Abstract
Lupus erythematosus (LE) with erythema multiforme-like lesions with its characteristic serological picture had been described in 1963. We report a 33-year-old married male who presented with skin lesions of various morphology on different body parts since four months. The skin lesions ranged from lupus-specific tumid LE to Rowell's syndrome and discoid LE. Histopathology of skin biopsy from all representative sites showed different forms of lupus erythematosus. Antinuclear and anti-double-stranded DNA was positive; however, serology for anti-SSA and anti-SSB was negative. There were no symptoms specific for organ involvement. It is unusual to document various morphological types in a single patient of lupus erythematosus. We document this case as all forms of cutaneous LE including Rowell's syndrome were evident in a single male patient.
Keywords: Discoid LE, lupus erythematosus, Rowell's syndrome, tumid LE
INTRODUCTION
Lupus erythematosus (LE) is an inflammatory connective tissue disease with variable manifestations. According to Gilliam's classification, cutaneous LE can be into chronic cutaneous LE (CCLE), subacute cutaneous LE (SCLE) and acute cutaneous LE (ACLE) all of which are accompanied by their specific stigmata.[1,2] The diagnosis and subclassification of LE is based, by convention, on the correlation of clinical manifestations with serological abnormalities. Rowell's syndrome (RS) is a rare presentation of lupus erythematosus (LE) with erythema multiforme-like lesions associated with antinuclear, anti-La (SS-B)/anti-Ro (SS-A) antibodies and rheumatoid factor (RF) positivity, which was described first in 1963.[3] RS is considered to be more common among females as overall incidence of cutaneous LE is higher among females.[4]
CASE REPORT
A 33-year-old married male presented to our clinic with multiple red to skin colored lesions on various body parts since four months associated with mild pruritus. He also reported to have multiple similar lesions on his back with central duskiness. Two months prior to reporting, he noticed dark colored patch on both the temples with occasional itching on sun exposure. During the same period, he noticed three smooth patches of hair loss on scalp with some scaling. The patient had no history of oral erosion, fever, chilblains, or joint pain. There was no history suggestive of neither internal organ involvement nor any neuropsychiatric disturbance. The patient did not give history of any drug consumption prior to eruption of skin lesions or unprotected sexual intercourse. Based on history and clinical examination, differential diagnosis of erythema nodosum leprosum, erythema multiforme, actinic lichen planus, and secondary syphilis were kept.
A detailed cutaneous examination showed multiple skin colored to erythematous papules of size 1–2 cm on flexor aspect of both forearms [Figure 1]. Extensor aspect of arms showed irregular erythematous scaly plaques with mild scaling and atrophic changes. Both the temple areas showed hyperpigmented ill-defined patches with few scattered macules on pinna [Figure 2]. Extensor of elbows and lower back revealed multiple well-defined irregular erythematous papules with central duskiness with few lesions showing targetoid morphology [Figure 3]. Scalp showed patches of cicatricial alopecia with follicular plugging [Figure 4]. There were no lesions on palms and soles. His oral and genital examinations were normal. Complete physical and systemic examinations were within normal reference range. His complete blood count (Hb 11.8 g/dL, white blood cell count 6700/mm3, platelets 206 × 103/mm3), serum chemistry (blood urea nitrogen 18 mg/dL, serum creatinine 0.8 mg/dL, alanine transaminase 14 U/L, aspartate transaminase 22 U/L) urinalysis were within normal limits. Serology for retroviral infection, herpes, and syphilis were negative. Antinuclear antibody (ANA) 23.59 IU/mL (positive: >20) and anti-dsDNA antibody 1.10 (positive: >1.00 optical density ratio) measured by solid phase enzyme immunoassay were positive with speckled pattern of ANA staining on immunofluorescence. However, antibodies for both soluble substance A (SSA/Ro) 2.06 RU/mL and soluble substance B (SSB/La) 1.88 RU/mL measured by enzyme immunoassay were negative (positive > 20 and above RU/mL for both SSA and SSB).
Figure 1.

Multiple skin-colored papules on volar forearm, which were lesions of tumid LE on biopsy
Figure 2.

Hyperpigmented patches on both temple areas. Note few hyperpigmented macules on pinna (shown by white arrow). Biopsy was consistent with discoid LE
Figure 3.

Multiple erythematous well- to ill-defined papules and plaques on lower back with center of the lesion showing duskiness and dyspigmentation. Biopsy showed features of RS
Figure 4.

A patch of cicatricial alopecia on the scalp, which was discoid lupus erythematosus on biopsy
Skin biopsy was drawn from the scalp, forearm, temple, and back under local anesthesia. Hematoxylin and eosin–stained section of the skin biopsy from the scalp and temple showed orthokeratotic stratum corneum, focal interface changes, dilated and plugged hair follicles, superficial and deep perivascular with periappendigeal lymphocytic infiltrate consistent with discoid lupus erythematosus [Figure 5]. Skin biopsy from forearm lesion showed superficial and deep lymphocytic infiltrate with pools of mucin in reticular dermis and deep lobular lymphocytic infiltrate of the panniculus, which was consistent with tumid LE [Figure 6]. Specimen from back lesion showed follicular orthokeratotic plug with interface dermatitis at the base of follicle with pools of mucin in deeper dermis characteristic of RS [Figure 7]. Direct immunofluorescence of the lesion skin was not done. Based on clinical (DLE, photosensitivity), laboratory (anemia, positive ANA, and anti-ds-DNA) and histopathology of lesional tissue, a diagnosis of LE with RS was made according to American College of Rheumatology (ACR criteria).
Figure 5.
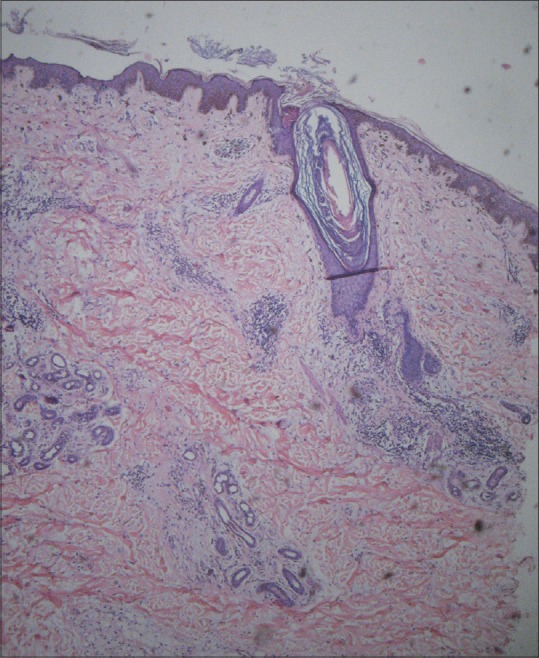
H and E-stained section from temple [Figure 2] showed moderately dense superficial and deep perivascular and periappendageal infiltrate of lymphocytes with focal interface vacuolar change. Dermoepidermal junction showed smudging with occasional necrotic keratinocytes/colloid bodies (×40)
Figure 6.
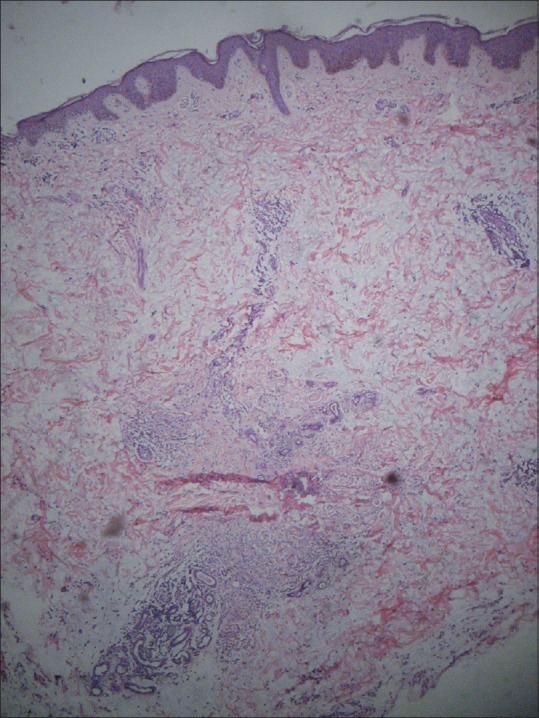
H and E-stained skin biopsy from forearm [Figure 1] showed moderately dense perivascular and periappendageal lymphocytic infiltrate in upper dermis and abundant deposits of mucin in reticular dermis
Figure 7.
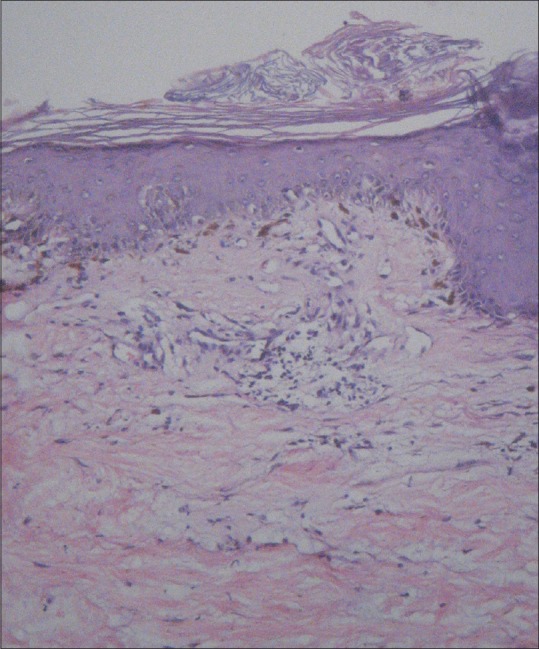
H and E specimen from lower back [Figure 3] mild vacuolar interface dermatitis with few foci of necrotic keratinocytes
The patient was started on oral prednisolone 40 mg, azathioprine 50 mg, hydroxychloroquine in dose of 200 mg twice daily along with topical mometasone furoate (0.1%) ointment and broad spectrum sunscreen (30 SPF). Two months after treatment, patient reported decrease in size of lesion and is in remission.
DISCUSSION
Shlotz in 1922 had first reported the association of erythema multiforme (EM) with lupus erythematosus.[5] In 1963, Neville Rowell and colleagues described a distinctive syndrome consisting of LE with EM-like lesions, speckled pattern antinuclear antibody (ANA), positive rheumatoid factor, and a precipitating antibody to saline extract of human tissues (anti-Sj-T) now regarded as similar to Ro(SSA).[6] The original criteria adopted by Rowell and colleagues for diagnosis of RS are as follows [Table 1].
Table 1.
Original criteria for Rowell's syndrome[3]
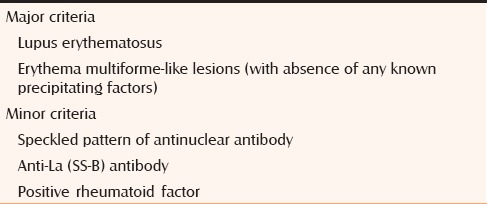
According to the original description, presence of two major and one minor criteria is required for making a diagnosis of RS. Recently in 2000, Zeitouni and colleagues have redefined this entity and proposed major and minor diagnostic criteria where chilblains were added as an additional criterion to distinguish RS from the coincidental association of erythema multiforme with LE [Table 2].[7]
Table 2.
New proposed criteria for Rowell's syndrome[7]
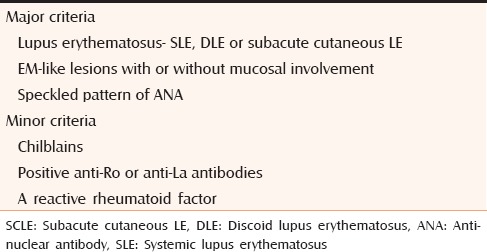
RS is defined by the presence of all major and one minor criteria.
However; RS has now been loosely interpreted as any type of cutaneous lupus lesion co-existing with erythema multiforme and associated with various serologies. A few authors have questioned the existence of RS as a distinct entity.[8] Our patient had all the major criteria but none of the minor criteria. Originally Rowell et al. have described erythema multiforme-like lesions in association with DLE, but various other authors have seen RS in association with SLE.[9,10] Khandpur et al. have reported two cases of RS in SLE who were negative for anti-Ro/SSA and anti-La/SSB.[10,11] In our patient, antibodies against both the soluble antigens were found to be negative, but as all the major criteria were met, we consider our case as a classic RS. Most of the cases reported until 2000 were in the females aged between 9 and 72 years.[10]
Before embarking on a diagnosis of RS, it is important to rule out common causes of erythema multiforme-like herpes and drugs. Our patient did not have any identifiable precipitating factor for erythema multiforme. Antiepileptic drug sodium valproate have been reported in causation of RS, however this association is yet to be substantiated.[12] Erythema multiforme of long duration or those not responding to a course of oral acyclovir should alert one of RS in background of appropriate serological tests.[13] However, cases of toxic epidermal necrolysis (TEN) in lupus erythematosus have been documented in the literature.[14,15,16] RS can progress into toxic epidermal necrolysis (TEN) as same pathogenetic process underlies both the condition. Acrosyringeal concentration of necrotic keratinocytes in erythema multiforme points toward drug etiology and can help in distinguishing between RS and drug-induced EM.[17] Marzano et al. and Pandhi et al. have reported cases of RS in association with antiphospholipid antibody syndrome.[6,18]
A high index of suspicion is needed for diagnosing RS. Treatment includes oral steroids in tapering doses, immunosuppressive agents (azathioprine, cyclophosphamide) along with antimalarial-like hydroxychloroquine or chloroquine.[10,19] Response to treatment is variable with frequent episodes of clinical exacerbation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Shadid NH, Thissen CA, van Marion AM, Poblete-Gutiérrez P, Frank J. Lupus erythematosus associated with erythema multiforme: Rowell's syndrome. Int J Dermatol. 2007;46(Suppl 3):30–2. doi: 10.1111/j.1365-4632.2007.03508.x. [DOI] [PubMed] [Google Scholar]
- 2.Crowson AN, Magro C. The cutaneous pathology of lupus erythematosus: A review. J Cutan Pathol. 2001;28:1–23. doi: 10.1034/j.1600-0560.2001.280101.x. [DOI] [PubMed] [Google Scholar]
- 3.Rowell's NR, Beck JS, Anderson JR. Lupus erythematosus and erythema multiforme-like lesions. A syndrome with characteristic immunological abnormalities. Arch Dermatol. 1963;88:176–80. doi: 10.1001/archderm.1963.01590200064012. [DOI] [PubMed] [Google Scholar]
- 4.Aydogan K, Karadogan S, Balaban Adim S, Tunali S. Lupus erythematosus associated with erythema multiforme: Report of two cases and review of the literature. J Eur Acad Dermatol Venereol. 2005;19:621–7. doi: 10.1111/j.1468-3083.2005.01233.x. [DOI] [PubMed] [Google Scholar]
- 5.Scholtz M. Lupus erythematosus acutus disseminatus haemorrhagicus. Arch Dermatol Syph. 1922;6:466. [Google Scholar]
- 6.Pandhi D, Singal A, Agarwal P. Rowell's syndrome and associated antiphospholipid syndrome. Clin Exp Dermatol. 2004;29:22–4. doi: 10.1111/j.1365-2230.2004.01433.x. [DOI] [PubMed] [Google Scholar]
- 7.Zeitouni NC, Funaro D, Cloutier RA, Gagné E, Claveau J. Redefining Rowell's syndrome. Br J Dermatol. 2000;142:343–6. doi: 10.1046/j.1365-2133.2000.03306.x. [DOI] [PubMed] [Google Scholar]
- 8.Shteyngarts AR, Warner MR, Camisa C. Lupus erythematosus associated with erythema multiforme: Does Rowell syndrome exist? J Am Acad Dermatol. 1999;40:773–7. doi: 10.1016/s0190-9622(99)70165-9. [DOI] [PubMed] [Google Scholar]
- 9.Dogra A, Minocha Y, Gupta M, Capalash P. Rowell's syndrome. Indian J Dermatol Venereol Leprol. 2000;66:324–5. [PubMed] [Google Scholar]
- 10.Khandpur S, Das S, Singh MK. Rowell's syndrome revisited: Report of two cases from India. Int J Dermatol. 2005;44:545–9. doi: 10.1111/j.1365-4632.2004.01995.x. [DOI] [PubMed] [Google Scholar]
- 11.Modi GM, Shen A, Mazloom A, Mawad J, Perez A, Sonabend ML, et al. Lupus erythematosus masquerading as erythema multiforme: Does Rowell syndrome really exist? Dermatol Online J. 2009;15:5. [PubMed] [Google Scholar]
- 12.Kacalak-Rzepka A, Kiedrowicz M, Bielecka-Grzela S, Ratajczak-Stefanska V, Maleszka R, Mikulska D. Rowell's syndrome in the course of treatment with sodium valproate: A case report and review of the literature data. Clin Exp Dermatol. 2009;34:702–4. doi: 10.1111/j.1365-2230.2008.02972.x. [DOI] [PubMed] [Google Scholar]
- 13.Khatri ML. Rowell's syndrome. Indian J Dermatol Venereol Leprol. 2000;66:262–3. [PubMed] [Google Scholar]
- 14.Mandelcorn R, Shear NH. Lupus-associated toxic epidermal necrolysis: A novel manifestation of lupus? J Am Acad Dermatol. 2003;48:525–9. doi: 10.1067/mjd.2003.107. [DOI] [PubMed] [Google Scholar]
- 15.Horne NS, Narayan AR, Young RM, Frieri M. Toxic epidermal necrolysis in systemic lupus erythematosus. Autoimmun Rev. 2006;5:160–4. doi: 10.1016/j.autrev.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 16.Paradela S, Martínez-Gómez W, Fernández-Jorge B, Castiñeiras I, Yebra-Pimentel T, Llinares P, et al. Toxic epidermal necrolysis-like acute cutaneous lupus erythematosus. Lupus. 2007;16:741–5. doi: 10.1177/0961203307079498. [DOI] [PubMed] [Google Scholar]
- 17.Zohdi-Mofid M, Horn TD. Acrosyringeal concentration of necrotic keratinocytes in erythema multiforme: A clue to drug etiology. Clinicopathological review of 29 cases. J Cutan Pathol. 1997;24:235–40. doi: 10.1111/j.1600-0560.1997.tb01587.x. [DOI] [PubMed] [Google Scholar]
- 18.Marzano AV, Berti E, Gasparini G, Caputo R. Lupus erythematosus with antiphospholipid syndrome and erythema multiforme-like lesions. Br J Dermatol. 1999;141:720–4. doi: 10.1046/j.1365-2133.1999.03118.x. [DOI] [PubMed] [Google Scholar]
- 19.Child FJ, Kapur N, Creamer D, Kobza Black A. Rowell's syndrome. Clin Exp Dermatol. 1999;24:74–7. doi: 10.1046/j.1365-2230.1999.00422.x. [DOI] [PubMed] [Google Scholar]


