Abstract
Osteochondritis dissecans (OCD) of the femoral head is not a common source of hip pain. Hip arthroscopy is becoming a more frequent indication for intra-articular pathologies of the hip. Osteochondral autologous transplantation is a promising technique that theoretically can reconstruct osteochondral lesions of the femoral head. We describe our technique for arthroscopic antegrade osteochondral autologous transplantation for the treatment of OCD of the femoral head. The advantages of this technique include that it is a less invasive method with the ability to assess and treat intra-articular pathologies associated with OCD of the femoral head at same time. Case series and outcomes after this technique are not currently reported in the literature; however, it could be a less invasive method and provide favorable clinical outcomes for patients with OCD lesions of the femoral head.
Osteochondritis dissecans (OCD) of the femoral head has been characterized as the separation of osteochondral lesions from the subchondral bone of the femoral head.1, 2 OCD lesions of the femoral head are uncommon, but they can cause pain and mechanical symptoms such as catching, locking, and progressive cartilage damage. There are limited treatment options.1 If the patient is asymptomatic or has open physes, conservative treatment options should first be considered.3 However, few cases will heal spontaneously, without surgery.
The vast majority of patients with symptomatic OCD lesions will require surgical management. Surgical removal of the free OCD fragment is usually considered when the fragment causes locking or catching. However, fragment removal can cause an increased risk of joint incongruity predisposing toward osteoarthritis. Thus, ideally, the aim of surgical intervention should be to restore the articular surface congruity and preserve normal joint kinematics.
To restore articular surface congruity, open surgical procedures generally have been used. Numerous procedures involving fragment fixation with bone pegs, osteochondral autograft transplantation (OAT), fresh-stored OAT allograft, and arthroplasty have been reported.4, 5 These surgical treatments usually require surgical dislocation approaches, which are more invasive. Hip arthroscopy is preferred over open surgery. Arthroscopic internal fixation of an OCD lesion in the acetabulum was first described by Matsuda and Safran.6 They reported having obtained a favorable clinical outcome with metal headless compression screws. Arthroscopic OAT would be more advantageous if an OCD lesion is irreparable. We show that using OAT for the arthroscopic management of an OCD lesion of the femoral head combined with femoroacetabular impingement is feasible (Video 1, Fig 1).
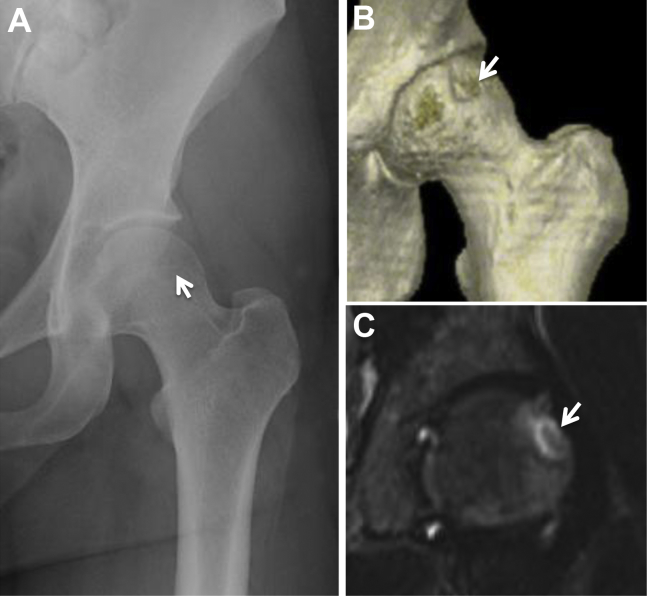
Fig 1.
Preoperative radiographs of a 37-year-old female patient who presented to our clinic with a 2-year history of insidious-onset, increasingly intense left hip pain. (A) Pelvic anteroposterior view showing a pistol-grip deformity and the center-edge angle (right, 32°; left, 25°). A round radiolucent lesion (arrow) suggests an osteochondritis dissecans (OCD) lesion at the anterosuperior portion of the left femoral head. (B) Preoperative 3-dimensional computed tomography also showing an OCD lesion (arrow) at the anterosuperior site of the femoral head. (C) Coronal magnetic resonance imaging view (short inversion time inversion-recovery sequence) showing a high-intensity round lesion (arrow) at the anterosuperior portion of the femoral head 1 month before surgery.
Surgical Technique
The patient was placed in a modified supine position on the traction table (Hip Positioning System; Smith & Nephew Endoscopy, Andover MA) under general and epidural anesthesia, with a padded perineal post and countertraction on the other leg (abduction). The involved hip was internally rotated and slightly flexed.
First, arthroscopic evaluation to assess for intra-articular lesions, including labral tearing and associated cartilage damage, was performed through an anterolateral portal (ALP) and midanterior portal. Capsule release using a beaver knife (BD, Franklin Lakes, NJ) was performed to improve accessibility of the arthroscope and surgical instruments. Partial tearing at the anterior site of the acetabular labrum (9:30 clock-face position) and associated cartilage delamination were observed, classified as Multicenter Arthroscopy of the Hip Outcomes Research Network grade I. Thermoplasty was carried out with a radiofrequency probe (VAPR; DePuy Mitek, Raynham, MA).
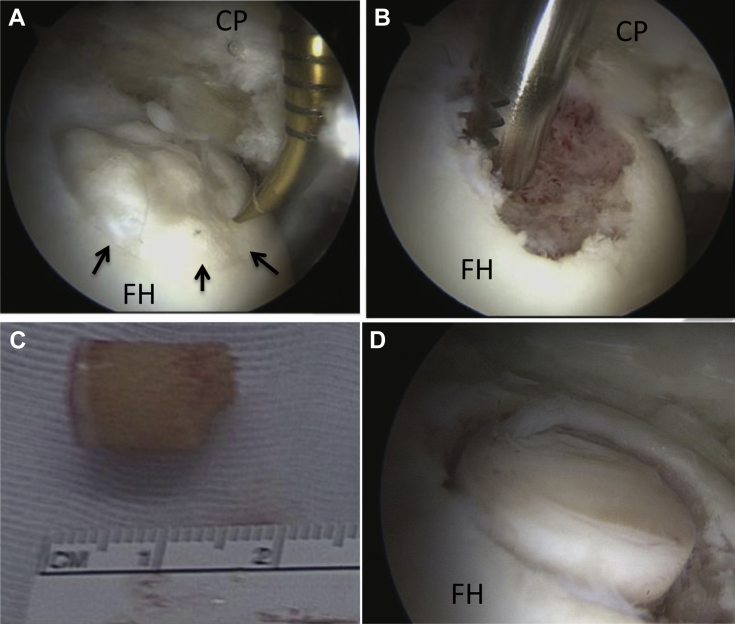
The OCD lesion was observed at the anterosuperior portion of the femoral head (Fig 2A). A proximal midanterior portal (PMAP) was established to access the OCD lesion, with the hip at 10° of extension. The condition of the cartilage was evaluated with a probe, and it was determined that it could not undergo refixation (Fig 2A).
Fig 2.
Surgical findings and technique. (A) An osteochondritis dissecans (OCD) lesion (arrows), classified as International Cartilage Repair Society grade III, was observed at the anterosuperior femoral head, with the arthroscope viewing from the anterolateral portal (ALP). An awl and probe through the proximal midanterior portal (PMAP) were used to evaluate the OCD lesion. (B) The degenerative OCD lesion was resected with a shaver (Dyonics Bonecutter Platinum, 4.5 mm), viewing from the ALP. (C) A cylindrical autologous osteochondral graft (8.5 mm in diameter) was harvested arthroscopically from the ipsilateral knee joint. (D) A drill guide was introduced through the PMAP, viewing from the ALP. The subchondral bone was drilled to a depth of 14 mm. The dilator was inserted into the drill guide and tapped to the desired depth. The autologous osteochondral graft was tamped into the lesion until the articular surface was flush with the host joint surface. (CP, capsule; FH, femoral head.)
A decision was made that osteochondral transplantation was necessary. Viewing from the ALP, the surgeon (S.U.) resected the degenerative cartilage lesion using a shaver (Dyonics Bonecutter Platinum, 4.5 mm; Smith & Nephew Endoscopy) and a curette (Relevator; DePuy Mitek) through the PMAP (Fig 2B). The OAT technique was performed using the Mosaicplasty autologous osteochondral grafting system (Smith & Nephew Endoscopy). The diameter of the lesion was determined to be 8.5 mm by using a chisel (Smith & Nephew Endoscopy) perpendicular to the articular surface. A cylindrical autologous osteochondral graft (8.5 mm in diameter) was harvested arthroscopically from the ipsilateral knee joint (Fig 2C). The superolateral aspect of the intercondylar notch was used as the donor site. The chisel was introduced through the superolateral portal. It was driven into the bone to a depth of 12 mm. The harvester, containing the graft, was then removed by twisting the T-handle.
At the recipient site, a drill guide was inserted at a 90° angle to the recipient site, through the PMAP, while the surgeon was viewing from an arthroscope located in the ALP. The subchondral bone was drilled to a depth of 14 mm. The dilator was inserted into the drill guide and tapped to the desired depth. The osteochondral autograft was placed over the lesion and tamped into position until the articular surface was flush with the host joint surface (Fig 2D).
After the central compartment procedure, traction was released to assess the peripheral compartment. A cam lesion that had diffuse cartilage damage (International Cartilage Repair Society grade II) was seen at the femoral head-neck junction. Arthroscopic dynamic assessment confirmed cam impingement.7 Thus cam osteoplasty was carried out with a motorized round burr.
Lastly, capsular closure was performed on the hip at 40° of flexion, through the midanterior portal, as described previously8 (Table 1). A total of 2 side-to-side stitches were placed to close the capsule.
Table 1.
Tips/Pearls and Pitfalls
| Tips and pearls |
| An interportal capsular cut is made from the 3- to 9-o’clock position to improve accessibility. |
| Optimum visualization can be obtained by using a shaver and radiofrequency probe. |
| Hip traction and 10° of extension on the traction table are used to improve access. |
| The proximal midanterior portal is useful to access OCD lesions. |
| Labral tearing must be repaired. |
| The capsule must be closed to restore the stability of the joint. |
| Pitfalls |
| Use of the anterior portal entails a risk of femoral lateral cutaneous nerve palsy. |
| The surgeon should ensure that the traction time is less than 90 min to avoid traction-related complications. |
OCD, osteochondritis dissecans.
Postoperative Rehabilitation
The patient should be placed in a brace (Philippon brace; Bledsoe, Dallas, TX) for 3 weeks to protect the hip and limit abduction and rotation. Gentle passive range-of-motion exercise is initiated during the first week, under the supervision of a physiotherapist. The patient remains non–weight bearing during the first 4 weeks. Active hip flexion is limited during phase 1 (the first 4 weeks) to minimize the risk of hip flexor inflammation. From week 4 to week 5, weight bearing is gradually increased, and full weight bearing is allowed at 8 weeks after surgery. The patient will usually show improvements in mobility, stability, and proprioception. The patient can start swimming and using a stationary bicycle with resistance at 3 months after surgery. Endurance strengthening should be commenced at 16 weeks after surgery—only after range of motion is maximized and good stability in gait and movement is achieved. Throughout this phase, no low-impact aerobic conditioning should be performed.
Discussion
We have described our arthroscopic technique for antegrade OAT for the treatment of OCD lesions of the femoral head. It is possible to achieve a good clinical result with this procedure (Fig 3).
Fig 3.
Postoperative results. (A) Anteroposterior view showing graft incorporation. (B) Modified Dunn view showing slight flattening of femoral head. (C, D) Magnetic resonance T2* radial views showing good integration of graft and homogeneous intensity.
The aim of treating OCD lesions of the femoral head should be the restoration of joint congruity and healthy cartilage of the femoral head. Recently, osteochondral transplantation procedures (mosaicplasty) have been reported for the treatment of OCD lesions as well as osteonecrosis of the femoral head.9, 10, 11, 12
Nam et al.11 reported on 2 cases that underwent OATS combined with osteochondral fragment fixation after traumatic anterior dislocation of the hip joints. They showed good clinical outcomes and graft incorporation using magnetic resonance imaging (MRI). Girard et al.10 described the surgical technique and clinical outcomes after OAT for the treatment of 10 patients with OCD lesions of the femoral head. They showed excellent well-healed incorporation of the autologous graft on all radiographs.
In their case report, Emre et al.9 showed a good, pain-free outcome at 3 years after surgery. Gagala et al.12 also reported good results after fragment fixation combined with OAT for the treatment of osteochondral defects after posterior fracture-dislocation of the hip joint. They proposed good clinical outcomes and graft congruity as investigated by MRI.
The aforementioned case reports described requiring an open surgical approach including surgical dislocation with greater trochanteric osteotomy to assess the osteochondral lesions. Open approaches can have higher rates of complications, such as nonunion of the greater trochanter.
Arthroscopic OAT procedures for treating OCD lesions of the femoral head are promising. Cetinkaya et al.13 reported an arthroscopic retrograde OAT procedure for treating OCD of the central portion of the femoral head. The patient showed good graft incorporation with proper joint resurfacing and had a favorable clinical outcome. Moreover, there are several reports using arthroscopic OAT for treating OCD lesions of the knee joint. Hangody et al.,14 using open OAT procedures, reported good or excellent outcomes in 92% of patients with OCD lesions of the medial condyle and 81% of patients with OCD lesions of the patellofemoral joint. They also reported a series of 21 cases that underwent arthroscopic OAT procedures in the knee. The modified Hospital for Special Surgery score improved from 62.18 preoperatively to 94.23 at 1-year follow-up. Of the 21 cases, 3 had postoperative complications involving a painful intra-articular hematoma. Marcacci et al.15 prospectively evaluated the clinical outcomes after arthroscopic OAT for treating cartilage defects in 37 patient knees. They showed that 29 of 37 patients (73%) had good or excellent results and 27 patients were able to return to sports at the same level.
Magnetic Resonance Observation of Cartilage Repair Tissue (MOCART) scoring system is a point-scoring system designed to systematically record the constitution of the osteochondral fragment fixation area and surrounding tissue. It has been shown to be reliable and reproducible when applied to various surgical cartilage repair procedures.16 Tetta et al.17 evaluated long-term MRI features (median follow-up, 113 months) using the MOCART scoring system and found a positive correlation with clinical outcome after arthroscopic OAT approaches to the knee. MRI showed a good survival rate for cartilage restoration in 62.5% of patients. The MOCART score was significantly correlated with subjective and objective International Knee Documentation Committee scores.
Arthroscopic OAT to treat OCD lesions of the femoral head has several advantages and some disadvantages (Table 2). The advantages include that this procedure is minimally invasive and has the potential for early rehabilitation, as well as a quicker recovery. Concurrent lesions can be readily identified and treated. Moreover, surgeons are able to evaluate impingement issues and other intra-articular pathologies, such as acetabular labral tears, ligamentous tearing, and cartilage delamination (as in our patient), because OCD of the femoral head is often associated with other pathologies.18 However, a considerable disadvantage is that this procedure requires meticulous technique and is technically demanding, but it is possible. The accessibility of this arthroscopic approach is limited only to the anterior aspect of the femoral head. Surgeons will still need to access the central area and posterior area with an open approach or an arthroscopic retrograde OAT procedure. In addition, there is a possibility of donor-site morbidity, such as donor-site pain in the knee joint.19, 20
Table 2.
Advantages and Disadvantages
| Advantages |
| Minimally invasive |
| Early rehabilitation |
| Quicker recovery |
| Decreased hospitalization time |
| Ability to assess and treat concurrent lesion (labral lesions and impingement issues) |
| Disadvantages |
| Meticulous technique and technically demanding |
| Steep learning curve |
| Accessibility limited only to anterior aspect of OCD lesion of femoral head |
| Possibility of all potential complications of hip arthroscopy |
| Donor-site morbidity |
OCD, osteochondritis dissecans.
The indications for the described technique are OCD lesions at the anterosuperior or anterolateral aspect of the femoral head and grade III and IV OCD lesions according to the International Cartilage Repair Society classification (Table 3). The contraindications for this technique include OCD lesions at the center and/or posterior aspect of the femoral head because of the inability to achieve access arthroscopically, as well as infection surrounding the hip joint and osteoarthritis.
Table 3.
Surgical Indications and Contraindications
| Indications |
| OCD lesion at anterosuperior and anterolateral aspect of femoral head |
| ICRS grade III or IV OCD lesion |
| Contraindications |
| OCD lesion at posterior and/or center aspect of femoral head (inability to access) |
| Infection surrounding anterolateral aspect of hip joint |
| Severe chondral damage at acetabulum, as detected on preoperative MRI |
| Osteoarthritis progressive to Tönnis grade II or III |
NOTE. Anterolateral, midanterior, and proximal midanterior portals are established for the described technique.
ICRS, International Cartilage Repair Society; MRI, magnetic resonance imaging; OCD, osteochondritis dissecans.
We recognize that data from only 1 patient, with 2 years’ follow-up, provide only limited information about clinical outcome, but this case does show the technical feasibility of the procedure. The long-term clinical outcome from multiple cases will be required to establish the clinical benefits of our approach. In conclusion, arthroscopic antegrade OAT is technically feasible for treating an OCD lesion with femoroacetabular impingement of the femoral head.
Footnotes
The authors report the following potential conflict of interest or source of funding: S.U. receives support from BioMed, DePuy Synthesis, Smith & Nephew, Stryker, and Daiichi Sankyo.
Supplementary Data
Hip arthroscopic osteochondral autologous transplantation for treating osteochondritis dissecans of femoral head. The patient was placed in the supine position with traction. Capsule release using a beaver knife and radiofrequency probe (VAPR) was performed to improve accessibility of the arthroscope and surgical instruments. A proximal midanterior portal (PMAP) was used to access the osteochondritis dissecans lesion, with the hip at 10° of extension. A decision was made that osteochondral transplantation was necessary. Viewing from the anterolateral portal, the surgeon resected the degenerative cartilage lesion using a shaver and a curette through the PMAP. The osteochondral autograft transplantation technique was performed using the Mosaicplasty autologous osteochondral grafting system. The diameter of the lesion was determined to be 8.5 mm by using a chisel perpendicular to the articular surface. A cylindrical autologous osteochondral graft was harvested from the ipsilateral knee joint. At the recipient site, a drill guide was inserted at a 90° angle to the recipient site, through the PMAP, while the surgeon was viewing from an arthroscope located in the anterolateral portal. The subchondral bone was drilled to a depth of 14 mm. The dilator was inserted into the drill guide and tapped to the desired depth. The osteochondral autograft was placed over the lesion and tamped into position until the articular surface was flush with the host joint surface.
References
- 1.Guilleminet M., Barbier J.M. Osteochondritis dissecans of the hip. J Bone Joint Surg Br. 1957;39:268–277. doi: 10.1302/0301-620X.39B2.268. [DOI] [PubMed] [Google Scholar]
- 2.Moulonguet M.P. Detection of osteochondritis dissecans lesions of the femoral head with origin from certain coxarthroses. Rev Rhum Mal Osteoartic. 1952;19:547–549. [in French] [PubMed] [Google Scholar]
- 3.Clanton T.O., DeLee J.C. Osteochondritis dissecans. History, pathophysiology and current treatment concepts. Clin Orthop Relat Res. 1982;167:50–64. [PubMed] [Google Scholar]
- 4.Evans K.N., Providence B.C. Case report: Fresh-stored osteochondral allograft for treatment of osteochondritis dissecans the femoral head. Clin Orthop Relat Res. 2010;468:613–618. doi: 10.1007/s11999-009-0997-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lea M.A., Barkatali B., Porter M.L., Board T.N. Osteochondral lesion of the hip treated with partial femoral head resurfacing. Case report and six-year follow-up. Hip Int. 2014;24:417–420. doi: 10.5301/hipint.5000121. [DOI] [PubMed] [Google Scholar]
- 6.Matsuda D.K., Safran M.R. Arthroscopic internal fixation of osteochondritis dissecans of the femoral head. Orthopedics. 2013;36:e683–e686. doi: 10.3928/01477447-20130426-37. [DOI] [PubMed] [Google Scholar]
- 7.Larson C.M., Wulf C.A. Intraoperative fluoroscopy for evaluation of bony resection during arthroscopic management of femoroacetabular impingement in the supine position. Arthroscopy. 2009;25:1183–1192. doi: 10.1016/j.arthro.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 8.Uchida S., Wada T., Sakoda S. Endoscopic shelf acetabuloplasty combined with labral repair, cam osteochondroplasty, and capsular plication for treating developmental hip dysplasia. Arthrosc Tech. 2014;3:e185–e191. doi: 10.1016/j.eats.2013.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Emre T.Y., Cift H., Seyhan B., Ceyhan E., Uzun M. Mosaicplasty for the treatment of the osteochondral lesion in the femoral head. Bull NYU Hosp Jt Dis. 2012;70:288–290. [PubMed] [Google Scholar]
- 10.Girard J., Roumazeille T., Sakr M., Migaud H. Osteochondral mosaicplasty of the femoral head. Hip Int. 2011;21:542–548. doi: 10.5301/HIP.2011.8659. [DOI] [PubMed] [Google Scholar]
- 11.Nam D., Shindle M.K., Buly R.L., Kelly B.T., Lorich D.G. Traumatic osteochondral injury of the femoral head treated by mosaicplasty: A report of two cases. HSS J. 2010;6:228–234. doi: 10.1007/s11420-010-9159-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gagala J., Tarczynska M., Gaweda K. Fixation of femoral head fractures with autologous osteochondral transfer (mosaicplasty) J Orthop Trauma. 2014;28:e226–e230. doi: 10.1097/BOT.0000000000000079. [DOI] [PubMed] [Google Scholar]
- 13.Cetinkaya S., Toker B., Taser O. Arthroscopic retrograde osteochondral autologous transplantation to chondral lesion in femoral head. Orthopedics. 2014;37:e600–e604. doi: 10.3928/01477447-20140528-64. [DOI] [PubMed] [Google Scholar]
- 14.Hangody L., Kish G., Karpati Z., Szerb I., Udvarhelyi I. Arthroscopic autogenous osteochondral mosaicplasty for the treatment of femoral condylar articular defects. A preliminary report. Knee Surg Sports Traumatol Arthrosc. 1997;5:262–267. doi: 10.1007/s001670050061. [DOI] [PubMed] [Google Scholar]
- 15.Marcacci M., Kon E., Zaffagnini S. Multiple osteochondral arthroscopic grafting (mosaicplasty) for cartilage defects of the knee: Prospective study results at 2-year follow-up. Arthroscopy. 2005;21:462–470. doi: 10.1016/j.arthro.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 16.Marlovits S., Singer P., Zeller P., Mandl I., Haller J., Trattnig S. Magnetic resonance observation of cartilage repair tissue (MOCART) for the evaluation of autologous chondrocyte transplantation: Determination of interobserver variability and correlation to clinical outcome after 2 years. Eur J Radiol. 2006;57:16–23. doi: 10.1016/j.ejrad.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 17.Tetta C., Busacca M., Moio A. Knee osteochondral autologous transplantation: Long-term MR findings and clinical correlations. Eur J Radiol. 2010;76:117–123. doi: 10.1016/j.ejrad.2009.05.011. [DOI] [PubMed] [Google Scholar]
- 18.Edmonds E.W., Heyworth B.E. Osteochondritis dissecans of the shoulder and hip. Clin Sports Med. 2014;33:285–294. doi: 10.1016/j.csm.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 19.LaPrade R.F., Botker J.C. Donor-site morbidity after osteochondral autograft transfer procedures. Arthroscopy. 2004;20:e69–e73. doi: 10.1016/j.arthro.2004.06.022. [DOI] [PubMed] [Google Scholar]
- 20.Reddy S., Pedowitz D.I., Parekh S.G., Sennett B.J., Okereke E. The morbidity associated with osteochondral harvest from asymptomatic knees for the treatment of osteochondral lesions of the talus. Am J Sports Med. 2007;35:80–85. doi: 10.1177/0363546506290986. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Hip arthroscopic osteochondral autologous transplantation for treating osteochondritis dissecans of femoral head. The patient was placed in the supine position with traction. Capsule release using a beaver knife and radiofrequency probe (VAPR) was performed to improve accessibility of the arthroscope and surgical instruments. A proximal midanterior portal (PMAP) was used to access the osteochondritis dissecans lesion, with the hip at 10° of extension. A decision was made that osteochondral transplantation was necessary. Viewing from the anterolateral portal, the surgeon resected the degenerative cartilage lesion using a shaver and a curette through the PMAP. The osteochondral autograft transplantation technique was performed using the Mosaicplasty autologous osteochondral grafting system. The diameter of the lesion was determined to be 8.5 mm by using a chisel perpendicular to the articular surface. A cylindrical autologous osteochondral graft was harvested from the ipsilateral knee joint. At the recipient site, a drill guide was inserted at a 90° angle to the recipient site, through the PMAP, while the surgeon was viewing from an arthroscope located in the anterolateral portal. The subchondral bone was drilled to a depth of 14 mm. The dilator was inserted into the drill guide and tapped to the desired depth. The osteochondral autograft was placed over the lesion and tamped into position until the articular surface was flush with the host joint surface.