Telemedicine (TM) is increasingly becoming part of the practice of medicine rather than a special practice that is separate from the normal practice of medicine. Health care planners are now seeking to identify technologies and settings where this practice can be best applied to improve outcomes, save time, and/or save money.
Definitions
TM is defined by the American Telemedicine Association as the use of medical information exchanged from 1 site to another via electronic communications to improve a patient’s clinical health status.1 TM incorporates multiple types of communication services such as 2-way video, email, texting, smartphones, tablets, wireless monitors, decision support tools, and other forms of telecommunication technologies.
The definition of mHealth is the use of mobile digital communication devices for health services and information.2 Wearable or portable sensors, smartphones, tablets, and other mobile wireless devices can deliver mHealth. Most mHealth systems incorporate a method of data storage utilizing remote distributed servers, which are also known as the cloud.
How Telemedicine Is Applied to Diabetes Care
Diabetes is well suited for being treated with TM. This disease has better outcomes when monitoring occurs and TM allows monitored data to be stored and analyzed. Many types of inputs affecting diabetes can be digitalized including blood glucose (BG) levels, time spent exercising, steps walked, calories ingested, medication doses administered, blood pressure, and weight. Patterns can be identified by software that can lead to specific treatment recommendations. Many decisions for diabetes management can be supported by or made in real time with algorithms. Finally the medical literature supports the value of using TM in diabetes management. The steps for how blood glucose data and other physiologic data can be measured, transmitted, aggregated, analyzed, stored, and then either presented as actionable information to a patient or else delivered to a treatment algorithm, where a specific action is advised, are presented in Figure 1. The result of generating actionable information is either to provide information that a patient can use to assist them in making a decision or else to provide a specific algorithm-determined recommendation that specifies a particular treatment. The decision results in data-driven action and hopefully better outcomes.
Figure 1.
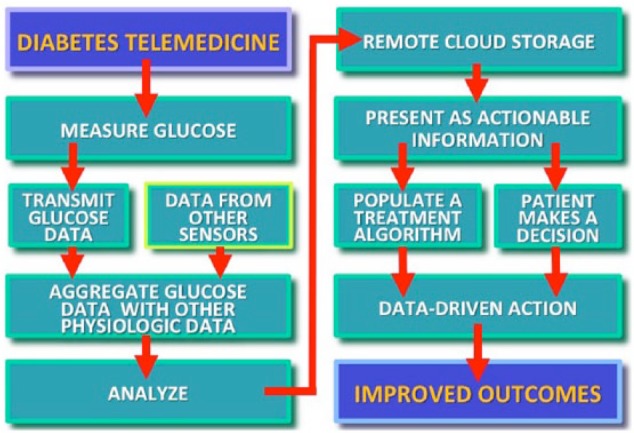
How diabetes telemedicine results in data-driven action and improved outcomes.
Sensor-Based TM
TM systems can be divided into 2 main categories: (1) systems that incorporate automatically uploaded digital sensor data and then provide descriptions, analysis, and treatment recommendations based on the data;3 and (2) systems that do not utilize sensors and facilitate communication between a patient and a health care professional (HCP) through intentionally uploaded messages or videos and provide responses back to the patient from the HCP.4
When the first type of TM system (digital sensor-based) uses a wearable device or a mobile carried device, then this form of TM is also known as mHealth. Mobile digital sensor TM systems almost always automatically upload their data, but a few mHealth systems ca be found where a patient must manually (nonautomatically) enter digital data for uploading to the cloud. Such mobile systems are rarely used because most patients find manual data entry tedious and generally refuse to use these systems. If the first type of (sensor-based) system TM (with a digital sensor) is part of an immobile system, such as a hospital-based hard-wired system or an immobile home-based sensor system, then such a system is known as a sensor-based TM system but not an mHealth system. When the second type of system (without a digital sensor) uses analog or digital data entry, the data entry can be either automatic or volitional (nonautomatic). The second (nonsensor) type of TM system is a more traditional type of TM because it has been in use even before mobile sensors became popular. The traditional non-sensor-based forms of TM mainly utilize phone, email, and video communications from the patient and almost all of these communication methods require specific volitional (nonautomatic) input. The data from mHealth TM systems (and immobile sensor-based systems) tends to be digital and amenable to automated analysis by software. However, the data that is extracted from traditional nonsensor TM systems tends to be analog and is generally not suitable for automated analysis by software.
Non-Sensor-Based TM
In the past few years non-sensor-based TM systems have evolved and some of them no longer use analog forms of communication (such as telephone or video) and instead use software applications that reside on mobile devices (smartphones and tablets) and provide digital communication. These non-sensor-based mobile applications are known as apps or mobile apps. Meanwhile the various types of software for analyzing sensor-based data automatically uploaded data (mHealth data) are increasinglyf residing not on fixed location computers (where they are known as programs) but on mobile devices where they are also known as mobile applications or apps. mHealth systems must be mobile and deliver digital data. These systems almost always embody automatic uploading, but volitional uploading of sensor information from a mobile system is still within the definition of mHealth. TM systems which deliver analog information, whether automatically or volitionally uploaded, are considered to be non-sensor-based TM systems and the lack of digital information relegates them to not being considered as mHealth systems. See Table 1 for a classification of TM systems according to whether they are fixed or mobile, and contain digital or analog data. The uploading method (automatic or nonautomatic) does not affect the classification of a TM system according to this classification.
Table 1.
Classification of Telemedicine Systems According to Whether They Are Fixed or Mobile and Whether They Accommodate Digital Sensor Data or Analog Data.
| Digital sensor data | Analog data | |
|---|---|---|
| Fixed system | Sensor-based TM | Non-sensor-based TM |
| Mobile system | mHealth and sensor-based TM | Non-sensor-based TM |
Further Classification of Telemedicine
There are several additional criteria for categorizing TM interventions in addition to distinguishing between automatically uploaded digital sensor data versus volitionally uploaded nonsensor data. The term TM can apply to acute or chronic diseases, synchronous versus asynchronous care, data that is automatically versus volitionally uploaded, use of mobile wearable or portable sensors versus fixed immobile home-based data collection systems, communication by email, text, or video, and can be based on proprietary versus nonproprietary sensor information.
Outcomes of TM Interventions
The medical literature can be difficult to interpret for the effects of a particular type of TM program because there are so many categories of TM to incorporate into an intervention and to then analyze. The medical literature tends to contains sweeping statements about benefits or deficiencies of TM that incorporate different types of TM in the same statement. Two recent meta analyses of the outcomes of TM were positive. In 2014 Zhai and colleagues reported a meta analysis of 35 randomized controlled trials of TM for type 2 diabetes. The type of portal for physician contact included video in 19 studies, phone in 12 studies, and email in 4 studies. They reported that TM, compared to control therapy, resulted in a clinically and statistically significant difference in A1C of –0.37% (P < .001).5 In 2015 Flodgren and colleagues performed a review of randomized controlled trials of TM outcomes diseases and of 93 studies that they identified, 21 we for diabetes. Among the diabetes TM studies, they found lower A1C levels in subjects allocated to TM than in controls with a difference of –0.31% (P < .00001) at a median of 9 months follow-up with a high certainty of evidence.6 In 2013 Klonoff reviewed the outcomes from mobile health programs for diabetes and found that the quality of many studies was poor. The results showed the potential for improved A1C, but evidence for the effectiveness of mHealth is weak.2
Seven main features must be specified to clearly classify a TM system: (1) the product, (2) the technology, (3) the user or customer, (4) the data, (5) the delivery, (6) the validation, and (7) the economic model for payment.7 To understand whether a specific type of TM program has demonstrated beneficial outcomes in the literature, then it will be necessary in the future to classify each TM intervention according to its specific features within these 7 areas. In this way, realistic comparisons can be made between different types of systems and within like systems.
Barriers and Solutions
There are many barriers to widespread adoption of TM. I have listed the top 12 potential barriers and solutions to these barriers in Table 2. The solutions often require mobilization of 1 or more stakeholders to modify an element of a program or apply pressure to achieve a breakthrough. Stakeholders in the success of TM for diabetes include payers, HCPs, sensor manufacturers, software developers, data transmission companies, payers, government regulators. Not all these barriers block TM in every situation where TM might be practiced. What determines the success or failure of a diabetes TM program is often the choices of technology, patients, and payment.
Table 2.
The Top 12 Barriers and Solutions to Implement Telemedicine.
| Barrier | Solution | |
|---|---|---|
| 1 | Reimbursement with FFS | Legislation or switch to ACO |
| 2 | Overutilization with ACO | Control use or switch to FFS |
| 3 | EHR integration | Users/workflow/data |
| 4 | Integrate with other disease mgt systems | Multidiscipline physiology (IOT) |
| 5 | Privacy & security | Cyberstandards/HIPPA |
| 6 | Securing support from MDs | Decreased workload |
| 7 | Perceived low quality of care | Outcomes data |
| 8 | Consumer trust & acceptance | MD satisfaction |
| 9 | Need for data entry and training | Human factors |
| 10 | Better internet coverage | Ongoing trend |
| 11 | Institutional support & funding | Industry collaboration |
| 12 | Multiple state licensing laws | Lobbying by payers/pts |
Future Trends
According to a November 2015 report in the National Law Review, 5 trends will result in greater adoption of TM in 2016. These trends include (1) expanding reimbursement and payments from various payers, (2) increased international arrangements for delivery of Western care to overseas patients through TM systems, (3) greater facilitation of TM access by state governments for licensing and interstate care, (4) proliferation of TM clinics at retail facilities and employee health centers, and (5) greater adoption of TM by accountable care organizations (ACOs) to save money for the plan and time for covered patients.8
Conclusions
TM is part of the new digital age that is transforming the world. The digital age is bringing instant telecommunication; novel wearable sensors; software-based treatment algorithms that utilize physiological and nonphysiological data streams; and precision medicine treatments that based on input from genetic data and multiple other sources to define previously unrecognized relationships. TM is well suited for treating diabetes. This disease and its related generate many types of numbers and require frequent treatment adjustments to achieve physiological homeostasis. TM is a natural tool for delivering care in real time when needed and in adequate time otherwise to improve outcomes. In the next decade health care researchers will be searching for the settings where specific types of TM have the most to offer both clinically and economically for diabetes and other diseases. These settings will be identified and TM will become increasingly adopted.
Footnotes
Abbreviations: ACO, accountable care organization; BG, blood glucose; HCP, health care professional; TM, telemedicine.
Declaration of Conflicting Interests: The author declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Consultant for Bayer, Insuline, Lifecare, Sanofi, Voluntis.
Funding: The author received no financial support for the research, authorship, and/or publication of this article.
References
- 1. American Telemedicine Association. What is telemedicine? Available at: http://www.americantelemed.org/about-telemedicine/what-is-telemedicine#.Vk6tD3arTIU. Accessed November 23, 2015.
- 2. Klonoff DC. The current status of mHealth for diabetes: will it be the next big thing? J Diabetes Sci Technol. 2013;7(3):749-758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dvorack K. Sensor-based remote monitoring system keeps elderly out of hospital. August 28, 2015. Available at: http://www.fiercehealthit.com/story/sensor-based-remote-monitoring-system-keeps-elderly-out-hospital/2015-08-28. Accessed November 23, 2015.
- 4. Landro L. Interactive video helps patients get access to medical specialists. May 12, 2014. Available at: http://www.wsj.com/articles/SB10001424052702304081804579557770525373400. Accessed November 23, 2015.
- 5. Zhai YK, Zhu WJ, Cai YL, Sun DX, Zhao J. Clinical- and cost-effectiveness of telemedicine in type 2 diabetes mellitus: a systematic review and meta-analysis. Medicine (Baltimore). 2014;93(28):e312. doi: 10.1097/MD.0000000000000312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Flodgren G, Rachas A, Farmer AJ, Inzitari M, Shepperd S. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2015;9:CD002098. doi: 10.1002/14651858.CD002098.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Steinberg D, Horwitz G, Zohar D. Building a business model in digital medicine. Nat Biotechnol. 2015;33:910-920. [DOI] [PubMed] [Google Scholar]
- 8. Lacktman NM. Five telemedicine trends transforming health care in 2016. November 16, 2015. Available at: http://www.natlawreview.com/article/five-telemedicine-trends-transforming-health-care-2016. Accessed November 23, 2015.


