Abstract
Suicide is a public health concern in older adults. Recent cross sectional studies suggest that impairments in executive functioning, memory and attention are associated with suicidal ideation in older adults. It is unknown whether these neuropsychological features predict persistent suicidal ideation. We analyzed data from 468 individuals ≥ age 60 with major depression who received venlafaxine XR monotherapy for up to 16 weeks. We used latent class growth modeling to classify groups of individuals based on trajectories of suicidal ideation. We also examined whether cognitive dysfunction predicted suicidal ideation while controlling for time-dependent variables including depression severity, and age and education. The optimal model using a zero inflated Poisson link classified individuals into four groups, each with a distinct temporal trajectory of suicidal ideation: those with ‘minimal suicidal ideation’ across time points; those with ‘low suicidal ideation’; those with ‘rapidly decreasing suicidal ideation’; and those with ‘high and persistent suicidal ideation’. Participants in the ‘high and persistent suicidal ideation’ group had worse scores relative to those in the “rapidly decreasing suicidal ideation” group on the Color-Word ‘inhibition/switching’ subtest from the Delis-Kaplan Executive Function Scale, worse attention index scores on the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) and worse total RBANS index scores. These findings suggest that individuals with poorer ability to switch between inhibitory and non-inhibitory responses as well as worse attention and worse overall cognitive status are more likely to have persistently higher levels of suicidal ideation.
Keywords: suicide, trajectory, antidepressant, depression, late life
Introduction
Suicide in older adults is a serious public health concern (Conwell et al., 2011); suicide rates peak in individuals age 65 and older worldwide (WHO Mental Health Suicide Prevention [SUPRE] http://www.who.int/mentalhealth/prevention/suicide/suicideprevent/en). Important risk factors for suicide in older adults include physical illness, financial problems, marital status, gender, chronic pain, race, loss of social ties, and social isolation (Juurlink et al., 2004; Sirey et al., 2008; Forkmann et al., 2012; Morrell et al., 1998; Barraclough, 1971). There is some evidence from cross sectional studies that certain cognitive deficits in older individuals increase their risk for suicidal behavior. In a cross-sectional study, King et al (2000) assessed the role of executive functioning in late-life suicide in a small group of older adults using the Trail Making Test Part B. The findings suggested that there is a greater decline in executive function in those who attempt suicide than in those who do not. In a subsequent cross sectional study, Dombrovski et al., (2008) reported that among older individuals with depression, those with suicidal ideation perform worse on measures of executive function, memory, and attention than those without suicidal ideation.
Gujral et al. (2013) examined global cognition and executive function as correlates of suicidal ideation and suicidal behavior in depressed older adults. Both suicide attempters and suicide ideators performed worse on the Executive Interview (EXIT; Royall et al 1992) compared to non-suicidal depressed or non-psychiatric control subjects. The authors noted that suicide attempters and ideators and non-suicidal depressed subjects had similar total scores on the Dementia Rating Scale score and its Memory and Attention subscales. However, attempters and ideators were impaired with these measures relative to non-psychiatric control subjects. Thus, taken together, these cross-sectional studies suggest that executive dysfunction and other cognitive deficits may play a role in suicidal behavior in older individuals. However, little is known with regard to whether cognitive deficits can predict the course of suicidal ideation over time in adults. Furthermore, another important unanswered question is whether cognitive status can predict persistent suicidal ideation in depressed older adults during the course of antidepressant treatment.
The longitudinal course of suicidal ideation over time in older individuals treated with antidepressants has been examined in 2 studies by Szanto et al (2003; 2007). The 2003 study used survival analysis to determine that while suicidality resolved in almost all older depressed patients with depression treatment, time to response was longer in those with higher suicide risk, i.e., those with a recent attempt or current suicidal ideation. In their 2007 study, the authors further classified elderly patients before and during 12 weeks of antidepressant treatment, as having 1) “non-suicidal”, 2) “emergent”, 3) “persistent”, or 4) “resolved” suicidality. Their classification scheme was based on the temporal patterns of the scores on the suicide item of the Hamilton Depression Rating scale (Hamilton, 1960).
We analyzed data from an NIMH-sponsored clinical trial: “Incomplete Response in Late Life Depression: Getting to Remission” (IRL-GRey; Lenze et al. 2015). The primary aim of this study was to characterize the trajectories of change in suicidal ideation over time in individuals being treated for depression. To address this primary aim, we used latent class growth modelling to explore whether participants could be classified into distinct groups based on clinically meaningful trajectories of suicidal ideation. Our initial hypothesis stated that the latent class modelling approach would classify participants similar to the 4 groups which Szanto et al (2007) noted, i.e., those with 1) “non-suicidal”, 2) “emergent”, 3) “persistent”, or 4) “resolved” suicidality.
Our secondary aim was to examine if cognition was a marker of poorer prognosis. To our knowledge, no published studies to date have examined prospectively the impact of cognitive dysfunction on suicidal ideation over time in elderly depressed individuals. The studies of Szanto et al (2007) compared factors which differed between patients with persistent suicidality and patients with resolving suicidality. They noticed that patients who had resolving suicidality were more likely to be on lithium while those with persistent suicidality were more likely to be on a second antidepressant. In our study, all patients were on venlafaxine XR monotherapy and no other therapeutic doses of secondary antidepressants and/or mood stabilizers; thus we wondered whether other factors such as cognitive dysfunction could have accounted for the differences. Given the recent cross sectional data suggesting that cognitive dysfunction in the elderly appears to be associated with suicidal behavior, we decided to extend those findings by examining whether the association of cognitive dysfunction and suicidal behavior occurs across time and if it could have distinguished groups with persistent suicidal ideation and resolving suicidal ideation. We hypothesized that trajectories of persistent suicidal ideation relative to trajectories of resolving suicidal ideation would be associated with: worse scores of executive function (hypothesis 2); worse subscale scores of the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) (hypothesis 3); and worse total RBANS scores (hypothesis 4).
Methods
We analyzed data from participants in the IRL-GRey study (Lenze et al. 2015), a clinical trial conducted at three academic sites (the University of Pittsburgh, the Centre for Addiction and Mental Health/University of Toronto, and Washington University). Data were collected between 7/2009 and 12/2014. In the current analysis, we included those who participated in the initial open treatment phase of the study (both those who completed the entire phase and those who dropped out). In this phase, individuals aged 60 and older with major depressive disorder were treated openly for up to 16 weeks with venlafaxine XR up to 300 mg/day. They were assessed at baseline, and at weeks one, two, four, six, eight, ten, and then finally at endpoint which was between weeks 12 and 16.
Depression, Suicide, and Neuropsychological Measures
Scales focusing on suicidal ideation and depression were administered at each time point. In addition, neuropsychological assessments were administered at baseline. For this analysis, our primary measure of suicidal ideation was the Beck Scale for Suicidal Ideation (SSI; Beck et al., 1979; 1999; Brown et al., 2000). Time-dependent depressive symptoms were measured with the Montgomery Asberg Depression Rating Scale (MADRS; Montgomery & Asberg, 1979). To assess executive functions, three measures from the Delis-Kaplan Executive Function Scale (D-KEFS; Delis et al., 2001) were used: 1) Color-Word condition 3, called “inhibition” which assesses participants’ ability to inhibit an automatic response (i.e., reading words); instead they must produce a response that requires more effort (i.e., naming the colors of the words); 2) Color-Word condition 4, called ‘inhibition/switching’ which measures both inhibition and set-shifting (i.e., cognitive flexibility); 3) the Trail Making comparison score (trails B/A ratio) which measures cognitive flexibility while controlling for fine motor speed. The DKFS Color Word Inhibition and Inhibition/Switching scores were used with permission from Pearson, Inc. Higher scores on the Color-Word ‘inhibition’ and ‘inhibition/switching’ test reflect better performance. The trails B/A ratio is calculated by dividing the number of seconds to complete condition 4 (which assesses cognitive flexibility) by the number of seconds to complete condition 5 (which assesses motor speed); this removes the ‘speed’ element from the test score so that cognitive flexibility can be ascertained independent of speed (Lezak et al., 2012). Higher scores on this score reflect worse performance.
We used the total score and subscale scores of the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) to characterize global cognitive performance (Duff et al., 2006). The RBANS was developed to assess neurocognitive status in older patients (Randolph et al., 1998). Its subscales assess five domains: immediate memory, delayed memory, language, attention, and visuospatial/constructional ability. The RBANS total score and subscale scores are standardized scores with a mean of 100 and standard deviation of 15. Higher scores reflect better performance.
Procedures
Eligibility criteria were as follows: inclusion criteria comprised age ≥ 60 years; major depressive disorder (MDD), single or recurrent, with a current major depressive episode as diagnosed by the Structured Clinical Interview for DSM-IV Axis 1 disorders (SCID; American Psychiatric Association, 2000); MADRS score ≥ 15. Exclusion criteria included inability to provide informed consent; dementia; lifetime diagnosis of bipolar I or II disorder, schizophrenia, schizoaffective disorder, schizophreniform disorder, delusional disorder, or current psychotic symptoms, as diagnosed by the SCID; abuse of or dependence on alcohol or other substances within the past 3 months; unstable physical illness; high risk for suicide (e.g., active suicidal ideation or current/recent intent or plan) that could not be managed safely in the clinical trial (e.g., unwillingness to be hospitalized); contraindication to venlafaxine XR or aripiprazole; failure to respond to at least 6 weeks of venlafaxine (≥ 225 mg/d) plus aripiprazole (≥ 10 mg/d). Failure to respond to aripiprapazole was an exclusion since later phases of the trial involved randomization to aripiprazole or to placebo (see Lenze et al. 2015).
All potential participants signed an informed consent form approved by the Institutional Review Board at the respective institutions. They were assessed with the SCID and the Mini-Mental State Examination (MMSE; Folstein et al., 1975) to confirm eligibility. All antidepressants and other psychotropic medications (except for low-dose benzodiazepines or sedative-hypnotics) were tapered and discontinued at least two weeks prior to the start of venlafaxine. The titration of venlafaxine was protocolized based on response and tolerability (Lenze et al. 2015).
Data Analysis
Analysis of Baseline and Time-Dependent Variables
Descriptive statistics for baseline demographic and clinical characteristics were computed (means and standard deviations for continuous variables; percentages for categorical variables) for age, years of education, gender, marital status, living status (living alone or not), employment status, and race. The suicide item score was subtracted from the total MADRS score at each time point to obtain a modified MADRS score; this modified score was utilized as a time dependent covariate.
Latent Class Growth Modelling
We employed group-based trajectory modeling to explore whether participants could be classified into distinct groups based on clinically meaningful trajectories of suicidal ideation. We used the PROC TRAJ procedure with STATA 13.0. This method partitions a cohort into subgroups based on repeated measurements of a variable over time. In doing so, it describes heterogeneity that may exist in populations based on longitudinal trajectories (Jones et al 2001; Jones and Nagin, 2007; Andruff et al 2009). Group-based trajectory modeling is data-driven, allowing an exploratory analysis of the patterns that exist within a population that may be difficult to identify a priori. PROC TRAJ can perform analyses using the logistic regression, the censored normal distribution, and the Zero Inflated Poisson model. In this analysis, we used a Zero Inflated Poisson link function given that the data were skewed and many individuals had SSI scores = 0. Furthermore, the logistic regression model was not used since it would have dichotomized the data and resulted in the loss of too much information. Missing data was considered ‘Missing at Random’.
The first step in model selection involved determining the optimal number of distinct subgroups using Bayesian information criterion (BIC; Schwartz et al 1978). This value was used to compare models with different numbers of latent groups. When comparing two models, the model with the smallest absolute value of the BIC was chosen as the more appropriate one (Nagin, 2005; Jones et al 2001). After the optimal number of groups was determined, the optimal polynomial degree of each trajectory was determined by examining permutations of 0 order, linear, quadratic, cubic, quartic, and quintic terms. This was also accomplished by examining the BIC values associated with each model and then choosing the model with the lowest absolute value of the BIC. A final criterion was that the number of subjects in each group had to be at least 5% of the total sample.
The next step in model selection involved adding potential risk factors. The following baseline factors were added: age, years of education, race, living situation (living independently vs. supervised), marital status (currently married: yes or no), gender, employment status, and the relevant cognitive factors (depending on the hypothesis being tested). Site was also included. We retained baseline covariates with p values < 0.05. In addition, education and age were retained regardless of the level of significance given the known dependence of these factors on cognition (Welsh-Bohmer and Attix, 2015); site was also retained regardless of the level of significance. The PROC TRAJ program also provided β coefficients for each covariate; these coefficients provided an estimate of the magnitude of association between a covariate and a particular trajectory and were obtained when comparing different trajectories. The β coefficients were also exponentiated to obtain odds ratios.
The overall process yielded 3 models to test each of the 3 separate hypotheses. The first model determined whether worse baseline scores of executive function were associated with trajectories of persistent suicidal ideation (hypothesis 2) and had the following covariates: education, age, site, Color Word ‘inhibition’ scores, Color Word ‘inhibition/switching’ scores, and Trail Making comparison scores. The second model determined whether worse baseline individual RBANS subscale scores were associated with trajectories of persistent suicidal ideation (hypothesis 3) and had the following covariates: education, age, site, and four of the five RBANS subscale scores: immediate memory, visuospatial construction, attention, and language. The third model determined whether worse RBANS total scores were associated with trajectories of persistent suicidal ideation (hypothesis 4) and included education, age, site and RBANS total scores.
Results
Descriptive Statistics
Summary statistics for baseline demographic and clinical variables are shown in Table 1. Table 2 depicts the time dependent variables – SSI scores (median and range) and total MADRS scores (means and standard deviations). The range of SSI scores over time was 0–31. Most of the SSI scores were 0 and the median SSI scores were 0 at each time point.
Table 1.
Demographic and Clinical Variables
| Demographic Variables | Mean (Standard Deviation) or N (Percent) |
|---|---|
| Race (% white) | 412 (88.03%) |
| Age | 69.03 (7.20) |
| Living status (% with supervision) | 17 (3.63%) |
| Employment status (% employed) | 87 (18.16%) |
| Gender (% female) | 304 (64.96%) |
| Marital Status (% married) | 206 (44.02%) |
| Years of education | 14.39 (2.84) |
| Measures of Executive Function | |
| *D-KEFS Tests | |
| Color Word Condition 4 | 9.91 (3.59) |
| Color Word Condition 3 | 10.10 (3.17) |
| Trail Making Test | |
| ** Trails B/A | 3.27 (0.88–19.50) |
| Repeatable Battery for the Assessment of Neuropsychologic Status (RBANS) | |
| Visuospatial/Construction Score Index | 91.78 (17.37) |
| Immediate Memory Index Score | 96.54 (18.21) |
| Attention Index Score | 98.37 (17.17) |
| Delayed Memory Index Score | 96.17 (15.63) |
| Language Index Score | 97.77 (12.37) |
| Total RBANS Index Score | 94.73(15.95) |
D-KEFS: Delis-Kaplan Executive Function Scale;
median (range); total n = 468
Table 2.
Time Dependent SSI and MADRS scores
| Week | Median (Range of Scale for Suicidal Ideation Scores) | N (Percentage) of Participants with Scale for Suicidal Ideation Scores > 0 | Montgomery Asberg Depression Rating Scale Scores |
|---|---|---|---|
| 0 | 0 (0–24) | 186 (39.8) | 26.67 (5.74) |
| 1 | 0 (0–31) | 107 (25.1) | 22.51 (7.65) |
| 2 | 0 (0–31) | 88 (20.6) | 20.52 (8.41) |
| 4 | 0 (0–20) | 81 (20.0) | 18.65 (8.69) |
| 6 | 0 (0–24) | 65 (16.1) | 17.30 (9.36) |
| 8 | 0 (0–23) | 61 (15.7) | 15.14 (9.36) |
| 10 | 0 (0–18) | 57 (15.1) | 14.24 (9.67) |
| 12–16 | 0 (0–24) | 59 (16.0) | 13.81(10.69) |
The Montgomery Asberg Depression Rating Scale (MADRS) scores represent total scores; the MADRS values represent means (standard deviation). SSI = Beck Scale for Suicidal Ideation
Latent class growth modelling
Our optimal model without covariates using the Zero Inflated Poisson link was a set of trajectories with four groups: the first group was called the ‘minimal suicidal ideation’ group; the second group, ‘low suicidal ideation’ group; the third group, ‘rapidly decreasing suicidal ideation’ group which represented resolving suicidal ideation; and the fourth group, ‘high and persistent suicidal ideation’ group. Our first hypothesis suggested that the four groups resulting from the analysis would be 1) “non-suicidal”, 2) “emergent”, 3) “persistent”, or 4) “resolved” suicidality. Only two of the four groups emerged from the latent class growth modelling procedure which appeared to be similar to the groups that Szanto et al (2007) noticed, i.e., “persistent” and “resolved.”
As depicted in Table 3, when exploring what the optimal number of groups were, we noticed that the absolute values of the BIC values obtained for the 2 group model were all higher than that of the 3 group model; likewise, as the number of groups increased, the absolute values of the BIC values decreased. The five group model yielded the lowest BIC values. Except for a few instances, the percentage of individuals in each of the 5 group models was not always 5% of greater. Thus we used a model which had 4 groups.
Table III.
BIC Values Obtained when Initially Determining the Optimal Numbers of Groups
| Number of groups | Two | Three | Four | Five |
|---|---|---|---|---|
| 1 1 −3918 |
1 1 1 −3355 |
1 1 1 1 −3050 |
1 1 1 1 1 −2956 |
|
| 2 2 −3870 |
2 2 −3306 |
2 2 2 2 −3023 |
2 2 2 2 2 −2938 |
|
| 3 3 −3837 |
3 3 3 −3253 |
3 3 3 3 −3007 |
3 3 3 3 3 −2927 |
|
| 4 4 −3834 |
4 4 4 −3248 |
4 4 4 4 −3009 |
4 4 4 4 4 −3017 |
|
| 5 5 −3836 |
5 5 5 −3272 |
5 5 5 5 −3499 |
5 5 5 5 5 −2962 |
This table depicts Bayesian Information Criteria (BIC) values for the initial model obtained with various groups and polynomial degrees with a zero inflated Poisson link function. Scale for Suicidal Ideation scores was the outcome variable. Since this was an initial exploratory analysis for the purposes of choosing the optimal number of groups, none of the demographic variables nor site were included as covariates; however MADRS scores (after subtracting out the suicide subscale) were still included as a covariate and time was included an independent variable. N= 468 in all cases. Each pair of values represent the polynomial degree of each group of the model (top value) and the associated BIC value (bottom value).
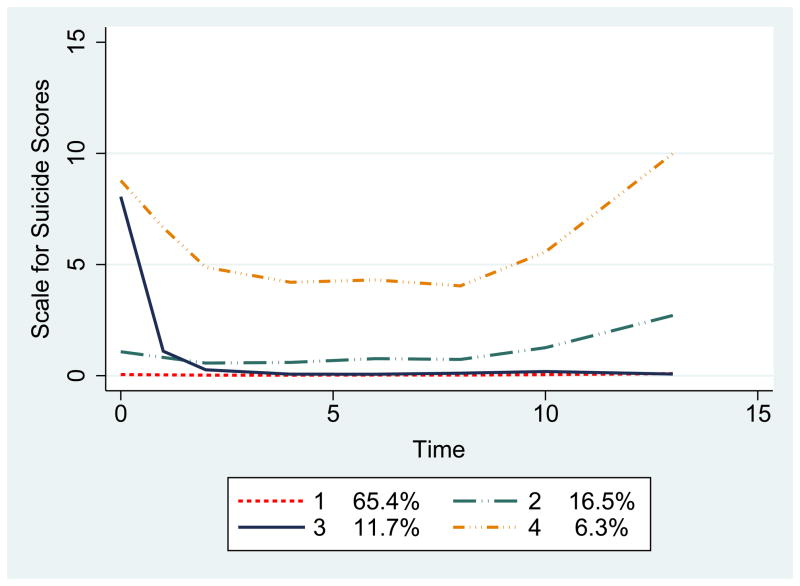
With our optimized model, the four groups remained very similar when different covariates were added (see Figure 1 for a representative set of trajectories from the first model which covaries for each of the three measures of executive function). The three models used to test each of the three different hypotheses differed only slightly in terms of the percent of individuals represented in each trajectory. Furthermore, there were only slight differences in the polynomial degree of each trajectory depending on which cognitive covariates were included. Also, none of the demographic covariates had significant β coefficients when included in the model. However, as mentioned above, we retained age, education, and site as covariates in all the models since these were determined to be important model covariates a priori.
Figure 1.
This figure depicts the four trajectories obtained for Model 1. Covariates included: site, education, age, Color Word ‘inhibition/switching’, Color Word ‘inhibition’ and trails B/A ratio. The percentage of participants in each of the four groups is provided: 1) ‘minimal suicidal ideation’ group; 2) ‘low suicidal ideation’ group; 3) ‘rapidly decreasing suicidal ideation’ group and 4) ‘high and persistent suicidal ideation’ group.
To test our second hypothesis, i.e, that worse executive function would be associated with trajectories of persistent suicidal ideation, we added the three additional cognitive covariates to model 1 which measure executive function: Color Word ‘inhibition’, Color Word ‘inhibition/switching’ and Trail Making comparison score. Based on BIC values, the optimal model obtained included 4 trajectories as follows: the ‘minimal suicidal ideation’ group with 65.4% of the participants and a zero polynomial order; the ‘low suicidal ideation’ group had 16.5% of the participants and a linear polynomial order; the ‘rapidly decreasing suicidal ideation’ group had 11.7% of the participants and a cubic polynomial order; the ‘high and persistent suicidal ideation’ group had 6.3% of the participants and a quadratic polynomial order (see Figure 1). The BIC value obtained with this model was −2902 (n = 443).
When testing hypothesis 2, we examined whether cognitive covariates were significant when comparing the ‘high and persistent suicidal ideation’ and ‘rapidly decreasing suicidal ideation’ groups. Worse scores on the Color Word ‘inhibition/switching’ test were associated with the ‘high and persistent suicidal ideation’ group. The β coefficient (± SD) associated with this covariate was negative and significant: −0.201 ± 0.091 (t = −2.201; df = 443; p = 0.028), consistent with hypothesis 2. The corresponding odds ratio was 0.818 indicating that participants having better scores on the Color Word ‘inhibition/switching’ test were approximately 18% less likely to belong to the ‘high suicidal ideation’ group than the ‘rapidly decreasing suicidal ideation’ group. The other two cognitive covariates -Color Word ‘inhibition’ score and the Trail Making comparison score- were not statistically significant when comparing the two trajectories.
To test our third hypothesis, we determined whether worse scores from each of the subscales of the RBANS were associated with trajectories of persistent suicidal ideation. In addition to including education, age and site as covariates, we included the following four subscales from the RBANS as covariates in Model 2: immediate memory, visuospatial/construction, attention, and language. Delayed memory was not included since the correlation between immediate memory and delayed memory was appreciable (Spearman’s rho = 0.7078). The labels used to describe the four trajectories in Model 2 were the same as that used for Model 1. The BIC value obtained with this model was −3001 (n = 455). In support of hypothesis 3, worse scores in attention were associated with the ‘high and persistent suicidal ideation’ group when compared to the ‘rapidly decreasing suicidal ideation’ group: β =−0.037 ± 0.0178 (t = −2.104; df= 455; p = 0.036). The corresponding odds ratio was 0.964 indicating that participants with higher scores on the RBANS attention subscale had an approximately 4% lower chance of being in the ‘high and persistent suicidal ideation’ group than in the ‘rapidly decreasing suicidal ideation’ group. There were no significant differences noted with the other RBANS subscale covariates.
To test hypothesis 4, we examined whether worse RBANS total score were associated with high and persistent suicidal ideation. In support of hypothesis 4, we determined that worse RBANS total scores were associated with the ‘high and persistent suicidal ideation’ group when compared to the ‘rapidly decreasing suicidal ideation’ group. The β coefficient was −0.0351 ± 0.0166 (t=−2.11; df = 455; p = 0.035). The corresponding odds ratio was 0.965 indicating that participants with higher scores on the RBANS had an approximately 3% lower likelihood to be in the ‘high and persistent suicidal ideation’ group than in the ‘rapidly decreasing suicidal ideation’ group. The BIC value obtained with this model was −2979 (n = 455).
Discussion
In this study, we used latent class growth modeling to examine patterns of suicidal ideation over time in older depressed patients receiving acute protocolized treatment with an antidepressant medication. We identified four distinct trajectories: a ‘minimal suicidal ideation’ group, a ‘low suicidal ideation ‘group, a ‘rapidly decreasing suicidal ideation’ group and a ‘high and persistent suicidal ideation’ group. Two of these trajectories, i.e., the ‘rapidly decreasing suicidal ideation’ group and a ‘high and persistent suicidal ideation’ group’ were similar to the groups which were observed by Szanto et al (2007) in their sample of elderly depressed participants receiving antidepressant treatment over time. We determined that worse baseline scores on measures of inhibition/switching, attention, and global cognitive functioning predicted high and persistent (as opposed to rapidly decreasing) suicidal ideation supporting our a-priori hypotheses.
Our results are consistent with the study of Gujral et al. (2013) that found that older individuals who had made a recent suicide attempt or who had current suicidal ideation had significantly worse EXIT scores than those who were depressed and without suicidal ideation or non-psychiatric controls. In our study, worse Color Word ‘inhibition/switching’ scores were associated with a trajectory of ‘high and persistent suicidal ideation’ relative to those with ‘rapidly decreasing suicidal ideation’. However, two other measures of executive functioning were not significantly associated with this trajectory of ‘high and persistent suicidal ideation’. Gujral et al. (2013) also reported that older depressed individuals who had made a recent suicide attempt or who had current suicidal ideation performed worse on the Attention subscale of the Dementia Rating Scale relative to non-psychiatric controls. Similarly, in our analysis, worse RBANS attention subscale scores (and worse RBANS total scores) were associated with a trajectory of high and persistent suicidal ideation.
The effects we observed may likely be due to a general cognitive factor which was captured by the RBANS Total Score and the ‘inhibition/switching’ task. The latter is a combined executive function task, and therefore more sensitive than tasks that assess individual executive subfunctions in isolation. These findings may have prognostic implications since neuropsychologic dysfunction is known to be associated with suicidal behavior. This has been demonstrated with tests examining sustained attention, perseveration, response inhibition, set shifting and verbal fluency (Bartafi et al 1990; Keilp et al, 2001; Jollant et al, 2005; Westheide et al 2008; Cha et al 2010). Keilp et al (2001) determined that individuals who were high-lethality suicide attempters also had evidence of executive deficits. They specifically demonstrated that tasks requiring focused effort and organization were abnormal in high lethality attempters. It is also plausible that cognitive deficits undermine the ability to find alternative solutions in a crisis, leading one to prematurely focus on suicide as a seemingly straightforward solution. This notion is supported by evidence of poor problem-solving in suicide attempters and ideators, assessed both objectively and through self-report (Evans et al 1992; Gibbs et al 2009; McLeavey et al 1987; Rudd et al 1994; Schotte and Clum, 1987).
In conclusion, the present study successfully applies latent class growth modeling to identify different trajectories of suicidal ideation over time in older depressed individuals. To our knowledge, this is the first study that reports that worse executive dysfunction, attention, and global cognition are associated with high and persistent suicidal ideation in older depressed adults adequately treated with antidepressant medication. These findings need to be reproduced. Furthermore, individuals with subtle cognitive dysfunction may not be easy to detect on routine clinical examination. It may be worthwhile to consider screening for these high risk individuals using sensitive instruments.
Acknowledgments
Supported by NIH grant R01-MH083660, P30 MH090333, the UPMC Endowment in Geriatric Psychiatry, Taylor Family Institute for Innovative Psychiatric Research, National Center for Advancing Translational Sciences and the Campbell Family Mental Health Research Institute. Clinicaltrial.gov number NCT00892047.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders Text Revision. 4. American Psychiatric Press; Washington, DC: 2000. [Google Scholar]
- Andruff H, Carraro N, Thompson A, Gaudreau P, Louvet B. Latent Class Growth Modelling: A Tutorial. Tutorials in Quantitative Methods for Psychology. 2009;5:11–24. [Google Scholar]
- Barraclough BM. Suicide in the elderly: Recent Developments in Psychogeriatrics. Br J Psychiatry Spec Suppl. 1971;6:87–97. [Google Scholar]
- Bartfai A, Winborg IM, Nordstrom P, Asberg M. Suicidal behavior and cognitive flexibility: design and verbal fluency after attempted suicide. Suicide Life Threat Behav. 1990;20:254–266. [PubMed] [Google Scholar]
- Beck AT, Brown GK, Steer RA, Dahlsgaard KK, Grisham JR. Suicide ideation at its worst point: a predictor of eventual suicide in psychiatric outpatients. Suicide Life Threat Behav. 1999;29:1–9. [PubMed] [Google Scholar]
- Beck A, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicidal Ideation. Journal of Consulting and Clinical Psychology. 1979;47:343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- Brown GK, Beck AT, Steer RA, Grisham JR. Risk factors for suicide in psychiatric outpatients: a 20-year prospective study. J Consult Clin Psychol. 2000;68:371–7. [PubMed] [Google Scholar]
- Cha CB, Najmi S, Park JM, Nock MK. Attentional bias toward suicide-related stimuli predicts suicidal behavior. Journal of abnormal psychology. 2010;119:616–622. doi: 10.1037/a0019710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conwell Y, Van Orden K, Caine ED. Suicide in older adults. Psychiatr Clin North Am. 2011;34:451–68. doi: 10.1016/j.psc.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delis DC, Kaplan E, Kramer JH. Delis–Kaplan Executive Function System™ (D–KEFS™) San Antonio, TX: 2001. [Google Scholar]
- Dombrovski AY, Butters MA, Reynolds CF, 3rd, Houck PR, Clark L, Mazumdar S, Szanto K. Cognitive performance in suicidal depressed elderly: preliminary report. Am J Geriatr Psychiatry. 2008;16:109–15. doi: 10.1097/JGP.0b013e3180f6338d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duff K, Langbehn DR, Schoenberg MR, Moser DJ, Baade LE, Mold J, Scott JG, Adams RL. Examining the repeatable battery for the assessment of neuropsychological status: factor analytic studies in an elderly sample. Am J Geriatr Psychiatry. 2006;14:976–9. doi: 10.1097/01.JGP.0000229690.70011.cd. [DOI] [PubMed] [Google Scholar]
- Evans J, Williams JM, O’Loughlin S, Howells K. Autobiographical Memory and Problem-Solving Strategies of Parasuicide Patients. Psychological Medicine. 1992;22:399–405. doi: 10.1017/s0033291700030348. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Forkmann T, Brahler E, Auggel S, Glaesmer H. Prevalence of suicidal ideation and related risk factors in the German general population. Journal of Nervous and Mental Diseases. 2012;200:401–405. doi: 10.1097/NMD.0b013e31825322cf. [DOI] [PubMed] [Google Scholar]
- Gibbs LM, Dombrovski AY, Morse J, Siegle GJ, Houck PR, Szanto K. When the Solution Is Part of the Problem: Problem Solving in Elderly Suicide Attempters. International Journal of Geriatric Psychiatry. 2009;24:1396–1404. doi: 10.1002/gps.2276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gujral S, Dombrovski AY, Butters M, Clark L, Reynolds CF, 3rd, Szanto K. Impaired Executive Function in Contemplated and Attempted Suicide in Late Life. Am J Geriatr Psychiatry. 2013 Feb 6; doi: 10.1016/j.jagp.2013.01.025. pii: S1064-7481(13)00030-4. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jollant F, Bellivier F, Leboyer M, Astruc B, Torres S, Verdier R, Castelnau D, Malafosse A, Courtet P. Impaired decision making in suicide attempters. American Journal of Psychiatry. 2005;162:304–310. doi: 10.1176/appi.ajp.162.2.304. [DOI] [PubMed] [Google Scholar]
- Jones BL, Nagin DS, Roeder K. A SAS Procedure Based on Mixture Models for Estimating Developmental Trajectories. Sociological Methods and Research. 2001;29:374–393. [Google Scholar]
- Jones BL, Nagin DS. Advances in Group Based Trajectory Modelling and a SAS Procedure for Estimating Them. Sociologic Methods Research. 2007;35:542–571. [Google Scholar]
- Juurlink DN, Herrmann N, Szalai JP, Kopp A, Redelmeier DA. Medical illness and the risk of suicide in the elderly. Arch Intern Med. 2004;164:1179–1184. doi: 10.1001/archinte.164.11.1179. [DOI] [PubMed] [Google Scholar]
- Keilp JG, Sackeim HA, Brodsky BS, Oquendo MA, Mann JJ. Neuropsychological dysfunction in depressed suicide attempters. American Journal of Psychiatry. 2001;158:735–741. doi: 10.1176/appi.ajp.158.5.735. [DOI] [PubMed] [Google Scholar]
- King DA, Conwell Y, Cox C, Henderson RE, Denning DG, Caine ED. A neuropsychological comparison of depressed suicide attempters and nonattempters. J Neuropsychiatry Clin Neurosci. 2000;12:64–70. doi: 10.1176/jnp.12.1.64. [DOI] [PubMed] [Google Scholar]
- Lenze EJ, Mulsant BH, Blumberger DM, Karp JF, Newcomer JW, Anderson SJ, Dew MA, Butters MA, Stack JA, Begley AE, Reynolds CF., 3rd Efficacy, safety, and tolerability of augmentation pharmacotherapy with aripiprazole for treatment-resistant depression in late life: a randomised, double-blind, placebo-controlled trial. Lancet. 2015 Sep 24; doi: 10.1016/S0140-6736(15)00308-6. pii: S0140-6736(15)00308-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lezak MD, Howieson DB, Bigler ED, Tranel D. Neuropsychological Assessment. 5. Oxford University Press; Oxford: 2012. [Google Scholar]
- McLeavey BC, Daly RJ, Murray CM, O’Riordan J, Taylor M. Interpersonal Problem-Solving Deficits in Self-Poisoning Patients. Suicide Life Threat Behav. 1987;17:33–49. doi: 10.1111/j.1943-278x.1987.tb00060.x. [DOI] [PubMed] [Google Scholar]
- Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. British Journal of Psychiatry. 1979;134:382–9. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- Morrell SL, Taylor RJ, Kerr CB. Jobless. Unemployment and young people’s health. Med J Aust. 1998;168:236–240. doi: 10.5694/j.1326-5377.1998.tb140139.x. [DOI] [PubMed] [Google Scholar]
- Nagin D. Group-based modeling of development. Cambridge: Harvard University Press; 2005. [Google Scholar]
- Randolph C, Tierney MC, Mohr E, Chase TN. The Repeatable Battery for the Assessment of Neuropsychological Status (RBANS): Preliminary clinical validity. The Journal of Clinical and Experimental Neuropsychology. 1998;20:310–319. doi: 10.1076/jcen.20.3.310.823. [DOI] [PubMed] [Google Scholar]
- Royall DR, Mahurin RK, Gray KF. Bedside assessment of executive cognitive impairment: the executive interview. J Am Geriatric Society. 1992;40:1221–1226. doi: 10.1111/j.1532-5415.1992.tb03646.x. [DOI] [PubMed] [Google Scholar]
- Rudd DM, Rajab MH, Dahm PF. Problem-Solving Appraisal in Suicide Ideators and Attempters. American Journal of Orthopsychiatry. 1994;64:136–49. doi: 10.1037/h0079492. [DOI] [PubMed] [Google Scholar]
- Sirey JA, Bruce ML, Carpenter M, Booker D, Reid MC, Newell KA, Alexopoulos GS. Depressive symptoms and suicidal ideation among older adults receiving home delivered meals. Int J Geriatr Psychiatry. 2008;23:1306–11. doi: 10.1002/gps.2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schotte DE, Clum GA. Problem-Solving Skills in Suicidal Psychiatric Patients. Journal of Consulting and Clinical Psychology. 1987;55:49–54. doi: 10.1037//0022-006x.55.1.49. [DOI] [PubMed] [Google Scholar]
- Schwarz GE. Estimating the dimensions of a model. Annals of Statistics. 1978;6:461–464. [Google Scholar]
- Szanto K, Mulsant BH, Houck P, Dew MA, Reynolds CF., 3rd Occurrence and course of suicidality during short-term treatment of late-life depression. Arch Gen Psychiatry. 2003;60:610–7. doi: 10.1001/archpsyc.60.6.610. [DOI] [PubMed] [Google Scholar]
- Szanto K, Mulsant BH, Houck P, Dew MA, Dombrovski A, Pollock BG, Reynolds CF., 3rd Emergence, persistence, and resolution of suicidal ideation during treatment of depression in old age. Journal of Affective Disorders. 2007;98:153–161. doi: 10.1016/j.jad.2006.07.015. [DOI] [PubMed] [Google Scholar]
- Welsh-Bohmer KA, Attix DK. Neuropsychological Assessment of Late-Life Cognitive Disorders. In: Steffins DC, Blazer DG, Thakus ME, editors. The American Psychiatric Publishing Textbook of Geriatric Psychiatry. American Psychiatric Publishing; Washington DC: 2015. [Google Scholar]
- Westheide J, Quednow BB, Kuhn KU, Hoppe C, Cooper-Mahkorn D, Hawellek B, Eichler P, Maier W, Wagner M. Executive performance of depressed suicide attempters: the role of suicidal ideation. Eur Arch Psychiatry Clin Neurosci. 2008 doi: 10.1007/s00406-008-0811-1. [DOI] [PubMed] [Google Scholar]