Abstract
Idiopathic adhesive capsulitis, or primary frozen shoulder syndrome, is a fairly common orthopaedic problem characterized by shoulder pain and loss of motion. In most cases, conservative treatment (6-month physical therapy program and intra-articular steroid injections) improves symptoms and restores shoulder motion. In refractory cases, arthroscopic capsular release is indicated. This surgical procedure carries several advantages over other treatment modalities. First, it provides precise and controlled release of the capsule and ligaments, reducing the risk of traumatic complications observed after forceful shoulder manipulation. Second, release of the capsule and the involved structures with a radiofrequency device delays healing, which prevents adhesion formation. Third, the technique is straightforward, and an oral postoperative steroid program decreases pain and allows for a pleasant early rehabilitation program. Fourth, the procedure is performed with the patient fully awake under an interscalene block, which boosts the patient's confidence and adherence to the physical therapy protocol. In patients with refractory primary frozen shoulder syndrome, arthroscopic capsular release emerges as a suitable option that leads to a faster and long-lasting recovery.
Idiopathic adhesive capsulitis, or primary frozen shoulder syndrome (PFSS), is characterized by shoulder pain and loss of motion.1, 2 Even though its precise cause remains unknown, certain factors increase the risk of this disorder developing, including female gender, diabetes mellitus, hyperlipidemia, thyroid disease, genetic predisposition, and Caucasian ethnicity.3 Classically, there are 3 sequential stages in the disease: freezing, frozen, and thawing. Given its self-limited behavior, recovery usually happens after 6 to 12 months. However, many patients diagnosed with PFSS report a 2-year (or even longer) history of shoulder pain or stiffness (or both).
In patients with PFSS, several non-surgical measures (physical therapy, anti-inflammatory medication, and corticoid injections) are usually effective for pain control.4, 5 After failing conservative measures, patients with moderate to severe pain require pain management, while arthroscopic capsular release (ACR)6 and manipulation under anesthesia (MUA)7, 8 are indicated in the setting of chronic shoulder stiffness. Although the long-term improvement in joint motion is similar with both surgical techniques, performing MUA alone can lead to humeral fracture.9, 10
Studies have shown that ACR provides complete and long-lasting improvement of shoulder pain and function, faster than any other treatment modality.10, 11 Indications to proceed with ACR and key points are summarized in Tables 1 and 2, respectively.
Table 1.
Indications for Arthroscopic Capsular Release
| Failure of well-performed, 6-mo rehabilitation program∗ |
| Failure after ≥3 steroid injections within 6-mo interval∗ |
| Failure of less invasive treatments such as joint distension or MUA∗ |
| Severe PFSS in patients with diabetes mellitus in whom steroid treatment is contraindicated |
| Patients with predilection for expedited recovery |
MUA, manipulation under anesthesia; PFSS, primary frozen shoulder syndrome.
Failure is defined as a pain score of over 5 of 10 on a visual analog scale and range of motion reduced to less than 50% of normal motion.
Table 2.
Key Points of Surgical Technique
| 1. Regional anesthesia is used. |
| 2. Preoperative and postoperative ROM assessment is performed with a conscious patient |
| 3. Adequate release of the rotator interval is performed, focusing on the coracohumeral ligament as the most important target. |
| 4. Care is required regarding the axillary nerve located underneath the capsule.18 The cutting device should be kept close to the labrum. Gentle mobilization in abduction expands the capsulotomy and makes this step safer. |
| 5. Postoperatively, oral cortisone medication is administered, and the postoperative rehabilitation program is started immediately. |
ROM, range of motion.
Surgical Technique
Surgical Anatomy and Preoperative Planning
The anterior shoulder girdle has four anatomic layers. The first two layers are made by the capsule, the glenohumeral ligaments, and the subscapularis tendon, whereas the coracohumeral ligament (CHL), coracoid, and coracoacromial ligament form the third and fourth layers. (Fig 1). All these layers can trigger pain, while CHL is primarily responsible for shoulder stiffness. The CHL goes from the coracoid base to the upper part of the bicipital groove (Fig 1) and represents an important target during the surgical procedure.13, 14
Fig 1.
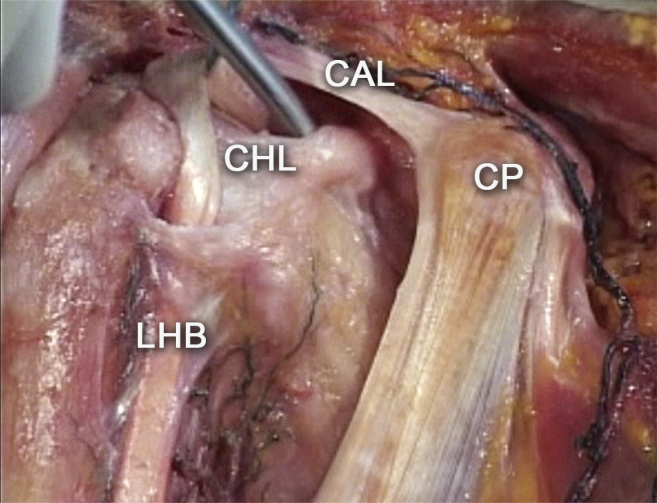
Anterior view of a dissected cadaveric specimen showing the rotator interval anatomy in a right shoulder. The coracohumeral ligament (CHL) runs from the coracoid base up to the proximal bicipital groove and constitutes one of the main structures involved in primary frozen shoulder syndrome. (CAL, coracoacromial ligament; CP, coracoid process; LHB, long head of biceps tendon.)
Reprinted with permission.12
Up until now, it is unclear the degree of surgical release required during ACR. We typically target the CHL and rotator interval, but also endorse freeing additional structures such as the inferior and posterior capsules in order to optimize shoulder elevation, internal and external rotations.15, 16, 17 Preoperative evaluation of shoulder motion should dictate the degree of capsular release necessary to obtain a satisfactory result. In addition, documentation of baseline (Video 1) and postoperative range of motion is essential to motivate patients at the beginning of rehabilitation.
Patient Positioning and Arthroscopic Examination
With the patient in the beach-chair position and under inter-scalene block, the patient's arm remains free for manipulation and the assessment of range of motion during the procedure. Diagnostic arthroscopy enables identification of synchronous injuries that may preclude ACR. Intraoperative evaluation usually shows reddish synovial and capsular tissue at the glenohumeral ligaments, the inferior part of the rotator cuff, and the insertion of the biceps tendon (Fig 2). Classically, there is obliteration of the triangle made by the biceps and subscapularis tendons. This obliteration is due to proliferative synovitis.
Fig 2.
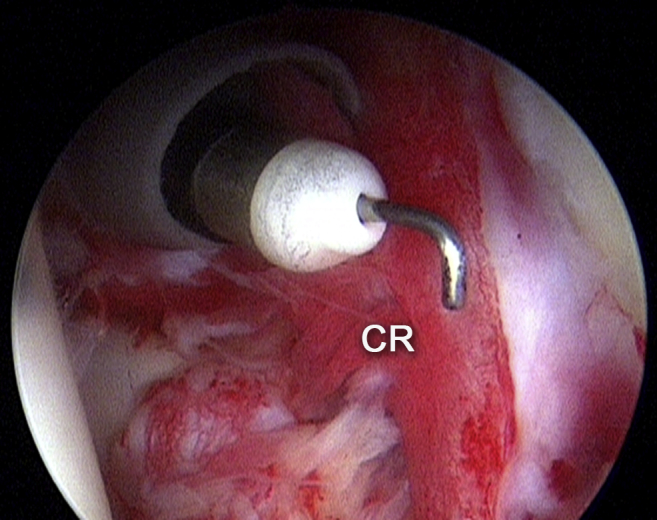
Arthroscopic view from the posterior portal in a right shoulder showing reddish capsular tissue (CR). An L-tipped radiofrequency device is used to perform rotator interval release and serial capsulotomies.
Reprinted with permission.12
Portals and Technique
We introduce the scope at the posterior portal and then place an antero-lateral portal utilizing an outside-in technique anterior to the biceps tendon. We place the anterior portal laterally to create an optimal angle and obtain access for the release of the rotator interval. At this stage, using a radiofrequency device specially designed for coagulation, cutting, and tissue vaporization (VAPR III; DePuy Mitek, Raynham, MA), we release the rotator interval and perform anterior and posterior capsulotomies. Rotator interval release entails full dissection of the CHL (Figs 3 and 4), whereas freeing the anterior structures allows for complete recovery of the shoulder's external rotation.
Fig 3.
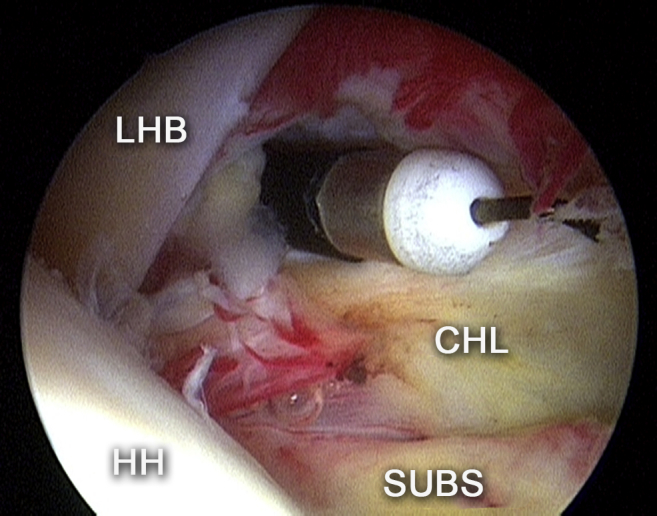
Arthroscopic view from the posterior portal in a right shoulder showing the radiofrequency wand in place for coracohumeral ligament (CHL) excision. After this surgical step, almost full external rotation is recovered. (HH, humeral head; LHB; long head of biceps; SUBS, subscapularis.)
Reprinted with permission.12
Using a switching stick helps position the scope at the anterior portal, while a radiofrequency device is used to free the posterior capsule and the posterior band of the inferior gleno-humeral ligament. Careful shoulder manipulation is often required to gain full forward flexion and abduction. These maneuvers help to release the inferior capsule and avoid the risk of using the radiofrequency device at the glenoid 6 o'clock area.
Awareness of the precise location of the axillary nerve is essential during the procedure. At the 6 o'clock glenoid position, the nerve is found laterally, adjacent to the humerus, roughly 12.5 mm from the glenoid edge and 2.5-4 mm from the capsule.18 Inferior capsule release is recommended near the labrum to prevent nerve damage.
Then, we release adhesions at the subacromial space and resect the lateral bursae. In general, a formal acromioplasty is not needed in these cases. Table 2 details key points for the appropriate surgical technique.
The patient normally gains full range of motion with almost 180° of pooled external and internal rotations immediately after the procedure, obtaining complete recovery of abduction and forward flexion. Demonstration of these results to the patient generates great reinforcement (Video 1).
A supervised rehabilitation program should start on the same day as surgery with active range of motion and mobilization. During the first month after surgery, the patient should receive oral prednisolone, 40 mg once a day, tapering 10 mg per week.
Discussion
ACR includes a few steps (block anesthesia, capsular releases, ligament splitting, resection of adhesions, and shoulder manipulation) followed by a postprocedural oral cortisone plan and a supervised rehabilitation program.1, 2 This technique plays a pivotal role in patients with PFSS and recalcitrant symptoms or in patients with PFSS who wish for an expedited recovery.
Although MUA improves shoulder elevation and abduction, rotation remains limited because of surgeons' concerns about forceful rotation maneuvers. Bone fractures, cuff tears, labral detachments, and SLAP lesions have been described after MUA alone, affecting MUA's effectiveness.9, 10 Given this risk, orthopaedic surgeons currently favor ACR. Table 3 lists the advantages of ACR over MUA.
Table 3.
Advantages of ACR Over Manipulation Under Anesthesia
| ACR allows more precision and control during capsular release. |
| ACR is a safer technique, preventing bone fractures and labral or rotator cuff injuries. |
| ACR reduces soft-tissue trauma and intra-articular bleeding, preventing further adhesions and delaying capsular healing. These issues allow less painful motion recovery. |
ACR, arthroscopic capsular release.
ACR bears several advantages that deserve mention. First, it releases shoulder structures in a precise and controlled fashion, providing a complete and predictable recovery of shoulder motion.11 This surgical procedure prevents not only adhesion recurrence but also the development of traumatic complications observed after forceful manipulation. Second, it constitutes a simple and short procedure that is very well tolerated by an awake patient. Postoperatively, the immediate improvements in symptoms and motion are readily perceived by the patient, which reinforces the patient's commitment to the rehabilitation process. Third, long-term (mean, 7 years; range, 4 to 13 years) outcomes after ACR are encouraging.
As previously mentioned, the optimal degree of release required during this surgical procedure is currently unknown. Some investigators propose freeing the subscapularis tendon, the inferior and posterior capsule and the global capsule in order to optimize shoulder elevation and rotation.13, 14 Possibly, assessment of motion loss prior to the procedure can guide the amount of capsular release.15
Our group typically defers surgical treatment of concomitant shoulder injuries such as cuff repair or biceps tenodesis until recovery of shoulder motion and relief of symptoms. The presence of diabetes mellitus may prevent the administration of steroid injections. ACR is usually the best alternative for the patients; however, surgical outcome is inferior to in non-diabetic patients.16, 17 The latter is likely due to glycemic injury at the microvascular level.
The most appropriate timing to indicate ACR is also controversial. While surgeons typically wait for failure of a 6-12 months conservative course, patients' wishes are forcing surgeons for an earlier surgical decision.
Fig 4.
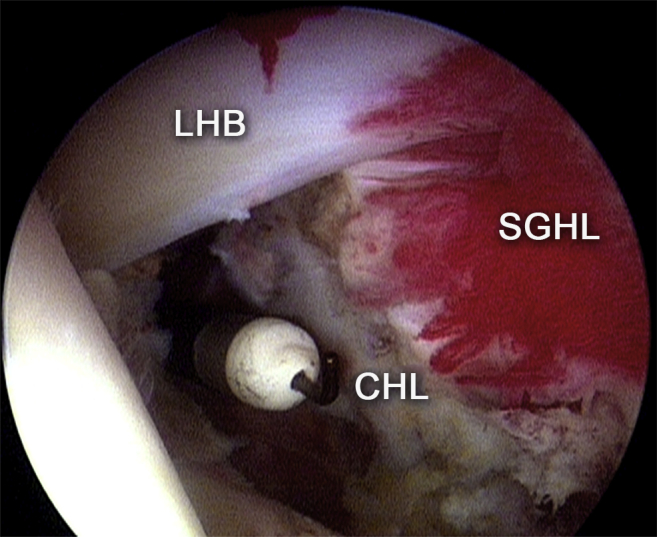
Arthroscopic view from the posterior portal in a right shoulder in which the superior glenohumeral ligament (SGHL) and coracohumeral ligament (CHL) have already been released by the radiofrequency device. The loosened ligament is shown after excision. The burned edges of the ligament preclude adhesion formation and lead to a delay in capsular healing, allowing for a tolerable rehabilitation program. (LHB, long head of biceps.)
Reprinted with permission.12
Footnotes
The author reports the following potential conflict of interest or source of funding: G.A. receives support from Mitek Sports Medicine and Storz.
Supplementary Data
Arthroscopic capsular release in the left shoulder of a patient with primary frozen shoulder syndrome. The patient is in the beach-chair position under regional anesthesia alone. The involved anatomic structures are shown. A precise capsular release with a radiofrequency device is performed. Tips and tricks for achieving safe, full motion recovery are described.
References
- 1.Zuckerman J.D., Rokito A. Frozen shoulder: A consensus definition. J Shoulder Elbow Surg. 2011;20:322–325. doi: 10.1016/j.jse.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 2.Nagy M.T., Macfarlane R.J., Khan Y., Waseem M. The frozen shoulder: Myths and realities. Open Orthop J. 2013;7:352–355. doi: 10.2174/1874325001307010352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang K., Ho V., Hunter-Smith D.J., Beh P.S., Smith K.M., Weber A.B. Risk factors in idiopathic adhesive capsulitis: A case control study. J Shoulder Elbow Surg. 2013;22:e24–e29. doi: 10.1016/j.jse.2012.10.049. [DOI] [PubMed] [Google Scholar]
- 4.Lorbach O., Kieb M., Scherf C., Seil R., Kohn D., Pape D. Good results after fluoroscopic-guided intra-articular injections in the treatment of adhesive capsulitis of the shoulder. Knee Surg Sports Traumatol Arthrosc. 2010;18:1435–1441. doi: 10.1007/s00167-009-1030-7. [DOI] [PubMed] [Google Scholar]
- 5.Lorbach O., Anagnostakos K., Scherf C., Seil R., Kohn D., Pape D. Nonoperative management of adhesive capsulitis of the shoulder: Oral cortisone application versus intra-articular cortisone injections. J Shoulder Elbow Surg. 2010;19:172–179. doi: 10.1016/j.jse.2009.06.013. [DOI] [PubMed] [Google Scholar]
- 6.Nicholson G.P. Arthroscopic capsular release for stiff shoulders: Effect of etiology on outcomes. Arthroscopy. 2003;19:40–49. doi: 10.1053/jars.2003.50010. [DOI] [PubMed] [Google Scholar]
- 7.Wang J.P., Huang T.F., Ma H.L., Hung S.C., Chen T.H., Liu C.L. Manipulation under anaesthesia for frozen shoulder in patients with and without non-insulin dependent diabetes mellitus. Int Orthop. 2010;34:1227–1232. doi: 10.1007/s00264-010-0968-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vastamaki H., Vastamaki M. Motion and pain relief remain 23 years after manipulation under anesthesia for frozen shoulder. Clin Orthop Relat Res. 2013;471:1245–1250. doi: 10.1007/s11999-012-2542-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Menendez M., Ishihara A., Weisbrode S., Bertone A. Radiofrequency energy on cortical bone and soft tissue: A pilot study. Clin Orthop Relat Res. 2010;468:1157–1164. doi: 10.1007/s11999-009-1150-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cinar M., Akpinar S., Derincek A., Circi E., Uysal M. Comparison of arthroscopic capsular release in diabetic and idiopathic frozen shoulder patients. Arch Orthop Trauma Surg. 2010;130:401–406. doi: 10.1007/s00402-009-0900-2. [DOI] [PubMed] [Google Scholar]
- 11.Le Lievre H.M., Murrell G.A. Long-term outcomes after arthroscopic capsular release for idiopathic adhesive capsulitis. J Bone Joint Surg Am. 2012;94:1208–1216. doi: 10.2106/JBJS.J.00952. [DOI] [PubMed] [Google Scholar]
- 12.Itoi E., Arce G., Bain G.I., editors. Shoulder stiffness: Current concepts and concerns. Springer-Verlag; Berlin/Heidelberg: 2015. [DOI] [PubMed] [Google Scholar]
- 13.Ozaki J., Nakagawa Y., Sakurai G., Tamai S. Recalcitrant chronic adhesive capsulitis of the shoulder. Role of contracture of the coracohumeral ligament and rotator interval in pathogenesis and treatment. J Bone Joint Surg Am. 1989;71:1511–1515. [PubMed] [Google Scholar]
- 14.Harryman D.T., II, Sidles J.A., Harris S.L., Matsen F.A., III The role of the rotator interval capsule in passive motion and stability of the shoulder. J Bone Joint Surg Am. 1992;74:53–66. [PubMed] [Google Scholar]
- 15.Pearsall A.W., IV, Holovacs T.F., Speer K.P. The intra-articular component of the subscapularis tendon: Anatomic and histological correlation in reference to surgical release in patients with frozen-shoulder syndrome. Arthroscopy. 2000;16:236–242. doi: 10.1016/s0749-8063(00)90046-x. [DOI] [PubMed] [Google Scholar]
- 16.Omari A., Bunker T.D. Open surgical release for frozen shoulder: Surgical findings and results of the release. J Shoulder Elbow Surg. 2001;10:353–357. doi: 10.1067/mse.2001.115986. [DOI] [PubMed] [Google Scholar]
- 17.Massoud S.N., Pearse E.O., Levy O., Copeland S.A. Operative management of the frozen shoulder in patients with diabetes. J Shoulder Elbow Surg. 2002;11:609–613. doi: 10.1067/mse.2002.127301. [DOI] [PubMed] [Google Scholar]
- 18.Price M.R., Tillett E.D., Acland R.D., Nettleton G.S. Determining the relationship of the axillary nerve to the shoulder joint capsule from an arthroscopic perspective. J Bone Joint Surg Am. 2004;86:2135–2142. doi: 10.2106/00004623-200410000-00003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic capsular release in the left shoulder of a patient with primary frozen shoulder syndrome. The patient is in the beach-chair position under regional anesthesia alone. The involved anatomic structures are shown. A precise capsular release with a radiofrequency device is performed. Tips and tricks for achieving safe, full motion recovery are described.


