ||
| Native Hawaiian/Pacific Islander | 3.1% | 5.3% | 2.0% | 3.3% | 3.4% | ||
| White | 16.7% | 12.6% | 12.7% | 15.3% | 15.6% | ||
| Other | 5.9% | 4.0% | 6.8% | 7.1% | 5.6% | ||
| Multi-ethnic/Multi-Racial | 5.8% | 7.5% | 6.8% | 5.5% | 6.0% | ||
| Highest Parental Education, % | -a | -ac | -bc | -b | .10 | <.0001 | |
| Unknown | 13.4% | 11.4% | 13.8% | 14.3% | 13.2% | ||
| 8th grade or less | 3.1% | 2.2% | 5.9% | 9.0% | 3.5% | ||
| Some high school | 6.8% | 10.7% | 12.5% | 13.8% | 7.9% | ||
| High school graduate | 13.4% | 18.2% | 21.1% | 14.9% | 14.5% | ||
| Some college | 17.0% | 17.0% | 11.8% | 22.2% | 17.1% | ||
| College graduate | 28.4% | 28.6% | 21.1% | 15.3% | 27.3% | ||
| Graduate degree | 17.9% | 11.9% | 13.8% | 9.5% | 16.5% | ||
Note. Ns range from 2873 to 3310 for each analysis due to different patterns of missing data or reporting “unknown” as a response. across outcomes. Results from omnibus and pairwise tests for group differences in psychiatric and substance use variables using generalized linear mixed models accounting for data nested by school. Groups that share superscripts are not significantly different from one another in pairwise contrasts using unadjusted p-values (p < .05).
Table 2.
Psychiatric and Substance Use by Lifetime Electronic and Conventional Cigarette Use Status
| Lifetime Conventional and Electronic Cigarette Use Status: Descriptive Statistics | Omnibus Test | ||||||
|---|---|---|---|---|---|---|---|
| Outcome | Cronbach α1 | Non-Use (N=2557) | Electronic Cigarettes Only (N=412) | Conventional Cigarettes Only (N=152) | Dual Use (N=189) | r | p |
| Clinical Syndromes, M(SD) | |||||||
| Mania | .77 | 5.15 (3.07)a | 6.22 (3.28)b | 6.34 (2.97)bc | 6.84 (3.58)c | .18 | <.0001 |
| Major Depression | .93 | 0.73 (0.68)a | 0.82 (0.67)c | 1.14 (0.60)b | 1.05 (0.84)b | .16 | <.0001 |
| Generalized Anxiety | .89 | 1.32 (0.77)a | 1.36 (0.76)a | 1.64 (0.81)b | 1.51 (0.84)b | .10 | <.0001 |
| Panic | .90 | 0.45 (0.56)a | 0.52 (0.57)c | 0.77 (0.77)b | 0.69 (0.78)b | .14 | <.0001 |
| Social Phobia | .92 | 1.33 (0.81)a | 1.27 (0.78)a | 1.52 (0.82)b | 1.24 (0.85)a | .05 | .03 |
| Obsessive Compulsive | .82 | 0.71 (0.63)a | 0.74 (0.61)a | 0.95 (0.70)b | 0.92 (0.73)b | .10 | <.0001 |
| Transdiagnostic Phenotypes, M(SD) | |||||||
| Anxiety Sensitivity | .88 | 1.69 (0.39)ac | 1.64 (0.38)a | 1.82 (0.42)bd | 1.73 (0.42)cd | .08 | .0003 |
| Distress Tolerance | .84 | 2.53 (0.84)a | 2.58 (0.79)a | 2.82 (0.88)b | 2.75 (0.98)b | .09 | <.0001 |
| Anhedonia | .90 | 1.65 (0.47)a | 1.79 (0.49)b | 1.86 (0.60)bc | 1.94 (0.61)c | .15 | <.0001 |
| Negative Urgency | .89 | 1.90 (0.64)a | 2.02 (0.62)c | 2.23 (0.67)b | 2.26 (0.66)b | .16 | <.0001 |
| Positive Urgency | .94 | 1.58 (0.61)a | 1.77 (0.63)c | 1.86 (0.65)bc | 1.92 (0.68)b | .16 | <.0001 |
| Impulsivity | .57 | 0.48 (0.30)a | 0.56 (0.26)b | 0.55 (0.29)b | 0.59 (0.26)b | .13 | <.0001 |
| Inhibitory Control | .38 | 2.36 (0.63)a | 2.49 (0.58)b | 2.57 (0.58)b | 2.52 (0.60)b | .10 | <.0001 |
| Lifetime Substance Use, % | |||||||
| Any prescription drug | 2.2%a | 8.8%c | 18.4%b | 27.8%b | .23 | <.0001 | |
| Any illicit drug | 6.1%a | 35.0%b | 46.1%b | 77.8%c | .38 | <.0001 | |
| Alcohol | 15.0%a | 53.5%b | 62.3%b | 84.9%c | .37 | <.0001 | |
| Marijuana | 5.7%a | 34.2%b | 44.1%b | 78.5%c | .38 | <.0001 | |
| Inhalants | 2.6%a | 11.1%b | 17.5%b | 32.6%c | .26 | <.0001 | |
| Substance Use Problems, M(SD) | |||||||
| Alcohol Problems | .91 | 2.25 (4.17)a | 4.24 (5.62)b | 5.18 (6.24)bc | 7.52 (0.83)c | .19 | <.0001 |
| Cannabis Abuse | .92 | 0.27 (1.55)a | 1.94 (3.73)b | 2.62 (4.28)b | 5.70 (5.97)c | .27 | <.0001 |
| Drug Abuse | .82 | 0.20 (0.79)a | 1.00 (1.66)b | 1.39 (1.76)b | 2.92 (2.50)c | .32 | <.0001 |
Note. Ns range from 3121 to 3310 for each analysis due to different patterns of missing data across outcomes. All outcomes are coded such that higher scores reflect more severe pathology. Results from omnibus and pairwise tests for group differences in psychiatric and substance use variables after adjusting for gender, age, ethnicity, and highest parental education using generalized linear mixed models accounting for data nested by school. Groups that share superscripts are not significantly different from one another in pairwise contrasts using an adjusted p-value, corrected for study-wise false discovery rate of .05.
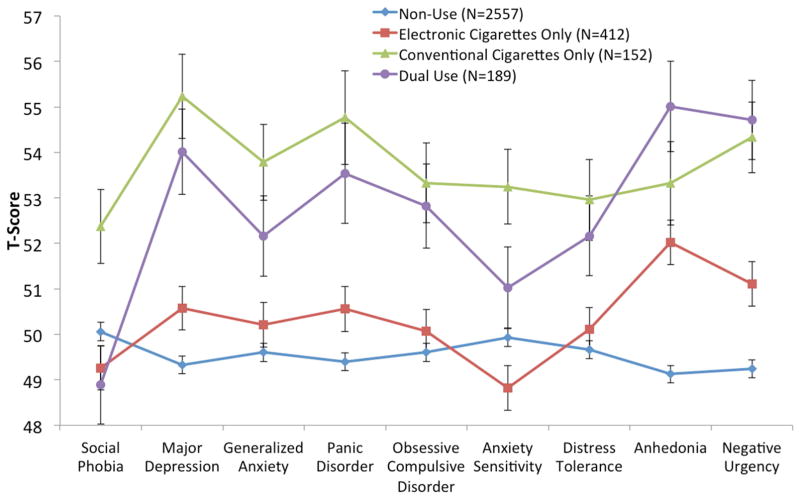
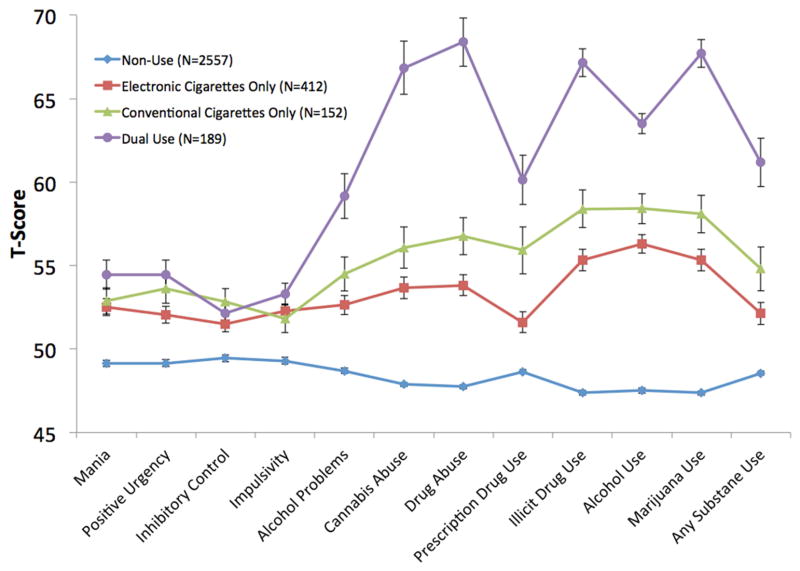
As illustrated in Table 2, there were omnibus differences across the four groups for all outcomes. Pairwise contrasts indicated that adolescents who used conventional cigarettes only reported worse mental health than non-users and e-cigarette only users on multiple internalizing emotional syndromes (i.e., major depression, generalized anxiety, panic, social phobia, and obsessive compulsive disorder) and transdiagnostic phenotypes (i.e., distress tolerance, anxiety sensitivity, negative urgency; see Table 2). On these internalizing-emotional outcomes, the conventional cigarettes only and dual use groups did not significantly differ. For some internalizing outcomes (i.e., anhedonia, major depression, panic disorder), e-cigarette only users had higher elevations than non-users, but lower problem levels than conventional only or dual users. Relative to non-users, use of either product (e-cigarettes only, conventional cigarettes only, or dual use) was related to the externalizing phenotypes of poorer inhibitory control and impulsivity. An ordered effect of dual use vs. e-cigarette use only vs. non-use was found for elevations in mania, positive urgency, and anhedonia. An ordered effect of dual use vs. either single product use (e-cigarettes only or conventional cigarettes only) vs. non-use was also found for lifetime use status and level of abuse/problems for all substances.
Given the differences in patterns across internalizing (i.e., negative emotion-related) and externalizing and positive-emotion seeking (i.e., mania, behavioral dyscontrol, substance use) behaviors, syndromes, and traits, we plotted standardized T-scores of the outcomes by conventional/e-cigarette use status separately in the two domains. These figures respectively illustrate general trends of: (a) differentiation of conventional and dual cigarette use from never and e-cigarette use on most internalizing outcomes (Figure 1), and (b) tri-level ordered differentiation of never vs. single product vs. dual use on externalizing outcomes (Figure 2).
Figure 1.
Mean (±SE) of Internalizing Type Syndromes and Traits by Lifetime Conventional/E-Cigarette Use. Reported as Standardized T-Scores (M=50, SD=15).
Figure 2.
Mean (±SE) of Externalizing Type Syndromes and Traits by Lifetime Conventional/E-Cigarette Use. Reported as Standardized T-Scores (M=50, SD=15).
Analyses of the substance problem outcomes utilizing the overall sample cannot distinguish between substance ever-users who report zero drug/alcohol-related problems and substance never-users. To identify whether e- and conventional-cigarette use status differentiates level of substance problems among substance ever-users, a supplementary analysis of the three substance problem outcomes was conducted that limited each analysis to ever-users of the respective substance using the same GLMM analytic strategy and covariates as the primary analyses with a continuous outcome distribution specified. As in the analysis in the primary sample, these analyses of substance ever-users generally showed an ordered pattern whereby dual tobacco product users reported the highest levels of alcohol, cannabis, and drug problems, followed by single tobacco product users (either conventional- or e-cigarette use), and then never-users of either tobacco product, respectively (see supplementary table 2).
DISCUSSION
This study is the first to comprehensively examine differences in psychiatric profiles between four different groups based on typologies of tobacco product use: (1) non-users; (2) e-cigarette only users; (3) conventional cigarette only users; and (4) dual users. This novel 4-group comparison is a critical innovation; with changes in the pattern of tobacco product use in the past several years, new typologies of adolescent tobacco product use have emerged, including both e-cigarette and dual use (Arrazola et al., 2015; Dutra & Glantz, 2014). Given the relative lack of data to suggest that additional psychiatric problems would be associated with e-cigarette vs. conventional cigarette or dual use, it was unclear whether e-cigarette only users would differ from the other user groups in psychiatric comorbidity.
This study’s main findings were that: (1) e-cigarette only users reported a level of internalizing mental health problems midway between non-use and conventional cigarette use; and (2) externalizing/substance use comorbidity was extensive and followed an ordered pattern with dual users having the most severe and pervasive comorbidity, followed by single-product users and non-users, respectively. These results are novel and raise an important question as to whether e-cigarette use may be common in ‘lower-risk’ subgroups of the adolescent population (including those with better mental health) who otherwise are not attracted to other tobacco products, like conventional cigarettes. These results are broadly consistent with recent data in adults (Cummins et al., 2014) as well as Wills et al.’s study of psychosocial risk factors and alcohol/marijuana use in Hawaiian 9th/10th graders, which found that e-cigarette users were at an intermediate risk status in between non-users and dual users (Wills et al., 2015). In the current sample of Los Angeles 9th graders, a similar pattern of differentiation by dual vs. e-cigarette only vs. non-use is seen that extends across a number of mental health syndromes and transdiangostic phenotypes. The current study also found that conventional cigarette only users have worse internalizing mental health problems than e-cigarette only users. Overall, it is clear that future research and intervention dedicated to comorbidity between use of tobacco (or tobacco-like) products and mental health problems in adolescents should assess and distinguish between use of conventional cigarettes only, e-cigarettes only, and dual use.
For eight internalizing emotional disorder symptoms and phenotypes, adolescents who used e-cigarettes only reported an intermediate level of problems which was lower than conventional cigarette only users on seven outcomes and higher than never-users on three outcomes. Prior research suggests that adolescents with better (vs. worse) emotional health are more strongly deterred from initiating smoking due to concerns about smoking’s negative effects on health and social acceptability (Stone & Leventhal, 2014). Thus, emotionally-healthier adolescents may be more willing to use e-cigarettes, which are generally perceived to be more socially acceptable and less harmful than conventional cigarettes (Wills et al., 2015). The availability of tobacco products that are perceived as less harmful and more socially acceptable, like e-cigarettes, may lower the threshold of risk for tobacco product experimentation associated with certain mental health problems.
Externalizing behavioral comorbidities (i.e., substance use and abuse, impulsivity, poor inhibitory control, tendency toward rash action during positive affect) and mania were elevated in adolescents who used e-cigarettes only versus those who use never used either tobacco product. Adolescents who used conventional cigarettes only also showed this pattern relative to those who never used either tobacco product, which extends prior research on tobacco-psychiatric comorbidity (Upadhyaya et al., 2002). Moreover, this study provides novel data indicating use of e-cigarettes per se is not universally linked with all types of mental health comorbidities; rather use of e-cigarettes alone (vs. non-use) is associated more prominently with externalizing problems and less prominently with internalizing problems.
A clear gradient was observed in which substance use/problems, mania, and positive urgency that successively increased with the number of tobacco products used (dual vs. single vs. never users). One explanation for these findings is that adolescent cigarette smokers with these comorbidities may be more nicotine dependent and may therefore be motivated to also use e-cigarettes to alleviate withdrawal during times when they cannot smoke (Peters et al., 2013). Indeed, these disorders are linked with more severe conventional cigarette dependence (Griesler, Hu, Schaffran, & Kandel, 2011). Another explanation is that adolescents with substance use and mania comorbidity who have experimented with e-cigarette use may not derive enough reinforcement from e-cigarettes, which may be an important factor given prior evidence that conventional cigarette smokers with these comorbidities report stronger motivation to smoke for positive reinforcement (Kahler et al., 2010). Because e-cigarettes have provided less reliable nicotine delivery and reinforcement than conventional cigarettes in novice users (Evans & Hoffman, 2014), adolescents with substance use and mania comorbidities who have tried e-cigarettes may be motivated to subsequently experiment with conventional cigarettes in an effort to find a product that provides stronger and more consistent rewarding effects. An additional perspective is that substance experimentation is driven by a drive for pleasure and means for rebelling against norms (Wills et al., 2015), and that teens with externalizing mental health problems are motivated to experiment with a wider array of multiple substances, including e-cigarettes, conventional cigarettes, and other drugs. Further longitudinal evaluation of these hypotheses is necessary and future research should explore whether there is a gradient in the intensity of intervention needed in preventing conventional cigarette smoking and dual use.
This study had several strengths, including a comprehensive four-group comparison strategy that distinguished four unique patterns of tobacco product use, broad sampling of mental health syndromes and cross-cutting traits, and utilization of a large, diverse sample. The cross-sectional design does not permit an assessment of the temporal precedence of the mental health problems and the use of conventional/e-cigarettes. Accordingly, this study cannot speak to etiological mechanisms underpinning the link between mental health and tobacco product use. Because the survey did not assess past 30-day e-cigarette use, use frequency and progression in use, persistence of use, and nicotine strength (i.e., whether products contain nicotine and at what level), several aspects regarding the quality and profile of e-cigarette and conventional cigarette use are not addressed in this study. Furthermore, the focus on lifetime use leaves unclear whether findings generalize to brief experimentation or more persistent use patterns. To limit burden on students and class time, brief self-report measures were used. As such, these results reflect self-reported symptoms, and the extent to which they generalize to psychiatric diagnoses is unclear. Future work utilizing structured clinical interviews are warranted to identify diagnoses associated with conventional and e-cigarette use.
This is first the investigation to characterize adolescent psychiatric comorbidity in an era when the extensive popularity of e-cigarettes in youth is now clearly established. The current data are of use for policy and tobacco and mental illness intervention by elucidating a subpopulation based on mental health status that may be at higher risk for use of traditional and emerging tobacco products. Describing patterns of psychiatric comorbidity between different forms of tobacco product use in teens provides clues to practitioners on assessment and intervention. For instance, these findings suggest that if a teen is a dual user or conventional cigarette smoker, she or he may be more likely to have comorbid mental health problems than teens who use e-cigarettes only; practitioners should thus make mental health assessment a priority such populations. Similarly, these findings suggest that teens with mild levels of emotional pathology may nonetheless be at elevated likelihood of e-cigarette use and should be asked by practitioners about their e-cigarette use patterns, particularly given recent evidence that teens who use e-cigarettes are more likely to initiate combustible tobacco product use.(Leventhal et al., 2015a; Primack, Soneji, Stoolmiller, Fine, & Sargent, 2015). These results also raise the possibility that adolescents with more severe and pervasive mental health problems could be more vulnerable to factors that increase risk of initiation of e-cigarettes and dual use in teen populations. Some of these risk factors could be targeted via regulation (e.g., youth exposure to e-cigarette advertising, restrictions on ability for minors to purchase e-cigarettes, flavorings and other elements of e-cigarettes and conventional cigarettes that could attract youths) or intervention (e.g., tobacco prevention media campaigns that tailor message characteristics to sufficiently resonate with youth with certain behavioral tendencies; Allen, Vallone, Vargyas, & Healton, 2009). The current results may also have implications for patterns of comorbidity that are likely to arise in the future. Namely, emotionally-healthier individuals who previously might be deterred from using any tobacco products may now be at risk for uptake of e-cigarettes or other emerging products. Furthermore, individuals with certain behavioral comorbidities may be more prone to use multiple products, which may alter the trajectory of future conventional cigarette smoking in patterns that remain to be seen.
Supplementary Material
Supplemental Table 1. Correlation Among Study Outcomes
Supplemental Table 2. Substance Use Problems by Lifetime Electronic and Conventional Cigarette Use Status in the Subsamples of Ever-Users of Each Respective Substance
HIGHLIGHTS.
Relative to conventional cigarette only users, e-cigarette only users reported lower levels of internalizing mental health syndromes (depression, generalized anxiety, panic disorder, social phobia, and obsessive-compulsive disorder) and traits (i.e., distress intolerance, fear of anxiety-related sensations, rash action during negative affect).
Depression, panic disorder, and inability to experience pleasure (i.e., anhedonia) were higher in e-cigarette only users vs. non-users.
For externalizing mental health (mania, rash action during positive affect, alcohol/drug use/abuse) and anhedonia, comorbidity was lowest in non-users, moderate in single-product users (conventional or e-cigarette), and highest in dual users.
Adolescent e-cigarette use is characterized by emotional problems midway between non-use and conventional cigarette use. Dual use is associated with pervasive psychiatric comorbidity.
Acknowledgments
Funding: This research was supported by National Institutes of Health Grant R01-DA033296, and the funding agency had no role in the design or execution of the study.
Footnotes
Disclosures: The authors report no potential conflicts of interests
Author contributions: AML conducting the analyses and oversaw data collection. AML and JAM conceptualized and wrote the majority of the manuscript text. DRS, MGK, SS, JBU, and JBT aided in study conceptualization and provided feedback on drafts.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allen JA, Vallone D, Vargyas E, Healton CG. The truth campaign: Using counter marketing to reduce youth smoking. In: Zimmerman BHR, editor. The new world of health promotion, New program development, implementation and evaluation. Sudbury, MA: Jones and Bartlett; 2009. pp. 195–215. [Google Scholar]
- Ambrose BK, Rostron BL, Johnson SE, Portnoy DB, Apelberg BJ, Kaufman AR, Choiniere CJ. Perceptions of the relative harm of cigarettes and e-cigarettes among U.S. youth. Am J Prev Med. 2014;47:S53–60. doi: 10.1016/j.amepre.2014.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arrazola RA, Singh T, Corey CG, Husten CG, Neff LJ, Apelberg BJ, Bunnell RE, Choiniere CJ, King BA, Cox S, McAfee T, Caraballo RS. Tobacco use among middle and high school students - United States, 2011–2014. MMWR Morb Mortal Wkly Rep. 2015;64:381–385. [PMC free article] [PubMed] [Google Scholar]
- Audrain-McGovern J, Rodriguez D, Epstein LH, Cuevas J, Rodgers K, Wileyto EP. Does delay discounting play an etiological role in smoking or is it a consequence of smoking? Drug Alcohol Depend. 2009;103:99–106. doi: 10.1016/j.drugalcdep.2008.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Audrain-McGovern J, Rodriguez D, Rodgers K, Cuevas J, Sass J, Riley T. Reward expectations lead to smoking uptake among depressed adolescents. Drug Alcohol Depend. 2012;120:181–189. doi: 10.1016/j.drugalcdep.2011.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Audrain-McGovern J, Rodriguez D, Tercyak KP, Cuevas J, Rodgers K, Patterson F. Identifying and characterizing adolescent smoking trajectories. Cancer Epidemiol Biomarkers Prev. 2004;13:2023–2034. [PubMed] [Google Scholar]
- Balfour DJ, Ridley DL. The effects of nicotine on neural pathways implicated in depression: a factor in nicotine addiction? Pharmacology, biochemistry, and behavior. 2000;66:79–85. doi: 10.1016/s0091-3057(00)00205-7. [DOI] [PubMed] [Google Scholar]
- Bastiani L, Siciliano V, Curzio O, Luppi C, Gori M, Grassi M, Molinaro S. Optimal scaling of the CAST and of SDS Scale in a national sample of adolescents. Addict Behav. 2013;38:2060–2067. doi: 10.1016/j.addbeh.2012.12.016. [DOI] [PubMed] [Google Scholar]
- Boschloo L, Spijker AT, Hoencamp E, Kupka R, Nolen WA, Schoevers RA, Penninx BW. Predictors of the onset of manic symptoms and a (hypo)manic episode in patients with major depressive disorder. PLoS One. 2014;9:e106871. doi: 10.1371/journal.pone.0106871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chorpita BF, Yim L, Moffitt C, Umemoto LA, Francis SE. Assessment of symptoms of DSM-IV anxiety and depression in children: a revised child anxiety and depression scale. Behaviour research and therapy. 2000;38:835–855. doi: 10.1016/s0005-7967(99)00130-8. [DOI] [PubMed] [Google Scholar]
- Cloninger C, Przybeck T, Syrakic D, Wetzel R. The Temperament and Character Inventory (TCI): A guide to its development and use. St. Louis, MO: Center for Psychobiology of Personality, Washington University; 1994. [Google Scholar]
- Collaco JM, Drummond MB, McGrath-Morrow SA. Electronic cigarette use and exposure in the pediatric population. JAMA Pediatr. 2015;169:177–182. doi: 10.1001/jamapediatrics.2014.2898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Counotte DS, Smit AB, Pattij T, Spijker S. Development of the motivational system during adolescence, and its sensitivity to disruption by nicotine. Developmental cognitive neuroscience. 2011;1:430–443. doi: 10.1016/j.dcn.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummins SE, Zhu SH, Tedeschi GJ, Gamst AC, Myers MG. Use of e-cigarettes by individuals with mental health conditions. Tobacco control. 2014;23(Suppl 3):iii48–53. doi: 10.1136/tobaccocontrol-2013-051511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders MA, Smith GT, Spillane NS, Fischer S, Annus AM, Peterson C. Integration of impulsivity and positive mood to predict risky behavior: development and validation of a measure of positive urgency. Psychol Assess. 2007;19:107–118. doi: 10.1037/1040-3590.19.1.107. [DOI] [PubMed] [Google Scholar]
- Dutra LM, Glantz SA. Electronic cigarettes and conventional cigarette use among U.S. adolescents: a cross-sectional study. JAMA Pediatr. 2014;168:610–617. doi: 10.1001/jamapediatrics.2013.5488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, Harris WA, Lowry R, McManus T, Chyen D, Lim C, Whittle L, Brener ND, Wechsler H. Youth risk behavior surveillance - United States, 2009. Morbidity and mortality weekly report. Surveillance summaries. 2010;59:1–142. [PubMed] [Google Scholar]
- Ellis L, Rothbart M. Revision of the Early Adolescent Temperament Questionnaire. Poster presented at the Biennial Meeting of the Society for Research in Child Development; Minneapolis, MN. 2001. [Google Scholar]
- Evans SE, Hoffman AC. Electronic cigarettes: abuse liability, topography and subjective effects. Tobacco control. 2014;23(Suppl 2):ii23–29. doi: 10.1136/tobaccocontrol-2013-051489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griesler PC, Hu MC, Schaffran C, Kandel DB. Comorbid psychiatric disorders and nicotine dependence in adolescence. Addiction. 2011;106:1010–1020. doi: 10.1111/j.1360-0443.2011.03403.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschfeld RM, Williams JB, Spitzer RL, Calabrese JR, Flynn L, Keck PE, Lewis L, McElroy SL, Post RM, Rapport DJ, Russell JM, Sachs GS, Zajecka J. Development and validation of a screening instrument for bipolar spectrum disorder: the Mood Disorder Questionnaire. Am J Psychiatry. 2000;157:1873–1875. doi: 10.1176/appi.ajp.157.11.1873. [DOI] [PubMed] [Google Scholar]
- Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, Sanislow C, Wang P. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167:748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Isolan L, Salum G, Menezes Flores S, de Carvalho HW, Gus Manfro G. Reliability and convergent validity of the Childhood Anxiety Sensitivity Index in children and adolescents. Jornal Brasileiro de Psiquiatria. 2012;61 [Google Scholar]
- Johnston LD, O’Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the Future National Survey Results on Drug Use 1975–2014: Overview: Key Findings on Adolescent Drug Use. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2015. [Google Scholar]
- Kahler CW, Leventhal AM, Daughters SB, Clark MA, Colby SM, Ramsey SE, Boergers J, Abrams DB, Niaura R, Buka SL. Relationships of personality and psychiatric disorders to multiple domains of smoking motives and dependence in middle-aged adults. Nicotine Tob Res. 2010;12:381–389. doi: 10.1093/ntr/ntq014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LEGLEYE S, KARILA L, BECK F, REYNAUD M. Validation of the CAST, a general population Cannabis Abuse Screening Test. Journal of Substance Use. 2007;12:233–242. [Google Scholar]
- Leventhal A, Unger J, Audrain-McGovern J, Sussman S, Volk H, Strong D. Measuring anhedonia in adolescents: A psychometric analysis. Journal of Personality Assessment. 2015 doi: 10.1080/00223891.2015.1029072. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal AM, Strong DR, Kirkpatrick MG, Unger JB, Sussman S, Riggs NR, Stone MD, Khoddam R, Samet JM, Audrain-McGovern J. Association of Electronic Cigarette Use With Initiation of Combustible Tobacco Product Smoking in Early Adolescence. JAMA. 2015a;314:700–707. doi: 10.1001/jama.2015.8950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal AM, Zvolensky MJ. Anxiety, depression, and cigarette smoking: a transdiagnostic vulnerability framework to understanding emotion-smoking comorbidity. Psychological bulletin. 2015b;141:176–212. doi: 10.1037/bul0000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyro TM, Zvolensky MJ, Bernstein A. Distress tolerance and psychopathological symptoms and disorders: a review of the empirical literature among adults. Psychol Bull. 2010;136:576–600. doi: 10.1037/a0019712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martino S, Grilo CM, Fehon DC. Development of the drug abuse screening test for adolescents (DAST-A) Addict Behav. 2000;25:57–70. doi: 10.1016/s0306-4603(99)00030-1. [DOI] [PubMed] [Google Scholar]
- Muris P, Meesters C. Reactive and Regulative Temperament in Youths: Psychometric Evaluation of the Early Adolescent Temperament Questionnaire-Revised. Journal of Psychopathology and Behavioral Assessment. 2008;31:7–19. [Google Scholar]
- Muris P, Schmidt H, Merckelbach H, Schouten E. Anxiety sensitivity in adolescents: factor structure and relationships to trait anxiety and symptoms of anxiety disorders and depression. Behaviour research and therapy. 2001;39:89–100. doi: 10.1016/s0005-7967(99)00179-5. [DOI] [PubMed] [Google Scholar]
- Pang R, Farrahi L, Glazier S, Sussman S, Leventhal A. Depressive symptoms, negative urgency and substance use initiation in adolescents. Drug and Alcohol Dependence. 2015 doi: 10.1016/j.drugalcdep.2014.09.771. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters RJ, Meshack A, Lin MT, Hill M, Abughosh S. The social norms and beliefs of teenage male electronic cigarette use. J Ethn Subst Abuse. 2013;12:300–307. doi: 10.1080/15332640.2013.819310. [DOI] [PubMed] [Google Scholar]
- Primack BA, Soneji S, Stoolmiller M, Fine MJ, Sargent JD. Progression to Traditional Cigarette Smoking After Electronic Cigarette Use Among US Adolescents and Young Adults. JAMA Pediatr. 2015:1–7. doi: 10.1001/jamapediatrics.2015.1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman WK, Fleisig W, Rabian B, Peterson RA. Childhood Anxiety Sensitivity Index. Journal of Clinical Child Psychology. 1991;20:162–168. doi: 10.1207/s15374424jccp2801_9. [DOI] [PubMed] [Google Scholar]
- Simons J, Gaher R. The Distress Tolerance Scale: Development and Validation of a Self-Report Measure. Motivation and Emotion. 2005;29:83–102. [Google Scholar]
- Sinha R. Chronic stress, drug use, and vulnerability to addiction. Ann N Y Acad Sci. 2008;1141:105–130. doi: 10.1196/annals.1441.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith GT, Fischer S, Cyders MA, Annus AM, Spillane NS, McCarthy DM. On the validity and utility of discriminating among impulsivity-like traits. Assessment. 2007;14:155–170. doi: 10.1177/1073191106295527. [DOI] [PubMed] [Google Scholar]
- Snaith RP, Hamilton M, Morley S, Humayan A, Hargreaves D, Trigwell P. A scale for the assessment of hedonic tone the Snaith-Hamilton Pleasure Scale. The British journal of psychiatry: the journal of mental science. 1995;167:99–103. doi: 10.1192/bjp.167.1.99. [DOI] [PubMed] [Google Scholar]
- Stone M, Leventhal A. Associations between Anhedonia and Risk Factors for Smoking Initiation among Adolescent Never Smokers. Poster presented at the 20th annual meeting of the Society for Research on Nicotine and Tobacco; Seattle, WA. 2014. [Google Scholar]
- Upadhyaya HP, Deas D, Brady KT, Kruesi M. Cigarette smoking and psychiatric comorbidity in children and adolescents. J Am Acad Child Adolesc Psychiatry. 2002;41:1294–1305. doi: 10.1097/00004583-200211000-00010. [DOI] [PubMed] [Google Scholar]
- Wagner KD, Hirschfeld RM, Emslie GJ, Findling RL, Gracious BL, Reed ML. Validation of the Mood Disorder Questionnaire for bipolar disorders in adolescents. J Clin Psychiatry. 2006;67:827–830. doi: 10.4088/jcp.v67n0518. [DOI] [PubMed] [Google Scholar]
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. J Stud Alcohol. 1989;50:30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR. The five factor model and impulsivity: Using a structural model of personality to understand impulsivity. Pers Individ Dif. 2001;30:669–689. [Google Scholar]
- Wills TA, Knight R, Williams RJ, Pagano I, Sargent JD. Risk factors for exclusive e-cigarette use and dual e-cigarette use and tobacco use in adolescents. Pediatrics. 2015;135:e43–51. doi: 10.1542/peds.2014-0760. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1. Correlation Among Study Outcomes
Supplemental Table 2. Substance Use Problems by Lifetime Electronic and Conventional Cigarette Use Status in the Subsamples of Ever-Users of Each Respective Substance