Abstract
Context:
Alopecia areata (AA), an autoimmune disorder, can affect any hair-bearing area. No treatment so far has produced a consistent response. Narrow band ultraviolet B (NBUVB) has not been studied in its management.
Aims:
Comparative evaluation of intralesional triamcinolone acetonide injection, NBUVB, and their combination in AA.
Materials and Methods:
Forty patients (28 males and 12 females) with at least three patches of hair loss were enrolled after obtaining written informed consent. Patches were subdivided as follows: Patch 1 was injected with triamcinolone acetonide 2.5 mg/ml (total of three injections) at 3 weeks interval. Patch 2 - NBUVB was given twice a week for a total of 12 weeks. Patch 3 - combination of injection and NBUVB. Therapeutic response was recorded as regrowth of terminal hair (G0 to G4).
Statistical Analysis Used:
Chi-square test. P < 5% was considered significant.
Results:
At the end of treatment and follow-up, that is, at week 12, more than 50% of hair regrowth was evident in 27 (67.5%) patients with intralesional steroid; 7 (17.5%) with NBUVB; and 25 (62.5%) patients with their combination. This difference in the clinical response was statistically significant.
Conclusions:
Intralesional steroid is more effective than NBUVB and their combination is not synergistic in terms of the clinical response in AA.
Keywords: Alopecia areata, narrow band ultraviolet B, triamcinolone acetonide
INTRODUCTION
Hair is extremely important cosmetically, emotionally, and psychologically. Alopecia areata (AA) is a recurrent, chronic, autoimmune, nonscarring type of hair loss that can affect any hair-bearing area occurring in genetically predisposed individuals. Intralesional corticosteroids are extensively used in the management of AA.[1] They are considered the first-line treatment in localized alopecia involving <50% of the scalp. However, intralesional steroid injections are associated with a variety of side effects and are also painful. As a result, the search for alternatives to steroids has been felt as the need of the hour. Impressed by the results of psoralen photochemotherapy in AA, we thought of trying narrow band ultraviolet B (NBUVB) in AA. An extensive review of the literature, however, revealed only one study done by Bayramgürler et al. in 2011. In this study, 8/25 (32%) patients received monthly intramuscular corticosteroid injections. Four (22.2%) patients in extensive patchy hair loss group and 2 (20%) patients in entire scalp hair loss group achieved an excellent response. Four of these six patients who achieved excellent response also received monthly intramuscular corticosteroid injections. NBUVB was found to have excellent treatment responses in 20% patients with severe AA, most of whom were also treated with systemic corticosteroids.[2] However, this study did not distinguish as to what was the cause of therapeutic effect: Steroids or NBUVB. Hence, this study was undertaken to do a comparative evaluation of intralesional triamcinolone acetonide injection, NBUVB, as well as their combination.
AIMS AND OBJECTIVES
To evaluate the therapeutic efficacy of intralesional triamcinolone acetonide injection 2.5 mg/ml in AA
To assess the therapeutic efficacy of NBUVB in AA
To assess the therapeutic efficacy of combined intralesional triamcinolone acetonide injection 2.5 mg/ml and NBUVB in AA
Comparative evaluation of intralesional triamcinolone acetonide injection 2.5 mg/ml, NBUVB, and their combination in AA.
MATERIALS AND METHODS
Study area
Department of Dermatology, Venereology, and Leprology, G. G. S. Medical College and Hospital, Faridkot.
Study population
A total of 40 patients of AA with at least three patches were enrolled from Outpatient Department of Dermatology, Venereology, and Leprology at G. G. S. Medical College and Hospital, Faridkot.
Diagnosis
The diagnosis was based upon the clinical examination, hair microscopy for exclamation mark hair, and potassium hydroxide examination to rule out fungal infection.
Inclusion criteria
Patients having a minimum of three patches of AA
Patients of both genders between the ages of 15-50 years.
Exclusion criteria
Children aged <15 years
Patients with cicatricial alopecia
Patients with alopecia universalis
Patients with history of photosensitivity
Patients with lupus erythematosus
Patients with past or present history of skin cancer
Patients taking photosensitizing/phototoxic drugs.
A written informed consent was taken from each patient before starting the study. A detailed history and general physical examination and local examination were conducted in each case and were recorded on a prescribed proforma.
Each patient was subjected to the following investigations at the time of reporting:
Hemoglobin
Total leucocyte count, differential leucocyte count
Peripheral blood film
Fasting blood sugar
Renal function tests
Liver function tests
Total and differential serum proteins
Serum electrolytes and serum calcium
Hair microscopy for exclamation mark hairs
Potassium hydroxide mounts to rule out fungal infection
Thyroid stimulating hormone, T3, T4
Anti-nuclear antibody
Venereal Disease Research Laboratory
Human immunodeficiency virus enzyme-linked immunosorbent assay.
Equipment
NBUVB chamber
UV blocking goggles
Black gown and sheets to protect the nondiseased parts of body
Injection triamcinolone acetonide 2.5 mg/ml
Insulin syringe
Sterile normal saline for a dilution of steroid injection.
Procedure
Patches of AA were subdivided as follows:
Patch 1: Patch was injected with triamcinolone acetonide 2.5 mg/ml. Normal saline was used to dilute triamcinolone acetonide which is commercially available as 10 mg/ml. After cleaning the area with povidone iodine solution, insulin syringe was used to give multiple injections of 0.1 ml each, approximately 1 cm apart. The solution was injected in or just beneath the dermis and a maximum of 3 ml in one visit were used
Patch 2: Patch was exposed to NBUVB with initial dose of 300 mJ/cm2 with increments of 10% at every visit, till minimal erythema developed
Patch 3: Patch was first injected with triamcinolone acetonide as described above followed by exposure to NBUVB with dose as mentioned above.
Schedule of treatment
Patch 1: Injection triamcinolone acetonide 2.5 mg/ml was given at day 0, week 3, and week 6. After that, follow-ups were done fortnightly for the next 6 weeks, completing a total period of 12 weeks
Patch 2: NBUVB exposure was done twice a week from day 0 to week 6. After that, follow-ups were done fortnightly for next 6 weeks, completing a total period of 12 weeks. During follow-ups, NBUVB exposures were continued if no hair regrowth was observed
Patch 3: Day 0 - injection triamcinolone acetonide 2.5 mg/ml was given into the patch followed by exposure to NBUVB twice weekly. At week 3 - injection triamcinolone acetonide was given into the patch followed by continued NBUVB exposure twice weekly. At week 6 - injection triamcinolone acetonide 2.5 mg/ml was given. After that, follow-ups were done fortnightly, completing a total period of 12 weeks.
All the selected patches were assessed clinically as well as photographically at the baseline, at each visit, and at each follow-up visit.
Patient's response to the treatment was graded as follows:
G0 no growth
G1 <25% regrowth (poor)
G2 <50% regrowth (fair)
G3 <75% regrowth (good)
G4 complete regrowth (excellent).
Results were analyzed photographically as well as statistically (using Chi-square test) after a follow-up period of 12 weeks.
RESULTS AND OBSERVATIONS
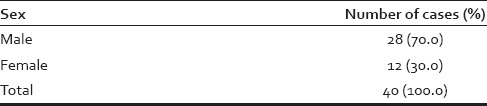
The maximum number of 14 patients was in the age group of 20-29 years and the minimum number of four subjects was in 40-49 years age group which shows decreasing incidence with age [Table 1]. Males outnumbered the females in this study [Table 2].
Table 1.
Age-wise distribution of cases
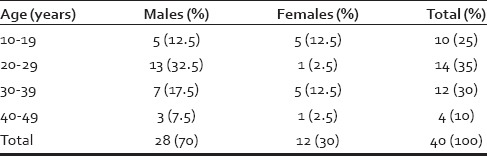
Table 2.
Sex-wise distribution of cases
Patients from the urban area were more than the rural ones [Table 3]. The maximum number of patients was farmers (35%) and the minimum was those in government service (5%) [Table 4]. The most common site affected was the scalp (67.5%) [Table 5]. Most of the patients had <1 year of history [Table 6]. The family history of AA was positive in one patient [Table 7]. Sixty five percentage of the patients had three lesions while the rest of the cases had 4-8 patches [Table 8]. Nail changes were seen in 42.5% of cases in this study [Table 9].
Table 3.
Location-wise distribution of cases
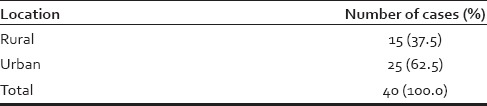
Table 4.
Occupation-wise distribution of cases
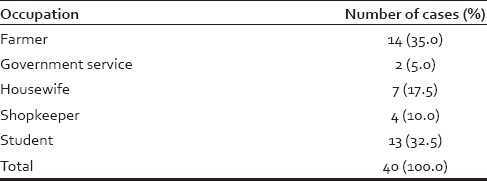
Table 5.
Distribution according to site affected
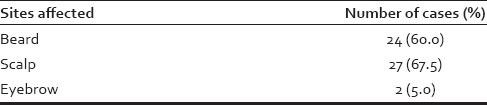
Table 6.
Distribution according to duration of disease

Table 7.
Distribution according to family history

Table 8.
Distribution according to the number of patches
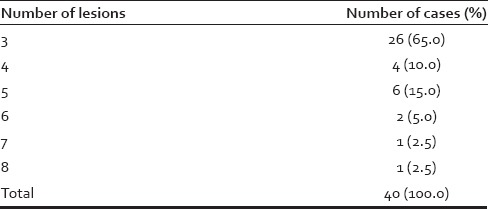
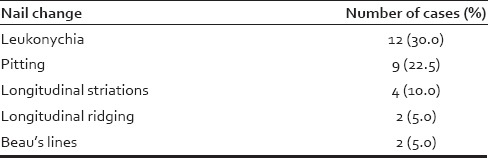
Table 9.
Nail changes in alopecia areata
Clinical response in terms of hair regrowth and re-pigmentation of hair is depicted in Tables 10–15 and Graphs 1–6.
Table 10.
Comparison of hair growth at week 4

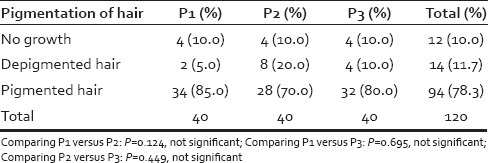
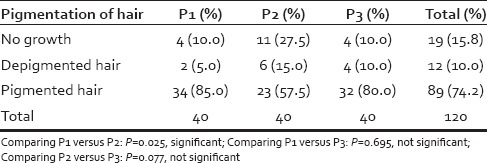
Table 15.
Comparison of hair pigmentation at week 12 in three patches
Graph 1.
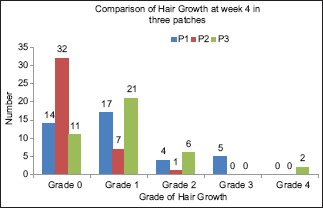
Comparison of Hair Growth at week 4 in three patches
Graph 6.
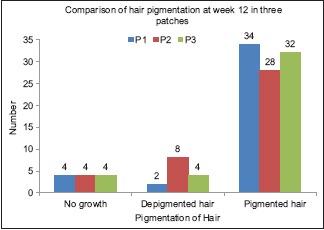
Comparison of hair pigmentation at week 12 in three patches
Table 11.
Comparison of hair growth at week 8
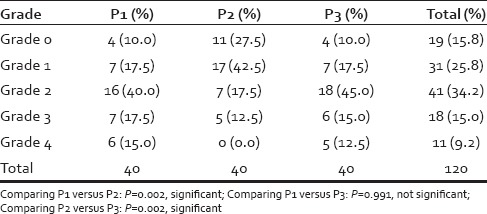
Table 12.
Comparison of hair growth at week 12
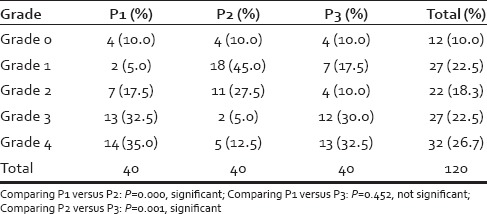
Table 13.
Comparison of hair pigmentation at week 4 in three patches
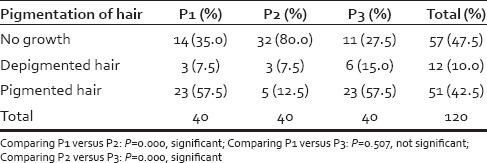
Table 14.
Comparison of hair pigmentation at week 8 in three patches
Graph 2.
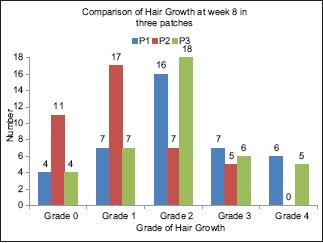
Comparison of Hair Growth at week 8 in three patches
Graph 3.
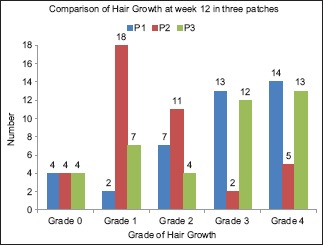
Comparison of Hair Growth at week 12 in three patches
Graph 4.
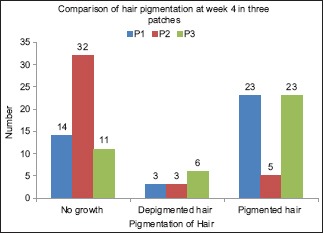
Comparison of hair pigmentation at week 4 in three patches
Graph 5.
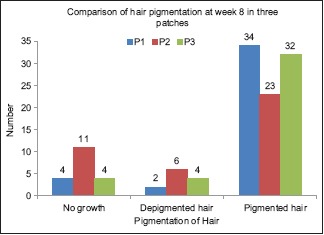
Comparison of hair pigmentation at week 8 in three patches
DISCUSSION
AA was previously known as pelade or area celsi. The disease was first described by Cornelius Celsus in 30 AD. The term AA was first used by Sauvages in 1760.
Age distribution of alopecia areata
In this study of 40 patients with age ranging from 15 to 50 years, majority of patients was in the age group of 20-29 years (35%), closely followed by 12 (30%) in the age group of 30-39 years, and 10 (25%) aged 10-19 years. Thus, a total of 90% occurred below the age of 40 years. This observation was similar to another study which states that 85.5% of the Asian patients with AA have disease onset before 40 years of age.[3]
Sex wise distribution of alopecia areata
In the present study comprising of 40 patients, there were 28 (70%) males and 12 (30%) females. Some studies show a significant male preponderance in the adult age group, although others identify contrasting results.[4,5]
Location
Patients from urban areas outnumbered the rural ones in this study. Of 40 cases, 25 (62.5%) were from urban area while 15 (37.5%) were rural.
Occupation
Of 40 subjects, 14 (35%) were farmers followed in decreasing frequency by students 13 (32.5%), housewives 7 (17.5%), shopkeepers 4 (10%), and the least common were those in government service 2 (5%).
Site of involvement in alopecia areata
The most common site affected was scalp in 27 (67.5%) while beard was involved in 24 (60%) cases. The least affected site was eyebrows in only 2 (5%) patients.
Duration
Duration of the disease ranged from 1 month to 8 years. Maximum number of the patients, that is, 26 (65%) had <1 year of history, 11 (27.5%) had duration between 1 and 5 years, and 3 (7.5%) had more than 5 years of the problem of hair loss.
Past history of alopecia areata
Of 40 patients, 12 (30%) had a past history of AA. Eight patients had a single episode, two had two episodes, and 1 patient each had three and multiple episodes, respectively.
Family history
One (2.5%) out of 40 patients had a positive family history of the disease in this study which differs from other studies having a significant family history.
Various other studies show that family incidence of AA varies from 10 to 20%.[6]
Number of lesions of alopecia areata
The majority of patients 26 (65%) had three lesions, 4 (10%) had four lesions while the remaining had five or more lesions. Small patches closely arranged in the reticulate pattern have been found to carry a poorer prognosis.[7]
Nail changes
Nail changes were evident in 17 (42.5%) of the total 40 patients in the form of leukonychia, pitting, longitudinal striations, longitudinal ridging, and beau's lines.
Gandhi et al. observed pitting to be the most common nail finding in patients with alopecia areata, but leukonychia was the most frequent nail change in this study.[8]
Response to treatment
At week 4, 5 (12.5%) achieved Grade 3 response and 4 (10%) had Grade 2 hair regrowth among P1 group. In P2 treated with NBUVB, only 1 (2.5%) could show Grade 2 response. In P3, 6 (15%) showed Grade 2 hair regrowth.
At week 8, more than 50% hair growth was seen in 13 (32.5%) in P1, 5 (12.5%) in P2, and 11 (27.5%) in P3. Again the response was statistically significant.
At the end of treatment and follow-up, that is, at week 12, more than 50% response was evident in 27 (67.5%) with 14 (35%) showing Grade 4 regrowth in P1 group. Among P2 patches treated with NBUVB, only 7 (17.5%) showed >50% response with 5 (12.5%) having Grade 4 hair regrowth. In P3, 25 (62.5%) had >50% hair gain with 13 (32.5%) showing Grade 4 response.
At week 4, 23 (57.5%) in P1, 5 (12.5%) in P2, and 23 (57.5%) in P3 showed growth of pigmented hair. De-pigmented hair were seen in 3 (7.5%) in P1, 3 (7.5%) in P2, and 6 (15%) in P3. This difference in the clinical response was statistically significant (P = 0.000).
Assessment at week 8 revealed 34 (85%) in P1 showing pigmented hair while corresponding values for P2 and P3 were 23 (57.5%) and 32 (80%), respectively (P = 0.050).
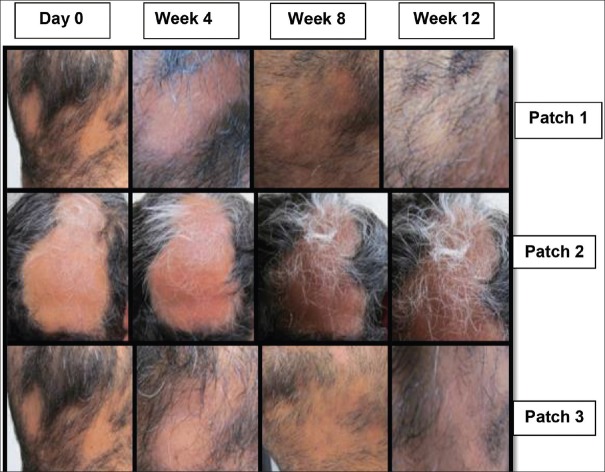
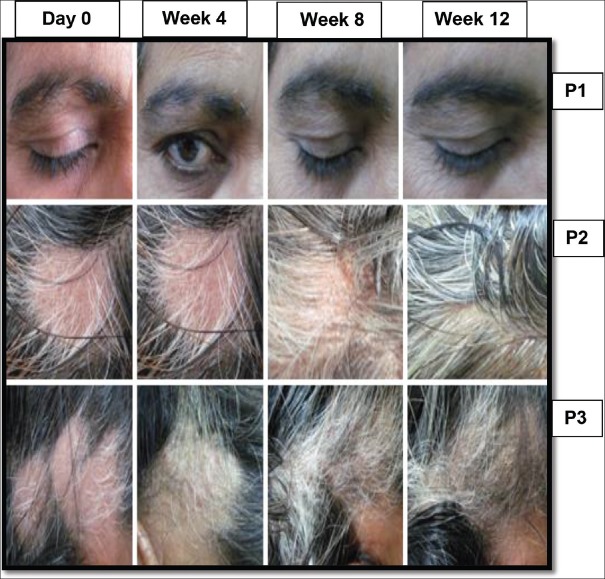
At week 10, the response in the form of pigmentation of hair among the three groups became insignificant (P = 0.331) with 34 (85%) in P1, 28 (70%) in P2, and 32 (80%) in P3 showing growth of pigmented hair. These effects were maintained at week 12 as well. The follow-ups of patients are depicted in [Figures 1 and 2].
Figure 1.
Response to intralesional triamcinolone acetonide injection (Patch 1), narrow band UVB (Patch 2), and their combination (Patch 3) at week 4, 8, and 12
Figure 2.
Response to intralesional triamcinolone acetonide injection (P1), narrow band UVB (P2), and their combination (P3) at week 4, 8, and 12
Review of literature regarding the use of NBUVB in AA revealed only one retrospective study done by Bayramgürler et al. which showed an excellent response in 20% of patients, most of whom were also treated with systemic corticosteroids. Hence, this study did not answer as to whether steroids or NBUVB led to clinical response.[2]
In this study, good clinical response to NBUVB in the form of more than 50% hair regrowth was seen in only 17.5% of cases which is lower than the treatment effect seen in the study done by Bayramgürler et al. This could be attributed to the concurrent use of systemic corticosteroids in the study done by Bayramgüürler et al.
Good hair growth was evident in 67.5% of patients treated with a total of three intralesional steroid injections given at 3 weekly intervals in this study which was close to what was observed by Abell and Munro.[9]
The side effects associated with NBUVB were minimal with minority of patients complaining of transient itching or redness in the treated area. Otherwise, it was well tolerated. However, intralesional triamcinolone acetonide injection was associated with significant side effects such as pain, minor bleeding, folliculitis, and transient atrophy.
CONCLUSIONS
To conclude, intralesional steroids were more effective than NBUVB and their combination was not synergistic in terms of the clinical response. There was no statistical difference in terms of pigmented hair regrowth in either of the treatment modalities. Minimal to no side effects were reported with NBUVB while intralesional steroid injection was associated with side effects such as pain, minor bleeding, folliculitis, and transient atrophy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
REFERENCES
- 1.Kumaresan M. Intralesional steroids for alopecia areata. Int J Trichology. 2010;2:63–5. doi: 10.4103/0974-7753.66920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bayramgürler D, Demirsoy EO, Aktürk AS, Kiran R. Narrowband ultraviolet B phototherapy for alopecia areata. Photodermatol Photoimmunol Photomed. 2011;27:325–7. doi: 10.1111/j.1600-0781.2011.00612.x. [DOI] [PubMed] [Google Scholar]
- 3.Tan E, Tay YK, Goh CL, Chin Giam Y. The pattern and profile of alopecia areata in Singapore - A study of 219 Asians. Int J Dermatol. 2002;41:748–53. doi: 10.1046/j.1365-4362.2002.01357.x. [DOI] [PubMed] [Google Scholar]
- 4.Kyriakis KP, Paltatzidou K, Kosma E, Sofouri E, Tadros A, Rachioti E. Alopecia areata prevalence by gender and age. J Eur Acad Dermatol Venereol. 2009;23:572–3. doi: 10.1111/j.1468-3083.2008.02956.x. [DOI] [PubMed] [Google Scholar]
- 5.Kavak A, Yesildal N, Parlak AH, Gökdemir G, Aydogan I, Anul H, et al. Alopecia areata in Turkey: Demographic and clinical features. J Eur Acad Dermatol Venereol. 2008;22:977–81. doi: 10.1111/j.1468-3083.2008.02699.x. [DOI] [PubMed] [Google Scholar]
- 6.Gip L, Lodin A, Molin L. Alopecia areata. A follow-up investigation of outpatient material. Acta Derm Venereol. 1969;49:180–8. [PubMed] [Google Scholar]
- 7.Macalpine I. Is alopecia areata psychosomatic. A psychiatric study? Br J Dermatol. 1958;70:117–31. doi: 10.1111/j.1365-2133.1958.tb13304.x. [DOI] [PubMed] [Google Scholar]
- 8.Gandhi V, Baruah MC, Bhattacharaya SN. Nail changes in alopecia areata: Incidence and pattern. Indian J Dermatol Venereol Leprol. 2003;69:114–5. [PubMed] [Google Scholar]
- 9.Abell E, Munro DD. Intralesional treatment of alopecia areata with triamcinolone acetonide by jet injector. Br J Dermatol. 1973;88:55–9. doi: 10.1111/j.1365-2133.1973.tb06672.x. [DOI] [PubMed] [Google Scholar]