Abstract
The most commonly reported reasons for persistent hip pain after hip arthroscopy are residual femoroacetabular impingement, dysplasia and dysplasia variants, or extra-articular impingement. There are some cases in which the underlying osseous pathomorphology has been appropriately treated, and the cause of persistent hip pain can be soft-tissue injuries such as chondrolabral tears or capsular abnormalities. Capsular defects after hip arthroscopy may suggest an alteration of the biomechanical properties of the iliofemoral ligament and lead to iatrogenically induced hip instability. There are a growing number of biomechanical and clinical studies showing the importance of capsular management during hip arthroscopy. We describe the workup, examination under anesthesia, diagnostic arthroscopy, and technique of capsular plication for iatrogenic instability of the hip.
Iatrogenically induced hip instability or microinstability is an increasingly common clinical problem and has been reported to be the primary diagnosis in up to 35% of revision hip arthroscopy cases.1 There are 7 reported cases of hip dislocation after hip arthroscopy,2, 3, 4, 5, 6, 7 but the actual number of dislocations is thought to be largely under-reported. Although gross instability of the hip is rare because of its osseous congruency, microinstability is attributed to improper capsular management after prior surgery.2, 8, 9 McCormick et al.10 reported capsular irregularities in all patients requiring revision hip arthroscopy without residual femoroacetabular impingement (FAI), and 7 of 9 patients had capsular defects visualized on magnetic resonance arthrography (MRA).
At present, capsulotomies are required for hip arthroscopy to visualize and treat the underlying hip pathology. Although the size, type, and location may vary according to surgeon preference, capsulotomies typically cut into the iliofemoral ligament, a Y-shaped structure believed by many surgeons to be the strongest ligament in the body. In this way, meticulous closure is critical to maintain the structure and function of the iliofemoral ligament.
Clinical Evaluation
Iatrogenic hip instability should be considered in any patient with persistent hip pain after hip arthroscopy. Treating surgeons should also consider medical, rheumatologic, connective tissue, and chronic pain conditions, such as fibromyalgia and chronic regional pain syndrome. The clinical presentation may vary from a macroinstability dislocation event to microinstability pain when attempting to increase activity. Patients may have difficulty with activities of daily living including prolonged standing or walking.
Physical examination should evaluate joint hypermobility, and generalized laxity should be assessed using Beighton's criteria (Table 1).11 Hip range of motion should be measured on the affected and opposite extremities. Some patients may have supraphysiological range of motion at baseline, but the affected hip may actually show decreased range of motion because of pain and apprehension. Excessive hip extension and external rotation may indicate a lack of capsular restraint. The instability test, when the examiner provides an external rotation moment on the foot with the leg in extension, has been described. In a normal hip, the foot will recoil toward a neutral position. In an unstable hip, the foot will remain in an externally rotated posture because of insufficiency of the iliofemoral ligament. Similar to the shoulder, the anterior apprehension test elicits a subjective feeling of uneasiness when the hip is placed into extension, abduction, and external rotation. The relocation test produces an improved sense of stability when the hip is flexed and internally rotated from an abducted position. This last test suggests relocation of a relatively lateralized femoral head, which may be present in cases of dysplasia or subtle instability.
Table 1.
Beighton's Physical Examination Criteria for Generalized Ligamentous Laxity11
| Criterion | Maximum Number of Points∗ |
|---|---|
| Thumb dorsiflexion to forearm | 2 |
| Little-finger hyperextension at metacarpophalangeal joint beyond 90° | 2 |
| Elbow hyperextension beyond 10° | 2 |
| Knee hyperextension beyond 10° | 2 |
| Lumbar forward flexion with ability to rest palms flat on floor | 1 |
Patients earn 2 points for bilateral involvement of each criterion. The maximum number of points earned is 9; greater than 4 points indicates hypermobility or joint laxity.
Plain radiographs may be used to evaluate early or progressive signs of arthritis, FAI, dysplasia, or extra-articular impingement. Preoperative radiographs may be compared with the most recent radiographs to determine interval changes in the amount of FAI. A computed tomography scan with 3-dimensional reconstruction is a critical study to obtain accurate assessment of the acetabulum and proximal femur at the level of the joint and rotational alignment. MRA is the preferred study to evaluate soft-tissue integrity. In addition to yielding information on the chondrolabral status, MRA can provide information on the containment of gadolinium within the joint, as well as capsular insufficiency or hypertrophy. If there is extravasation of gadolinium or capsular insufficiency, the surgeon should suspect hip joint instability.
Surgical Technique
The patient is positioned supine, and general anesthesia is induced for complete muscle relaxation. The patient is positioned on the table (Smith & Nephew, Memphis, TN) with a well-padded perineal post and boots. The pelvis is slightly translated toward the contralateral hip, and gentle distraction is applied to the contralateral limb. We perform an examination with the patient under anesthesia without traction to assess the degree of capsular laxity or microinstability. The operative limb is placed in about 20° of abduction, and manual distraction is attempted during live fluoroscopic visualization. In some cases, only 2 fingers are required for gross distraction, and significant joint space widening with minimal force indicates gross instability (Fig 1, Video 1, Table 2).
Fig 1.
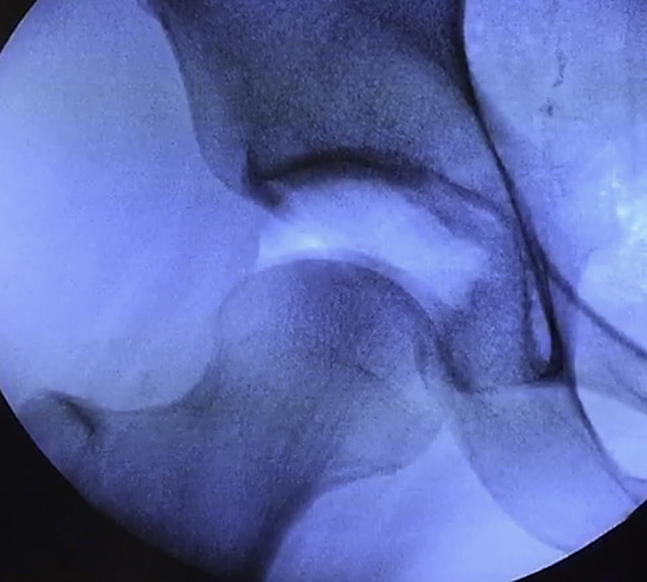
Microinstability of a right hip is indicated by significant joint space widening under fluoroscopy while the operative limb is manually distracted in 20° of abduction.
Table 2.
Pearls and Pitfalls of Hip Arthroscopy to Treat Microinstability
|
|
Traction is applied to the operative limb first with the hip flexed 20° and abducted 20°. Gentle oscillations are then used to alleviate muscular tension as the limb is slowly extended and adducted. The joint should distract up to 10 mm with this maneuver, and an audible pop may be heard, indicating disruption of the chondrolabral suction seal. Once the suction seal has been violated, the force required for distraction is much less, and the leg can be brought back into the starting position while releasing some distraction. The hip is positioned for optimal surgical maneuvering by extension parallel to the floor, neutral adduction, and internal rotation of 45° for maximal femoral neck length. Nursing staff should note the onset of traction because there have been case reports of avascular necrosis from prolonged traction.12, 13, 14
After sterile preparation and draping, the anterior superior iliac spine is marked, and a vertical line is extended down the thigh toward the center of the knee. The greater trochanter is marked as well. Prior arthroscopic incisions should be demarcated and reused unless they are suboptimally situated. The anterolateral (AL) portal is established first, 1 cm proximal and 1 cm anterior to the AL tip of the greater trochanter. In thinner individuals, this portal should be more posterior to avoid abutting other anterior portals. Typically, the spinal needle should enter the joint parallel to the floor and just 1 to 2 mm above the head on fluoroscopy so that it sits below the labrum. In revision cases with deficient capsular tension, the surgeon may have fewer palpatory clues when passing the needle through the capsule. Standard cannulation (8.5 × 110 mm; Smith & Nephew) allows intra-articular visualization with a 70° arthroscope (Smith & Nephew). The anterior portal starts 4 to 5 cm medial and 1 cm inferior to the AL portal without crossing the vertical anterior superior iliac spine line to protect the femoral nerve and vessels. Under direct visualization, the anterior portal should enter as close as possible to the AL portal to minimize the interportal capsulotomy. This portal should traverse the thickest capsule corresponding to the iliofemoral ligament and the 12- to 3-o’clock position. The camera is briefly switched to the anterior portal to ensure that the AL portal has not violated the labrum.
We then conduct a diagnostic arthroscopy from the AL portal with the capsule still on tension. The surgeon should evaluate for a patulous capsule or frank capsular defects (Fig 2). Capsulolabral adhesions are frequently seen in revision cases and may be a representation of inadequate capsular closure from the prior operation; if not adequately repaired before, the anterior capsule may become matted down to the labrum (Fig 3). Similar to the drive-through sign in knee and shoulder arthroscopy,15, 16, 17 increased laxity of the hip capsule can be shown by the ease of passing an arthroscope between the femoral head and labrum at the level of the iliofemoral ligament (Fig 4). Adhesions and a positive drive-through sign thus indicate the need for not just a lysis of adhesions but a capsular plication or reconstruction as well.
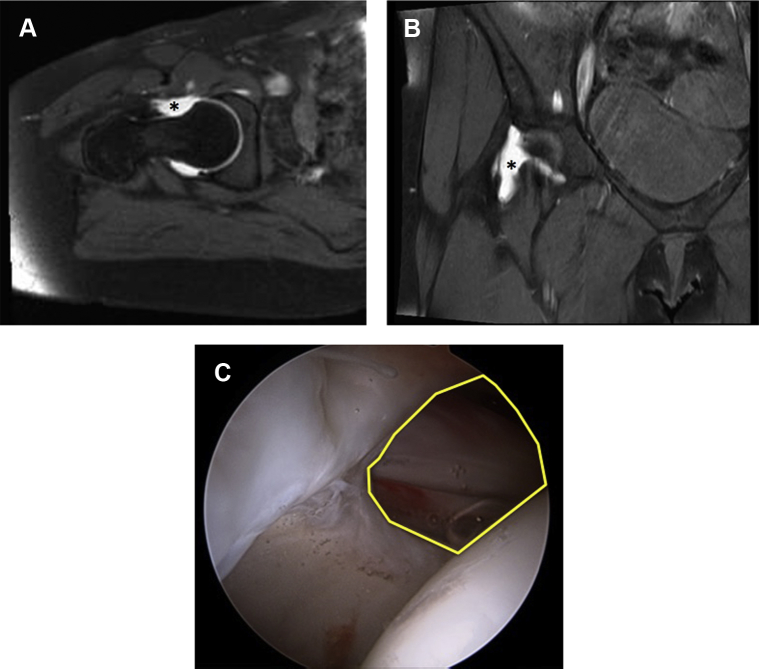
Fig 2.
(A) Axial and (B) coronal T2-weighted magnetic resonance imaging cuts of a right hip show a patulous capsule with extravasation of contrast suggestive of an anterior capsular defect (asterisks). (C) Revision hip arthroscopy confirms a large anterosuperior capsular defect (yellow outline).
Fig 3.
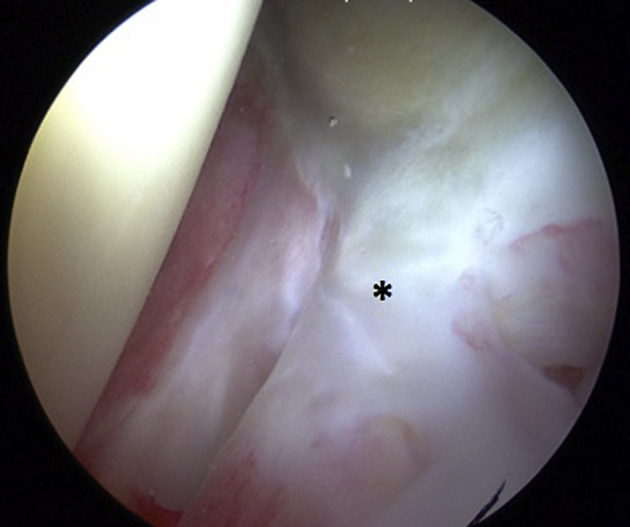
Left hip arthroscopy, viewed from the anterolateral portal, shows adhesions (asterisk) at the capsulolabral interval, which may indicate microinstability in the context of a positive drive-through sign.
Fig 4.
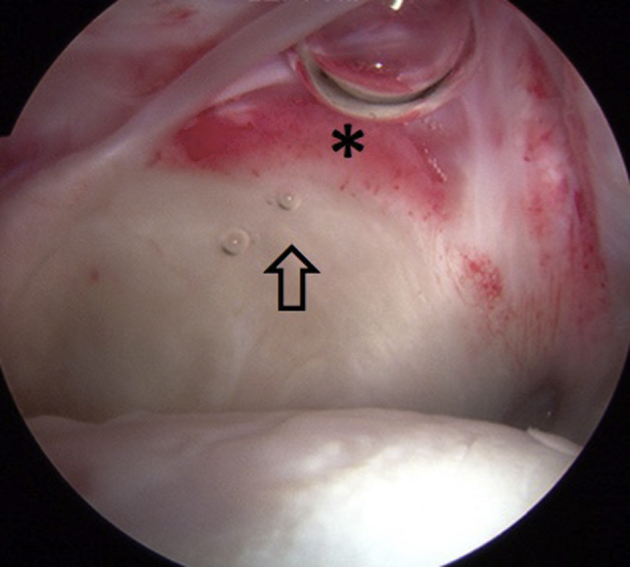
A positive drive-through sign is shown by the ease of maneuvering the arthroscope deep to the iliofemoral ligament on arthroscopy of a left hip, viewed from the anterolateral portal. One should note that this patient has a redundant capsule with a clear interface between the normal capsule (arrow) and inflamed scar tissue (asterisk) between the capsule and acetabulum.
After assessing the capsular integrity, we perform a transverse interportal capsulotomy using an arthroscopic beaver blade (Samurai; Stryker Sports Medicine, Greenwood Village, CO) 8 mm from the labrum and spanning 10 to 15 mm in length. The degree of acetabular coverage is then reviewed fluoroscopically and from preoperative radiographic measurements. Capsular laxity may be associated with borderline hip dysplasia, and acetabular rim trimming should be exercised with caution if the lateral center-edge angle is less than 25°. Thermal soft-tissue ablation proximal to the labrum improves visualization of the chondrolabral junction. A distal anterolateral accessory portal is established 4 to 6 cm straight distal to the AL portal for suture anchor placement. Labral refixation or reconstruction is performed depending on the integrity of the native labrum. Our preference is to preserve the native chondrolabral tissue whenever possible, but an allograft is ordered in cases of labral insufficiency.
Next, the peripheral compartment can be visualized and addressed. Traction is released, and the hip is flexed 20° to 30° depending on the extent of the cam deformity. The surgeon can extend a T-capsulotomy perpendicular to the interportal capsulotomy down the center of the femoral neck. This capsulotomy runs between the iliocapsularis muscle medially and gluteus minimus muscle laterally to the capsular reflection at the intertrochanteric line. If indicated, a femoral neck osteochondroplasty is performed to ensure impingement-free motion. Up to 30% of the femoral neck diameter may be resected before altering its load-bearing capacity and increasing its susceptibility to fracture.18, 19
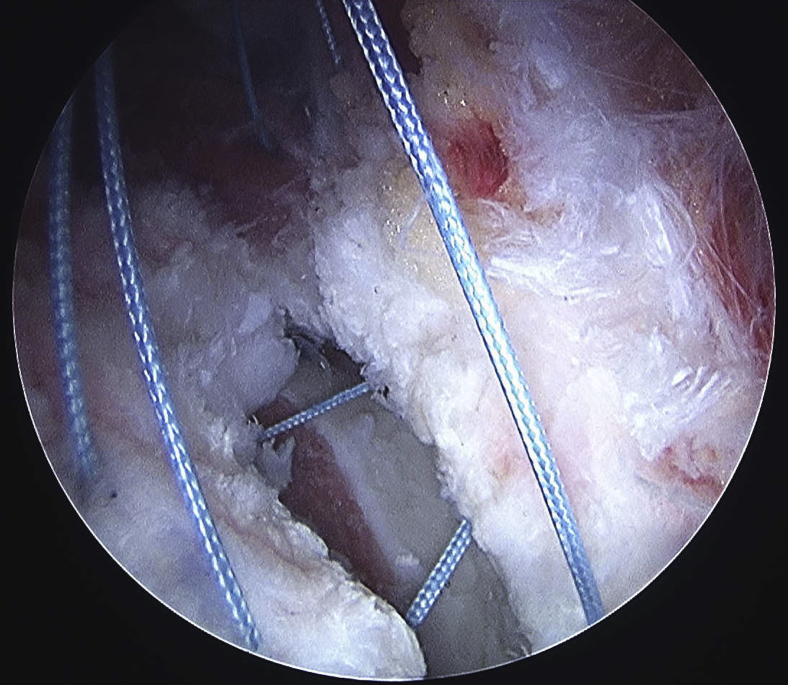
Capsular plication may be accomplished either in a direct side-to-side fashion or with a component of an inferior capsular shift. The vertical component of the T-capsulotomy is closed first, beginning at the base of the iliofemoral ligament. An 8.5 × 90–mm cannula is placed in the AL portal for ease of maneuvering instruments in the extracapsular space, while an 8.5 × 110–mm cannula is retained through the distal anterolateral accessory portal. A suture-passing device—either a Spectrum (ConMed Linvatec, Key Largo, FL) or Slingshot (Stryker Sports Medicine)—is placed through the AL portal and through the lateral leaflet of the iliofemoral ligament. Monofilament nonabsorbable suture (PDS; Ethicon, Somerville, NJ) is shuttled and retrieved with a tissue penetrator through the medial leaflet. Greater bites of capsular tissue allow greater degrees of plication. No. 2 nonabsorbable high-strength suture is passed through and tied on the outer capsular surface using reverse half-hitches on alternating posts. Successive sutures are placed along the vertical capsulotomy, for a total of 3 to 4 stitches. The horizontal interportal capsulotomy is closed using a Spectrum, Slingshot, or InJector II (Stryker Sports Medicine), which allows closure through a single cannula. The InJector II first grasps and passes 1 suture end through the acetabular side of the iliofemoral ligament. The other end of the suture is then placed in the InJector II and passed through the femoral side of the iliofemoral ligament. This distal suture end may be passed in such a way to create either a direct side-to-side repair or an inferomedial capsular shift as described by Domb et al.20 The latter technique involves taking a larger, more medial bite of capsule on the distal femoral side. This results in an inferomedial capsular shift and augments the “screw-home” mechanism by which spiral, leash-like capsular fibers twist and tighten during hip extension and external rotation.9 We prefer to pass 2 to 3 sutures with the hip in 20° to 30° of flexion (Fig 5) and then tie all of the interportal sutures at the end with the hip in neutral extension.
Fig 5.
For closure of the horizontal interportal capsulotomy, 2 to 3 sutures are passed with the hip in 20° to 30° of flexion, as shown on arthroscopy of a left hip, viewed from the anterolateral portal. After all sutures have been passed, the hip is brought into neutral extension and the sutures are then tied sequentially.
Postoperatively, patients are placed into an abduction pillow, which should be worn at night to prevent the foot from falling into external rotation. In the recovery unit, patients are fitted for a hip orthosis (Ossur, Foothill Ranch, CA) that allows 0° to 90° of flexion and avoids hip extension and external rotation. Patients are instructed to use crutches with 20-lb flat-foot weight-bearing restrictions for 6 weeks. They are encouraged to use a continuous passive motion device and a stationary bicycle for the first 3 weeks. Muscle strengthening is focused on core strengthening and proximal neuromotor control.
Discussion
Iatrogenic hip instability is becoming a more commonly recognized source of hip pain and dysfunction after prior hip arthroscopy. The diagnosis of iatrogenic hip instability can be obvious with a macroinstability event, or hip dislocation, but it may be less obvious without such an event. It is thought that microinstability may be a much more common complication but is under-reported because of the difficulty of diagnosis. When evaluating a patient with failure of a prior hip arthroscopy, the treating surgeon has to determine the cause of failure. Foremost, the untreated or undertreated residual FAI, unrecognized dysplasia, or extra-articular impingement has to be evaluated by clinical examination and 3-dimensional imaging studies. In cases in which osseous pathomorphology is not thought to be the primary reason for failure, MRA is important to understand the integrity of the joint capsule. Evidence of capsular defects or insufficiency should raise suspicion for iatrogenic hip microinstability.
Frank et al.21 recently published a comparative matched-pair analysis of patients who underwent T-capsulotomy with partial repair versus complete repair. Partial repair entailed closure of only the vertical component of the capsulotomy, whereas complete repair entailed closure of the interportal capsulotomy as well. Each group had 32 age-, gender-, and morphology-matched patients. After 2 years, both groups had significant improvements in the Hip Outcome Score–Activities of Daily Living. The complete repair group, however, showed a superior Hip Outcome Score–Sport-Specific activities as early as 6 months after surgery and maintained this improvement after 2 years. Moreover, the partial repair group had a 13% revision rate compared with no revisions in the complete repair cohort. These findings may be a harbinger of what is to come for hip arthroscopists as a greater number of revisions are performed for inadequate capsular closure.
Seven published case reports have documented gross dislocation after hip arthroscopy.2, 3, 4, 5, 6, 7 Most of these cases have been successfully treated with revision primary capsular closure.2, 3 Conversely, Dierckman and Guanche4 reported a case of anterior dislocation after an unclosed capsulotomy site progressed to a large 2.5 × 4–cm capsular defect; at revision surgery, the senior author reconstructed the anterior capsule with iliotibial band autograft. Iliofemoral ligament reconstruction has also been used effectively in the arthroplasty population.22
Although it is poorly understood, iatrogenic hip instability is an increasingly common problem that warrants further attention. The anatomic and biomechanical properties of the iliofemoral ligament are still not completely defined, but recent scientific and clinical studies have shown the importance of capsular repair to maintain stability of the hip joint capsule.8, 23, 24, 25, 26, 27 At this point, there is no consensus regarding capsular repair, but there is a growing body of data suggesting the importance of capsular management. Although capsulotomy is required for adequate visualization and treatment of FAI, we recommend that primary capsular closure or plication may minimize the risk of iatrogenic hip instability.
Footnotes
The authors report the following potential conflict of interest or source of funding: M.J.S. receives support from Linvatec and Smith & Nephew. R.C.M. receives support from KNG Health Consulting, Pivot Medical, Smith & Nephew, and Stryker. S.K.A. receives support from Pivot Medical and Stryker. S.J.N. receives support from Stryker, Ossur, Allosource, Arthrex, Athletico, DJ Orthopaedics, Linvatec, Miomed, and Smith & Nephew.
Supplementary Data
Technique for examination under anesthesia, diagnostic arthroscopy, and capsular plication for iatrogenic hip microinstability. Arthroscopy is shown in a left hip from an anterolateral viewing portal with the patient in the supine position. One should note that the portion of the video showing the examination under anesthesia was taken from the case of a different patient and that the isolated photograph of joint space widening under fluoroscopy corresponds to a right hip.
References
- 1.Philippon M.J., Schenker M.L., Briggs K.K., Kuppersmith D.A., Maxwell R.B., Stubbs A.J. Revision hip arthroscopy. Am J Sports Med. 2007;35:1918–1921. doi: 10.1177/0363546507305097. [DOI] [PubMed] [Google Scholar]
- 2.Ranawat A.S., McClincy M., Sekiya J.K. Anterior dislocation of the hip after arthroscopy in a patient with capsular laxity of the hip. A case report. J Bone Joint Surg Am. 2009;91:192–197. doi: 10.2106/JBJS.G.01367. [DOI] [PubMed] [Google Scholar]
- 3.Matsuda D.K. Acute iatrogenic dislocation following hip impingement arthroscopic surgery. Arthroscopy. 2009;25:400–404. doi: 10.1016/j.arthro.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 4.Dierckman B.D., Guanche C.A. Anterior hip capsuloligamentous reconstruction for recurrent instability after hip arthroscopy. Am J Orthop. 2014;43:E319–E323. [PubMed] [Google Scholar]
- 5.Benali Y., Katthagen B.D. Hip subluxation as a complication of arthroscopic debridement. Arthroscopy. 2009;25:405–407. doi: 10.1016/j.arthro.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 6.Sansone M., Ahldén M., Jónasson P., Swärd L., Eriksson T., Karlsson J. Total dislocation of the hip joint after arthroscopy and ileopsoas tenotomy. Knee Surg Sports Traumatol Arthrosc. 2013;21:420–423. doi: 10.1007/s00167-012-2300-3. [DOI] [PubMed] [Google Scholar]
- 7.Mei-Dan O., McConkey M.O., Brick M. Catastrophic failure of hip arthroscopy due to iatrogenic instability: Can partial division of the ligamentum teres and iliofemoral ligament cause subluxation? Arthroscopy. 2012;28:440–445. doi: 10.1016/j.arthro.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 8.Shu B., Safran M.R. Hip instability: Anatomic and clinical considerations of traumatic and atraumatic instability. Clin Sports Med. 2011;30:349–367. doi: 10.1016/j.csm.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 9.Ferguson S.J., Bryant J.T., Ganz R., Ito K. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech. 2003;36:171–178. doi: 10.1016/s0021-9290(02)00365-2. [DOI] [PubMed] [Google Scholar]
- 10.McCormick F., Slikker W., Harris J.D. Evidence of capsular defect following hip arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2014;22:902–905. doi: 10.1007/s00167-013-2591-z. [DOI] [PubMed] [Google Scholar]
- 11.Beighton P. Hypermobility scoring. Br J Rheumatol. 1988;27:163. doi: 10.1093/rheumatology/27.2.163. [DOI] [PubMed] [Google Scholar]
- 12.Sampson T.G. Complications of hip arthroscopy. Clin Sports Med. 2001;20:831–835. doi: 10.1016/s0278-5919(05)70288-x. [DOI] [PubMed] [Google Scholar]
- 13.Scher D.L., Belmont P.J., Owens B.D. Case report: Osteonecrosis of the femoral head after hip arthroscopy. Clin Orthop Relat Res. 2010;468:3121–3125. doi: 10.1007/s11999-010-1256-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sener N., Gogus A., Akman S., Hamzaoglu A. Avascular necrosis of the femoral head after hip arthroscopy. Hip Int. 2011;21:623–626. doi: 10.5301/HIP.2011.8693. [DOI] [PubMed] [Google Scholar]
- 15.LaPrade R.F. Arthroscopic evaluation of the lateral compartment of knees with grade 3 posterolateral knee complex injuries. Am J Sports Med. 1997;25:596–602. doi: 10.1177/036354659702500502. [DOI] [PubMed] [Google Scholar]
- 16.Pagnani M.J., Warren R.F. Arthroscopic shoulder stabilization. Oper Tech Sports Med. 1993;1:276–284. [Google Scholar]
- 17.Pagnani M.J., Warren R.F., Altchek D.W., Wickiewicz T.L., Anderson A.F. Arthroscopic shoulder stabilization using transglenoid sutures. A four-year minimum followup. Am J Sports Med. 1996;24:459–467. doi: 10.1177/036354659602400409. [DOI] [PubMed] [Google Scholar]
- 18.Mardones R.M., Gonzalez C., Chen Q., Zobitz M., Kaufman K.R., Trousdale R.T. Surgical treatment of femoroacetabular impingement: Evaluation of the effect of the size of the resection. J Bone Joint Surg Am. 2005;87:273–279. doi: 10.2106/JBJS.D.01793. [DOI] [PubMed] [Google Scholar]
- 19.Ayeni O.R., Bedi A., Lorich D.G., Kelly B.T. Femoral neck fracture after arthroscopic management of femoroacetabular impingement: A case report. J Bone Joint Surg Am. 2011;93:e47. doi: 10.2106/JBJS.J.00792. [DOI] [PubMed] [Google Scholar]
- 20.Domb B.G., Philippon M.J., Giordano B.D. Arthroscopic capsulotomy, capsular repair, and capsular plication of the hip: Relation to atraumatic instability. Arthroscopy. 2013;29:162–173. doi: 10.1016/j.arthro.2012.04.057. [DOI] [PubMed] [Google Scholar]
- 21.Frank R.M., Lee S., Bush-Joseph C.A., Kelly B.T., Salata M.J., Nho S.J. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: A comparative matched-pair analysis. Am J Sports Med. 2014;42:2634–2642. doi: 10.1177/0363546514548017. [DOI] [PubMed] [Google Scholar]
- 22.Fujishiro T., Nishikawa T., Takikawa S., Saegusa Y., Yoshiya S., Kurosaka M. Reconstruction of the iliofemoral ligament with an artificial ligament for recurrent anterior dislocation of total hip arthroplasty. J Arthroplasty. 2003;18:524–527. doi: 10.1016/s0883-5403(03)00073-1. [DOI] [PubMed] [Google Scholar]
- 23.Elkins J.M., Stroud N.J., Rudert M.J. The capsule’s contribution to total hip construct stability—A finite element analysis. J Orthop Res. 2011;29:1642–1648. doi: 10.1002/jor.21435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bayne C.O., Stanley R., Simon P. Effect of capsulotomy on hip stability-a consideration during hip arthroscopy. Am J Orthop. 2014;43:160–165. [PubMed] [Google Scholar]
- 25.Hewitt J., Guilak F., Glisson R. Regional material properties of the human hip joint capsule ligaments. J Orthop Res. 2001;19:359–364. doi: 10.1016/S0736-0266(00)00035-8. [DOI] [PubMed] [Google Scholar]
- 26.Martin H.D., Savage A., Braly B.A., Palmer I.J., Beall D.P., Kelly B. The function of the hip capsular ligaments: A quantitative report. Arthroscopy. 2008;24:188–195. doi: 10.1016/j.arthro.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 27.Ito H., Song Y., Lindsey D.P., Safran M.R., Giori N.J. The proximal hip joint capsule and the zona orbicularis contribute to hip joint stability in distraction. J Orthop Res. 2009;27:989–995. doi: 10.1002/jor.20852. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Technique for examination under anesthesia, diagnostic arthroscopy, and capsular plication for iatrogenic hip microinstability. Arthroscopy is shown in a left hip from an anterolateral viewing portal with the patient in the supine position. One should note that the portion of the video showing the examination under anesthesia was taken from the case of a different patient and that the isolated photograph of joint space widening under fluoroscopy corresponds to a right hip.