Abstract
Massive irreparable rotator cuff tears have been troublesome entities to treat, especially in younger patients. Few good options exist, leaving most patients in recent years receiving a reverse total shoulder arthroplasty. Reverse shoulder arthroplasty carries serious risks, a limited lifespan, and no other viable options should it fail. Recent biomechanical studies have shown that the superior capsule is critical to containing the glenohumeral joint reduced, allowing the larger muscles like the deltoid and pectoralis major to function properly. The superior capsular reconstruction is an anatomic reconstruction of the superior capsule to restore the normal restraint to superior translation that occurs with a deficient rotator cuff. The technique described in this article is an arthroscopic reconstruction of the superior capsule with dermal allograft.
The treatment of massive irreparable rotator cuff tears presents a significant challenge to health care providers. Options range from nonoperative care to operative debridement and biceps tenotomy,1, 2 partial repair of the rotator cuff,3, 4, 5, 6, 7 bridging patch grafts,7 muscle transfers,8, 9, 10, 11 and reverse total shoulder arthroplasty. However, the results of such treatments are often mixed with a significant risk of complications. The superior capsular reconstruction (SCR) was originally described as an alternative to the aforementioned procedures.11 In the original description, autograft fascia lata was harvested from the patient's thigh and was secured from the glenoid to the greater tuberosity. This restored the normal superior restraint to proximal migration of the humeral head and in several cases resulted in reversal of pseudoparalysis.12 The original biomechanical and preliminary clinical results are quite promising. The technique described in this article is an arthroscopic reconstruction of the superior capsule with dermal allograft.
Operative Technique
The indications for an arthroscopic SCR are a massive irreparable supraspinatus and/or infraspinatus tear, minimal to no arthritis, and a fully functioning deltoid muscle (Table 1). The procedure can be performed either in an open manner or arthroscopically (beach-chair or lateral decubitus position). In this description, the patient is positioned in the beach-chair position. The arm is maintained comfortably at the patient's side (“neutral abduction”) and in neutral rotation. The glenohumeral joint is thoroughly evaluated with a 30° arthroscope (Arthrex, Naples, FL) from both the posterior and lateral viewing portals (Video 1). An attempt is made to repair as much of the rotator cuff as possible (e.g., subscapularis and infraspinatus) to aid in balancing the normal force couples of the shoulder. If the biceps is either torn or unstable, a biceps tenodesis or tenotomy is performed. If at least the supraspinatus still cannot be repaired, the superior glenoid and greater tuberosity bone beds should be debrided and prepared for reconstruction, using a Torpedo shaver and PowerRasp (Arthrex). The superior labrum is left intact because it is an important stabilizer to the glenohumeral joint.13, 14 We prepare the superior glenoid just medial to the superior labrum because this is the normal attachment of the superior capsule.
Table 1.
Indications and Contraindications to Superior Capsular Reconstruction
|
|
A lateral portal is created, and a 10-mm PassPort cannula (Arthrex) is placed into the portal. The length is determined based on the size of the patient and tissue depth and is usually 4 cm. With the arthroscope placed through the lateral portal, a Neviaser portal is created. A 3.0-mm BioComposite SutureTak (Arthrex) is placed percutaneously through this portal medial to the labrum and posteriorly. An anterosuperior portal is created, just anterior to the acromioclavicular joint. A second 3.0-mm BioComposite SutureTak is placed percutaneously through this portal medial to the labrum and anteriorly (Video 1).
Through a superolateral portal, two 4.75-mm BioComposite Vented SwiveLock anchors (Arthrex) with attached swedged FiberTapes (Arthrex) are placed into the medial row at the greater tuberosity both anteriorly and posteriorly (Fig 1, Video 1). By use of the attached No. 2 FiberWire (Arthrex) to each anchor, the Arthrex intra-articular measurement device is used to measure the distance between each of the anchors (medial, lateral, anterior, and posterior), using the individual sutures from the anchors. This allows for exact measurement between the anchors and for the graft itself to span the whole defect, by measuring the distances even over a curved area (Video 1).
Fig 1.

After placement of 2 superior glenoid and 2 medial greater tuberosity anchors (right shoulder, beach-chair position, posterolateral viewing portal).
The ArthroFlex dermal allograft (Arthrex) is 3.5 mm thick and measures 4 × 7 cm in the package. The ArthroFlex graft is cut and prepared from the arthroscopic measurements from the glenoid and greater tuberosity anchors (Fig 2, Video 1). In general, we add 2 cm to the distances measured from the medial to lateral anchors and 2 cm to the distances measured from the anterior to posterior anchors to determine our graft size; however, care is taken to determine the best measurements to fully cover the defect in the superior capsule. The average graft size has been found to be 5.5 cm medial-lateral. By use of a 2.0-mm sterile tissue biopsy punch (or 14-gauge spinal needle or dental dam punch), holes are created at the 4 points corresponding to the 4 anchors to help the sutures slide through the graft without catching and twisting the graft. At least 5 mm of allograft is adjacent to each of the 4 points to decrease the chance of sutures cutting out of the graft. Margin-convergence suture holes in the graft may be prepared at this time; however, we have found that the Scorpion suture-passing device (Arthrex) can pass sutures after the graft is positioned in the shoulder.
Fig 2.
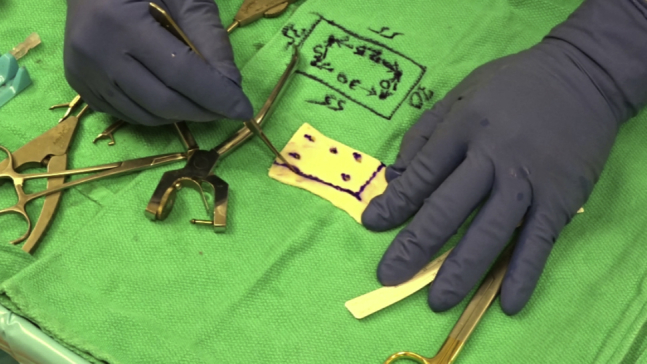
Preparation of ArthroFlex graft based on intra-articular measurements from each anchor.
The sutures are then brought out through the PassPort cannula 1 anchor set at a time. We recommend pulling the sutures out in the following order: anterior glenoid, posterior glenoid, anteromedial tuberosity, and posteromedial tuberosity. We also recommend having an assistant separate the sutures and apply tension to the suture limbs during the passage of the suture limbs out of the PassPort cannula to decrease the chance of tangling the sutures. After the sutures are passed through the cannula, each suture set is passed through its respective punched holes in the graft (Fig 3, Video 1). Medially, 1 FiberWire limb from each SutureTak is tied together. Laterally, 1 limb from each FiberWire is tied together. This creates 2 double-pulley systems—1 medial and 1 lateral (Fig 4, Video 1). The ArthroFlex graft is then introduced through the PassPort and into the subacromial space using a KingFisher grasper (Arthrex). By pulling on the limbs from each double pulley, the graft will set itself into position medially and laterally.
Fig 3.
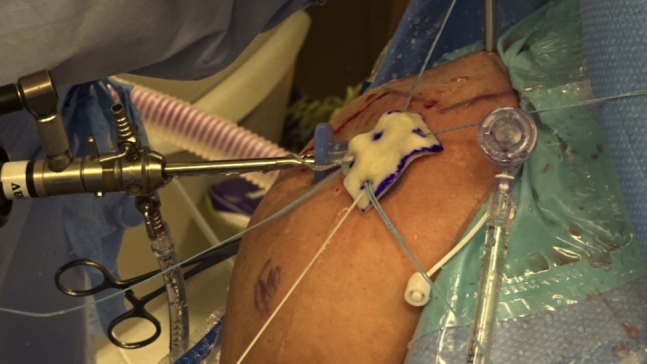
All of the sutures from the glenoid and greater tuberosity anchors are passed through the appropriate holes in the graft (right shoulder, beach-chair position).
Fig 4.
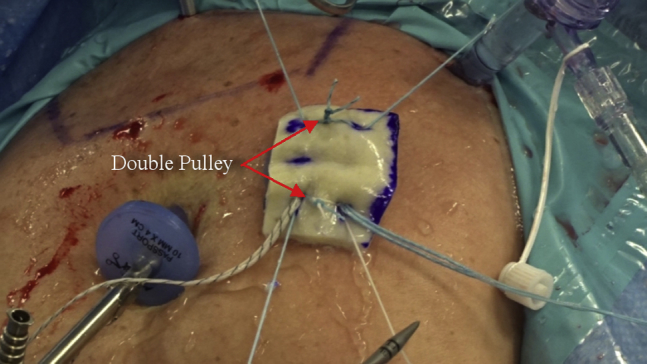
One suture limb from each glenoid anchor is tied together with the double-pulley technique (right shoulder, beach-chair position). In a similar fashion, 1 FiberWire suture limb from each greater tuberosity anchor is tied together with the double-pulley technique to aid in graft passage, positioning, and security.
The medial double-pulley sutures are brought through the Neviaser portal. A bone hole is prepared through this portal on the medial glenoid neck, and a Labral SwiveLock suture anchor (Arthrex) is used to secure the medial double-pulley sutures. The anchor is implanted, and the excess sutures are cut. This completes the medial glenoid attachment in a PASTA (partial articular supraspinatus tendon avulsion) Bridge configuration. As an alternative, if the medial glenoid neck is difficult to visualize, the double-pulley sutures can be tied as a double surgeon's knot instead of using the PASTA bridge configuration and a Labral SwiveLock anchor.
The swedged FiberTapes from the tuberosity anchors are now cut and separated. One FiberTape limb from each medial-row tuberosity anchor and the sutures from the lateral double pulley are attached to a 4.75-mm Vented SwiveLock anchor (Arthrex). After a socket is punched into the anterolateral greater tuberosity, the sutures are tensioned, and the SwiveLock anchor is placed into the bone socket, fixing the sutures and graft. The remaining FiberTapes are brought posterolaterally to the final 4.75-mm Vented SwiveLock anchor and fixed in place. This completes the SpeedBridge configuration (Arthrex) on the lateral tuberosity (Fig 5, Video 1).
Fig 5.
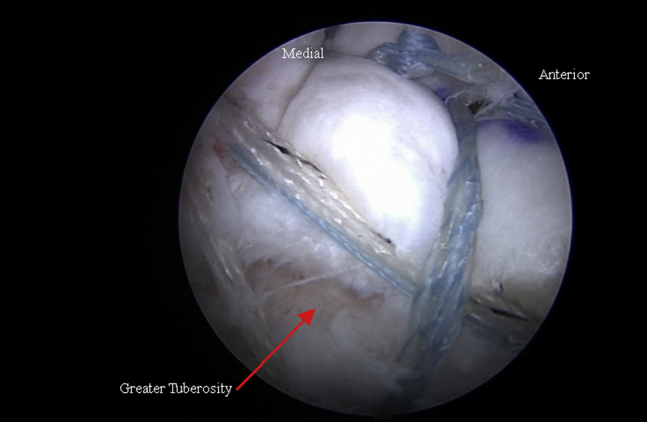
Completed SpeedBridge component of arthroscopic superior capsular reconstruction (right shoulder, beach-chair position, posterolateral viewing portal).
By use of either a No. 2 FiberWire suture and a Scorpion suture-passing device or a 90° straight SutureLasso (Arthrex) with a No. 2 FiberStick (Arthrex), a suture is passed through the infraspinatus tendon and into the posterior margin of the graft. The suture is tied with a knot pusher. The process is repeated to complete the remaining margin-convergence sutures posteriorly (Fig 6, Video 1). The surgeon must not over-tension the graft and surrounding tissues. Anterior margin convergence can aid in graft tensioning, but the rotator interval tissues can sometimes be absent. Care should be taken not to over-constrain the shoulder anteriorly by attaching the graft to the subscapularis. This would be equivalent to closing the rotator interval. Posterior margin convergence is necessary to prevent subluxation of the humeral head and to allow restoration of the rotator cable.
Fig 6.
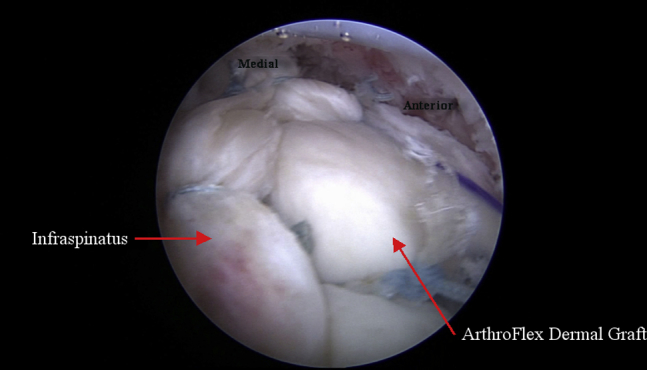
Final reconstruction of superior capsule with anterior and posterior margin-convergence sutures between graft and native rotator interval tissue and between graft and native infraspinatus tendon, respectively (right shoulder, beach-chair position, posterolateral viewing portal).
Discussion
The SCR is an anatomic reconstruction of the superior capsule to restore the normal restraint to superior translation that occurs with a deficient rotator cuff. In their original description, Mihata et al.11 published good short-term results of this reconstructive procedure. In their experience, they have found this to be a safe and reproducible procedure and have had far fewer of the reported complications seen with procedures such as the reverse total shoulder arthroplasty.11, 15 Furthermore, we are not aware of any “burned bridges” with this procedure because a salvage reverse shoulder arthroplasty could be performed later if necessary (Table 2).
Table 2.
Advantages and Disadvantages of Superior Capsular Reconstruction
|
|
The recent studies on the biomechanics of the superior capsule suggest that the original ideas suggested by Burkhart et al.16 regarding the rotator cable complex were correct in their assessment of its necessity to keep the glenohumeral joint stable and reduced. This complex does keep the humeral head from subluxating superiorly. However, the actual key stabilizer is not the rotator cuff. The rotator cuff is not the main constraint to maintaining the glenohumeral joint reduced; the capsule is the key static superior stabilizer. The rotator cuff is a dynamic stabilizer; it helps to reinforce the capsule and gives strength to movements overhead. This concept explains why the SCR can alleviate the severe pain and disability from irreparable massive rotator cuff tears and illustrates how the rotator cuff does not have to be repaired in these salvage situations. The rotator cuff is key to the restoration of complete strength, but function can be significantly improved with just the reconstruction of the superior capsule. The pain in these situations is a result of the humeral head being out of position and the rest of the muscles trying to make the shoulder work without the proper fulcrum.
The described technique improves on the originally described procedure in many ways (Table 3). It uses a strong, thick dermal allograft, negating the need to take a large fascial autograft that is described as 6 to 9 mm thick. When combined with our stronger fixation methods, this technique allows for faster mobilization postoperatively. Our technique also allows for more accurate measurement and placement of the graft. Using the 2 double pulleys, we allow placement of the graft to be more reliable, preventing twisting and tangling of the grafts and sutures. We believe the described technique will aid surgeons in performing an SCR in the appropriate patient.
Table 3.
Tips and Pearls
| Position the arm in neutral position |
| Repair subscapularis tears |
| Span the defect with enough anchors |
| Accurately measure between the anchors |
| Perform graft measurement using sutures, which allows for exact measurements even over curved areas |
| Use the ArthroFlex dermal allograft of 3.5 mm thickness |
| Punch graft holes for suture sliding |
| Use a 10-mm PassPort cannula for graft passage |
| Incorporate any infraspinatus repairs into graft fixation |
| Do not over-constrain the shoulder |
| Always perform margin convergence posteriorly |
| Perform margin convergence anteriorly if there is adequate tissue |
Footnotes
The authors report the following potential conflict of interest or source of funding: A.M.H. and C.R.A. receive support from Arthrex.
Supplementary Data
The superior capsular reconstruction is performed for massive irreparable rotator cuff tears with minimal to no arthritis and a fully functioning deltoid muscle. With the arthroscope through the lateral portal, a Neviaser portal is created. A 3.0-mm BioComposite SutureTak anchor is placed percutaneously medial to the labrum and posterior. An anterosuperior portal is created, and a second SutureTak is placed anteriorly. Through a superolateral portal, two 4.75-mm BioComposite Vented SwiveLock anchors with attached swedged FiberTapes are placed into the medial row at the greater tuberosity, 1 anterior and 1 posterior. By use of the attached No. 2 FiberWire to each anchor, an intra-articular measurement device is used to measure the distance between each of the anchors (medial, lateral, anterior, and posterior). The ArthroFlex dermal allograft is 3.5 mm thick and is cut and prepared from the arthroscopic measurements from the anchors. With a punch, holes are created at the 4 points corresponding to the 4 anchors to help the sutures slide through the graft without catching and twisting the graft. The sutures are then brought out the PassPort cannula 1 anchor set at a time. We recommend keeping the sutures separated into quadrants and applying tension to the suture limbs to decrease the chance of tangling the sutures. After the sutures are passed through the cannula, each suture set is passed through its respective punched holes in the graft. Medially, 1 FiberWire limb from each SutureTak is tied together. Laterally, 1 FiberWire limb from each SwiveLock is tied together. This creates 2 double-pulley systems—1 medial and 1 lateral. The ArthroFlex graft is then introduced through the PassPort and into the subacromial space using a KingFisher grasper. By pulling on the limbs from each double pulley, the graft will set itself into position medially and laterally. The medial double-pulley sutures are brought through the Neviaser portal and tensioned. The lateral double pulley is tightened by pulling on its sutures. A bone hole is prepared through the Neviaser portal on the medial glenoid neck. A Labral SwiveLock suture anchor is used to secure the medial double-pulley sutures. The anchor is implanted, and the excess sutures are cut. This completes the medial glenoid attachment in a PASTA (partial articular supraspinatus tendon avulsion) Bridge configuration. The blue suture, the posterior limb from the lateral double-pulley system, is passed through the residual infraspinatus, followed by the white posterior swedged FiberTapes, by use of a Scorpion suture passer. This will incorporate the infraspinatus into the SpeedBridge construct posterolaterally. A socket is punched into the anterolateral aspect of the greater tuberosity. The swedged FiberTapes from the tuberosity anchors are cut and separated. One FiberTape limb from each medial-row tuberosity anchor and the sutures from the lateral double pulley are attached to a 4.75-mm Vented SwiveLock anchor and fixed into the socket. The posterolateral socket is punched, and the remaining FiberTapes are brought posterolaterally to the final SwiveLock anchor and fixed in place. This completes the SpeedBridge configuration on the lateral tuberosity. A No. 2 FiberWire suture is passed through the infraspinatus tendon and into the posterior margin of the graft and tied together for our posterior margin convergence. Anteriorly, a Scorpion suture passer is used to pass sutures through the graft and then through the anterior rotator interval tissue. The anterior margin-convergence suture is then tied with a knot pusher. We performed medial margin convergence between the anterior tissues and the infraspinatus. This completes the superior capsular reconstruction with infraspinatus repair as seen from the bursal side.
References
- 1.Liem D., Lengers N., Dedy N., Poetzl W., Steinbeck J., Marquardt B. Arthroscopic debridement of massive irreparable rotator cuff tears. Arthroscopy. 2008;24:743–748. doi: 10.1016/j.arthro.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 2.Lee B., Cho N., Rhee Y. Results of arthroscopic decompression and tuberoplasty for irreparable massive rotator cuff tears. Arthroscopy. 2011;27:1341–1350. doi: 10.1016/j.arthro.2011.06.016. [DOI] [PubMed] [Google Scholar]
- 3.Kim S., Lee I., Kim S. Arthroscopic partial repair of irreparable large to massive rotator cuff tears. Arthroscopy. 2012;28:761–768. doi: 10.1016/j.arthro.2011.11.018. [DOI] [PubMed] [Google Scholar]
- 4.Yoo J., Koh K., Woo K., Shon M., Koo K. Clinical and radiographic results of partial repairs in irreparable rotator cuff tears: Preliminary report. Arthroscopy. 2010;26:E3. (abstr) [Google Scholar]
- 5.Wellmann M., Lichtenberg S., da Silva G., Magosch P., Habermeyer P. Results of arthroscopic partial repair of large retracted rotator cuff tears. Arthroscopy. 2013;29:1275–1282. doi: 10.1016/j.arthro.2013.05.006. [DOI] [PubMed] [Google Scholar]
- 6.Holtby R., Razmjou H. A prospective outcome study of patients with large and massive rotator cuff tears: Role of complete vs. partial repair. Arthroscopy. 2011;27:E88–E89. (abstr) [Google Scholar]
- 7.Mori D., Funakoshi N., Yamashita F. Arthroscopic surgery of irreparable large or massive rotator cuff tears with low-grade fatty degeneration of the infraspinatus: Patch autograft procedure versus partial repair procedure. Arthroscopy. 2013;29:1911–1921. doi: 10.1016/j.arthro.2013.08.032. [DOI] [PubMed] [Google Scholar]
- 8.Chang V., Grimberg J., Kany J., Valenti P., Duranthon L., Garret J. Early clinical results of arthroscopic latissimus dorsi transfer for irreparable cuff tears. Arthroscopy. 2012;28:E14. (abstr) [Google Scholar]
- 9.Yamakado K. Arthroscopic assisted latissimus dorsi transfer for irreparable cuff tears. Arthroscopy. 2015;31:E11–E12. doi: 10.1016/j.arthro.2014.10.005. (abstr) [DOI] [PubMed] [Google Scholar]
- 10.Grimberg J., Kany J., Valenti P., Amaravathi R., Ramalingam A. Arthroscopic-assisted latissimus dorsi tendon transfer for irreparable posterosuperior cuff tears. Arthroscopy. 2014;31:599–607. doi: 10.1016/j.arthro.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 11.Mihata T., Lee T.Q., Watanabe C. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459–470. doi: 10.1016/j.arthro.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 12.Mihata T., McGarry M.H., Pirolo J.M., Kinoshita M., Lee T.Q. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: A biomechanical cadaveric study. Am J Sports Med. 2012;40:2248–2255. doi: 10.1177/0363546512456195. [DOI] [PubMed] [Google Scholar]
- 13.Patzer T., Habermeyer P., Hurschler C. The influence of superior labrum anterior to posterior (SLAP) repair on restoring baseline glenohumeral translation and increased biceps loading after simulated SLAP tear and the effectiveness of SLAP repair after long head of biceps tenotomy. J Shoulder Elbow Surg. 2012;21:1580–1587. doi: 10.1016/j.jse.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 14.McMahon P.J., Burkart A., Musahl V., Debski R.E. Glenohumeral translations are increased after a type II superior labrum anterior-posterior lesion: A cadaveric study of severity of passive stabilizer injury. J Shoulder Elbow Surg. 2004;13:39–44. doi: 10.1016/j.jse.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 15.Saltzman B.M., Chalmers P.N., Gupta A.K., Romeo A.A., Nicholson G.P. Complication rates comparing primary with revision reverse total shoulder arthroplasty. J Shoulder Elbw Surg. 2014;23:1647–1654. doi: 10.1016/j.jse.2014.04.015. [DOI] [PubMed] [Google Scholar]
- 16.Burkhart S., Esch J., Jolson R. The rotator crescent and rotator cable: An anatomic description of the shoulder’s “suspension bridge.”. Arthroscopy. 1993;9:611–616. doi: 10.1016/s0749-8063(05)80496-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The superior capsular reconstruction is performed for massive irreparable rotator cuff tears with minimal to no arthritis and a fully functioning deltoid muscle. With the arthroscope through the lateral portal, a Neviaser portal is created. A 3.0-mm BioComposite SutureTak anchor is placed percutaneously medial to the labrum and posterior. An anterosuperior portal is created, and a second SutureTak is placed anteriorly. Through a superolateral portal, two 4.75-mm BioComposite Vented SwiveLock anchors with attached swedged FiberTapes are placed into the medial row at the greater tuberosity, 1 anterior and 1 posterior. By use of the attached No. 2 FiberWire to each anchor, an intra-articular measurement device is used to measure the distance between each of the anchors (medial, lateral, anterior, and posterior). The ArthroFlex dermal allograft is 3.5 mm thick and is cut and prepared from the arthroscopic measurements from the anchors. With a punch, holes are created at the 4 points corresponding to the 4 anchors to help the sutures slide through the graft without catching and twisting the graft. The sutures are then brought out the PassPort cannula 1 anchor set at a time. We recommend keeping the sutures separated into quadrants and applying tension to the suture limbs to decrease the chance of tangling the sutures. After the sutures are passed through the cannula, each suture set is passed through its respective punched holes in the graft. Medially, 1 FiberWire limb from each SutureTak is tied together. Laterally, 1 FiberWire limb from each SwiveLock is tied together. This creates 2 double-pulley systems—1 medial and 1 lateral. The ArthroFlex graft is then introduced through the PassPort and into the subacromial space using a KingFisher grasper. By pulling on the limbs from each double pulley, the graft will set itself into position medially and laterally. The medial double-pulley sutures are brought through the Neviaser portal and tensioned. The lateral double pulley is tightened by pulling on its sutures. A bone hole is prepared through the Neviaser portal on the medial glenoid neck. A Labral SwiveLock suture anchor is used to secure the medial double-pulley sutures. The anchor is implanted, and the excess sutures are cut. This completes the medial glenoid attachment in a PASTA (partial articular supraspinatus tendon avulsion) Bridge configuration. The blue suture, the posterior limb from the lateral double-pulley system, is passed through the residual infraspinatus, followed by the white posterior swedged FiberTapes, by use of a Scorpion suture passer. This will incorporate the infraspinatus into the SpeedBridge construct posterolaterally. A socket is punched into the anterolateral aspect of the greater tuberosity. The swedged FiberTapes from the tuberosity anchors are cut and separated. One FiberTape limb from each medial-row tuberosity anchor and the sutures from the lateral double pulley are attached to a 4.75-mm Vented SwiveLock anchor and fixed into the socket. The posterolateral socket is punched, and the remaining FiberTapes are brought posterolaterally to the final SwiveLock anchor and fixed in place. This completes the SpeedBridge configuration on the lateral tuberosity. A No. 2 FiberWire suture is passed through the infraspinatus tendon and into the posterior margin of the graft and tied together for our posterior margin convergence. Anteriorly, a Scorpion suture passer is used to pass sutures through the graft and then through the anterior rotator interval tissue. The anterior margin-convergence suture is then tied with a knot pusher. We performed medial margin convergence between the anterior tissues and the infraspinatus. This completes the superior capsular reconstruction with infraspinatus repair as seen from the bursal side.


